Back to Journals » Clinical Interventions in Aging » Volume 11
The effect of nocturia on sleep quality and daytime function in patients with lower urinary tract symptoms: a cross-sectional study
Authors Shao I , Wu C, Hsu H, Chang S, Wang H, Chuang H, Tam Y
Received 20 January 2016
Accepted for publication 16 March 2016
Published 29 June 2016 Volume 2016:11 Pages 879—885
DOI https://doi.org/10.2147/CIA.S104634
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
I-Hung Shao,1,* Chia-Chen Wu,2,* Hueih-Shing Hsu,1 Shyh-Chyi Chang,1 Hsu-Hsiang Wang,1 Heng-Chang Chuang,1 Yuan-Yun Tam3
1Division of Urology, Department of Surgery, Lotung Poh-Ai Hospital, Yilan County, 2Department of Otorhinolaryngology – Head and Neck Surgery, Linkou Chang Gung Memorial Hospital, Chang Gung University, Taoyuan, 3Department of Otorhinolaryngology – Head and Neck Surgery, Lotung Poh-Ai Hospital, Yilan County, Taiwan, Republic of China
*These authors contributed equally to this work
Background: Nocturia has been proven to have a negative impact on the quality of life and sleep quality in general elderly population. However, there are limited studies on the quantitative effect of nocturia on sleep quality and daytime dysfunction, specifically in patients with lower urinary tract symptoms.
Patients and methods: During March 1, 2015 to December 31, 2015, a total of 728 patients who visited our urology department due to voiding dysfunction and experienced nocturia at least once per night were enrolled. Three questionnaires were administered to them after obtaining their written consents. Pittsburgh Sleep Quality Index (PSQI) questionnaire, Epworth Sleepiness Scale (ESS) questionnaire, and International Prostate Symptom Score (IPSS) questionnaire were applied to evaluate their sleep quality, daytime dysfunction, and voiding problems, respectively. Statistical analysis of the impact of nocturia on sleep quality and daytime dysfunction was performed.
Results: The mean age of patients was 61 years, with a male-to-female ratio of 2.7. The mean nocturia number was 3.03. The IPSS, PSQI, and ESS scores were 17.56, 8.35, and 8.22, respectively. The nocturia number increased with age and was significantly correlated to ESS score (daytime dysfunction) and PSQI total score (sleep quality) in overall group. Among subgroups divided by age and sex, there was a significant correlation between nocturia number and daytime dysfunction in male patients or patients younger than 65 years.
Conclusion: In patients with lower urinary tract symptoms, nocturia number increased with age and was significantly correlated with poor sleep quality. Nocturia plays an important role in patients younger than 65 years in daytime dysfunction.
Keywords: nocturia, sleep quality, lower urinary tract symptoms, daytime dysfunction
A Letter to the Editor has been received and published for this article.
Introduction
The International Continence Society defines nocturia as the need to void one or more times during the night, with each of the voids preceded and followed by sleep. Nocturia has the following two main causes: increased nocturnal urine volume and vesical instability.1 As one of the most common complaints in patients with lower urinary tract symptoms (LUTS), nocturia is reported to negatively affect the quality of life and quality of sleep.2,3 Since its prevalence and severity increase with age,4 the negative effect of nocturia on the elderly requires more attention. Jensen et al5 reported that 25% of falls experienced by older individuals occur during the night and 25% of these occur when the individual is waking up to void.
Studies have shown a significant association between nocturia and sleep quality, but most of these investigations were among the general elderly population.6–8 Obayashi et al used objective actigraphy and subjective questionnaires to quantitatively evaluate the association between nocturnal voiding frequency and sleep quality in the general elderly population.9,10 Considerable number of patients with benign prostate hyperplasia, bladder outlet obstruction, overactive bladder, or other diseases that affect urinary function may suffer from nocturia, and there are some reports focusing on nocturia and sleep.6,11,12 However, studies on the quantitative effect of nocturia on both sleep quality and daytime function, specifically in adult patients with LUTS, are sparse. In this cross-sectional study of 728 individuals with LUTS, we used three survey tools to evaluate the effect of nocturia on sleep quality and daytime sleepiness.
Patients and methods
Participants and study protocol
Our study is a cross-sectional and questionnaire-based survey conducted among patients with LUTS and nocturia. Inclusion criteria were as follows: patients who visited our urologic department from March 1, 2015 to December 31, 2015 due to LUTS and experienced nocturia at least once per night were enrolled in this study. Exclusion criteria were as follows: patients with a history of drug treatment for LUTS and those with concomitant urinary tract infection or urolithiasis were excluded. A total of 728 patients met the criteria and completed the questionnaires. All patients provided written informed consent to participate in this study. The Cathay General Hospital Institutional Review Board approved the study protocol.
Data collection
We conducted our face-to-face survey based on three internationally validated, reliable, and widely used questionnaires, namely Pittsburgh Sleep Quality Index (PSQI) questionnaire,10,13 Epworth Sleepiness Scale (ESS) questionnaire,14,15 and International Prostate Symptom Score (IPSS) questionnaire. After obtaining their written informed consents, the patients were asked to complete the questionnaires at their first visit before medications for LUTS were prescribed, with the assistance of trained research assistants. Each interview took ~10–20 minutes.
Measuring sleep quality and daytime dysfunction
The PSQI questionnaire was used to evaluate sleep quality and disturbance over the past month. It contains 19 items. The first four items are open questions, and 5–19 items are rated on a four-point scale. The item scores yield the following seven subscores ranging from 0 to 3: sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleep medication use, and daytime dysfunction due to sleepiness. The total scores ranging from 0 to 21 were obtained by summing up the seven subscores. Most studies have consistently stated that a total PSQI score of ≤5 suggests a good sleep quality, whereas a total PSQI score of >5 suggests a poor sleep quality.10,13,16,17
The ESS questionnaire consists of eight questions that are rated on a four-point scale ranging from 0 to 3. A total score between 0 and 24 is used to evaluate our participants’ general level of daytime sleepiness or the average sleep propensity over the past month. An ESS score of >8 suggests significant sleepiness.14,16,17
Measuring LUTS
We used the IPSS questionnaire to evaluate their voiding dysfunction. It is a basic and widely used questionnaire used by urologists. It contains the seven-item American Urological Association (AUA) Symptom Index and one question on the quality of life, which is used to evaluate male LUTS, such as benign prostate hyperplasia-related voiding problem. The seven-item AUA Symptom Index, developed and psychometrically validated by an AUA Measurement Committee in 1992, reliably assesses the severity of LUTS and is responsive to changes in treatment.18 The World Health Organization in 1993 adopted the eight-item IPSS, which uses the same seven questions assessing LUTS severity as the AUA Symptom Index and an eighth disease-specific quality of life question that assesses the pain associated with LUTS. It has also been proven reliable for the evaluation of female patients with lower urinary tract dysfunction.19 The seven questions are divided into the following two parts: IPSS voiding scores and IPSS storage scores.20 The IPSS voiding scores consist of weak stream, intermittency, straining, and feeling of incomplete bladder emptying, whereas the IPSS storage scores consist of frequency, urgency, and nocturia. Each scoring ranges from 1 to 5 for a total of maximum 35 points. The eighth question on voiding-related quality of life is assigned a score of 0–6. The higher the score is, the lower the quality is.
Other parameters
Nocturia number was defined as the number of voids during the time from going to bed at night to waking up next morning, excluding the last void before bedtime and the first void after waking up in the morning. Patients’ basic characteristics, including age, sex, height, weight, and body mass index, were collected from their medical charts.
Statistical analyses
The statistical analyses were performed on a personal computer using the statistical package SPSS for Windows (Version 17.0, SPSS Inc., Chicago, IL, USA). We used generalized linear model to perform multivariate analysis between several parameters versus PSQI and ESS scores. We used the independent samples t-test to compare the differences of age, nocturia number, ESS score, PSQI score, and IPSS score between subgroups dividing by sex and age (<65 and ≥65 years). The associations between nocturia number and sleep quality (PSQI scores C1–C7 and total score) and daytime dysfunction (ESS score) were analyzed by Pearson’s correlation test. The analysis was performed not only for the overall patient group but also for the patients divided into subgroups according to age (older than and younger than 65 years) and sex (male and female). Pearson’s correlation test was used to compare the subgroups.
Results
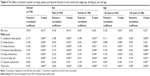
The patients’ characteristics and detailed subscale scores of IPSS, ESS, and PSQI are presented in Table 1. The mean age of the patients was 61.4±13.7 years, with a male-to-female ratio of 2.7. Of the 728 patients, 101 (13.9%) patients reported one nocturia episode, 188 (25.8%) patients reported two nocturia episodes, 170 (23.4%) patients reported three nocturia episodes, 124 (17.0%) patients reported four nocturia episodes, and 145 (19.9%) patients reported five or more nocturia episodes. The mean nocturia number was 3.03 per night. The mean IPSS total score, PSQI total score, and ESS score were 17.56±8.62, 8.35±3.66, 3.23±2.48, and 8.22±5.07, respectively. The results revealed that our participants have both poor sleep quality and daytime dysfunction compared to the normal population.10,13–16
The result of multivariate analysis using the generalized linear model is disclosed in Table 2. Taking the ESS total score as a dependent variable, we found that it is positively correlated with PSQI score with statistical significance, and the 95% confidence interval does not cover zero. While using the PSQI score as a dependent variable, we found that it is positively correlated with nocturia number and ESS score with statistical significance, and the 95% confidence interval does not cover zero. The PSQI score is higher in female patients.
By age and sex, we divided our participants into subgroups (male and female, <65 years and ≥65 years). The independent samples t-test was used to clarify the differences between them. The results are shown in Table 3. The mean age, nocturia number, IPSS storage score, and voiding-related quality of life were similar between different sex groups, whereas a higher PSQI total score, a lower IPSS voiding score, and a lower IPSS total score were found in female group with significant difference. Among subgroups of patients <65 and ≥65 years old, patients older than 65 years had significantly worse performance in all parameters, including nocturia number, PSQI total and subscores, IPSS total and subscores, and voiding-related quality of life, except for ESS score.
The effects of nocturia number on sleep quality and daytime function, which were analyzed using Pearson’s correlation test, are revealed in Table 4. In the overall group, the higher nocturia number was significantly correlated with the higher ESS score and the higher PSQI scores C1–C6 and total score but not for score C7. In subgroups divided by age, nocturia number was still significantly correlated with the higher ESS score in patients younger than 65 years, but it had no significant effect on ESS score in patients older than 65 years. The severity of nocturia significantly correlated with higher PSQI total score in both subgroups. For patients divided by sex, more nocturia number was still significantly correlated with ESS score in male patients but not in female patients. In both subgroups, the higher nocturia number was significantly correlated with higher PSQI total scores. The relationships between nocturia numbers and ESS score and PSQI score respectively are shown in Figure 1.
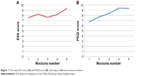  | Figure 1 The mean ESS score (A) and PSQI score (B) referring to different nocturia numbers. |
Discussion
Nocturia is a persistent LUTS and is often regarded as a natural consequence of aging.21 However, the negative effect of nocturia has been underestimated until recently, not only for its underreported prevalence7,22,23 but also for the resulting physical and psychiatric problems.2,3,24,25 Increasing numbers of studies are now describing the negative effect of nocturia on sleep quality, associated diseases, and mortality in the aging population. Most of the previous studies have reported an association between nocturia that was categorized using cutoff points but have not quantified its severity.9 In this study, we investigated the correlation of nocturia number with sleep quality and daytime dysfunction in patients with LUTS.
In this study, we also compared the differences of each parameter between males and females and patients older than or younger than 65 years. Female patients had similar nocturia number and daytime dysfunction but had significant worse sleep quality than male patients. Such a correlation was revealed by multivariate analysis in our study shown in Table 2. The average of PSQI total score was 9.80 in female and 7.80 in male patients, which is shown in Table 3. This is consistent with the relatively higher frequency of prescription sleep aids use in the female population,26 and in our data, the PSQI C6 scores were 0.69 and 0.43 among females and males, respectively (PSQI C6 score refers to use of sleeping medication: never =0; <1 per week =1; 1–2 per week =2; and ≥3 per week =3).10 The IPSS storage score for females was similar to that for males, but the IPSS voiding score was significantly lower for females than for males. The high prevalence of prostatic disorder-related voiding dysfunction in aging males could explain this finding.20 As for age, in patients older than 65 years, all parameters were significantly worse than those in the younger group, except for similar ESS scores, which were compatible with some published study results.7–9 In multivariate analysis, PSQI score was positively correlated with age, but the ESS score was not.
Nocturia has been recognized as a potential risk for sleep disturbance.27 Our study also found that the severity of nocturia increased significantly with age in patients with LUTS. More severe nocturia also significantly correlated with worse sleep quality and daytime dysfunction. However, score C7 (daytime dysfunction) is not correlated with higher nocturia number (Table 4), which is not compatible with other published studies.28 This inconsistency with ESS score could be explained by the fact that the score C7 ranges from 0 to 3 while the ESS score ranges from 0 to 24. We suggested that ESS score is a more definite and detailed evaluation for daytime dysfunction. We found that the negative effect of nocturia on daytime dysfunction (ESS score) among patients older than 65 years and female patients was not statistically significant. This phenomenon could be explained by the fact that the subjective perception of daytime dysfunction is more obvious and stronger in people with jobs who need higher concentration and focus. Most patients older than 65 years were retired from active work, and the impact of nocturia on daytime function is easily overlooked. Foley et al28 reported that frequent napping is common among older adults or patients without employment to compensate their sleep disruption. A similar situation exists for the female subgroup of our participants. A considerably high proportion (68%) of our female participants were housewives, for whom working hours are more flexible and who have less need to concentrate for a long time. Such result suggested that nocturia plays an important role in patients younger than 65 years in daytime dysfunction, and hence treating nocturia might improve their work performance. Clinically, this blunt perception of the effect of nocturia on daytime spirit and dysfunction among aging people might also be one of the causes of nocturia being underestimated or regarded as a natural consequence of getting older and resulting in delays in seeking treatment.
We used questionnaires to quantify the negative effect of nocturia not only on sleep quality but also on daytime function among patients with LUTS. We also evaluated the severity of nocturia, rather than using a binary yes-or-no measure, and found a significant correlation. However, the evaluations of sleep quality and daytime dysfunction were based on subjective perception only. More objective tools, such as actigraphy and polysomnography, may provide more accurate information on actual sleep quality in future studies. The male-to-female ratio was 2.7, reflecting the fact that our patients were sourced mainly from the urologic department. The relatively small size of the female population may have affected the statistical analysis. In Table 4, Pearson’s correlation coefficients are not high but still with statistical difference, which might result from the large number of our participants. In order to emphasize on the effect of nocturia numbers, more prospective studies are also needed.
Conclusion
In patients with LUTS, nocturia number increased with age and was significantly correlated with poor sleep quality. Nocturia plays an important role in patients younger than 65 years in daytime dysfunction, which should not be overlooked. With similar nocturia number, female patients reported worse sleep quality, with higher rate of sleeping pill use.
Acknowledgment
The authors wish to acknowledge the support of the Biostatistical Center for Clinical Research of Linkou Chang Gung Memorial Hospital (CLRPG3D0041).
Disclosure
The authors report no conflicts of interest in this work.
References
van Kerrebroeck P, Abrams P, Chaikin D, et al; Standardisation Sub-committee of the International Continence Society. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21(2):179–183. | ||
Hetta J. The impact of sleep deprivation caused by nocturia. BJU Int. 1999;84(suppl 1):27–28. | ||
Ancoli-Israel S, Bliwise DL, Norgaard JP. The effect of nocturia on sleep. Sleep Med Rev. 2011;15(2):91–97. | ||
Schatzl G, Temml C, Schmidbauer J, Dolezal B, Haidinger G, Madersbacher S. Cross-sectional study of nocturia in both sexes: analysis of a voluntary health screening project. Urology. 2000;56(1):71–75. | ||
Jensen J, Lundin-Olsson L, Nyberg L, Gustafson Y. Falls among frail older people in residential care. Scand J Public Health. 2002;30(1):54–61. | ||
Asplund R. Nocturia in relation to sleep, somatic diseases and medical treatment in the elderly. BJU Int. 2002;90(6):533–536. | ||
Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E. The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA. BJU Int. 2003;92(9):948–954. | ||
Bing MH, Moller LA, Jennum P, Mortensen S, Skovgaard LT, Lose G. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60–80 years. BJU Int. 2006;98(3):599–604. | ||
Obayashi K, Saeki K, Kurumatani N. Quantitative association between nocturnal voiding frequency and objective sleep quality in the general elderly population: the HEIJO-KYO cohort. Sleep Med. 2015;16(5):577–582. | ||
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. | ||
Bal K, Ayik S, Issi Y, Bolukbasi A, Akhan G. Sleep analysis of patients with nocturia and benign prostatic obstruction. Urology. 2012;80(2):383–388. | ||
Endeshaw YW, Johnson TM, Kutner MH, Ouslander JG, Bliwise DL. Sleep-disordered breathing and nocturia in older adults. J Am Geriatr Soc. 2004;52(6):957–960. | ||
Tsai PS, Wang SY, Wang MY, et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14(8):1943–1952. | ||
Chen NH, Johns MW, Li HY, et al. Validation of a Chinese version of the Epworth sleepiness scale. Qual Life Res. 2002;11(8):817–821. | ||
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. | ||
Buysse DJ, Hall ML, Strollo PJ, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4(6):563–571. | ||
Mondal P, Gjevre JA, Taylor-Gjevre RM, Lim HJ. Relationship between the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in a sleep laboratory referral population. Nat Sci Sleep. 2013;5: 15–21. | ||
Barry MJ, Fowler FJ Jr, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1549–1557; discussion 64. | ||
Hsiao SM, Lin HH, Kuo HC. International Prostate Symptom Score for assessing lower urinary tract dysfunction in women. Int Urogynecol J. 2013;24(2):263–267. | ||
Jiang YH, Lin VC, Liao CH, Kuo HC. International Prostatic Symptom Score-voiding/storage subscore ratio in association with total prostatic volume and maximum flow rate is diagnostic of bladder outlet-related lower urinary tract dysfunction in men with lower urinary tract symptoms. PLoS One. 2013;8(3):e59176. | ||
van Dijk L, Kooij DG, Schellevis FG, Kaptein AA, Boon TA, Wooning M. Nocturia: impact on quality of life in a Dutch adult population. BJU Int. 2004;93(7):1001–1004. | ||
Umlauf MG, Goode S, Burgio KL. Psychosocial issues in geriatric urology: problems in treatment and treatment seeking. Urol Clin North Am. 1996;23(1):127–136. | ||
MacDiarmid S, Rosenberg M. Overactive bladder in women: symptom impact and treatment expectations. Curr Med Res Opin. 2005;21(9):1413–1421. | ||
Kobelt G, Borgstrom F, Mattiasson A. Productivity, vitality and utility in a group of healthy professionally active individuals with nocturia. BJU Int. 2003;91(3):190–195. | ||
Feldstein CA. Nocturia in arterial hypertension: a prevalent, underreported, and sometimes underestimated association. J Am Soc Hypertens. 2013;7(1):75–84. | ||
Pillai V, Cheng P, Kalmbach DA, Roehrs T, Roth T, Drake CL. Prevalence and predictors of prescription sleep-aid use among individuals with DSM-5 insomnia: the role of hyperarousal. Sleep. Epub 2016 Jan 15. | ||
Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, Walsh JK. Nocturia and disturbed sleep in the elderly. Sleep Med. 2009;10(5):540–548. | ||
Foley DJ, Vitiello MV, Bliwise DL, Ancoli-Israel S, Monjan AA, Walsh JK. Frequent napping is associated with excessive daytime sleepiness, depression, pain, and nocturia in older adults: findings from the National Sleep Foundation ‘2003 Sleep in America’ Poll. Am J Geriatr Psychiatry. 2007;15(4):344–350. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.