Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
The effect of night shift on sleep quality and depressive symptoms among Chinese nurses
Authors Dai C, Qiu H, Huang Q, Hu P, Hong X, Tu J, Xie Q, Li H, Ren W, Ni S, Chen F
Received 12 October 2018
Accepted for publication 17 January 2019
Published 7 February 2019 Volume 2019:15 Pages 435—440
DOI https://doi.org/10.2147/NDT.S190689
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jun Chen
Caijun Dai,1,* Huihua Qiu,2,* Qiqi Huang,2,* Pinglang Hu,2 Xianchai Hong,2 Junwei Tu,1 Qiangli Xie,2 Haiyan Li,2 Wenwei Ren,2 Shuhong Ni,1 Fujian Chen3
1Jinhua Municipal Central Hospital, Jinhua 321000, China; 2The First Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, China; 3Anji County People’s Hospital, Huzhou 313300, China
*These authors contributed equally to this work
Purpose: Night shift is associated with adverse physical and psychological health outcomes such as poor sleep quality and depressive symptoms. We aimed to compare sleep quality as well as depressive symptoms in nurses working night shifts to those working day shifts only and explore the association between sleep quality and depressive symptoms among nurses.
Patients and methods: Eight hundred sixty-five nurses were enrolled in the current study. Sleep quality and depressive symptoms among nurses were evaluated by the Pittsburgh Sleep Quality Index (PSQI) and Hospital Anxiety and Depressive Disorders Rating Scale (HADS), respectively.
Results: PSQI and HADS scores were both significantly higher in the nurses working night shifts (P<0.05) than in those working day shifts only. Besides, there was a positive correlation between PSQI and HADS scores. Binary logistic regression showed that night shift and poor sleep quality were independent risk factors of depressive symptoms among nurses.
Conclusion: Higher rates of depression among Chinese nurses working night shifts may be associated with poor sleep quality induced by night shift.
Keywords: nurse, depression, night shift, sleep
Introduction
As a result of growing demand for quality of care, rising public expectations and economic constraints, nurses are continually under both acute and chronic workplace stressors which predispose them to vulnerability to psychological disorders such as depression.1 In the United States, the prevalence of depressive symptoms is approximately twice as high among registered nurses in hospitals as in the general population.2 Recently, China has reported a series of violent injuries to medical workers, which has attracted worldwide attention.3 As revealed in a survey including 588 nurses in China, the rates of physically and nonphysically violent experiences were 7.8% and 71.9%, respectively,4 which might bring additional psychological pressure to Chinese nurses. Therefore, early recognition of depressive symptoms among Chinese nurses is of great importance, which is an essential step in the prevention of adverse consequences to patients, nurses and health care organizations.5
Hospitals are institutions where service is given for 24 hours 7 days a week and nurses are largely locked into schedules including night shift.6 Unfortunately, night shift may negatively impact work–life balance and social interactions, resulting in greater mental distress.7 Moreover, previous studies have revealed that night shift is associated with an increased risk of depressive symptoms.8–10
Night shift is known to disturb the cortisol and melatonin rhythms,11 which is tightly associated with sleep quality.12,13 One of the most common complaints of night-shift workers is a lack of adequate sleep during the day following a night shift.14,15 A study revealed that nurses working night shifts had worse sleep quality that negatively impacted their health status.16 Besides, sleep quality is also associated with depressive symptoms. As shown in an epidemiological study, sleep disturbances were reported in up to 90% of individuals with depressive symptoms.17 Similarly, another study reported that shorter sleep duration across 6 months predicted depression severity in patients who developed an episode.18
The role of sleep quality in the association between night shift and disturbed physiological and psychological health status had been investigated in several previous studies.19,20 However, none of the previous studies has ever explored the role of sleep quality in the association between night shift and depressive symptoms among nurses. Based on the close relationship among night shift, sleep quality and depressive symptoms, we hypothesize that poor sleep quality may play a role in the association between depressive symptoms and night shift among Chinese nurses. The objective of this study was to investigate 1) the association between depressive symptoms and night shift among nurses and 2) the association between depressive symptoms and sleep quality among nurses.
Patients and methods
Patients and study design
This cross-sectional study was implemented from June to October 2017 in Jinhua Municipal Central Hospital in Zhejiang Province (Southern China). One thousand two hundred eighty-eight nurses were invited to complete self-administered anonymous questionnaires and 423 nurses declined to take part in for no interest. Finally, 865 nurses agreed to participate and completed self-administered anonymous questionnaires. According to self-report, nurses working night shifts were those whose work shifts involved night work, which was defined by having a work schedule encompassing midnight. The most common start and end hour of the night shift was 11:00 pm and 8:00 am. Besides, day shifts were defined by having a work schedule during 8:00 am to 11:00 pm, which included the evening shifts.
The study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Research Ethics Committee in Jinhua Municipal Central Hospital. All the participants had read the purpose statement of the investigation and signed an informed consent.
Clinical variables and assessments
In the study questionnaire, data on participants’ sociodemographic variables and other clinically relevant variables were collected. Information on clinical variables was collected using the following instrument:
Sleep quality of the patients was evaluated by Pittsburgh Sleep Quality Index (PSQI), which is a commonly used 19-item psychometrically validated measure of sleep quality and disturbances. It has a score range of 0–21, with scores ≤5 associated with good sleep quality and >5 associated with poor sleep quality.21
Depressive symptoms were measured using Hospital Anxiety and Depressive Disorders Rating Scale (HADS).22 The items were scored on a 4-point scale, with responses ranging from 0 (not present) to 3 (considerable), with higher score indicating higher symptom levels. Participant with a score >7 was considered to have depressive symptoms.
Statistical analysis
Baseline characteristics were compared using ANOVA for continuous variables and chi-squared test for categorical variables. Fisher’s exact test was used for categorical variables in the cases where the assumptions underlying chi-squared test were not fulfilled.
Pearson correlation was performed for bivariate correlation between PSQI and HADS scores. The influence of night shift and sleep quality on depressive symptoms was estimated by binary logistic regression analysis. To control the effects of potential confounders, factors with P<0.05 in the univariate analysis between groups were included in the logistic regression analysis. The results were indicated as adjusted OR (95% CI). Statistical analysis was performed using SPSS 20.0 (SPSS Inc., Chicago, IL, USA). Two-tailed P-values <0.05 were considered statistically significant.
Results
Among the 865 nurses, 353 (40.8%) were considered to have depressive symptoms. As shown in Table 1, compared to nurses working day shifts only, nurses working night shifts were younger, with lower job rank and marriage rate, higher PSQI and HADS scores, and longer working hours (all P<0.05). Besides, there was also a positive correlation between PSQI and HADS scores (r=0.428, P<0.001).
  | Table 1 Demographic, lifestyle and clinical characteristics for two groups |
As shown in Table 2, with all nurses taken as a whole, depression symptoms’ occurrence taken as a dependent variable, the logistic regression analysis demonstrated that night work was independently associated with the presence of depressive symptoms (OR, 1.832; 95% CI, 1.232–2.724, P=0.003), with the age, marriage status, work hours and job rank being controlled. Moreover, nurses with poor sleep quality were also at higher risk of depression (OR, 2.558; 95% CI, 1.704–3.839, P<0.001). In addition, marriage status was associated with depressive symptoms (OR, 1.751; 95% CI, 1.237–2.478, P=0.002).
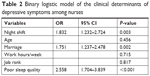  | Table 2 Binary logistic model of the clinical determinants of depressive symptoms among nurses |
Discussion
The main findings of this study were the following: 1) nurses working night shifts showed more depressive symptoms than those working day shifts only; 2) nurses with poorer sleep quality showed more depressive symptoms; 3) nurses working night shifts showed poorer sleep quality than those working day shifts only. Higher rates of depressive symptoms in nurses working night shifts may be associated with poorer sleep quality induced by night shift.
The prevalence of depressive symptoms among nurses in this study (40.8%) was within the range of rates reported in previous studies in China,23,24 which was higher than that reported in western countries such as France and the United States.25,26 The relatively high prevalence of depressive symptoms among Chinese nurses may be due to heavy workload, rising public expectations and unsatisfactory nurse–patient relationship caused by medical disputes.27
The relationship among sleep, cognitive and mental health has been studied in other contexts. For instance, previous studies in workers had observed that shift work may lead to poor sleep quality and diseases such as diabetes and hypertension.28 Besides, good sleep quality may increase cognitive skills and reduce depressive symptoms of workers aged over 45 years.29 Moreover, several previous studies in different contexts found that shift work was associated with poor sleep quality, depressive symptoms and fatigue in nurses.30–33 Consistent with previous studies, the present research found that nurses working night shifts showed poorer sleep quality and nearly 2-fold increased risk of depression than those working day shifts. The main contribution of this paper is to analyze the role of sleep quality and depressive symptoms among Chinese nurses, which can extend previous studies. The disturbed circadian rhythms induced by night shift may explain for the findings.34 Several studies had also demonstrated that circadian rhythm disturbances were associated with sleep quality and depressive symptoms,30,35–37 which may be attributable to abnormal patterns of cortisol secretion and disruption of social rhythms.38 In addition, it had been reported that treatment of the disruption of circadian rhythms may improve depressive symptoms.39
The present study also found a positive correlation between poor sleep quality and depressive symptoms, which was in accord with earlier findings.40,41 In addition, sleep quality in individuals with depressive symptoms could predict treatment outcomes. Several studies found that poor sleep quality predicted poor response to nonpharmacological and/or pharmacological treatments of depressive symptoms.42,43 Based on the relationship among night shift, sleep quality and depressive symptoms, we may infer that the sleep quality may play a role in the association between night shift and depressive symptoms among Chinese nurses. The role of poor sleep quality in the association between night shift and depressive symptoms might be explained by the disturbance of the internal circadian rhythm or insufficient recovery due to sleep disorders.44 Several clinical observations supported that the various expressions of mood disorders may result from circadian dysregulation.45 For example, patients with depressive symptoms showed abnormalities in phase timing, with a phase-advanced elevation of nocturnal body temperature occurring over the 24-hour diurnal cycle. Besides, patients with depressive symptoms showed increased cortisol secretion and a phase advance in its rhythm,46 whereas, in healthy individuals, maximal secretion of cortisol occurs in the morning, followed by a progressive reduction throughout the day until a nadir is reached in the evening. Moreover, previous studies in patients with depressive symptoms reported reductions in melatonin secretion and phase delays in the circadian rhythm of melatonin.47,48 In addition, previous studies had also demonstrated that disruption of social rhythms was associated with depressive symptoms.38,49
However, conflicting findings have been noticed. In a study among Norwegian nurses, no significant differences were observed between night shift and depressive symptoms as well as sleepiness.50 Inconsistencies in the existing literature might be explained by the difference in medical system, workload, work settings and work environments.
Several limitations of this study should be mentioned. First, owing to the cross-sectional nature of the present study, causal inference of the night shift with sleep quality and depressive symptoms cannot be confirmed. Future studies should adopt a longitudinal study design to confirm the causal relations among night shift, sleep quality and depressive symptoms. Despite the direction of causation, the fact that nurses working night shifts had greater risks of poor sleep quality and depressive symptoms still poses a health concern about nurses working night shifts. Second, owing to the limitation of the questionnaire design, work schedules could only be classified into day vs night shifts, leaving other domains of shift work undetermined. Finally, nurses working night shifts were younger, had lower job rank and worked longer hours. These factors might impose some selection bias on the results, although we had adjusted for these potential confounders in the logistic regression analysis. Future research should improve the assessment of shift work patterns. Finally, aggression and violence among nurses were not measured.
Conclusion
This study shows that higher rates of depressive symptoms in nurses working night shifts may be associated with poorer sleep quality induced by night shift. Considering previous studies in different contexts, the main contribution of this paper is to analyze the role of sleep quality and depressive symptoms among Chinese nurses. Further investigation may focus on a longitudinal study to confirm the causal relations among night shift, sleep quality and depressive symptoms.
Acknowledgments
The authors thank all study participants who were involved and contributed to the procedure of data collection. Caijun Dai, Huihua Qiu and Qiqi Huang should be considered joint first author.
Author contributions
FC, SN and CD designed the study and wrote the protocol; CD, HQ, QH, PH and XH conducted literature searches and provided summaries of previous research studies. JT, QX, HL and WR conducted the statistical analysis. CD and HQ wrote the first draft of the manuscript. All authors reviewed and approved the final version of the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Mealer M, Burnham EL, Goode CJ, Rothbaum B, Moss M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depress Anxiety. 2009;26(12):1118–1126. | ||
Letvak S, Ruhm CJ, McCoy T. Depression in hospital-employed nurses. Clin Nurse Spec. 2012;26(3):177–182. | ||
Yang T, Zhang H, Shen F, Li J-W, Wu M-C. Appeal from Chinese doctors to end violence. Lancet. 2013;382(9906):1703–1704. | ||
Jiao M, Ning N, Li Y, et al. Workplace violence against nurses in Chinese hospitals: a cross-sectional survey. BMJ Open. 2015;5(3):e006719. | ||
Brown P, Fraser K, Wong CA, Muise M, Cummings G. Factors influencing intentions to stay and retention of nurse managers: a systematic review. J Nurs Manag. 2013;21(3):459–472. | ||
Korompeli A, Muurlink O, Tzavara C, Velonakis E, Lemonidou C, Sourtzi P. Influence of shiftwork on Greek nursing personnel. Saf Health Work. 2014;5(2):73–79. | ||
Vogel M, Braungardt T, Meyer W, Schneider W. The effects of shift work on physical and mental health. J Neural Transm. 2012;119(10):1121–1132. | ||
Bara AC, Arber S. Working shifts and mental health – findings from the British Household Panel Survey (1995–2005). Scand J Work Environ Health. 2009;35(5):361–367. | ||
Silva Ddos S, Tavares NV, Alexandre AR, et al. Depression and suicide risk among nursing professionals: an integrative review. Rev Esc Enferm USP. 2015;49(6):1023–1031. | ||
Gong Y, Han T, Yin X, et al. Prevalence of depressive symptoms and work-related risk factors among nurses in public hospitals in southern China: a cross-sectional study. Sci Rep. 2015;4(1):7109. | ||
Weibel L, Brandenberger G. Disturbances in hormonal profiles of night workers during their usual sleep and work times. J Biol Rhythms. 1998;13(3):202–208. | ||
Steiger A. Sleep and the hypothalamo-pituitary-adrenocortical system. Sleep Med Rev. 2002;6(2):125–138. | ||
Reiter RJ, Tan DX, Fuentes-Broto L. Melatonin: a multitasking molecule. Progress in Brain Research. 2010;181:127–151. | ||
Ferguson SA, Baker AA, Lamond N, Kennaway DJ, Dawson D. Sleep in a live-in mining operation: the influence of start times and restricted non-work activities. Appl Ergon. 2010;42(1):71–75. | ||
Tucker P, Folkard S, Ansiau D, Marquié JC. The effects of age and shiftwork on perceived sleep problems: results from the VISAT combined longitudinal and cross-sectional study. J Occup Environ Med. 2011;53(7):794–798. | ||
Huth JJ, Eliades A, Handwork C, Englehart JL, Messenger J. Shift worked, quality of sleep, and elevated body mass index in pediatric nurses. J Pediatr Nurs. 2013;28(6):e64–e73. | ||
Tsuno N, Besset A, Ritchie K, Clin J. Sleep and depression. J Clin Psychiatry. 2005;66(10):1254–1269. | ||
Perlman CA, Johnson SL, Mellman TA. The prospective impact of sleep duration on depression and mania. Bipolar Disord. 2006;8(3):271–274. | ||
Silva-Costa A, Griep RH, Rotenberg L. Disentangling the effects of insomnia and night work on cardiovascular diseases: a study in nursing professionals. Braz J Med Biol Res. 2015;48(2):120–127. | ||
Vallières A, Azaiez A, Moreau V, Leblanc M, Morin CM. Insomnia in shift work. Sleep Med. 2014;15(12):1440–1448. | ||
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. | ||
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. | ||
Gao YQ, Pan BC, Sun W, Wu H, Wang JN, Wang L. Depressive symptoms among Chinese nurses: prevalence and the associated factors. J Adv Nurs. 2012;68(5):1166–1175. | ||
Lin HS, Probst JC, Hsu YC. Depression among female psychiatric nurses in southern Taiwan: main and moderating effects of job stress, coping behaviour and social support. J Clin Nurs. 2010;19(15–16):2342–2354. | ||
Welsh D. Predictors of depressive symptoms in female medical-surgical hospital nurses. Issues Ment Health Nurs. 2009;30(5):320–326. | ||
Nourry N, Luc A, Lefebvre F, Sultan-Taïeb H, Béjean S. Psychosocial and organizational work environment of nurse managers and self-reported depressive symptoms: cross-sectional analysis from a cohort of nurse managers. Int J Occup Med Environ Health. 2014;27(2):252–269. | ||
Ending violence against doctors in China. Lancet. 2012;379(9828):1764. | ||
Guo Y, Liu Y, Huang X, et al. The effects of shift work on sleeping quality, hypertension and diabetes in retired workers. PLoS One. 2013;8(8):e71107. | ||
Giuntella O, Han W, Mazzonna F. Circadian rhythms, sleep, and cognitive skills: evidence from an Unsleeping giant. Demography. 2017;54(5):1715–1742. | ||
Kim HS, Choi KS, Eom M, Joo EJ. Role of circadian types and depressive mood on sleep quality of shift work nurses. Korean J Psychopharmacol. 2011;22(2):96–104. | ||
Son YJ, Park YR. Relationships between sleep quality, fatigue and depression on health promoting behavior by shift-work patterns in university hospital nurses. J Korean Biol Nurs Sci. 2011;13(3):229–237. | ||
Chan MF. Factors associated with perceived sleep quality of nurses working on rotating shifts. J Clin Nurs. 2010;18(2):285–293. | ||
Lin SH, Liao WC, Chen MY, Fan JY. The impact of shift work on nurses’ job stress, sleep quality and self-perceived health status. J Nurs Manag. 2014;22(5):604–612. | ||
McClung CA. How might circadian rhythms control mood? Let me count the ways. Biol Psychiatry. 2013;74(4):242–249. | ||
Hori H, Koga N, Hidese S, et al. 24-h activity rhythm and sleep in depressed outpatients. J Psychiatr Res. 2016;77:27–34. | ||
Maglione JE, Ancoli-Israel S, Peters KW, et al. Depressive symptoms and circadian activity rhythm disturbances in community-dwelling older women. Am J Geriatr Psychiatry. 2014;22(4):349–361. | ||
Bumb JM, Enning F, Mueller JK, et al. Differential melatonin alterations in cerebrospinal fluid and serum of patients with major depressive disorder and bipolar disorder. Compr Psychiatry. 2016;68:34–39. | ||
Peeters F, Nicolson NA, Berkhof J. Levels and variability of daily life cortisol secretion in major depression. Psychiatry Res. 2004;126(1):1–13. | ||
Jones SG, Benca RM. Circadian disruption in psychiatric disorders. Sleep Med Clin. 2015;10(4):481–493. | ||
Klumpp H, Roberts J, Kapella MC, Kennedy AE, Kumar A, Phan KL. Subjective and objective sleep quality modulate emotion regulatory brain function in anxiety and depression. Depress Anxiety. 2017;34(7):651–660. | ||
Ohayon MM, Caulet M, Lemoine P. Comorbidity of mental and insomnia disorders in the general population. Compr Psychiatry. 1998;39(4):185–197. | ||
Lowe A, Rajaratnam SM, Hoy K, Taffe J, Fitzgerald PB. Can sleep disturbance in depression predict repetitive transcranial magnetic stimulation (rTMS) treatment response? Psychiatry Res. 2013;210(1):121–126. | ||
Manglick M, Rajaratnam SM, Taffe J, Tonge B, Melvin G. Persistent sleep disturbance is associated with treatment response in adolescents with depression. Aust N Z J Psychiatry. 2013;47(6):556–563. | ||
Szuba MP, Yager A, Guze BH, Allen EM, Baxter LR Jr. Disruption of social circadian rhythms in major depression: a preliminary report. Psychiatry Res. 1992;42(3):221–230. | ||
Monteleone P, Maj M. The circadian basis of mood disorders: recent developments and treatment implications. Eur Neuropsychopharmacol. 2008;18(10):701–711. | ||
Cervantes P, Gelber S, Kin FN, Nair VN, Schwartz G. Circadian secretion of cortisol in bipolar disorder. J Psychiatry Neurosci. 2001;26(5):411–416. | ||
Nair NP, Hariharasubramanian N, Pilapil C. Circadian rhythm of plasma melatonin in endogenous depression. Prog Neuropsychopharmacol Biol Psychiatry. 1984;8(4–6):715–718. | ||
Claustrat B, Chazot G, Brun J, Jordan D, Sassolas G. A chronobiological study of melatonin and cortisol secretion in depressed subjects: plasma melatonin, a biochemical marker in major depression. Biol Psychiatry. 1984;19(8):1215–1228. | ||
Haynes PL, Ancoli-Israel S, McQuaid J. Illuminating the impact of habitual behaviors in depression. Chronobiol Int. 2005;22(2):279–297. | ||
Øyane NM, Pallesen S, Moen BE, Åkerstedt T, Bjorvatn B. Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One. 2013;8(8):e70228. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
