Back to Journals » International Journal of Women's Health » Volume 11
The effect of amniotomy on urine protein creatinine ratio test accuracy
Authors Herrera Gonzalez A , Quinn S, Lennon J, Zabo J, Dierking E, Anasti J
Received 11 January 2019
Accepted for publication 23 April 2019
Published 10 June 2019 Volume 2019:11 Pages 371—375
DOI https://doi.org/10.2147/IJWH.S201210
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Aaron Herrera Gonzalez, Sara Quinn, Jessica Lennon, Jordan Zabo, Elizabeth Dierking, James Anasti
St. Luke’s University Health Network, Department of Obstetrics and Gynecology, Bethlehem, PA, USA
Introduction: While the gold standard for evaluation of maternal urinary protein is a 24-hr urine collection, spot urine protein/creatinine ratio has been instituted as an alternative for quantification proteinuria. Though it seems intuitive to obtain a catheterized urine sample on patients with ruptured amniotic membranes, it is a common practice to forgo this step under the argument that there is no data to show its necessity. Data on the effect of amniotomy, spontaneous or artificial, on the accuracy of the protein/creatinine ratio are scant. The present study was designed to address this issue and objectively compare protein/creatinine ratio values on samples obtained from the same patient before and after amniotomy.
Methods: We conducted a prospective non-interventional study. Women presenting in active labor or for labor induction with intact amnion were enrolled. Separate random catch urines for the protein/creatinine ratio were obtained prior to and immediately after spontaneous or assisted amniotomy. The urine samples were analyzed in the hospital chemistry department, and the results were compared.
Results: Of the 137 patients consented, 63 had pre- and post-amniotomy protein/creatinine ratios collected. The mean age was 28.5±5.6 y, Gravidity 2.7±1.6, Gestational age 39.2±1.8 wks, and BMI 31.6±6.4 kg/m2. Comorbidities included gestational diabetes (5/63, 7.9%), chronic hypertension (3/63, 4.7%), and pre-eclampsia (5/63, 7.9%). Post-amniotomy protein/creatinine ratio was significantly higher than pre-amniotomy ratio (1.3±2.5 vs 0.34±0.83, p<0.001). In addition, the number of patients with protein/creatinine ratio greater than 0.3 was higher post-amniotomy than pre-amniotomy (41/63 vs 14/63, p<0.001).
Conclusion: Amniotomy results in a false elevation of the protein/creatinine ratio in term patients. Urine samples should be obtained by catheterization in the setting of ruptured membranes to reduce falsely elevated results. Although the same can be assumed for other gestational ages, further studies including this population need to be conducted.
Keywords: amniotic fluid, protein creatinine ratio, preeclampsia, urine protein, pregnancy, gestational hypertension
Introduction
Preeclampsia is a multi-system disorder characterized by new-onset hypertension with proteinuria and/or end-organ dysfunction, which occurs at the 20th week of gestation or later. The exception to this time of presentation can be seen in multiple gestations, eg, twin, triplet gestations, as well as molar pregnancies in which preeclampsia can develop earlier than 20 weeks gestation. It is estimated to occur in 3.4% of the pregnancies in the United States, and over the past two decades, has increased by 25%.1–3 Preeclampsia can result in significant maternal and fetal morbidity and mortality, thus timely diagnosis is crucial.
When blood pressure is equal or higher than 140 mmHg for systolic or 90 mmHg for diastolic on two occasions at least 4 hrs apart in gestations greater than 20 weeks, evaluation for preeclampsia should ensue. This should include blood pressure monitoring and laboratory testing to evaluate for both end-organ dysfunction and urine protein levels.
The gold standard for evaluation of maternal proteinuria is a 24-hr urine collection with protein of 300 mg/dL or greater considered abnormal.1 The results of a 24-hr urine collection are not immediately available to guide the management of a patient with new-onset hypertension.
In both pregnant and non-pregnant patients, a spot urine protein/creatinine ratio has been validated for the evaluation of urine protein excretion in individuals with hypertension (HTN), diabetes, and renal disease.4,5
Furthermore, in studies involving pregnant patients, a similarly high correlation between a 24-hr protein collection and a random urine protein/creatinine ratio have been noted.6–9 Due to these findings, the protein/creatinine ratio has been adopted as first line in the evaluation of preeclampsia in pregnant patients, with a value of 0.3 or greater suggesting a 24-hr urine protein of at least 300 mg.1,10 One benefit of the spot urine protein/creatinine ratio is that the results are available within hours following a random urine collection, which facilitates prompt evaluation, diagnosis, and management of preeclampsia.
Ruptured amniotic membranes are a common clinical situation for a patient to present to the labor and delivery floor, with coexisting potential for the same patient to have either a history of gestational hypertension or elevated blood pressures appreciated at time of hospital presentation. Amniotic fluid in the third trimester is composed of fetal urine, fetal lung fluid, and fetal mucous membranes secretions, containing growth factors, carbohydrates, lipids, urea, and most importantly, proteins. Intramembranous transfer of fluid and solutes across the amniotic membranes changes the composition of the amniotic fluid.11
Information is limited as to the appropriate method for urine collection in the setting of spontaneous rupture of membranes or amniotomy.6–10
In patients without rupture of membranes, there seems to be no difference on the mode of collection, ie, clean catch versus catheterized sampling.12
The goal of this study was to determine whether or not amniotic fluid leads to falsely elevated protein levels on non-catheterized maternal urine samples used for the calculation of protein/creatinine ratio as part of the diagnostic work up for preeclampsia.
Methods
This is a prospective non-interventional study conducted between June 2016 and December 2016 at St. Luke’s University Health Network, a community tertiary care center with locations in Allentown and Bethlehem, Pennsylvania. This study was approved by the St. Luke’s University Health Network Institutional Review Board. All women admitted in active labor or for induction of labor, who were greater than 24 weeks gestation, and with intact membranes were approached for inclusion in the study. Both verbal and written informed consent was obtained from all patients and this study was conducted in accordance with the Declaration of Helsinki.
Women were excluded if they had preexisting renal disease, known proteinuria of greater than 300 mg in a 24-hr urine specimen, gross hematuria, an untreated urinary tract infection (UTI), placental abruption, age younger than 18 years, or presented for a scheduled cesarean section. Informed consent was obtained from each patient. A random, non-clean catch urine specimen was collected on admission (preROM) and immediately after the rupture of membranes (postROM), whether spontaneous or artificial. These specimens were sent to the St. Luke’s University Health Network chemistry department for analysis. Samples not indicated for direct clinical care were run in daily batches. Many, but not all, paired samples were run in the same batch. The Dimension Vista Intelligent Lab System Flex reagent cartridge (Siemens Healthcare, Erlangen, Germany) was employed to determine the protein and creatinine components, followed by a computer-calculated ratio.13 Women acted as their own controls, and samples were obtained regardless of the patient’s hypertension status.
A sample size of 84 was needed to find a difference of 0.35 in the protein/creatinine ratio, with an estimated standard deviation of 0.80 (Power 80%, p=0.05). Pre- and postROM protein/creatinine ratio values were compared using paired t-test or Mann–Whitney Rank Sum test, as appropriate. Proportions of patients with a protein/creatinine ratio >0.30 before and after rupture of membranes were compared using chi-squared test. All values are listed as the mean±standard deviation, unless otherwise specified. Statistical analysis was performed on Sigma-Stat statistical software (Systat Software, San Jose, CA).
Results
Overall, 137 patients were consented to participate in the study, with 74 patients unable to provide a postROM urine sample due to inability to void after epidural analgesia. These patients were subsequently excluded from the study. Therefore, 63 patients with complete data for analysis participated in the study. The patient demographics and comorbidities are listed in Table 1. The average age was 28.5 y±5.6 with an average gestational age of 39.2 weeks±1.8 and a mean BMI of 31.6 kg/m2±6.4. Comorbidities included preeclampsia (5/63, 7.9%), gestational diabetes (5/63, 7.9%), and chronic hypertension (3/63, 4.7%). Artificial rupture of membranes was performed in 49 of 63 patients (78%) (Table 1).
 | Table 1 Patient characteristics |
The mean protein/creatinine ratio preROM was 0.34±0.83 with 21.5% (14/63) of the patients having a protein/creatinine ratio greater than 0.3. An increase in protein/creatinine ratio was noted in 56 (89%) patients postROM. Six (9.5%) patients were noted to have a decrease in postROM protein/creatinine ratio, and no change was noted in one patient. The mean protein/creatinine ratio postROM was 1.3±2.5 with 65% (41/65) of the patients having a protein/creatinine ratio greater than 0.30 (Table 2). The mean protein/creatinine ratios before and after rupture of membranes were significantly different (p<0.001), as was the proportion of patients with protein/creatinine ratio greater than 0.3 before and after rupture of membranes (P<0.001). In addition, this difference remained significant even after excluding patients with pre-eclampsia or chronic hypertension. An interim analysis of the results obtained prior to complete enrollment of our target population showed statistical significance, thus enrollment was terminated early.
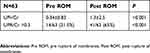 | Table 2 Urine/protein ratios before and after amniotomy |
Discussion
As suspected, rupture of membranes caused a dramatic effect on the protein/creatinine ratio, with 41/63 (65%) patients in our study population demonstrating an abnormal protein/creatinine ratio after rupture of membranes, either artificial or spontaneous. If we excluded the patients with preeclampsia, 37/59 (63%) still had an elevated postROM protein/creatinine ratio greater than 0.3. In addition, we noted that 14 of 63 (22%) patients had an elevated preROM protein/creatinine ratio, which was an unexpected secondary finding.
Chen et al suggests that clean catch urine should be used due to possible vaginal secretion contamination which would falsely elevate the protein/creatinine ratio.10 However, no supporting reference was provided in the article, and there was no control group utilizing a random urine collection for comparison to the clean catch specimen protein/creatinine ratio included in their study. The original studies that validated urine spot protein/creatinine ratio as a predictor of 24-hr total urine protein used random non-clean catch random urines specimens.5,7,8,14 In those studies, the urine protein/creatinine ratios had an r value of 0.93–0.99 in estimating total protein excreted in 24 hrs, thus demonstrating a high correlation. However, the status of membranes was not reported. At our institution, we use a Siemens-based test to determine the protein/creatinine ratio. In the product insert, the company states that no special patient preparation is necessary.
In an effort to explain the elevated protein/creatinine ratio appreciated in 14 pre-rupture samples, a detailed chart review of these patients was performed. This included a search for any obvious reasons for an initial elevated protein/creatinine ratio value, such as active or current treatment for bacterial vaginosis or other vaginal infection, vaginal bleeding upon admission, or an admission workup for leakage of fluid and possible rupture of membranes. One patient was noted to have minimal vaginal bleeding upon arrival. The majority of these patients were admitted for induction of labor for different indications, and none of them were found to have rupture of membranes on admission to the hospital. Additionally, 8 of these 14 patients had a markedly elevated postROM sample, which was more than double their preROM result. No identifiable cause was found in the majority of the normotensive patients with elevated pre-rupture protein/creatinine ratio, and the reason for this difference remains elusive. One possibility is the average gestational age in our study was 39.2 weeks, which is significantly different from the prior study which had a mean gestational age of 29.8 weeks.9 This later gestational age may have accounted for the increase in contaminating proteins such as a vaginal transudate, especially for those in labor. Another explanation for the ten patients who had an elevation in both the preROM and postROM samples, without elevated blood pressures, could be gestational proteinuria, which is a diagnosis of exclusion.15
The present study shows that ruptured membranes, with the ensuing amniotic fluid contamination of urine sample, can cause a significant elevation in the urine protein/creatinine ratio. For patients with preeclampsia, the cut-off for the spot urine protein/creatinine ratio has been the subject of debate, with values between 0.21 and 0.30 being suggested.6,16 We chose 0.3 because it is the cut-off proposed by the American College of Obstetricians and Gynecologists (ACOG).1 In term patients, like those enrolled in this study, the presence of an elevated urine protein/creatinine in individuals with elevated blood pressures (but not in the severe range) would not have altered management. However, falsely elevated urine protein/creatinine ratio may lead to unnecessary interventions in future pregnancies. The U.S. Preventive Services Task Force and ACOG do not recommend aspirin administration in patients with a history of gestational hypertension, but they do for those with a history of preeclampsia.1,17,18 Therefore, a falsely elevated protein/creatinine ratio would prompt physicians to administer aspirin to patients without additional risk factors for preeclampsia, such as multifetal gestation, chronic hypertension, type 1 or 2 diabetes, or renal disease. Aspirin has proven benefit in the management of certain at-risk pregnant populations; however, some studies have reported an increased frequency on postpartum hemorrhage with the recommendation of balancing benefits versus potential higher risk of postpartum hemorrhage.
After an extensive electronic PUBMED and MEDLINE literature search for English and Spanish articles using the Medical Subject Heading (MeSH) Keywords, Amniotic fluid, protein creatinine ratio, preeclampsia, urine protein, pregnancy, gestational hypertension, we were unable to find any studies directly addressing the effect on amniotic fluid on protein/creatinine ratio results. As such, to the best of our knowledge, this is at least one of the first if not the only study conducting a prospective non-interventional study to prove amniotic fluid affects the accuracy of the protein/creatinine ratio test.
The most recent study we found assessing protein creatinine ratio results in the pregnant population, investigated the level of proteinuria in the antepartum and postpartum period, in both vaginal and cesarean section delivery modes. This study used a catheter in the same patient for sampling before and after delivery.12 The fact that our patients served as their own controls avoided additional confounding variables. Our study was carried out in a busy community labor and delivery floor and answers an everyday question in a common clinical environment.
One of the limitations of our study was the high attrition rate secondary to inability to void following epidural analgesia. In trying to overcome this obstacle, attempts were made to have the patient void on a bedpan. However, the amount of urine voided was extremely small, and the specimen composition was virtually all amniotic fluid. Thus, we abandoned bedpan voids in this study. Another limitation is that we did not have clean catch urine specimens, catheterized urine specimens, or 24-hr urine protein specimens to compare with our results. The ability to obtain the two data sets used in this study simultaneously, along with findings from previous studies that validate the use of random urine specimens justifies the current study design.7,19
This important clinical question should be addressed in future studies.
Given that our patient population was term pregnancies either in labor or admitted for induction, the results of this study can only prove that amniotomy significantly elevates protein creatinine ratio in this specific group. One could postulate that this is likely the case in all states of ROM at all gestational ages, however additional studies would be necessary to prove it.
In conclusion, the present study proved that in patients at term with ruptured membranes, protein creatinine ratio was significantly elevated when collected without a catheter and suggests that in the setting of ruptured amniotic membranes, the use of a straight or Foley catheter should be used for sample collection in patients who need urine protein creatinine ratio determination.
Precis
Amniotomy results in a false elevation of the protein/creatinine ratio.
Acknowledgments
The abstract of this paper was presented at the American College of Obstetrics and Gynecology annual meeting 2017 at San Diego, California, USA, as an abstract presentation with interim findings. The poster abstract was published in “poster abstracts” in the Green Journal and can be found at:
Disclosure
The authors report no conflicts of interest in this work.
References
1.
2.
3. Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. Br Med J. 2013;347:f6564.
4. Ginsberg JM, Chang BS, Matarese RA, Garella S. Use of single voided urine samples to estimate quantitative proteinuria. N Engl J Med. 1983;309(25):1543–1546. doi:10.1056/NEJM198312223092503
5. Morris RK, Riley RD, Doug M, Deeks JJ, Kilby MD. Diagnostic accuracy of spot urinary protein and albumin to creatinine ratios for detection of significant proteinuria or adverse pregnancy outcome in patients with suspected preeclampsia: systematic review and meta-analysis. Br Med J. 2012;345:e4342
6. Wheeler TL, Blackhurst DW, Dellinger EH, Ramsey PS. Usage of spot urine protein to creatinine ratios in the evaluation of preeclampsia. Am J Obstet Gynecol. 2007;196:5. doi:10.1016/j.ajog.2006.12.016
7. Roudsari FV, Ayati S, Ayatollahi H, Shakeri MT. Protein/creatinine ratio on random urine samples for prediction of proteinuria in preeclampsia. Hypertens Pregnancy. 2010;31(2):240–242. doi:10.3109/10641955.2010.507838
8. Boler L, Zbella EA, Gleicher N. Quantitation of proteinuria in pregnancy by the use of single voided urine samples. Obstet Gynecol. 1987;70(1):99–100.
9. Neithardt AB, Dooley SL, Borensztajn J. Prediction of 24-hour protein excretion in pregnancy with a single voided urine protein-to-creatinine ratio. Am J Obstet Gynecol. 2002;186(5):883–886.
10. Chen BA, Parviainen K, Jeyabalan A. Correlation of catheterized and clean catch urine protein/creatinine ratios in preeclampsia evaluation. Obstet Gynecol. 2008;112(3):606–610. doi:10.1097/AOG.0b013e3181827c89
11. Underwood MA, Gilbert WM, Sherman MP. Amniotic fluid: not just fetal urine anymore. J Perinatol. 2005;25:341–348. doi:10.1038/sj.jp.7211290
12. Aziz MM, Kulkarni A, Shah L, Lashley S, Oyelese Y. Physiologic proteinuria in labor and postpartum: the results of postpartum proteinuria. Pregnancy Hypertens. 2018;13:22–24. doi:10.1016/j.preghy.2018.04.019
13. Dimension Vista Flex reagent cartridge [package insert]. Erlkangen, Germany: Siemens; 2015.
14. Papanna R, Mann LK, Kouides RW, Glantz JC. Protein/creatinine ratio in preeclampsia. Obstet Gynecol. 2008;112(1):135–144. doi:10.1097/AOG.0b013e3181778cfc
15. Gabbe SG. Obstetrics: Normal and Problem Pregnancies. Philadelphia (PA): Elsevier; 2017.
16. Robert M, Sepandj F, Liston RM, Dooley KC. Random protein-creatinine ratio for the quantitation of proteinuria in pregnancy. Obstet Gynecol. 1997;90(6):893–895. doi:10.1016/S0029-7844(97)00536-X
17. Henderson JT, Whitlock EP, O’Connor E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;160:695–703. doi:10.7326/M13-2844
18. Final recommendation statement: low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: preventive medication. U.S. Preventive Services Task Force. December 2016. Available from: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/low-dose-aspirin-use-for-the-prevention-of-morbidity-and-mortality-from-preeclampsia-preventive-medication
19. Van Vliet E, Askie L, Mol B, Antiplatelet OM. Agents and the prevention of spontaneous preterm birth. Obstet Gynecol. 2017;129(2):327–336. doi:10.1097/AOG.0000000000001848
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
