Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
The Effect of a Three-Level Remote Alliance on Critical Care in Grassroot Areas: A Multi-Center, Retrospective Study
Authors Feng X, Zhang G, Zhang S, Chen D, Zhou M, Zeng L, Yang T
Received 21 September 2022
Accepted for publication 17 November 2022
Published 9 December 2022 Volume 2022:15 Pages 2809—2815
DOI https://doi.org/10.2147/JMDH.S390711
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xiaodong Feng,1,* Guiliang Zhang,1,* Shiyang Zhang,2 Dihong Chen,3 Mengxue Zhou,1 Lihua Zeng,1 Tianmin Yang1
1Department of Critical Care Medicine, Mianzhu People’s Hospital, Mianzhu, 618200, People’s Republic of China; 2Department of Gastroenterology, Mianzhu People’s Hospital, Mianzhu, 618200, People’s Republic of China; 3Mianzhu People’s Hospital, Mianzhu, 618200, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaodong Feng, Department of Critical Care Medicine, Mianzhu People’s Hospital, No. 268, Section 1, Nanjing Avenue, Mianzhu, Sichuan Province, 618200, People’s Republic of China, Tel +8613518265506, Email [email protected]
Purpose: To explore an effective model to promote the homogeneous development of intensive care units (ICUs) in grassroot, impoverished and remote areas.
Methods: A three-level remote alliance model (in-place and online assistance) was adopted to guide the cross-talk of ICUs between counties and cities. The observed indicators included the mortality of ICU patients and those with APACHE II scores ≥ 15 points, deep vein thrombosis, ventilator-associated pneumonia, the completion rate of septic shock goals in 3-hour and 6-hour bundles, and the rates of patient transfers.
Results: After the implementation of the remote alliance, there was significant reduction in the mortality of ICU patients in the county and city-level tertiary hospitals (7.6% vs 4.5%, P = 0.004; OR = 1.734, 95% CI 1.189– 2.532) and the mortality rates of patients with APACHE II scores ≥ 15 points (11.9% vs 7.1%, P = 0.004; OR = 1.763, 95% CI 1.189– 2.614). There was a significant reduction in the incidence of ventilator-associated pneumonia (0.9% vs 5.0%, P < 0.001) and deep vein thrombosis (52.4% vs 13.6%, P < 0.001). The completion rate of 3-hour bundle therapies for septic shock was significantly improved (95.7% vs 68.4%, P < 0.001), as well as 6-hour bundle therapies for septic shock (97.9% vs 81.6%, P < 0.001). The hospital transfer rate decreased significantly in the grassroots and impoverished areas (2.6% vs 4.7%, P < 0.001).
Conclusion: A three-level remote alliance might be helpful in improving the quality of critical care in remote areas and promoting the homogeneous development of disciplines.
Keywords: medical quality, remote alliance, in-place and online, critical care medicine, mortality rate
Introduction
Critically sick patients are treated not just in metropolitan medical facilities but also in rural and outlying locations. Rural health care institutions demand that medical staffs perform as skilled generalists because they often provide treatment to patients with a variety of diseases during the same shift.1,2 Critical care physicians working in rural or distant locations may not have the chance to polish these more complicated skills or exercise them as often given that rural patients can be just as complex as those presenting in more metropolitan health care settings.2 All medical staffs working in rural or distant locations must care for the severely sick when the circumstance requires it since there is sometimes a limited number of critical care units. The regional development was uneven, with some remote and poor areas still utilising archaic medical technology, particularly for critically ill patients.3 In addition, the homogeneity of medical technology in various regions is low.4–7 Experts from developed areas have been dispatched to poor grassroots areas to provide support in recent years.8 Still, only a tiny expert pool is available for assignment to support these areas. This assistance has not been sufficient in addressing the problems with shortages in local medical personnel, outdated medical technology and difficulty in training medical personnel.
A recent survey of medical practitioners showed that the primary medical personnel demand for remote training and guidance reached 66.1% and 90.3%, respectively.9 This approach is promising in narrowing the gap in medical quality between urban and rural areas, as well as between rich and poor areas. Can remote training, advice and in-place teaching quickly improve medical access in remote areas, adequately train medical personnel and allow patients to receive standardised and homogeneous medical care? However, there are currently no relevant statistics to address these questions.
For this reason, we developed a three-level remote alliance model for critical care medicine that guides grassroots areas via in-place and online frameworks. In this study, we aimed to explore the effectiveness of this model in promoting the rapid development of critical care disciplines in grassroots, poor and remote areas.
Methods
Study Design and Population
This study included all patients admitted to the intensive care unit (ICU) of Mianzhu People’s Hospital (a county-level city hospital referred to as Mianzhu Hospital) from 2018 to 2019 and the People’s Hospital of County A in Liangshan Yi Autonomous Prefecture (referred to as Hospital A). This study is retrospective, and the patient data is strictly confidential and approved by the Ethics Committee of Mianzhu People’s Hospital. These were conducted depending on whether patients were admitted before or after the alliance was established. Those patients admitted in the year before the establishment (2018) were divided into the 2018 group, and the patients admitted one year after the establishment date were added to the 2019 group.
Three-Level Remote Alliance of Critical Care Medicine
The three-level remote alliance of critical care medicine was implemented between ICUs of three different care-level hospitals: the ICU of West China Hospital of Sichuan University (referred to as West China ICU), ranked fourth in the country in the “China Hospital Specialty Reputation Ranking” of Fudan University; Mianzhu Hospital, a grassroot, tertiary-level B general hospital; and a second-class B-level public hospital, which is a grassroots hospital located in a remote, poverty-stricken region. The three hospitals are remote and more than 300 kilometres from Hospital A. In addition, they are located in areas with many mountainous roads and inconvenient transportation, with a one-way commute averaging more than 6 hours.
The alliance was enacted on 21 December 2018. The ICU of West China Hospital is the leading guide of the ICU of Mianzhu Hospital. The ICU of Mianzhu Hospital primarily guides the ICU of Hospital A. However, both ICUs of West China and Mianzhu Hospitals advise the ICU of Hospital A on complex and unique problems, thus forming a three-level alliance. The work is done with in-place and online mode combinations, described as follows:
In-place mode: The guiding department routinely sends medical staff to the instructed hospital to supervise at least twice a month.
Online mode: All three hospital departments are equipped with hardware and software necessary for this method and to achieve efficient network and medical record data exchanges at least once a week, such as computers, cameras, microphones, RVs, and a Zhikang remote ward rounds system. Emergency guidance is available 24 hours a day with responses within 15 minutes and includes “four-line” department instruction. The alliance also conducts multiple remote academic activities such as medical record discussions, radiology reading meetings, educational lectures, scientific research report readings and nursing training every week.
Indicators
A third party was hired to check Mianzhu Hospital’s inpatient statistics tables, hospital infection detection statistics log, ICU nurse logs, acute physiology rates and chronic health status scoring system (acute physiology and chronic health evaluation scoring system, APACHE) registration forms. Data collected included the mortality rate statistics of ICU patients, patient mortality rates with an APACHE II score ≥15 points, the prevention rates of deep vein thrombosis, the incidences of ventilator-associated pneumonia, the completion rates of septic shock goals in 3-hour and 6-hour bundles and the incidences of ventilator-associated pneumonia (VAP). In addition, they reviewed the hospitalisation work statistics table of Hospital A and counted the patient transfer rates before and after the establishment of the remote alliance with Hospital A.
Acute physiology score, patient age, and chronic health status constitute the APACHE II score.10 Twelve physiological markers comprise the acute physiology score, including body temperature, blood pressure, heart rate, and others. The worst number during the first 24 hours after hospital admission will be chosen. A patient’s chronic health status is measured by how well their immune system is functioning. The APACHE II score might theoretically reach a maximum of 71 points; the higher the score, the more serious the patient’s condition. After 48 hours of ventilator support treatment and within 48 hours following tracheal intubation withdrawal, individuals with tracheal intubation may develop trachea, bronchi, or lung infections known as VAP.11 The clinical condition known as acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is characterized by a sudden deterioration of respiratory symptoms and airway function.12
Statistical Analysis
The SPSS version 21.0 software (IBM Corp. Silicon Valley, CA, USA) was used for data processing. The continuous data were tested for normality using the histogram or Q-Q plots. Variables with normal distribution were expressed as mean ± standard deviation and compared by the Student’ t-test. Variables with non-normal distribution were expressed as median (interquartile range) and compared by the Mann–Whitney U-test. The categorical data were expressed as counts (percentage) and compared by the Chi-square test. A two-tailed P-value of < 0.05 was considered statistically significant. PASS 15 Software (NCSS, LLC. Kaysville, Utah, USA) was used for sample size calculation. The power for the primary endpoint mortality was calculated based on the Chi-square test with a significance level of 5%. Group sample sizes of 736 in group 2018 and 736 in group 2019 achieved 90.019% power to detect a difference between the group proportions. The proportions in group 2018 and group 2019 were assumed to be 8% and 4%, respectively. The significance level of the test (alpha value) is 0.05.
Results
Baseline Characteristics
The ICU of Mianzhu Hospital has treated 1981 patients in two years, with 921 in the 2018 group and 1060 in the 2019 group. Hospital A admitted 56,245 patients, including 26,592 in the 2018 group and 29,653 in the 2019 group.
There were no statistically significant differences in essential characteristics such as age, gender, main disease composition, APACHE-II scores in the first 24 hours and expected mortality between the two groups in Mianzhu Hospital, and all were comparable. The results are shown in Table 1.
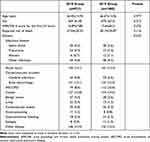 |
Table 1 Comparison of General Conditions of Two Groups of Patients in Mianzhu ICU |
Quality Indicators from Mianzhu Hospital ICU
There was a statistically significant difference in the case fatality rates between 2018 and 2019 (P = 0.004). Further comparison showed that the fatality rates in 2018 were significantly higher than in 2019. The mortality rate was further analysed by stratified statistical analysis. In the first 24 hours, patients with APACHE-II scores ≥ 15 points had a statistically significant difference in mortality rate (P = 0.004). The difference was higher in the 2018 case fatality rates than in 2019 (OR = 1.763, 95% CI range 1.189–2.614). These results are shown in Table 2. The DVT prevention rate, VAP, and the 3- and 6-hour bundle completion rates in the 2019 group were all statistically significant (P < 0.001) and higher than those in the 2018 group.
 |
Table 2 Comparison of ICU Quality Indicators in Mianzhu Hospital |
The Transfer Rate of Hospital A
There were 29,653 and 26,592 discharges in the 2018 and 2019 groups, respectively. After the application of the model, the rate of patients transferred to higher-level hospitals in the 2019 group in Hospital A was significantly lower than that in the 2018 group (2.6% vs 4.7%, P < 0.001).
Discussion
In this study, we investigated the effect of a three-level remote alliance model for critical care medicine that guides grassroots areas via in-place and online frameworks. The main findings were as follow: 1) the mortality of ICU patients in the county and city-level tertiary hospitals decreased significantly after the implementation of the model; 2) there was a significant reduction of ICU indicators including the incidence of ventilator-associated pneumonia and deep vein thrombosis; 3) the completion rates of 3-hour and 6-hour bundle therapies for septic shock was improved; 4) The hospital transfer rate decreased significantly in the grassroots and impoverished areas. In the future, this model is expected to improve the quality of critical care in remote areas and promoting the skill development of medical staffs.
Our findings are consistent with Kalb et al13,14 This is mainly related to in-place and online complementary support operation modes. Online training systematically improves the theoretical level, and in-place guidance makes up for the lack of an image of online advice and demonstration. The 24-hour online and 15-minute remote response has guaranteed the homogeneity of current diagnosis and treatment technologies. The normalised distance teaching has made up for the difficulties of continuing education for medical staff in the border area and the slow improvement of their technical level. Information sharing and remote external communication have expanded the academic vision of grassroots doctors and overcome the shortcomings of grassroots doctors with little knowledge of cutting-edge information. These results ensure the continuous improvement of current and future medical quality at the grassroots level.
The long-term and orderly operation of the alliance has several advantages. First, it achieves the convergence and shunting of patients and is a win–win situation for all parties. Through online ward rounds, patients with complex, challenging and rare diseases will be transferred to tertiary hospitals, achieving accurate hierarchical diagnosis and treatment. It can not only alleviate the problem of the shortage of beds in tertiary hospitals but also make full use of the abundant bed resources of primary hospitals to provide convenience for people.15 Second, the alliance has transcended time and space constraints and enabled superior resources to be used more efficiently,16 which is conducive to the rapid improvement of medical levels in the grassroots, border and poor areas. Ordinary people can enjoy high-level and homogeneous medical services without leaving the county, which alleviates the difficulty and cost of seeing a doctor and improves people’s ability to obtain medical treatment.17 Third, it overcomes the difficulty of the shortage of human resources and improves efficiency. A high-level department can guide multiple hospitals with only a tiny number of human resources and is further enlarged by the second-level hospitals in the alliance. Fourth, the alliance guidance is more professional. Compared with the incumbent support of a single medical staff, the alliance is one department corresponding to another department. Its sub-specialty coverage is more comprehensive, and the guidance is more professional. Fifth, the alliance enables the rapid improvement of the medical quality of ICUs in hospitals at all levels and eliminates the concern of patients being siphoned away. Hospitals and departments are willing to participate actively. Sixth, the alliance provides opportunities and resources for physicians to learn and improve, meet their needs7 and enables physicians to participate actively.18
The lack of sharing and integration of medical resources is the main obstacle hindering the progress of medical and health care.19 The alliance is highly dependent on the internet and information sharing, and trouble-free communication and data transmission play a decisive role in “online” work. It is necessary for the smooth development and the important content of alliance cooperation.20–22 Therefore, alliance cooperation should strengthen the informatisation framework within the alliance, break down information barriers and realise the interconnection and interoperability of medical resources, information and services to improve operational efficiency.23 At the same time, attention should be paid to information security and patient privacy protection.24
There were some limitations in this study. First, this was a study involving several centers in specific areas with a relatively small sample size. The results may be vulnerable to potential selection bias. Second, the ICU of Hospital A was newly established, and there was no data about before the alliance and the disease spectrum of Hospital A. This study was carried out under a close medical alliance and a support obligation relationship among these hospitals. Therefore, the generalizability of findings may be limited and subsequent studies are needed to validate the effectiveness of the model. Currently, the medical insurance of each medical unit in China’s medical consortium implements a unique payment method, which cannot reflect a win–win benefit distribution mechanism. Previous studies have shown that the remote alliance needs to formulate unified charging standards, medical insurance distribution mechanisms and supervision mechanisms, clarify responsibilities and rights and form a closer and more effective interest alliance to ensure the healthy and sustainable development of the alliance,25–28 which is also one of the future perspectives on this issue.
In conclusion, this three-level remote alliance model might be helpful in improving medical quality of critical care and promoting the homogeneous development of ICUs in grassroots, poor, and remote areas despite various challenges including unbalanced medical resources and space constraints.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Mianzhu People’s Hospital. Written informed consent was obtained from all participants/local guardians.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study is funded by Scientific Research Project of Sichuan Provincial Health Commission (No. 20PJ253) and Scientific research project of Deyang Science and Technology Bureau (No. 2020SZZ080). Funding agencies did not play a role in study design, data collection, analysis and interpretation, and manuscript writing.
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately.
References
1. Bigbee J. The uniqueness of rural nursing. Nurs Clin North Am. 1993;28(1):131–144. doi:10.1016/S0029-6465(22)02843-2
2. Seright T, Winters C. Critical care in the critical access hospital. Crit Care Nurs. 2015;35(5):62–67. doi:10.4037/ccn2015115
3. Lu ZH, Meng QY, Wang Y. Equity in basic health resources allocation before and after health reform in China. Chin J Public Health. 2017;33(08):1203–1205.
4. General Office of the State Council. Guiding opinions of the general office of the state council on promoting the construction and development of medical complexes. State Office. 2017;32:2017.
5. An YF. Characters and improvement strategies of distribution of high-quality medical resources. China Health Qual Manage. 2011;18(5):110–113.
6. World Health Organization. The World Health Report 2000: Health Systems; Improving Performance. Switzerland; 2000.
7. The Propaganda Department of the Central Committee of the Communist Party of China. The Outline of Xi Jinping Thought on Socialism with Chinese Characteristics for a New Era. Beijing: Learning Publishing House: People’s Publishing House; 2019:12–20.
8. Xia LG, Liu TT, Liu H, et al. Problem and countermeasure of regional health synergetic development based on “Teng-Shan medical NACF”. Soft Sci Health. 2016;30(06):22–27.
9. Wu K, Zheng Y, Wan Y, Yang SC, Yang Z. Current situation and effect evaluation of medical staff’s demand and utilization of medical alliance services in Sichuan Province. Chin J Public Health. 2020;36(10):1406–1408.
10. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. doi:10.1097/00003246-198510000-00009
11. Association CCMBoCM. Guidelines for the prevention, diagnosis, and treatment of ventilator-associated pneumonia (2013). Chin J Intern Med. 2013;52(6):524–543.
12. Zinellu A, Zinellu E, Mangoni AA, et al. Clinical significance of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in acute exacerbations of COPD: present and future. Eur Respir Rev. 2022;31(166):220095. doi:10.1183/16000617.0095-2022
13. Kalb TH. Increasing quality through telemedicine in the intensive care unit. Crit Care Clin. 2015;31(2):257–273. doi:10.1016/j.ccc.2014.12.005
14. Kalb T, Raikhelkar J, Meyer S, et al. A multicenter population-based effectiveness study of teleintensive care unit-directed ventilator rounds demonstrating improved adherence to a protective lung strategy, decreased ventilator duration, and decreased intensive care unit mortality. J Crit Care. 2014;29(4):691.e7–14. doi:10.1016/j.jcrc.2014.02.017
15. Mattick K, Barnes R, Dieppe P. Medical education: a particularly complex intervention to research. Adv Health Sci Educ Theory Pract. 2013;18(4):769–778. doi:10.1007/s10459-012-9415-7
16. Guo JJ, Bao YT, Jing M. Building of multipath remote consultation platform based on medical alliance. J Med Inf. 2018;39(01):22–25.
17. Wang JY. “Four stops” rehabilitation service mode based on the medical union. Chin Gen Prac. 2018;21(5):555–558.
18. Li YN, Wu HB. A comparative study of Chinese and American medical alliances. Med Higher Vocat Educ Mod Nurs. 2017;34(4):152–156.
19. Xu JD. The mode of medical association and the trend of future development. China Health Stand Manage. 2019;10(2):29–32.
20. Shi YX, Jiao Y. Research on and discussion about informatization construction strategy of medical alliance. China Digital Med. 2016;11(7):5–7.
21. Huang QH, Hu M. Model analysis of medical alliance construction and reference to international experience. China Hosp. 2015;19(10):56–59.
22. Koncz V, Kohlmann T, Bielmeier S, Urban B, Prückner S. Telenotarzt: Neues Versorgungskonzept in der Notfallmedizin [Tele-emergency physician: new care concept in emergency medicine]. Unfallchirurg. 2019;122(9):683–689. German. doi:10.1007/s00113-019-0679-8
23. Zheng XY. Information technology boosts the medical alliance to innovate the medical service model. e-Healthcare. 2014;7(1):46,50.
24. Hua HH, Wei S, Wu D, Li ZG, Wei C. PEST analysis of the development of online medicine in China and its countermeasures. Chin Health Serv Manage. 2020;37(11):801–803, 807.
25. Sheng MF, Xia CB, Zhu CE, Song BX. Difficulties and countermeasures encountered in the construction of medical union in Jiangsu. Jiangsu Health Syst Manage. 2018;29(7):745–747.
26. Luo YF, Yang GL. Practice and thinking on building the regional medical commonwealth of a hospital in Wuhan City. Med Soc. 2015;28(6):74–76.
27. Qian DF, Wang ZL, Lin ZP, Hu Y, Chen JY. Review and prospect of research on the integration of urban medical service system. Med Philos. 2011;32(2):43–45.
28. Rogove H, Stetina K. Practice challenges of intensive care unit telemedicine. Crit Care Clin. 2015;31(2):319–334. doi:10.1016/j.ccc.2014.12.009
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
