Back to Journals » Nature and Science of Sleep » Volume 14
The Effect of a Gluten-Free Diet on Sleep Disturbances in Children with Celiac Disease
Authors Suzer Gamli I , Keceli Basaran M
Received 19 December 2021
Accepted for publication 3 March 2022
Published 16 March 2022 Volume 2022:14 Pages 449—456
DOI https://doi.org/10.2147/NSS.S354811
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ahmed BaHammam
Ipek Suzer Gamli,1 Meryem Keceli Basaran2
1Istanbul Erenkoy Mental and Neurological Diseases Training and Research Hospital Child and Adolescent Psychiatry Unit, Istanbul, Turkey; 2Basaksehir Cam and Sakura State Hospital, Department of Pediatrics, Division of Pediatric Gastroenterology, Istanbul, Turkey
Correspondence: Ipek Suzer Gamli, Istanbul Erenkoy Mental and Neurological Diseases Training and Research Hospital Child and Adolescent Psychiatry Unit, Istanbul, Turkey, Fax +90 2163560496, Email [email protected]
Purpose: Sleep disturbances are common in patients with celiac disease (CD), but their response to a gluten-free diet (GFD) treatment remains scarce. This study investigated the alteration in sleep disturbances within 6 months of starting a GFD in children with CD.
Patients and Methods: A total of 103 children initially diagnosed with CD, with no psychiatric diagnosis and not receiving psychotropic medication, were included in this study. Sociodemographic data were collected, and the Children’s Sleep Habits Questionnaire (CSHQ) was completed both before and after six months of initiating a GFD.
Results: Overall, the total average CSHQ score was 46; after starting the GFD, this decreased to 40, which was under the clinically significant cutoff level for sleep disturbance (p < 0.001). A total of 74 patients (71.8%) had a CSHQ score above the clinically significant cutoff before treatment, which decreased to 40 patients (38.8%) six months after GFD (p < 0.001). A significant improvement was detected in all CSHQ subscale scores and in the total CSHQ score after starting the GFD (p < 0.001). Parasomnia and the total CSHQ score were higher in children who were diagnosed incidentally compared to symptomatic children but did not differ after GFD (p < 0.005). In 39 patients (37.8%), the total CSHQ score remained high 6 months after starting the GFD. Maternal and paternal ages were significantly higher in children whose scores remained high (p < 0.05).
Conclusion: A significant improvement in sleep scores was detected after starting a GFD, regardless of initial age, sex, and symptom status. With a GFD, children may fall asleep more easily and sleep for longer with less interruptions. GFD may help to reduce sleep disturbances in CD, but future studies should investigate the certain conditions in patients who do not respond to a GFD.
Keywords: disorder, enteropathy, pediatric, screening, sleep
Introduction
Sleep plays a significant role in the physical and mental well-being of children.1 However, sleep related problems are common in childhood; in particular, the disturbance rate is higher in children and adolescents with chronic medical conditions and atopic diseases.2,3 Chronic conditions such as asthma, cystic fibrosis, sickle cell disease, gastroesophageal reflux, neuromuscular diseases, and chromosomal disorders have been associated with a poorer sleep quality.4
Celiac disease (CD) is a life-long, chronic disease that affects about 1% of the population. CD is an autoimmune disorder characterized by protein intolerance to gluten, which is common in wheat, rye, and barley. Gastrointestinal (GI) symptoms and extraintestinal/systemic findings are common with gluten consumption.5 Some children with CD may be asymptomatic or have only extraintestinal symptoms at baseline.6 A gluten-free diet (GFD) is the only treatment shown to have a positive effect on both symptoms and quality of life in children with CD.7
Childhood CD is associated with a greater (1.4-fold) risk of behavioral problems, psychiatric disorders, and neurologic conditions compared with the general population.6,8,9 Sleep problems are also common in CD.10 Zingone et al have reported that sleep disorders should be checked in untreated patients with CD.11 However, the mechanism underlying the association between CD and sleep disorders has not yet been clarified.
One explanation for the psychological symptoms of CD is insufficient iron and vitamin levels due to malabsorption of nutrients, which may lead to neurotransmitter deficiencies and immunological dysregulation.12,13 Frequent atopic conditions and increased levels of proinflammatory cytokines in children with CD may also influence their sleep.14,15 Presence of anti-neuronal antibodies, combined with antigliadin and tissue transglutaminase (tTG) antibodies, may contribute to neurologic manifestations via apoptosis in CD.16
Gluten-sensitive enteropathy has been linked to sleep and neurological problems in patients with CD,8,16 and so the effect of GFD on sleep disturbances is of particular interest. One study reported that anti-ganglioside antibodies and neurological symptoms disappeared in approximately half of patients following GFD.6 Sleep disturbances are less studied in CD compared to other GI disorders, and most previous research has been conducted in the adult population. Nevertheless, data have been contradictory; one study found no effect of a GFD on insomnia in patients with CD compared to individuals without CD.17 Zingone et al reported that in patients with CD, while sleep and sleep-related problems decrease with GFD, they remain more prevalent than in people without CD.11 Therefore, it is evident that more research is needed in this area, particularly in children and adolescents with CD. To this aim, the present study screened sleep disturbances in children and adolescents with untreated CD and determined, through parental reports, if there was a difference in sleep scores after 6 months of GFD.
Materials and Methods
Participants
A total of 103 children aged between 7 and 18 years who had been referred to the Pediatric Gastroenterology Clinic at the Basaksehir Cam and Sakura State Hospital were included in this prospective follow-up study. The inclusion criteria were as follows: (1) children had been diagnosed with CD, (2) were treatment-naïve, (3) did not have any psychiatric diagnoses, (4) were not using any psychotropic medication, (5) were eligible for 6 months of a strict GFD following their diagnosis, and (6) volunteered to participate in the study. Ethical approval for the study was provided by the Non-Invasive Clinical Research Committee at Gaziosmanpasa Education and Research Hospital (30.12.2020; reference number: 202). The study was conducted in accordance with the Declaration of Helsinki’s Ethical Principles. The study was performed in Basaksehir Cam and Sakura State Hospital; however, the hospital did not have any ethical review board at the time of application. Therefore, due to the rules of provincial health department, the nearest hospital with an ethical board was chosen for application. Written informed consent was obtained from the parents and children who agreed to participate in the study.
Diagnosis and Follow-Up of Celiac Disease
In our study, diagnosis of CD was based on IgA and IgG (tTG-IgA and IgG) antibodies and duodenal biopsy results. Upper GI endoscopy was performed in children with tTG-IgA and IgG antibody levels that were 10 times higher than normal levels. tTG-IgA testing was performed in all patients to rule out selective IgA deficiency. A definite CD diagnosis was made by evaluating biopsy samples from the duodenum and bulbus using the Marsh classification.18,19 The serum level of these autoantibodies was scrutinized to monitor compliance with GFD therapy. Thus, compliance with the GFD and the dietary inconveniences of the patient were verified. Moreover, children’s family members with subclinical CD were identified via family screening. Patients and families were informed about CD during the initial diagnosis and routine controls. Furthermore, a written document describing CD and its symptoms, the recommended diet, and treatment process was provided to the families and children. Laboratory tests were carried out to identify systemic diseases that might affect sleep quality and cause sleep disturbances. Parents of children with CD were called 6 months after diagnosis. Dietary compliance and clinical findings were checked during the control. Serum tests at the time of initial diagnosis were re-analyzed in terms of CD dietary compliance and accompanying diseases (such as micronutrient deficiency and anemia).
Measures
Initially, a sociodemographic questionnaire was provided to collect data on the patient’s age, birth history, developmental stages, medical history, parental education, employment status, and family characteristics. Second, the CD compliance questionnaire, developed by the authors, was completed by physicians through responses from parents. With this questionnaire, we collected data on the timing between the start of the symptoms and the diagnosis, and whether the diagnosis was made upon screening (incidentally) or with a symptom. The Turkish version of Children’s Sleep Habits Questionnaire (CSHQ)-Abbreviated Form was completed by parents both before and 6 months after commencement of the GFD.
Children’s Sleep Habits Questionnaire
The abbreviated CSHQ was developed by Owens et al, and assesses sleep habits and disturbances in school-aged children through parental reports.20 It consists of 33 items that are rated on a three-point Likert scale, whereby parents rate behaviors as occurring “rarely” = 0–1 night per week, “sometimes” = 2–4 nights per week, and “usually” = 5–7 nights per week; these ratings were scored as 1, 2, and 3 on the Likert scale, respectively. The 32nd and 33rd questions were rated differently, as “not sleepy” = 0–1 night per week, “very sleepy” = 2–4 nights per week, and “falls asleep” = 5–7 nights per week. In addition, there were three more open-ended questions regarding bedtime, amount of sleep, and waking-up time. Items 1, 2, 3, 10, 11, and 26 were coded and calculated inversely. CSHQ items were grouped into the following eight subscales: bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night waking, parasomnias, daytime sleepiness, and sleep-disordered breathing. A total score of 41 is the cutoff for sleep disturbances.20 Fis et al tested the validity and reliability of the Turkish version and reported that CSQH is a valid and reliable tool for assessing sleep problems in Turkish children.21
Statistical Analyses
The Statistical Package for the Social Sciences (SPSS), version 20.00, was used for statistical analyses (SPSS Inc.; Chicago, IL, USA). The assumption of normality for quantitative variables was checked using the Kolmogorov–Smirnov test. Spearman correlation analysis was used to examine the relationship between quantitative variables. Independent groups were compared using the Mann–Whitney U and Chi square tests. Dependent measurements were compared using the Wilcoxon Signed-Rank test. Dependent qualitative variables were compared using the McNemar test. Descriptive statistics are presented as the mean ± standard deviation for quantitative variables, and as the median and 25th to 75th percentile or frequency, n (%) for ordinal data. In all analyses, a p-value < 0.05 was accepted as the level of statistical significance.
Results
The study comprised 103 patients, including 67 (65%) girls and 36 (35%) boys. Initially, 154 children were screened. However, 51 children were excluded from the study because of the presence of a psychiatric condition, psychotropic medication use, or non-adherence to the diet. The mean age of the participants was 11.36±3.42 years. The mean age of the mothers was 39.89±5.77 years, and the mean age of the fathers was 44.06±6.41 years. The questionnaires were completed by mothers; 96 patients (93.2%) came to follow-up and controls together with their mothers. Birth weight, breastfeeding time, and developmental stages were within the normal range for all participants. Parameters such as sex, number of siblings, parental age, educational status, monthly income, birth weight, and breastfeeding duration had no significant influence on CSHQ sleep scores (p > 0.05). No significant difference was found between the sleep scores of children who had their own room and those who shared room with two or more siblings (p = 0.068). Furthermore, there was no difference in sleep scores according to the order of the children within the family (p = 0.075).
Of all participants, 53 (51.5%) had growth retardation, 20 (19.4%) had anemia, and 41 (39.8%) had GI symptoms when they were referred to a pediatric gastroenterology clinic; 14 (13.6%) patients were diagnosed incidentally. GIS findings were detected in 16 patients after GFD (5 patients had nausea, 4 had bloating, 3 had vomiting, and 4 patients had abdominal pain). There was no difference in the sleep score between the patients with and without GIS findings (p = 0.938). The tTG antibody level of 41 patients (39.8%) returned to a normal range after 6 months of GFD. Patients with normal tTG antibody levels and patients with high tTG antibody levels were found to be similar in terms of their sleep score (p = 0.088). There was a significant positive correlation between the Marsh stage and tTG antibody level (p < 0.001). Thirty-three patients were Marsh stage 3a, 33 were Marsh stage 3b, and 37 were Marsh stage 3c. Of the patients with symptomatic CD, 28 were Marsh stage 3a, 29 patients were Marsh stage 3b, and 32 patients were Marsh stage 3c. Marsh stage, tTG antibody level, and the total sleep score of asymptomatic and symptomatic patients were similar, with no significant difference between the two subgroups (p > 0.05). Table 1 presents a comparison of CSHQ scores in all patients with CD before and after 6 months of GFD.
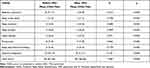 |
Table 1 Descriptive Data and Comparison Results of CSHQ Scores of All Patients with CD (n = 103) Before and After Initiating a GFD |
In 35 patients (34%), the total scores fell below the cutoff score for sleep disturbance after treatment. In these patients, the median scores (25th–75th percentile) before and after treatment were 44 (46.5–55.5) and 38 (35–40), respectively. However, in 39 patients (37.8%) the total scores remained high despite the GFD. For the remaining patients, the scores were below the clinical cutoff both before and after the treatment, except for 1 patient (1%) who exceeded the cutoff score after treatment but not before (ie 40 vs 45). These two patient groups were compared in terms of descriptive patterns. The maternal median age was 38 (34–45) years in the recovering group, whereas it was 43 (39–45) years in the treatment-resistant group (p = 0.009). The paternal median age was 41 (38–49) and 46 (43–49) years in the recovering group and in the treatment-resistant group, respectively, at the time of the diagnosis (p = 0.004). There was no significant difference in other family characteristics (p > 0.005) with regard to sociodemographic data. Table 2 shows a comparison of CSHQ scores in symptomatic and asymptomatic children at the initial diagnosis. Class frequency distributions are shown according to the cutoff value after GFD, as defined by Owens et al (as shown in Table 3).20
 |
Table 2 Comparison of Sleep Scores in Patients with CD According to Diagnosis Status |
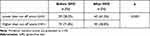 |
Table 3 Frequency Distribution of Total Sleep Score Groups Calculated Before and After GFD |
Discussion
Sleep is fundamental for physical and mental health in children. Good sleep habits are associated with adequate cognitive performance, higher educational achievement, stronger emotional regulation, and higher quality of life.22,23 Inversely, shorter sleep durations have been associated with negative physical and mental health outcomes. Since sleep problems are associated with a wide range of adversities in many domains, their negative impact may be more severe in children with chronic medical conditions. The consensus is that sleep problems may worsen symptoms and complicate treatment in people with chronic illnesses.24 Early recognition of these problems may avoid adverse outcomes and ameliorate the course of the medical condition.25
As a chronic medical condition, CD has been associated with various psychological and behavioral symptoms, including sleep problems.10 Ballou et al reported that 61% of patients with CD had deficiencies in sleep habits, and this rate is listed among the worst in patients with GI diseases.26 As in our study, the mean total sleep score and the number of patients above the clinical cutoff for sleep disturbances indicate that sleep problems may be common in children with untreated CD. Patients who suffer from GI symptoms such as bloating, gas, abdominal pain, nausea, or vomiting, especially after gluten consumption during dinner, may have difficulties in falling asleep at night. Based on our observations from the present study, children and their parents frequently complain of GI symptoms, especially after meals, which may disrupt sleep. Vitamin deficiency secondary to malabsorption may also trigger sleep disturbance in these patients.12,13 Furthermore, the association between CD and psychiatric disorders may also explain the higher rates of sleep problems. In the literature, increased anxiety and depressive and aggressive behaviors were detected in children with CD, which in turn have negative impacts on sleep.10 However, the exclusion of patients with a psychiatric disorder makes this less likely as an explanation for the present results.
To the best of our knowledge, there are limited data on whether sleep disturbances in children with CD improve with a GFD. In our study, the significant reductions in the subscale scores, total score, and the average score indicate that there is an association between gluten consumption and sleep problems that can be improved through a GFD. Our observations during the study suggest that children get to bed more comfortably and fall asleep less painstakingly after treatment. These improvements might be associated with less night-time waking; longer sleep duration; and less sleep interruption due to pain, bloating, or the need to vomit after treatment. An increase in the quality of night-time sleep may indicate less daytime drowsiness.
The relationship or the lack thereof between GI symptom severity and the level of sleep disturbances is an area of interest. GI symptom severity and insomnia, poor sleep quality, and use of sleep medications have been found to be significantly associated.27 In our study, although symptom severity was not measured, no discrepancy was found between pre- and post GFD sleep scores in children with GI symptoms. Patients with CD were divided into two groups according to the way they had been diagnosed. Patients who were diagnosed with CD incidentally and those who were referred to gastroenterology clinics for further investigation due to growth retardation, anemia, or GI symptoms were shown to have different sleep characteristics, as measured by CSHQ scores. During treatment, the gap in scores tended to close, with no significant differences after the GFD. Although the sample size was relatively small, this may suggest that symptomatic children benefited more from GFD. In turn, this strengthens the possibility that there is an association between gluten consumption and sleep disturbances in these children.
When patients were grouped based on their response to GFD, they were classified as the recovered group, whose scores fell below the cutoff score, and the resistant group, whose scores remained high despite treatment. In the resistant group, maternal and paternal ages at the time of initial diagnosis were significantly higher than those in the recovered group. These have not been stated as risk factors in CD by previous literature. Therefore, parental age may be questioned, especially in cases with persistent sleep problems.
According to the literature, nearly half of patients with chronic illness experience sleep disturbances.4 In our study, the sleep scores of more than 1/3 of the patients remained high after 6 months of GFD. The aforementioned rate is nonetheless thought to be high compared to typically developing children.4 According to the present results, there are still plenty of children with CD who continue to experience sleep disturbances after GFD, although this diet can help to reduce sleep problems in many. Therefore, GFD may be beneficial in decreasing symptoms, but may not be the only possible intervention for all patients with CD.
Conclusion
Sleep problems are high in untreated patients with CD. Our study shows that sleep scores are higher in patients with CD and tend to improve with implementation of a GFD, independent of GI symptoms. This suggests that there is a multifaceted relationship between CD and sleep problems. Therefore, in the presence of GFD-resistant sleep disturbances, patients should be referred to relevant units for further investigation.
This study has some limitations. Sleep and related disorders were screened using the CSHQ, which was completed by parents. Previous work has found that prevalence rates may vary according to who the information is obtained from.20 Furthermore, the lack of normalization of sleep hours by age and the absence of a non-CD control group are also important limitations. Moreover, whether or not an objective sleep test can be used to identify the disturbances may be considered as another limitation. Further research with a larger sample size is needed to clarify the relationship between CD and sleep disturbances, the effect of GFD on sleep, the characteristics of resistant patients, and how to manage CD in the presence of sleep disorder.
Abbreviations
CD, Celiac disease; CSHQ, Children’s Sleep Habits Questionnaire; GFD, Gluten-free Diet; GI, Gastrointestinal; GIS, Gastrointestinal System; tTg, Tissue Transglutaminase.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, Ipek Suzer Gamli, upon reasonable request.
Ethics Approval
Ethical approval for the study was provided by the Non-Invasive Clinical Research Committee at Gaziosmanpasa Education and Research Hospital (30.12.2020; reference number: 202).
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received to support the research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786. doi:10.5664/jcsm.5866
2. Koinis-Mitchell D, Craig T, Esteban CA, Klein RB. Sleep and allergic disease: a summary of the literature and future directions for research. J Allergy Clin Immunol. 2012;130(6):1275–1281. doi:10.1016/j.jaci.2012.06.026
3. Owens J. Classification and epidemiology of childhood sleep disorders. Prim Care. 2008;35(3):533–546, vii. doi:10.1016/j.pop.2008.06.003
4. Bandla H, Splaingard M. Sleep problems in children with common medical disorders. Pediatr Clin North Am. 2004;51(1):203–227. doi:10.1016/S0031-3955(03)00185-8
5. Rostom A, Murray JA, Kagnoff MF. American Gastroenterological Association (AGA) Institute technical review on the diagnosis and management of celiac disease. Gastroenterology. 2006;131(6):1981–2002. doi:10.1053/j.gastro.2006.10.004
6. Volta U, De Giorgio R, Granito A, et al. Anti-ganglioside antibodies in coeliac disease with neurological disorders. Dig Liver Dis. 2006;38(3):183–187. doi:10.1016/j.dld.2005.11.013
7. Caio G, Volta U, Sapone A, et al. Celiac disease: a comprehensive current review. BMC Med. 2019;17(1):142. doi:10.1186/s12916-019-1380-z
8. Potocki P, Hozyasz K. Psychiatric symptoms and coeliac disease. Psychiatr Pol. 2002;36(4):567–578.
9. Butwicka A, Lichtenstein P, Frisén L, Almqvist C, Larsson H, Ludvigsson JF. Celiac disease is associated with childhood psychiatric disorders: a population-based study. J Pediatr. 2017;184:87–93. doi:10.1016/j.jpeds.2017.01.043
10. Smith LB, Lynch KF, Kurppa K, et al. Psychological manifestations of celiac disease autoimmunity in young children. Pediatrics. 2017;139(3):e20162848. doi:10.1542/peds.2016-2848
11. Zingone F, Siniscalchi M, Capone P, et al. The quality of sleep in patients with coeliac disease. Aliment Pharmacol Ther. 2010;32(8):1031–1036. doi:10.1111/j.1365-2036.2010.04432.x
12. Halfdanarson TR, Litzow MR, Murray JA. Hematologic manifestations of celiac disease. Blood. 2007;109(2):412–421. doi:10.1182/blood-2006-07-031104
13. Ji X, Grandner MA, Liu J. The relationship between micronutrient status and sleep patterns: a systematic review. Public Health Nutr. 2017;20(4):687–701. doi:10.1017/S1368980016002603
14. Khanijow V, Prakash P, Emsellem HA, Borum ML, Doman DB. Sleep dysfunction and gastrointestinal diseases. Gastroenterol Hepatol (N Y). 2015;11(12):817–825.
15. Zauli D, Grassi A, Granito A, et al. Prevalence of silent coeliac disease in atopics. Dig Liver Dis. 2000;32(9):775–779. doi:10.1016/S1590-8658(00)80354-0
16. Cervio E, Volta U, Verri M, et al. Sera of patients with celiac disease and neurologic disorders evoke a mitochondrial-dependent apoptosis in vitro. Gastroenterology. 2007;133(1):195–206. doi:10.1053/j.gastro.2007.04.070
17. Zylberberg HM, Demmer RT, Murray JA, Green PHR, Lebwohl B. Depression and insomnia among individuals with celiac disease or on a gluten-free diet in the USA: results from a national survey. Eur J Gastroenterol Hepatol. 2017;29(9):1091–1096. doi:10.1097/MEG.0000000000000932
18. Marsh MN. Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity (‘celiac sprue’). Gastroenterology. 1992;102(1):330–354. doi:10.1016/0016-5085(92)91819-P
19. Husby S, Koletzko S, Korponay-Szabó IR, et al. European society for pediatric gastroenterology, hepatology, and nutrition guidelines for the diagnosis of coeliac disease [published correction appears in J Pediatr Gastroenterol Nutr. 2012;54(4):572]. J Pediatr Gastroenterol Nutr. 2012;54(1):136–160. doi:10.1097/MPG.0b013e31821a23d0
20. Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21(1):27–36. doi:10.1097/00004703-200002000-00005
21. Fis NP, Arman A, Ay P, et al. Turkish validity and reliability of child sleep habits questionnaire. Anat J Psychiatry. 2010;11:151–160.
22. Matricciani L, Paquet C, Galland B, Short M, Olds T. Children’s sleep and health: a meta-review. Sleep Med Rev. 2019;46:136–150. doi:10.1016/j.smrv.2019.04.011
23. Chaput JP, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S266–282. doi:10.1139/apnm-2015-0627
24. Baiardini I, Braido F, Cauglia S, Canonica GW. Sleep disturbances in allergic diseases. Allergy. 2006;61(11):1259–1267. doi:10.1111/j.1398-9995.2006.01221.x
25. Carter KA, Hathaway NE, Lettieri CF. Common sleep disorders in children. Am Fam Physician. 2014;89(5):368–377.
26. Ballou S, Alhassan E, Hon E, et al. Sleep disturbances are commonly reported among patients presenting to a gastroenterology clinic. Dig Dis Sci. 2018;63(11):2983–2991. doi:10.1007/s10620-018-5237-7
27. Honaker SM, Meltzer LJ. Sleep in pediatric primary care: a review of the literature. Sleep Med Rev. 2016;25:31–39. doi:10.1016/j.smrv.2015.01.004
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
