Back to Journals » Risk Management and Healthcare Policy » Volume 13
The Effect and Mechanism of Adverse Childhood Experience on Suicide Ideation in Young Cancer Patients During Coronavirus Disease 2019 (COVID-19) Pandemic
Authors Yang G, Xiao C, Li S, Yang N
Received 18 June 2020
Accepted for publication 8 August 2020
Published 24 August 2020 Volume 2020:13 Pages 1293—1300
DOI https://doi.org/10.2147/RMHP.S266269
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Guoqing Yang1 ,* Chenchang Xiao2 ,* Shiyue Li,3 Ningxi Yang1
1College of Humanities and Social Sciences, Harbin Engineering University, Harbin, People’s Republic of China; 2City College, Wuhan University of Science and Technology, Wuhan, People’s Republic of China; 3School of Health Sciences, Wuhan University, Wuhan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ningxi Yang College of Humanities and Social Sciences
Harbin Engineering University, NO. 145 Nantong Road, Harbin, Heilongjiang, People’s Republic of China
Tel +86 45182569608
Email [email protected]
Background and Aim: Coronavirus disease 2019 (COVID-19) is currently prevalent worldwide. This research aimed to explore the effect of adverse childhood experience (ACE) on suicide ideation in young cancer patients during the COVID-19 pandemic. Self-reported questionnaires analyzed the mediating effects of sleep quality, anxiety symptoms, and inflammatory conditions between ACE and suicide ideation.
Materials and Methods: A total of 197 young cancer patients (age 18– 40) completed questionnaires and a blood test. Correlation analysis and structural equation model were used to explore the relationships between ACE, sleep quality, anxiety symptom, serum C-reactive protein (CRP) levels and suicide ideation. The mediating roles of sleep quality, anxiety symptoms, and CRP levels on the influence of ACE on suicide ideation were explored.
Results: ACE was positively related to anxiety symptoms, CRP levels, and suicide ideation, and negatively related to sleep quality. Anxiety symptoms and CRP levels were positively related to suicide ideation, while sleep quality was negatively related to suicide ideation. Anxiety symptoms were positively related to CRP levels but negatively related to sleep quality. From these results, we found ACE affected suicide ideation directly and was mediated by roles sleep quality, anxiety symptom and CRP.
Conclusion: ACE not only directly affected suicide ideation but also affected suicide ideation through sleep quality, anxiety symptoms, and inflammatory conditions in young cancer patients during the COVID-19 pandemic. Therefore, targeted intervention and help for cancer patients from the perspective of ACE should be put into practice.
Keywords: coronavirus disease 2019, psychosocial oncology, adverse childhood experience, anxiety symptom, sleep quality, suicide ideation
Introduction
Adverse childhood experience (ACE) refers to the psychological or physical harm and threats suffered by individuals before the age of 18. These encounters are known to bring adverse effects on the overall health and survival of victims.1 ACEs mainly include emotional neglect, emotional abuse, physical neglect, physical abuse, sexual abuse, and family dysfunction (ie separation or divorce of parents, family drug users, mental disorders in the immediate family, family members who committed suicide, and family members with criminal records).2 Previous research has demonstrated that as a chronic stress, ACE affected victims’ physical and mental health. For example, ACE is more likely to cause future mental illnesses, such as depression, schizophrenia, and attention deficit hyperactivity disorders (ADHD), and negative emotions, such as depression and anxiety.3,4 In addition, studies have shown that ACEs are associated with physical inflammation and other physical health conditions.5
Currently, coronavirus disease 2019 (COVID-19) is prevalent worldwide. Although several drugs on immune system may protect against COVID-19, the epidemic situation is remains a major public health problem, threatening people’s health.6 As of June 4th, 2020, more than 6.5 million people have been infected worldwide, and more than 380,000 people have died due to COVID-19.7 Not only does this disease have a huge impact on physical health, such as causing problems to people with chronic diseases,8 it also causes a series of mental health problems, such as depression, anxiety, and panic attacks.9 Similarly, young cancer patients experience more stress from COVID-19 compared to the average adults and elder patients because their life expectancy, lifestyle, even marriage may be affected by cancer; therefore, some young patients may have suicidal thoughts.10 In addition, some cancer patients may have Alexithymia, which can increase their suicidal thoughts.11,12
With the current prevalence of infectious diseases, the lifestyle and medical behaviors of young cancer patients have been changed. Therefore, they may face more physical and mental challenges, which require more attention from medical staff. In the context of the COVID-19 pandemic, the psychological problems caused by ACEs may be more serious. ACEs may also affect sleep and inflammation.13–15 In addition, anxiety, sleep problems, and inflammation may, in turn, affect suicidal ideation.16,17 Therefore, in this study, we focused on the mental and physical health of young cancer patients, analyzed the influence of ACEs on suicidal ideation, and verified whether anxiety, sleep, and inflammation played an intermediary role between ACE and suicidal ideation. We propose two hypotheses: 1) ACEs directly affect suicidal ideation; and 2) ACEs affect suicidal ideation through sleep, anxiety, and inflammation conditions.
Materials and Methods
Participants
From January to May 2020, 197 young cancer patients were recruited by online recruitment and snowball sampling. The inclusion criteria for this study were as follows: 1) diagnosed with cancer, had completed radical surgery; 2) were in the early stages of cancer, and the disease stage was I or II. Patients were in the rehabilitation stage, and were not currently completing chemotherapy, endocrine therapy and/or immunotherapy; 3), not currently suffering from any other infectious or autoimmune diseases or other diseases which may affect C-reactive protein (CRP) levels; 4) not diagnosed with mental illness, and do not take psychoactive drugs; and 5) were 18–40 years old and were aware of their diagnosis. All participants provided informed consent for their participation in this study. This study was conducted based on the principle of the Declaration of Helsinki. This study was approved by the Ethics Committee of the Wuhan University School of Medicine (20180928; Wuhan, China).
Study Design
This was an observational and cross-sectional study which contained self-assessment questionnaires (for demographic information, and information related to sleep, anxiety, and suicidal ideation) and blood biochemical examination (CRP levels).
Measures
Adverse Childhood Experience
The ACE questionnaire (ACE scale) which was first applied by the Kaiser Permanent and Centers for Disease Control of the USA was used to investigate the effect of various adverse events experienced by participants under the age of 18. Participants were asked to answer “Yes” or “No” to 10 prompts including: “Parents or other adults often or sometimes abuse and belittle you”, “Parents or other adults often or sometimes hit you or throw things at you”, and “Your parents are divorced or separated”. If the participant answered “Yes”, 1 point was scored, and if the answer was “No”, 0 points were scored. The total score ranged from 0 to 10 points.18 The Cronbach’s alpha for this survey was 0.739.
Anxiety Symptoms
The self-rating Anxiety Scale (SAS) was used to evaluate participants’ anxiety symptom. Participants answered the questions according to their mental state in the last week. The SAS is made up of a 4-points Likert Scale with 20 questions. Each item is scored from 1 to 4, with the total score ranging from 20 to 80. The total score is then multiplied by 1.25 to get the standard score, and a higher score indicated more anxiety symptoms.19 The Cronbach’s alpha for this survey was 0.813.
Sleep Quality
The Pittsburgh Sleep Quality Index (PSQI) questionnaire was administered to measure the participants’ sleep quality. The questionnaire contained 18 questions in 7 sections (sleep duration, sleep latency, sleep quality, habitual sleep efficiency, sleep disturbances, use of sleeping pills, and daytime dysfunction). The score of each section ranged from 0 to 3, with an aggregate score ranging from 0 to 21. The higher the aggregate score, the lower the participant’s sleep quality.20 The Cronbach’s alpha for this survey was 0.801.
Suicide Ideation
The Beck Suicide Ideation Scale (BSI) was used to measure the participants’ suicide ideation. This survey contained a 3-point Likert Scale (scored 0 to 2) for each of the 19 statements. The total survey score ranged from 0 to 38, with a higher score indicating more suicide ideation.21,22 The Cronbach’s alpha for this survey was 0.792.
C-Reactive Protein
CRP was tested to estimate participants’ inflammatory condition. Participants’ blood samples were collected on the day they completed the questionnaires. Blood samples were tested for CRP levels. The normal value of serum CRP level is 0–10.0mg/L.
Statistical Analysis
We used EpiData Entry version 3.1 and SPSS version 25.0 to enter and analyze the data. We presented all data by mean ± standard deviation (SD). Pearson correlation analysis and structural equation modeling (SEM) were used to analyze the relationships between variables. SPSS Amos version 21.0 was used to assess the variables’ mediation effects, and the bootstrap number was set to 5000. A nonparametric percentile bootstrap method with bias correction was used to determine the significance of specific mediations. We used path analysis through the SEM to test the relationships and their significance. A P-value <0.05 was considered statistically significant.
Results
Sample
For this study, a total of 240 patients were invited, and 197 agreed to participate (participation rate of 82.08%). Because this study was carried out during the epidemic period of infectious diseases, and blood was collected from hospitals, some patients were worried about being infected by COVID-19. As a result, some participants were not willing to participate in our study. The average age of participants was 36.5 years (89 male, 108 female). The average course of disease among participants was 2.6 years. A total of 53 patients had breast cancer, 32 patients had gynecological cancer (cervical or ovarian cancer), 56 patients had lung cancer, and 56 patients had gastrointestinal cancer (liver, stomach, colorectal, or esophagus cancer).
Correlations Among ACE (ACE Scale), Sleep Quality (PSQI), Anxiety Symptom (SAS), CRP, and Suicide Ideation (BSI)
Table 1 presents the correlations among scores of ACE, PSQI, SAS, CRP, and BSI questionnaires. The ACE score was positively and significantly related to PSQI (r=0.422, P < 0.01), SAS (r =0.386, P < 0.01), CRP (r = 0.475, P < 0.01), and BSI (r =0.509, P < 0.01). The PSQI (r =0.506, P < 0.01), SAS (r =0.578, P < 0.01), and CRP (r =0.512, P < 0.01) were positively and significantly related to BSI. Finally, SAS was positively and significantly related to PSQI (r=0.459, P<0.01) and CRP (r=0.523, P<0.01). Based on the scoring rules of each scale, these correlations indicated that ACE was positively related to anxiety symptoms, CRP levels, and suicide ideation, and was negatively related to sleep quality. In addition, anxiety symptoms and CRP levels were positively related to suicide ideation, while sleep quality was negatively related to suicide ideation. Finally, anxiety symptoms were positively related to CRP, while they were negatively related to sleep quality.
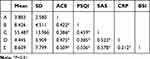 |
Table 1 Correlations Among ACE (ACE Scale), Sleep Quality (PSQI), Anxiety Symptom (SAS), CRP and Suicide Ideation (BSI) of Young Cancer Patients |
Path Analysis of the Influence of ACE (ACE Scale) on Suicide Ideation (BSI)
Using an SEM, a path analysis was completed so that the associations of ACE on BSI could be tested. The fit indices of this structural equation were ideal and demonstrated a high goodness-of-fit (GFI=0.996), a high comparative fit index (CFI=0.997), a high Tucker-Lewis index (TLI=0.971), a high incremental fit index (IFI=0.997), a high-normed fit index (NFI=0.994), a high adjusted goodness-of fit-index (AGFI=0.943), and a high root-mean-square error of approximation (RMSEA=0.067, χ2/df=1.892). The relationships among ACE, PSQI, SAS, CRP, and BSI resulting from the path analysis are presented in Figure 1.
 |
Figure 1 The path analysis model of relationships of score of ACE, PSQI, SAS, CRP and BSI of young cancer patients, with standardized β-weights. Note: e1–e4, residual error. |
The normalized path coefficient is presented in Table 2. The ACE scores significantly and positively affected the PSQI scores (β=0.288, P<0.001), SAS (β=0.386, P<0.001), CRP (β=0.322, P<0.001), and BSI (β=0.226, P<0.001). The SAS scores significantly and positively affected the PSQI scores (β=0.348, P<0.001), CRP (β=0.399, P<0.001) and BSI (β=0.313, P<0.001). The PSQI scores (β=0.205, P<0.001) and CRP (β=0.164, P=0.011) significantly and positively affected BSI scores. Based on the scoring rules of each scale, these results indicated that: ACE significantly and positively affected anxiety symptoms, CRP, and suicide ideation, but significantly affected sleep quality negatively. In addition, anxiety symptoms significantly affected CRP levels and suicide ideation positively but significantly and negatively affected sleep quality. Finally, sleep quality significantly and negatively affected suicide ideation, while CRP levels significantly and positively affected suicide ideation. These results demonstrated that ACE could directly affect suicide ideation, which indicated that Hypothesis 1 was reasonable.
 |
Table 2 The Normalized Path Coefficients of ACE (ACE Scale), Sleep Quality (PSQI), Anxiety Symptom (SAS), CRP and Suicide Ideation (BSI) of Young Cancer Patients |
Intermediary Effect of Sleep Quality (PSQI), Anxiety Symptom (SAS), CRP in the Influence of ACE (ACE Scale) on Suicide Ideation (BSI)
The results of Bootstrap indirect effects analysis are presented in Table 3. The following results were achieved when 0 was not included in the confidence interval. In the path of ACE-SAS-BSI, SAS had a significant mediating effect between ACE and BSI (β=0.121, P<0.001). In the path of ACE-PSQI-BSI, PSQI had a significant mediating effect between ACE and BSI (β=0.059, P=0.003). In the path of ACE-CRP-BSI, CRP had a significant mediating effect between ACE and BSI (β=0.053, P=0.011). In the path of ACE-SAS-PSQI-BSI, SAS and PSQI had a significant chain mediating effect between ACE and BSI (β=0.027, P=0.003). In the path of ACE-SAS-CRP-BSI, SAS and CRP had a significant chain mediating effect between ACE and BSI (β=0.025, P=0.011). These results indicated that Hypothesis 2 was reasonable.
 |
Table 3 Bootstrap Indirect Effects Results of ACE (ACE Scale), Sleep Quality (PSQI), Anxiety Symptom (SAS), CRP and Suicide Ideation (BSI) of Young Cancer Patients |
Discussion
This study demonstrated that young cancer patients demonstrated high levels of anxiety symptoms and suicide ideation, and low sleep quality, during the COVID-19 pandemic. Similar to previous studies, during this epidemic period of acute infectious disease, participants demonstrated poor mental health.23 As a new type of infectious disease, COVID-19 spreads quickly, and since we do not currently fully understand the therapeutic effect and prognosis of COVID-19, it is more likely to cause panic attacks and other negative emotions. Moreover, cancer patients are prone to negative emotions. Due to their diagnosis, cancer patients often pay more attention, and feel more sensitivity and uncertainty about their body and disease subjectively, and require regular and objective physical examination.24 Because the epidemic makes their routine medical activities more difficult, this could induce more negative emotions.
This study confirmed the effect of ACE on suicidal ideation. These results demonstrated that ACE not only directly affected suicidal ideation, but also affected it through sleep quality, anxiety symptoms, and CRP levels. The more ACE the participants experienced, the more serious suicide ideation they had. As a source of long-term chronic stress, the effect of ACE on physical and mental health has been confirmed by previous research.18,25 This may be because those who have experienced ACE may have formed cognitive deviations and negative thinking patterns, and experience more psychological distress, which last to adulthood.26 Since they are more sensitive to negative events, it is more likely these participants to have or increase suicidal ideation under the dual pressure of infectious disease epidemics while also having cancer.
ACE also affected suicidal ideation by acting on sleep quality, anxiety symptoms and CRP levels. Similar to previous studies, our results demonstrated that ACE affected anxiety symptoms and sleep quality.27,28 People with ACEs are prone to stress and insecurity, which in turn makes them prone to anxiety symptoms or sleep problems in the future.29 In addition, ACE affects brain development and cognition. ACE can induce brain structure changes, especially as it involves areas of the brain involved in emotional regulation and decision-making, such as decreasing the size of the gyrus frontalis inferior.30 This has a negative impact on emotional regulation, such as symptoms of anxiety and other negative emotions, which may cause sleep problems. ACE is considered a type of chronic stress, and the ensuing effects of chronic stress on inflammatory factors have been confirmed.31 Even in the face of similar environment, individuals who have had ACE, or a certain intensity of ACE exposure, have a more sensitive response to stress during their life. Under repeated stimulation (ie in chronic stress), the transcription of inflammatory genes will be enhanced.15
Sleep quality, anxiety symptoms, and CRP levels affect suicidal ideation. Previous studies have confirmed that sleep was associated with suicidal ideation.32 This is because poor sleep can lead to a state of trance and hopelessness, which may lead to suicidal thoughts.33 In addition, poor sleep can increase the risk of suicide through a variety of physiological mechanisms, including hypothalamic pituitary adrenal (HPA) axis dysfunction and 5-hydroxytryptamine (5-HT) dysfunction, among others.34 Our findings confirmed the results of previous studies showing that anxiety symptoms cause suicidal ideation.35 Individuals in a state of anxiety tend to think more negatively and may feel more negatively towards the meaning of life, and are prone to suicide.36 In addition, anxiety may cause changes to physiological indexes, such as sleep, which may also cause suicidal ideation.37
Inflammatory conditions, such as increased CRP levels may also affect suicidal ideation.38 Inflammatory factors affect the metabolism of the dopamine system, neurotransmitters, neuroendocrine function, and local brain activity, which may make people feel dejected or down.39 In turn, these factors may help to strengthen suicidal ideation. Therefore, when it comes to mental health, such as suicidal ideation, medical staff and medical social workers should pay attention to the patients’ ACE and provide proper intervention.
There are some limitations to this study. This study was a cross-sectional design and the sample size was small, so the causal relationship between variables was difficult to determine. A cohort study is necessary to provide further insight. As the variables measured here are based on a self-assessment scale, objective measurement results are required. For instance, sleep quality could be measured by polysomnography. In addition, the unique sensory processing patterns of individuals with major affective disorders and their relationship with psychiatric symptomatology have been clearly reported. Hyposensitivity or hypersensitivity may be “trait” markers of individuals with major affective disorders.40 Therefore, when considering the effect of ACE, the individual’s unique sensory profiles and their behavioral and functional impact in the context of real life should be considered.
Conclusion
In young cancer patients, ACE not only affected suicide ideation directly but also affected suicide ideation by affecting sleep quality, anxiety symptoms, and inflammatory conditions during the COVID-19 pandemic. Therefore, when facing a negative mental state of cancer patients during the COVID-19 pandemic, medical staff, psychotherapists, and medical social workers can consider targeted intervention and help for patients from the perspective of ACE.
Acknowledgments
We thank all cancer patients who took part in this study.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Prev Med. 1998;14(4):245–258. doi:10.1016/s0749-3797(98)00017-8
2. Ramiro LS, Madrid BJ, Brown DW. Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse Negl. 2010;34(11):842–855. doi:10.1016/j.chiabu.2010.02.012
3. Jimenez ME, Wade RJ, Schwartz-Soicher O, et al. Adverse childhood experiences and ADHD diagnosis at age 9 years in a national urban sample. Acad Pediatr. 2017;17(4):356–361. doi:10.1016/j.acap.2016.12.009
4. Westermair AL, Stoll AM, Greggersen W, et al. All unhappy childhoods are unhappy in their own way—Differential impact of dimensions of adverse childhood experiences on adult mental health and health behavior. Front Psychiatry. 2018;9:198. doi:10.3389/fpsyt.2018.00198
5. Gouin JP, Caldwell W, Woods R, et al. Resilience resources moderate the association of adverse childhood experiences with adulthood inflammation. Ann Behav Med. 2017;51(5):782–786. doi:10.1007/s12160-017-9891-3
6. Del Vecchio GC, Schettini F, Piacente L, et al. Effects of deferiprone on immune status and cytokine pattern in thalassaemia major. Acta Haematol. 2002;108:144–149. doi:10.1159/000064705
7. Johns Hopkins Coronavirus Resource Center. Available from: https://coronavirus.jhu.edu/map.html.
8. Lassandro G, Palladino V, Palmieri VV, et al. Covid-19 and children with immune thrombocytopenia: emerging issues. Mediterr J Hematol Infect Dis. 2020;12(1):e2020028. doi:10.4084/mjhid.2020.028
9. Xiao H, Zhang Y, Kong DS, et al. Social capital and sleep quality in individuals who self-isolated for 14 days during the Coronavirus Disease 2019 (covid-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921. doi:10.12659/MSM.923921
10. Kim YJ, Lee KJ. Relationship of social support and meaning of life to suicidal thoughts in cancer patients. J Korean Acad Nurs. 2010;40(4):524–532. doi:10.4040/jkan.2010.40.4.524
11. Berardis D, Fornaro M, Orsolini L, et al. Alexithymia and suicide risk in psychiatric disorders: a mini-review. Front Psychiatry. 2017;8:148. doi:10.3389/fpsyt.2017.00148
12. Okanli A, Karabulutlu EY, Karakaş SA, et al. Alexithymia and perception of illness in patients with cancer. Eur J Cancer Care. 2018;27(3):e12839. doi:10.1111/ecc.12839
13. Pereira-Sanchez V, Adiukwu F, El Hayek S, et al. COVID-19 effect on mental health: patients and workforce. Lancet Psychiatr. 2020;7(6):e29–e30. doi:10.1016/S2215-0366(20)30153-X
14. Kajeepeta S, Gelaye B, Jackson CL, et al. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med. 2015;16(3):320–330. doi:10.1016/j.sleep.2014.12.013
15. Levine ME, Cole SW, Weir DR, et al. Childhood and later life stressors and increased inflammatory gene expression at older ages. Soc Sci Med. 2015;130:16–22. doi:10.1016/j.socscimed.2015.01.030
16. Don Richardson J, King L, St Cyr K, et al. Depression and the relationship between sleep disturbances, nightmares, and suicidal ideation in treatment-seeking Canadian Armed Forces members and veterans. BMC Psychiatr. 2018;18(1):204. doi:10.1186/s12888-018-1782-z
17. Park RJ, Kim YH. Association between high sensitivity CRP and suicidal ideation in the Korean general population. Eur Neuropsychopharmacol. 2017;27(9):885–891. doi:10.1016/j.euroneuro.2017.06.010
18. Cheong EV, Sinnott C, Dahly D, et al. Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor. BMJ Open. 2017;7(9):e013228. doi:10.1136/bmjopen-2016-013228
19. Olatunji BO, Deacon BJ, Abramowitz JS, et al. Dimensionality of somatic complaints: factor structure and psychometric properties of the self-rating anxiety scale. J Anxiety Disord. 2006;20(5):543–561. doi:10.1016/j.janxdis.2005.08.002
20. Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh sleep quality index. J Psychosom Res. 1998;45(1):5–13. doi:10.1016/s0022-3999(97)00298-5
21. Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the scale for suicide ideation. J Consult Clin Psychol. 1979;47(2):343–352. doi:10.1037//0022-006x.47.2.343
22. Li XY, Fei LP, Tong YS, et al. Reliability and validity of the Chinese version of beck suicide ideation scale(BSI-CV) in adult community residents. Chin Ment Health J. 2010;24(4):250–255. doi:10.3969/j.issn.1000-6729.2010.04.003
23. Umar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health. 2020. doi:10.1080/09638237.2020.1757052
24. Parker PA, Davis JW, Latini DM, et al. Relationship between illness uncertainty, anxiety, fear of progression and quality of life in men with favourable-risk prostate cancer undergoing active surveillance. BJU Int. 2016;117(3):469–477. doi:10.1111/bju.13099
25. Barboza Solís C, Kelly-Irving M, Fantin R, et al. Adverse childhood experiences and physiological wear-and-tear in midlife: findings from the 1958 British birth cohort. Proc Natl Acad Sci USA. 2015;112(7):E738–746. doi:10.1073/pnas.1417325112
26. Strine TW, Dube SR, Edwards VJ, et al. Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. Am J Health Behav. 2012;36(3):408–423. doi:10.5993/AJHB.36.3.11
27. Sareen J, Henriksen CA, Bolton SL, et al. Adverse childhood experiences in relation to mood and anxiety disorders in a population-based sample of active military personnel. Psychol Med. 2013;43(1):73–84. doi:10.1017/S003329171200102X
28. Chapman DP, Wheaton AG, Anda RF, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011;12(8):
29. Bader K, Schäfer V, Schenkel M, et al. Adverse childhood experiences associated with sleep in primary insomnia. J Sleep Res. 2007;16(3):285–296. doi:10.1111/j.1365-2869.2007.00608.x
30. Luby JL, Barch D, Whalen D, et al. Association between early life adversity and risk for poor emotional and physical health in adolescence: a putative mechanistic neurodevelopmental pathway. JAMA Pediatr. 2017;171(12):1168–1175. doi:10.1001/jamapediatrics.2017.3009
31. Cole SW. Social regulation of human gene expression: mechanisms and implications for public health. Am J Public Health. 2013;103:S84–92. doi:10.2105/AJPH.2012.301183
32. Liu JW, Tu YK, Lai YF, et al. Associations between sleep disturbances and suicidal ideation, plans, and attempts in adolescents: a systematic review and meta-analysis. Sleep. 2019;42(6):zsz054. doi:10.1093/sleep/zsz054
33. Winsler A, Deutsch A, Vorona RD, et al. Sleepless in Fairfax: the difference one more hour of sleep can make for teen hopelessness, suicidal ideation, and substance use. J Youth Adolesc. 2015;44(2):362–378. doi:10.1007/s10964-014-0170-3
34. Woznica AA, Carney CE, Kuo JR, et al. The insomnia and suicide link: toward an enhanced understanding of this relationship. Sleep Med Rev. 2015;22:37–46. doi:10.1016/j.smrv.2014.10.004
35. Rønnstad ATM, Halling-Overgaard AS, Hamann CR, et al. Association of atopic dermatitis with depression, anxiety, and suicidal ideation in children and adults: a systematic review and meta-analysis. J Am Acad Dermatol. 2018;79(3):448–456.e30. doi:10.1016/j.jaad.2018.03.017
36. Sokol Y, Eisenheim E. The relationship between continuous identity disturbances, negative mood, and suicidal ideation. Prim Care Companion CNS Disord. 2016;18(1). doi:10.4088/PCC.15m01824
37. Baeken C, Vanderhasselt MA, De Raedt R. Baseline ‘state anxiety’ influences HPA-axis sensitivity to one sham-controlled HF-rTMS session applied to the right dorsolateral prefrontal cortex. Psychoneuroendocrinology. 2011;36(1):60–67. doi:10.1016/j.psyneuen.2010.06.006
38. Chang CC, Tzeng NS, Kao YC, et al. The relationships of current suicidal ideation with inflammatory markers and heart rate variability in unmedicated patients with major depressive disorder. Psychiatry Res. 2017;258:449–456. doi:10.1016/j.psychres.2017.08.076
39. Unszain PA, Hepgul N, Pariante CM. Inflammation and depression. Curr Top Behav Neurosci. 2013;14:135–151. doi:10.1007/7854_2012_211
40. Engel-Yeger B, Muzio C, Rinosi G, et al. Extreme sensory processing patterns and their relation with clinical conditions among individuals with major affective disorders. Psychiatry Res. 2016;236:112–118. doi:10.1016/j.psychres.2015.12.022
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
