Back to Journals » Infection and Drug Resistance » Volume 15
The Dissemination of Fusidic Acid Resistance Among Staphylococcus epidermidis Clinical Isolates in Wenzhou, China
Received 4 March 2022
Accepted for publication 12 May 2022
Published 17 May 2022 Volume 2022:15 Pages 2537—2544
DOI https://doi.org/10.2147/IDR.S365071
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Shuying Chen,* Lulin Rao,* Chunchan Lin
Department of Laboratory Medicine, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, 325000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chunchan Lin, Email [email protected]
Purpose: Fusidic acid (FA), a potent steroidal antibiotic, is used topically to treat skin and soft tissue infections (SSTIs) caused by Staphylococci. The aim of this study is to report the prevalence of fusidic acid resistance among Staphylococcus epidermidis clinical isolates from a tertiary hospital in Wenzhou, east China.
Methods: The antibiotic susceptibility of S. epidermidis isolates was determined by disc diffusion method and agar dilution method. Then, FA-resistant S. epidermidis isolates were characterized by multi-locus sequence typing, SCCmec typing and pulsed-field gel electrophoresis.
Results: In the present study, the 55 (7.7%) FA-resistant S. epidermidis among 711 S. epidermidis clinical isolates were isolated from different parts of 53 patients. Fifty-five FA-resistant S. epidermidis isolates with FA MIC values ranged from 4 to 32 μg/mL. Among them, 50 (90.9%) were identified as methicillin-resistant Staphylococcus epidermidis (MRSE), in which mecA were positive. Meanwhile, the positive rates of fusB and fusC genes among FA-resistant S. epidermidis isolates were 85.5% (47/55) and 7.3% (4/55), respectively. All 55 isolates mentioned above were susceptible to vancomycin. More than 50% of FA-resistant isolates were resistant to non-β-lactam antimicrobials including erythromycin (80.0%, 44/55), clindamycin (65.5%, 36/55), ciprofloxacin (63.6%, 35/55) and sulfamethoxazole (63.6%, 35/55). A total of 14 sequence types (STs) were identified among the 55 FA-resistant S. epidermidis isolates, of which, ST2 (24/55, 43.6%) was the most predominant type. And the eBURST analysis showed that CC2, CC5 and CC247 accounted for 43.6% (24/55), 27.3% (15/55) and 14.5% (5/55), respectively. Meanwhile, a total of four SCCmec types (I, III, IV, V) were identified among the 55 FA-resistant S. epidermidis. Furthermore, the pulsed field gel electrophoresis divided the 55 isolates into 20 types, namely A-T. Q-type strains were most prevalent, accounting for 30.9% (17/55).
Conclusion: Taken together, the dissemination of S. epidermidis ST2 clone with FA resistance can cause trouble in controlling S. epidermidis infections.
Keywords: Staphylococcus epidermidis, fusidic acid, resistance, molecular characteristics
Introduction
Staphylococcus epidermidis is a member of the coagulase-negative staphylococci (CoNS), considered a component of the normal commensal microflora in human.1 Colonization by S. epidermidis contributes to the maintenance of a healthy skin flora, especially by competing with potentially harmful microorganisms such as Staphylococcus aureus.2 However, in recent decades, with the increased use of indwelling or implanted medical devices and the increase of sickly, elderly and immunocompromised patients, S. epidermidis has emerged as an important opportunistic pathogen responsible for hospital-acquired infections, particularly biofilm-associated infections.3
Fusidic acid, employed for the treatment of superficial and systemic disease caused by staphylococci, is a valuable alternative to vancomycin for the infections caused by multi-drug resistant Staphylococci, especially the infection of methicillin-resistant Staphylococcus aureus.4–6 But there is a concern that there is a significant trend towards increased FA resistance among Staphylococci with increased duration of use, which is an even greater problem for limiting our therapeutic options.1,7 Fusidic acid inhibits elongation factor G (EF-G) release from ribosomes and eventually blocks the synthesis of bacterial proteins.8 As in S. aureus, resistance to FA in S. epidermidis results either from the mutation of fusA, or acquiring fusB or fusC resistance genes.9,10
Strikingly, studies have shown the proportion of fusidic acid-resistant S. epidermidis higher than that in S. aureus.11,12 Molecular analysis for S. epidermidis isolates associated with nosocomial infections has shown considerable clonal diversity and is much less studied than that for S. aureus.13 Multi-locus sequence typing (MLST) based on nucleotide sequencing of seven housekeeping genes revealed distinct related clones of MRSE from clinically significant isolates and showed a worldwide predominance of only a few hospital-associated, epidemic clonal lineages.13 Clonal complex 2 (CC2) was major genetic lineage among the population structure of hospital-acquired S. epidermidis worldwide.14,15 Limited information of the resistance of S. epidermidis clinical isolates to FA is available. The purpose of our study is to investigate the dissemination of FA resistance and molecular characteristics of S. epidermidis isolates from hospitalized patients in a tertiary hospital in Wenzhou, east China.
Materials and Methods
Collection of S. Epidermidis Clinical Isolates
Seven hundred and seventy-one non-duplicate S. epidermidis isolates were collected consecutively from various specimens of inpatients at the first Affiliated Hospital of Wenzhou Medical University. The isolates were identified as S. epidermidis by using Gram’s stain, catalase test and VITEK automatic microbiology analyzer (bioMe´rieux, Marcy l’Etoile, France).
Screening for Fusidic Acid-Resistant S. Epidermidis
The minimum inhibitory concentration (MIC) of FA for S. epidermidis isolates was determined by the agar dilution method. The interpretive criterion of FA susceptibility for Staphylococci was in accordance with the European Committee for Antimicrobial Susceptibility Testing (EUCAST)/British Society of Antimicrobial Chemotherapy (BSAC) criteria (susceptible, MIC < 2 μg/mL; resistant, MIC ≥ 2 μg/mL).
Antimicrobial Susceptibility Testing
In vitro antimicrobial susceptibility testing was determined by the disk diffusion method with antimicrobials in accordance with the standards recommended by the Clinical and Laboratory Standards Institute (CLSI).16 Antibiotic discs were tested as follows: penicillin (10U), vacomycin (30 μg), erythromycin (15 μg), clindamycin (2 μg), linezolid (30 μg), tetracycline (30 μg), trimethoprim/sulfamethoxazole (1.25/23.75 μg), gentamicin (10 μg), ciprofloxacin (5 μg), and levofloxacin (5 μg). All disks were obtained from Oxoid Ltd. S. aureus ATCC25923 was used as quality control strain for antimicrobial susceptibility testing. The minimum inhibitory concentration of vancomycin was determined using the agar dilution method according to the guidelines of the CLSI.16,17
Detection of Fusidic Acid Resistance Determinants by PCR
Isolates were tested for the presence of fusB and fusC by PCR, as previously described.18 Then, the amplified DNA fragments were sequenced for further confirmation.
Multi-Locus Sequence Typing (MLST)
Multi-locus sequence typing for S. epidermidis isolates was performed by amplification of internal fragments of the seven housekeeping genes including arcC, aroE, gtr, mutS, pyrR, tpiA, and yqiL of S. epidermidis as described previously.19 The PCR products of seven housekeeping genes tested for MLST typing were purified and sequenced. The numbers of alleles and sequence types were assigned using online database (http://sepidermidis.mlst.net/). The eBURST algorithm was used to infer the evolutionary relatedness of the STs.
Staphylococcal Cassette Chromosome (SCCmec) Typing
Primers for SCCmec typing were designed according to literature.20 The 8 pairs of primers of CCr gene were CIF, KDP, MECI, DCS, RIF4, RIF5 and PUBl10R1, and the 8 pairs of primers (Type I ~ Type V) sequence were detected for mec complex. The strains harmany21 (SCCmec I), harmany24 (SCCmec II), harmany20 (SCCmec III), harmany22 (SCCmec IV) and HS662 (SCCmec V) of SCCmec were used as positive control for SCCmec typing.
Pulsed-Fifield Gel Electrophoresis (PFGE)
Our test was slightly modified from the previously described method.21 The restriction enzyme SmaI was used and the following electrophoresis conditions: switch time, 4 s to 40s; running time, 19 h in a 1% agarose gel.
Results
A total of 711 strains of Staphylococcus epidermidis isolated from patients with clinical and infectious symptoms were considered for invasive isolates and included in the investigation. Among 711 S. epidermidis isolates, 55 (7.7%) FA-resistant S. epidermidis were isolated from blood (n = 18), catheter (n = 14), sputum (n = 5), ascites (n = 3), tissue (n = 3), drainage (n = 2), wound exudate (n = 2), urine (n = 2), dialysate (n = 2), marrow (n = 1), and other sources (n = 2).
Antimicrobial Susceptibility of FA-Resistant S. epidermidis Clinical Isolates
The distribution of FA MIC levels among FA-resistant S. epidermidis is shown in Table 1. The MIC values ranging from 4 to 32 μg/mL were resistant to FA. Among 55 isolates, 50 (90.9%, 50/55) and 5 (9.1%, 5/55) FA-resistant isolates were MRSE and MSSE, respectively. Besides FA resistance, the 55. S. epidermidis were also resistant to non-beta-lactam antimicrobials as shown in Table 2. The FA-resistant isolates exhibited more than 50% of resistance rates to erythromycin (n = 44), clindamycin (n = 36), trimethoprim-sulfamethoxazole (n = 36) and ciprofloxacin (n = 35), but less than 50% of resistance rates to others including gentamicin (n = 27), rifampin (n = 26) and tetracycline (n = 13). All 55 isolates mentioned above were susceptible to vancomycin and linezolid.
 |
Table 1 Distribution of FA MIC Levels in S. epidermidis Isolates |
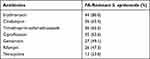 |
Table 2 Prevalence of Antibiotic Resistance in FA-Resistant S. epidermidis |
Detection of FA Resistance Determinants
Among 55. S. epidermidis isolates with FA resistance, 47 (85.5%) and 4 (7.3%) were positive for fusB and fusC, respectively. However, no resistance genes were detected in four strains.
Molecular Characteristics of S. epidermidis Clinical Isolates with FA Resistance
PCR was used to amplify arcC, aroE, gtr, mutS, pyrR, tpi and yqiL genes from 55. Strains of FA resistant Staphylococcus epidermidis. The molecular characteristics of the 55 FA-resistant S. epidermidis isolates are listed in Figure 1. A total of 14 STs were identified among the 55. S. epidermidis isolates with FA resistance, among which ST2 was the most prevalent, accounting for 43.7% (24/55), followed by ST130 (9.1%, 5/55), ST64 (7.3%, 4/55), ST59 (5.5%, 3/55), ST210 (3.6%, 2/55) and ST23 (3.6%, 2/55). Other STs was only found one isolate each, such as ST125. The STs for five isolates were not identified. In the study, ST2 was the most prevalent so that the comparison of drug resistance between ST2 and non-ST2 strains is presented in Table 3. The resistance profiles of 24 ST2 S. epidermidis isolates were similar that they were resistance to penicillin, ciprofloxacin, levofloxacin, gentamicin and trimethoprim-sulfamethoxazole, however, susceptibility to vancomycin, linezolid and tetracycline.
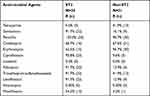 |
Table 3 The Comparison of Drug Resistance Between ST2 Type and Non-ST2 in FA-Resistant S. epidermidis |
 |
Figure 1 Results of PFGE and molecular characteristics of FA-resistant S. epidermidis isolates. |
According to the 448 ST models in the MLST database, the eBURST software analysis was performed, and the 55 clinical isolates in this study were analyzed by eBURST algorithm. Most of the isolates belonged to SCCmec III (n = 18), while 4, 3, 3 and 1 isolates belonged to SCCmec IV a, SCCmec IVd, SCCmec Vand SCCmec I, respectively. Intriguingly, half of the 24 ST2 strains were SCC mec III, and only one strain was SCCmec V. It was found that most of the strains in the clinical isolates belonged to CC2, accounting for 43.7% (24/55), while 15 and 8 strains belonged to CC5 and CC247, respectively. The founder of the clinical isolates found in this study was ST2, which was consistent with the founder found in the analysis of the S. epidermidis global database, and ST5 has the largest number in the subgroup founder, which was the single-locus variant (SLV) of ST2 (Figure 2).
Results of Pulsed Field Gel Electrophoresis (PFGE)
According to the band analysis of pulsed field gel electrophoresis, the clones with more than 80% similarity were divided into 20 types (A-T) (Figure 1), showing considerable diversity. Seventeen isolates including 12 ST2 isolates (70.6%, 12/17) belonged to PFGE Q type, indicating clonal dissemination of S. epidermidis isolates with FA resistance. Of 12 ST2 isolates with same PFGE type isolated from blood (6), catheter (5) and sputum (1) mainly distributed in ICU and comprehensive disease area. Seven isolates including 3 ST130, 2 ST2, 1 ST248 and 1 ST210 isolates belonged to PFGE type E. These 7 isolates with same PFGE type were isolated from catheter (3), urine (2), blood (1) and peritoneal dialysate (1), respectively.
Discussion
Staphylococcus epidermidis, as a conditional pathogen, often causes a series of infections in people with low immunity or in infants and the elderly. To understand the origin of FA-resistant S. epidermidis and monitor them from different sources, analysis of molecular characteristics was performed in our study.
Chen et al found that the majority of FA-resistant S. epidermidis isolates were also resistant to methicillin.22 Our result was consistent with the above study that Methicillin-resistant Staphylococcus epidermidis was the predominates. McLaws et al reported a high prevalence rate (46%, 23/50) of resistance to fusidic acid in S. epidermidis clinical isolates.12 Twenty-five percent of methicillin-resistant CNS and 15% of methicillin susceptible CNS strains isolated from blood cultures of septicemic patients in Turkey were resistant to FA.23 Compared with the reports mentioned above, the prevalence of FA in the present study was relatively low.
Two major FA resistance mechanisms were reported, the alteration of the drug target site caused by the mutations in fusA encoding elongation factor G (EF-G) or rplF encoding ribosome protein L6 and the protection of the drug target site by fusB family proteins including fusB, fusC, and fusD, which have been reported in S. aureus.4 In Staphylococci, high-level FA resistance is usually associated with mutations in fusA, while low-level resistance is generally caused by plasmid-mediated resistance genes including fusB, fusC and fusD.24 In the present study, 47 FA-resistant S. epidermidis clinical isolates were positive for fusB, while only four were positive for fusC. Colonized Staphylococci on skin may be reservoir for fusidic acid resistance genes.25 The monitor for presence of fusidic acid resistance genes among S. epidermidis should be helpful for preventing the dissemination of FA-resistant S. epidermidis.
So far, a total of 448 ST types of S. epidermidis have been found worldwide. The main ST types of FA-resistant S. epidermidis in the drug resistance spectrum were ST2, ST130, ST64 and ST59. Studies had shown that ST2 was the main ST type of clinical isolates of S. epidermidis in the reports in the United States, Germany and other countries.26,27 In our study, ST2 was also found to be the most prevalent clone among S. epidermidis isolates with FA resistance, which was consistent with the main ST type of S. epidermidis found in other countries. In the present study, 24 ST2 MRSE with FA resistance isolated from blood, catheter, sputum, urine and ascites distributed among 9 wards, indicating that ST2 S. epidermidis clone with FA resistance has disseminated in this hospital. The drug resistance rate of ST2 to gentamicin, ciprofloxacin, rifampicin, levofloxacin and moxifloxacin was more than 5 times higher than that of non-ST2. A report from China showed that 91.7% (297/324) of S. epidermidis from the community and hospital environments belonged to CC2.15 CC2 comprises 74% of the S. epidermidis isolates from 17 national centers between 1996 and 2001.14 The majority (62/71; 87.3%) of S. epidermidis clinical isolates from US hospitals belonged to CC2.28 We speculate that acquiring resistance to FA, as well as multi-resistance to other antimicrobial agents, contributes to the spread of S. epidermidis ST2 clone. ST23 was found among linezolid-resistant S. epidermidis isolates.29,30 In the present study, ST23 was identified in 2 S. epidermidis isolates with resistance to FA, which was first found among S. epidermidis isolates isolated from China. Although ST125 exist in online database (http://sepidermidis.mlst.net/), the literatures about S. epidermidis ST125 isolates was not found. The present study first reported ST125 among S. epidermidis clinical isolates. Taken together, the dissemination of S. epidermidis ST2 clone with FA resistance can cause trouble in controlling S. epidermidis infections.
In addition, although the results of PFGE for the 55 strains showed considerable diversity (20 PFGE types), 17 isolates including 12 ST2 isolates belonged to PFGE Q type, indicating clonal dissemination of S. epidermidis isolates with FA resistance has occurred. Clonal dissemination was the main reason for the cross-medical structure, cross-regional and even transnational global epidemic of S. epidermidis. Therefore, the etiological methods of tracking and monitoring strains should clarify the homology and clonal dissemination of S. epidermidis strains timely and accurately at the type, subtype and molecular level, so as to effectively control the nosocomial infection of Staphylococcus epidermidis and the cloning and dissemination of bacterial drug resistance genes.
Ethics Statement
As the Staphylococcus epidermidis clinical isolates in this study were a part of the routine hospital laboratory procedure, the Ethics Committee of the first Affiliated Hospital of Wenzhou Medical University exempted this research for review.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by grants from Wenzhou Municipal Science and Technology Bureau (Y2020848).
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014;27(4):870–926. doi:10.1128/CMR.00109-13
2. Otto M. Molecular basis of Staphylococcus epidermidis infections. Semin Immunopathol. 2012;34(2):201–214. doi:10.1007/s00281-011-0296-2
3. Onishi M, Urushibara N, Kawaguchiya M, et al. Prevalence and genetic diversity of arginine catabolic mobile element (ACME) in clinical isolates of coagulase-negative staphylococci: identification of ACME type I variants in Staphylococcus epidermidis. Infect Genet Evol. 2013;20:381–388. doi:10.1016/j.meegid.2013.09.018
4. Wang JL, Tang HJ, Hsieh PH, et al. Fusidic acid for the treatment of bone and joint infections caused by methicillin-resistant Staphylococcus aureus. Int J Antimicrob Agents. 2012;40(2):103–107. doi:10.1016/j.ijantimicag.2012.03.010
5. Schofer H, Simonsen L. Fusidic acid in dermatology: an updated review. Eur J Dermatol. 2010;20(1):6–15. doi:10.1684/ejd.2010.0833
6. Whitby M. Fusidic acid in the treatment of methicillin-resistant Staphylococcus aureus. Int J Antimicrob Agents. 1999;12(Suppl 2):S67–71. doi:10.1016/S0924-8579(98)00075-2
7. Martins A, Cunha Mde L. Methicillin resistance in Staphylococcus aureus and coagulase-negative staphylococci: epidemiological and molecular aspects. Microbiol Immunol. 2007;51(9):787–795. doi:10.1111/j.1348-0421.2007.tb03968.x
8. Farrell DJ, Castanheira M, Chopra I. Characterization of global patterns and the genetics of fusidic acid resistance. Clin Infect Dis. 2011;52(Suppl 7):S487–92. doi:10.1093/cid/cir164
9. O’Neill AJ, McLaws F, Kahlmeter G, Henriksen AS, Chopra I. Genetic basis of resistance to fusidic acid in staphylococci. Antimicrob Agents Chemother. 2007;51(5):1737–1740. doi:10.1128/aac.01542-06
10. O’Neill AJ, Chopra I. Molecular basis of fusB-mediated resistance to fusidic acid in Staphylococcus aureus. Mol Microbiol. 2006;59(2):664–676. doi:10.1111/j.1365-2958.2005.04971.x
11. Chen HJ, Tsai JC, Hung WC, Tseng SP, Hsueh PR, Teng LJ. Identification of fusB-mediated fusidic acid resistance islands in Staphylococcus epidermidis isolates. Antimicrob Agents Chemother. 2011;55(12):5842–5849. doi:10.1128/AAC.00592-11
12. McLaws F, Chopra I, O’Neill AJ. High prevalence of resistance to fusidic acid in clinical isolates of Staphylococcus epidermidis. J Antimicrob Chemother. 2008;61(5):1040–1043. doi:10.1093/jac/dkn071
13. Widerstrom M, Wistrom J, Sjostedt A, Monsen T. Coagulase-negative staphylococci: update on the molecular epidemiology and clinical presentation, with a focus on Staphylococcus epidermidis and Staphylococcus saprophyticus. Eur J Clin Microbiol Infect Dis. 2012;31(1):7–20. doi:10.1007/s10096-011-1270-6
14. Miragaia M, Thomas JC, Couto I, Enright MC, de Lencastre H. Inferring a population structure for Staphylococcus epidermidis from multilocus sequence typing data. J Bacteriol. 2007;189(6):2540–2552. doi:10.1128/JB.01484-06
15. Du X, Zhu Y, Song Y, et al. Molecular analysis of Staphylococcus epidermidis strains isolated from community and hospital environments in China. PLoS One. 2013;8(5):e62742. doi:10.1371/journal.pone.0062742
16. CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 24th Informational Supplement (M100-S24). Clinical and Laboratory Standards Institute; 2014.
17. CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 24th Informational Supplement (M100-S24). Wayne, PA, USA: Clinical and Laboratory Standards Institute; 2014.
18. Chen HJ, Hung WC, Tseng SP, Tsai JC, Hsueh PR, Teng LJ. Fusidic acid resistance determinants in Staphylococcus aureus clinical isolates. Antimicrob Agents Chemother. 2010;54(12):4985–4991. doi:10.1128/AAC.00523-10
19. Li T, Song Y, Zhu Y, Du X, Li M. Current status of Staphylococcus aureus infection in a central teaching hospital in Shanghai, China. BMC Microbiol. 2013;13(1):153. doi:10.1186/1471-2180-13-153
20. Chongtrakool P, Ito T, Ma XX, et al. Staphylococcal Cassette Chromosome mec (SCCmec) typing of methicillin-resistant Staphylococcus aureus strains isolated in 11 Asian countries: a proposal for a new nomenclature for SCCmec elements. Antimicrob Agents Chemother. 2006;50(3):1001–1012. doi:10.1128/aac.50.3.1001-1012.2006
21. McDougal LK, Steward CD, Killgore GE, Chaitram JM, McAllister SK, Tenover FC. Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: establishing a national database. J Clin Microbiol. 2003;41(11):5113–5120. doi:10.1128/jcm.41.11.5113-5120.2003
22. Chen HJ, Chang YC, Tsai JC, et al. New structure of phage-related islands carrying fusB and a virulence gene in fusidic acid-resistant Staphylococcus epidermidis. Antimicrob Agents Chemother. 2013;57(11):5737–5739. doi:10.1128/aac.01433-13
23. Koksal F, Yasar H, Samasti M. Antibiotic resistance patterns of coagulase-negative staphylococcus strains isolated from blood cultures of septicemic patients in Turkey. Microbiol Res. 2009;164(4):404–410. doi:10.1016/j.micres.2007.03.004
24. McLaws FB, Larsen AR, Skov RL, Chopra I, O’Neill AJ. Distribution of fusidic acid resistance determinants in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2011;55(3):1173–1176. doi:10.1128/AAC.00817-10
25. Hung WC, Chen HJ, Lin YT, et al. Skin commensal staphylococci may act as reservoir for fusidic acid resistance genes. PLoS One. 2015;10(11):e0143106. doi:10.1371/journal.pone.0143106
26. Sharma P, Satorius AE, Raff MR, Rivera A, Newton DW, Younger JG. Multilocus sequence typing for interpreting blood isolates of Staphylococcus epidermidis. Interdiscip Perspect Infect Dis. 2014;2014:787458. doi:10.1155/2014/787458
27. Mertens A, Ghebremedhin B. Genetic determinants and biofilm formation of clinical Staphylococcus epidermidis isolates from blood cultures and indwelling devises. Eur J Microbiol Immunol. 2013;3(2):111–119. doi:10.1556/EuJMI.3.2013.2.4
28. Mendes RE, Deshpande LM, Costello AJ, Farrell DJ. Molecular epidemiology of Staphylococcus epidermidis clinical isolates from U.S. hospitals. Antimicrob Agents Chemother. 2012;56(9):4656–4661. doi:10.1128/AAC.00279-12
29. Brenciani A, Morroni G, Pollini S, et al. Characterization of novel conjugative multiresistance plasmids carrying cfr from linezolid-resistant Staphylococcus epidermidis clinical isolates from Italy. J Antimicrob Chemother. 2016;71(2):307–313. doi:10.1093/jac/dkv341
30. Martinez-Melendez A, Morfin-Otero R, Villarreal-Trevino L, et al. Molecular epidemiology of coagulase-negative bloodstream isolates: detection of Staphylococcus epidermidis ST2, ST7 and linezolid-resistant ST23. Braz J Infect Dis. 2016;20(5):419–428. doi:10.1016/j.bjid.2016.05.007
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

