Back to Journals » Journal of Healthcare Leadership » Volume 13
The Diffusion of Home-Based Reablement in Norwegian Municipalities
Authors Bliksvær T , Bertelsen TM , Fabritius MK, Hansen MB , Lunde BV, Waldahl RH
Received 26 June 2021
Accepted for publication 2 September 2021
Published 12 October 2021 Volume 2021:13 Pages 231—242
DOI https://doi.org/10.2147/JHL.S326663
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Russell Taichman
Trond Bliksvær,1 Tilde Marie Bertelsen,2 Merete Kvamme Fabritius,1 Morten Balle Hansen,2 Bente Vibecke Lunde,3 Ragnhild Holmen Waldahl1
1Nordland Research Institute, Bodø, Norway; 2Center for Organization, Management and Administration (COMA), Department of Politics and Society, Aalborg University, Aalborg, Denmark; 3Faculty of Social Sciences, Nord University, Bodø, Norway
Correspondence: Trond Bliksvær
Nordland Research Institute, Pb 1490, Bodø, 8049, Norway
Tel +47 95075408
Email [email protected]
Introduction: Home-based reablement (HBR) has achieved significant international prominence in recent years. In the Nordic countries, HBR has been introduced as an innovative care model within the municipal health care sector that answers the need for better and more effective service delivery. But knowledge about how innovations can be spread in the municipal health care sector is scarce. We also know little about what role first-line managers (FLMs) may play for the diffusion of innovations.
Purpose: To describe and explain adoption of HBR in municipalities in Norway and to explore if there is a relationship between early/late adoption and the FLM’s perception of innovativeness in their organization. Such knowledge is valuable for the understanding of the role of FLM for the diffusion of innovations in the health care sector.
Methods: A cross-sectional national online survey was carried out among FLM in the eldercare sector in 422 Norwegian municipalities. The response rate was 64%. The analysis was based on univariate and bivariate techniques, factor analysis, and multiple linear regression.
Results: A bivariate analysis revealed that early adoption is associated with a high score on perception of innovativeness among FLMs. Innovators and early adopters scored highest (5.65) on perception of innovativeness, followed by early majority (5.31) and late majority (5.18). The lowest score was found among Laggards. A multiple regression analysis revealed that a substantial part of the positive relationship between early adoption and perception of innovativeness can be explained by FLMs’ length of service in the organization and their educational level. Wealth of the municipality does not have an effect on innovativeness.
Conclusion: An implication of the results is that mature and stable personnel in key positions in the organization, and personnel with higher education, can be positive for innovativeness in the municipal health care sector.
Keywords: restorative care, innovativeness, diffusion of innovations, health care service, elderly care
Introduction
The municipal health and care sector in many western countries has to handle the prospect of increasing demand for health care services and limited resources to provide them – and a corresponding imperative to be innovative and find better and more effective ways to deliver services.1,2 In the Nordic countries, home-based reablement (HBR) has been promoted as an example of innovation policy in the care and health sector,3,4 but also in other countries (Europe, Australia, USA, and New Zealand) similar interventions have been implemented during the last decades, often designated as “restorative care”.5,6 Although several of the key elements in this form of rehabilitation have existed in the municipal health care service for a long time, HBR is an important, some would say paradigmatic, shift in the way health care for the elderly is understood and delivered.3,7 It is an early, time-limited, home-based intervention that emphasizes intensive, goal-oriented, and interprofessional rehabilitation focusing on the elderly’s own resources.8 The first HBR initiatives were seen in Norway around 2010,9 though these drew important inspiration from early Danish experiences. In Denmark, early versions of HBR started in 2007, and HBR has been mandated by law since 2015.3
We know little about how this model has spread among municipalities,10 what the drivers are, and what role central actors in the diffusion of innovations in organizations may have played. In the research literature, there has been significant interest in the influence of first-line managers on innovativeness.11 Against this background, the focus of this paper is twofold: to describe and explain variations in the adoption of HBR in municipalities in Norway and to explore the degree to which adoption of HBR is associated with first-line managers’ own perception of innovativeness in their organization. The results of the article are thus relevant for the understanding of the role of first-line managers in the diffusion of innovations in the health care sector, and how a subjective conceptualization of innovativeness among an important group of stakeholders may be connected to the objective conceptualization often used in diffusion studies of innovation.11,12 The paper uses data from a 2018 survey about HBR in Norwegian municipalities in which respondents were first-line managers in the municipal health care sector.
Home-Based Reablement as Innovation in the Care Service Sector
Home-based reablement is a rather recent trend within the health care sector.3 In a Nordic context, its forerunner was first introduced in the late 1990s in Östersund municipality in Sweden, while Denmark and Norway introduced the model in 2007 and 2010, respectively.9 In Norway, the focus on HBR was stimulated by two national reforms: 1) “The Coordination Reform,”13 which addressed the need for better coordinated services for an aging population needing complex health services, and 2) the Norwegian Ministry of Health and Care Services’ “Future Care”14 report to Parliament, which recommended that HBR should be developed further. In contrast to neighboring Denmark, the Norwegian government has not legally mandated HBR. Instead, a more voluntary approach has been used. Three professional organizations (the Norwegian Nurses Organisation, the Norwegian Occupational Therapy Association, and the Norwegian Physiotherapist Association) ran a national collaborative project from 2012 to 2015. The project received financial support from the government, and the aim was to facilitate the introduction of HBR in Norwegian municipalities.9 The project’s intention was to increase the municipalities’ knowledge about the methodology and the effects of HBR through the development of educational materials, establishing networks, and strengthening “innovative thinking” within health and care services.15 Over a period of three years starting in 2013, the Norwegian Directorate of Health granted 63.4 million kroner (approx. 6 million Euro) to 43 Norwegian municipalities that applied for financial support to develop and test HBR in their organizations.16 Hence, even though legal measures were not used, the collaboration between various organizations and the government seems to have significantly facilitated the development of HBR in a number of municipalities in the early years.
There is no explicit and clear-cut definition of HBR, but it has been described as a more generic form of rehabilitation than the specialized and diagnosis-oriented traditional approach to rehabilitation.5,9 People who struggle to cope with activities of daily living at home, or who cannot participate in activities in the local community, are eligible for home-based reablement.17 Furthermore, HBR is interdisciplinary, intensive, and time-limited, and associated with values like collaboration, user-centeredness, and active ageing.8,9 Several of these elements have been part of rehabilitation services for many years already,9 but the recent prioritization of rehabilitation in people’s homes or local communities is a prominent characteristic of HBR. HBR thus conforms with conventional conceptualizations of social innovation as “a set of novel, creative, human-centered, and value-driven processes aiming to bring about change” at the organizational or societal level, often with stakeholders that collaborate to make improvements.18
Explaining the Adoption of Home-Based Reablement
The question of how innovations spread from one context to another is a core topic in literature on innovation. According to theories on the diffusion of innovations, innovativeness can be defined as one individual or organization’s inclination to adopt a new idea relatively earlier than other members of society.12,19 Rogers12 has suggested five adopter categories, which are defined by the number of standard deviations (sd) from the average time of adoption: 1) “Innovators” (observations more than 2 sd from the mean on the left side of the normal curve), 2) “Early adopters” (observations between 1 and 2 sd on left side), 3), “Early majority” (observations less than 1 sd on the left side), 4) “Late majority,” and 5) “Laggards” – both on the right hand side of the mean (less than 1 sd and greater than 1 sd respectively).
Another approach to the distribution of innovations, translation theory, focuses on the involved actors’ subjective frames of reference and how they negotiate the importance of innovations by telling convincing stories. This is a neo-institutional approach that argues that local actors translate and recreate innovations and incorporate their own meaning into the concept of innovation.20 Thus, the research literature has identified factors at both the organizational and individual level as possible drivers for the adoption of innovations.12,21–24 Research has emphasized organizational size as an important factor in innovativeness. While empirical findings from single studies remain inconsistent, findings from systematic reviews report a primarily positive relationship between size and innovation.25,26 The larger the organization, the more prone it is to early adoption of an innovation.12,23,27,28 Larger organizations tend to possess greater resources, are more differentiated and professionalized, and therefore more capable of organizational change. Municipal wealth is indicative of organizational capacity, which is generally believed to foster innovation.11 Organizations with ample or slack resources have room to experiment with the adoption of innovations since they are less vulnerable to the risks associated with adopting the innovations.27 Still, the relationship between economic resources and innovativeness is debated since researchers have also observed a negative relationship between the two, indicating that economic need can also be a driver of innovativeness.29 The need to solve a problem may also drive the adoption of innovations.11 Research has indicated that the more professionalized a municipal administration is, the more likely it is that the administration will adopt an innovation.11
Research has, to an increasing extent, shown the importance of individual actors, such as first-line managers, as facilitators of innovations.11,12,19,27,28,30 The literature has identified various managerial characteristics that influence the adoption of innovations, such as gender, age, education, length of service in the organization, political orientation, and attitude towards innovation.28,31,32 In this paper, we focus on educational level, leadership education, and length of service as well as gender and age. First-line managers that have higher education are expected to have gained theoretical knowledge, which increases their ability to find effective solutions to complex problems.12,31,33 Analytical skills and theoretical knowledge mean that they are more likely to initiate and implement innovations and have incentives to initiate and work with innovations in their organization.11 Higher education also makes managers relevant and competent partners in research and special projects. Another prerequisite for innovation is the capacity to motivate and convince colleagues, and to involve them in collaborations that can stimulate the innovation process – capacities that are likely to be attained through management education. Modern leadership models that see leadership as a processual and relational task which is realized through collaboration and dialogue with colleagues are the most successful in stimulating collaborative innovation.34–36 Since such competencies are likely to be attained through formal leadership education, we include management education as a factor in our analysis. The impact of length of service (tenure) for innovativeness has been discussed in the literature; however, the relationship seems unclear. On the one hand, research has recognized that newcomers may bring new ideas and practices, and that they have less commitment to the existing formal and informal structures and routines of the organization. They may contribute to “hybrid situations” where ingredients from different contexts are combined into new and innovative practices through “boundary crossing.”37 On the other hand, one can also hypothesize a positive relationship: experience and persistence in a leadership position provides legitimacy and contextual knowledge that is helpful for the management of complex processes and social relations.31,38 Benner’s classic study of nursing practices shows how nurses develop their practice through stages, and how experience and maturity resulted in an expert’s stance where they applied intuition and reflection to find new solutions.39
Materials and Methods
The paper is based on a nation-wide survey that was distributed in 2018 by the first, second, fourth and fifth author among first-line managers and coordinators in the eldercare sector in Norwegian municipalities. The survey was inspired by a Danish survey about HBR that was carried out in Danish municipalities in 2017 with the aim to study the implementation and organisation of HBR ten years after the introduction of the model and two years after it was mandated by law.3 The Norwegian questionnaire included many of the same questions and design as the Danish study and had the purpose of studying the diffusion of HBR as an innovative eldercare measure in a Norwegian context, where HBR was not legally mandated. The Norwegian questionnaire was supplemented with a question measuring the respondent’s own perception of the innovativeness of his/her organisation, in order to facilitate analyses of the association between “objective” and “subjective” conceptualizations of innovativeness in the municipal health care sector. This paper thus seeks to answer the following, twofold, research question: To what extent is early/late adoption of HBR associated with first-line managers’ perception of innovativeness in their organisation? What factors can explain early or late adoption of home-based reablement (HBR) in Norwegian municipalities? The empirical analysis is based on quantitative methods, and applies univariate and bivariate techniques, factor analysis, and multiple linear regression.
Sample and Setting
The survey was carried out in November–December 2018 through an online questionnaire, administered by the authors. The response rate was 64% (274 of in total 422 municipalities), which is normal for this kind of survey. Smaller municipalities are less represented than larger ones, which is also expected. The response rate was higher among municipalities that had implemented HBR (83%) than among the other municipalities. To some extent, this can be explained by respondents in municipalities that had started using HBR being more highly motivated to participate in the survey. This bias is not expected to be a substantial problem for the purpose of this analysis, which is not to estimate population values but to investigate statistical relationships between factors. However, we need to be somewhat careful with our generalizations, in particular, for the nonadopters, where the non-response rate was highest. Respondents were first-line managers (leaders/coordinators) at various levels in the municipal organization. Thirty-four percent (N=92) were leaders in the healthcare sector, which is the second highest level of administrative leadership in Norwegian municipalities. The other respondents represented subordinate levels within their organizations: these were coordinators/leaders of home-based reablement (32%/N=88), coordinators/leaders of rehabilitation services (14%/N=34), or leaders/coordinators within home-based care services (23%/N=64). Eighty-five percent of the respondents were female, while 15% were male. The mean age was 47 years. Nineteen percent (N=51) in the sample had education at masters level and 46% (N=127) had management education. The mean number of years employed in organization was 12.9 years (median=10 years).
Measurement
We thus have two indicators of “innovativeness” that partly correspond to two different theoretical lenses within innovation research: theories of diffusion of innovations and translation theory. For the former, the adoption of HBR was measured by the self-reported year of commencement of HBR in the municipality and varied from 2010 to 2018. For easier interpretation in the regression analysis, the variable was recoded into number of years since adoption. A limitation with this type of measurement is that organizations may develop gradually11 rather than annually. However, annual registration is a conventional way of registering organizational events over longer periods and serves our needs in the analyses we carry out here. One should also remember that there is some subjective judgement involved in the question of when HBR was “started.” As we have no reason to believe that this bias varies systematically with the independent variables, we do not consider it to be a significant problem.
The second dependent variable, subjective perception of innovativeness, was measured using a battery of five items, which consisted of statements related to different themes or areas that are thought to be central to social innovation (Tables 1 and 2). The first item was a general statement: that the persons’ municipality is generally innovative within health and care services. Thereafter, four statements were presented, each relating to a dimension that is thought to characterize social innovation:40 new types of services, new welfare technology, new forms of collaboration within local public services, and new forms of collaboration with private actors or the civic sector (“co-production”). The response scale was a Likert scale with seven values, from 1 (totally disagree) to 7 (totally agree). The five items were combined into an index that expressed the mean value of the five items/variables for each observation. The index was tested for internal consistency with Cronbach's alpha.41 This gave us a score of 0.86 (N of items=5), which is considered acceptable. The subjective perception of innovation index thus ranged from 1 as the lowest possible value to 7 as the highest possible value. On average, the municipalities scored 5.2 (the minimum score was 2, the maximum score was 7) on the index, which indicates that the first-line managers in the health care sector were more inclined to agree than to disagree with the statements about innovativeness in their sector.
 |
Table 1 Descriptives of Five Statements About Innovativeness |
 |
Table 2 Descriptive Statistics. (Municipalities That Have Adopted HBR Only) |
Explanatory variables at both the individual and organizational levels were included in the analysis. At the individual level, five variables were included in the model: gender (male/female), age (interval-scaled, recoding of year born), tenure (interval-scaled, measured by number of years employed in the municipal organization), educational level (master’s level or lower), and managerial education (no/yes). At the organizational level, five variables were included the number of inhabitants in the municipality (interval-scaled), which measured the organizational size; inhabitants per square kilometer (interval-scaled), which measured population density; persons above retirement age (67+), which measured the need for health care services; and tax base per inhabitant, which measured the municipality’s financial capacity. Two variables, the number of inhabitants and inhabitants per square kilometer, were log-transformed when included in the model to adjust for non-normality.42 We also included participation in the development project funded by the Norwegian Directorate of Health in the period 2013–2015 as an explanatory variable (no/yes).
Results
The Diffusion of HBR Among Norwegian Municipalities
There is no official list of the Norwegian municipalities that have implemented HBR, but an informal Facebook group run by the Norwegian Occupational Therapy Association combined with data from the survey of Norwegian municipalities used in this paper indicate that about 63% of a total of 422 Norwegian municipalities had adopted the model by the end of 2018. The first initiatives that introduced HBR in Norwegian municipalities started in 2010, and, as can be seen from our sample (Figure 1), new adopters of HBR peaked in 2015 and 2016. In those years, 35–36 new municipalities a year started implementing HBR, and thereafter the pace of adoption flattened out or slowed down. The data collection ended in late November 2018, so the numbers for 2018 were probably a bit higher by the end of the year. The cumulative adoption rate has formed the characteristic S-shaped curve that can be expected of diffusion of innovations over time.12
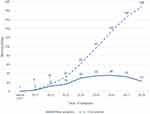 |
Figure 1 Year of adoption of reablement. Number of new adopters of HBR each year, and cumulative number. |
Uptake of HBR and Subjective Perception of Innovativeness
A main question in our research concerns the relationship between the time of the adoption of the HBR model in the organization and the perception of innovativeness among first-line managers in the health care sector. To what extent did early adoption of HBR correspond to a high score on first-line managers’ subjective perception of innovativeness? Learning networks that focused on HBR were established, and the government offered initial funding for municipalities that started implementing HBR.9 That there was an early and fairly strong political focus on the introduction of HBR as a new way of thinking about and working with rehabilitation and care in the municipal sector in Norway means that one might expect a positive relationship between these factors. However, subjective perceptions may change with the passing of time, and recent events are easier to remember than events that happened several years ago. If this assumption is correct, a more recent adoption of HBR would be expected to lead to a high score on the subjective perception of innovativeness, ie a negative correlation.
In this section, we first compare non-adopters and adopters of HBR, in order to see whether the expected positive bivariate relationship between adoption of HBR and perception of innovativeness among first-line managers in the health and care sector was confirmed. We observed a clear positive relationship (Table 3). First-line managers in municipalities that had fully implemented HBR had a higher score on the perception of innovation (5.35) than on all other categories, and significantly higher than first-line managers in municipalities that had not started or had no plans to start using HBR (4.77).
 |
Table 3 Subjective Perception of Innovativeness by HBR Adoption Status (Scale from 1 to 7) |
Figure 2 displays the bivariate relationship between perception of innovativeness and year of adoption of HBR, grouped according to the adopter categories defined by Rogers (with some adjustments due to sample composition).12 The variable has four categories, adoption year 2011–2013 (corresponding to “Innovators and early adopters”), adoption year 2014–2015 (corresponding to “Early majority”), adoption year 2016–2017 (corresponding to “Late majority”), and adoption 2018 or “not adopted” (corresponding to “Laggards”). The question is whether adopter category was associated with perception of innovativeness, and in what direction. We see a clear bivariate relationship, where early adoption is associated with a high score on perception of innovativeness. Innovators and early adopters score the highest (5.65) on perception of innovativeness, followed by Early majority (5.31), and Late majority (5.18). The lowest score is among “Laggards” (4.89 for Not adopted).
 |
Figure 2 Perception of innovativeness (scale from 2 to 7) by year of adoption of HBR. |
Multivariate Analysis
A two-step multiple linear regression analysis was carried out on each of the two indicators for innovativeness in order to explore the explanatory factors at the individual and organizational levels that were discussed in the previous sections (Table 5). For estimations, the statistical software package IBM SPSS 26.0 was used. Two blocks of independent variables were entered in the model for each dependent variable: one block with variables at the individual level (the first-line manager’s gender, age, years employed in organization, educational level, management education), and a second block with variables at the organizational (municipal) level (number of inhabitants in the municipality, population density (inhabitants per square km), share of elderly in the population, unemployment rate, and tax base). We also included participation (or not) in the collaborative HBR-project 2013–2015 as an independent variable.
When we look at the number of years since adoption of HBR as a dependent variable, the results show that the variables in model 1 explain a modest share of the total variation in the number of years since adoption (9%). Three variables – having participated in the collaborative project (Beta=0.23***), years employed in the organization (Beta=0.24**) and having higher education (Beta=0.17*) – show significant positive effects. Having participated in the HBR project increased the time since adoption of HBR by 1.14 years on average, while having worked 10 years or more in the organization increases the time since adoption by half a year on average. Having higher education increases the time since adoption by 0.79 years. When we include organizational factors in the regression model (model 2) the explained variance increases noticeably, to 15%. The size of the municipality has significant effect (Beta=0.25*). The coefficients for years employed in the organization (Beta=0.20*), and participation in the collaboration project 2013–2015 (Beta=0.17*), are reduced but still significant. The proportion of elderly in the population has no significant effect, and neither does employment rate of the municipality, nor tax base. The three significant effects in model 1 are reduced in model 2, indicating which suggests that municipal size to some degree is a confounding factor in these relationships.
When we turn to first-line managers’ perception of innovation as a dependent variable (right hand part of table), we observe a different story. The variables in model 1 provide the highest explanatory power (14% explained variance), while the variables at the structural level (model 2) add no extra to the explanatory power, nor alter the coefficients observed in model 1 to any noticeable degree. Interestingly, participation in the collaborative project in 2013–2015 has no impact on the subjective perception of innovation. Years employed in the organization (Beta=0.32***) and higher education (Beta=0.22**) have a relatively strong effect, indicating that experience in the municipal organization and having higher education increase the perception of innovativeness.
Exploring the Relationship Between Years Since Adoption of HBR and Subjective Perception of Innovativeness
In the final section, we look at years since adoption of HBR as the main explanatory variable, in a stepwise multiple regression analysis of perception of innovativeness among first-line managers (Table 4). The main question is whether, and to what degree, the managers’ perception of innovation reflects the number of years since adoption of HBR in their municipality. We are also interested in what role the other factors at the individual and organizational level may play for the managers’ perception of innovation after we control for early/late adoption of HBR.
 |
Table 4 Multiple Linear Regression. Subjective Perception of Innovativeness |
The regression analysis was run in four steps, successively introducing control factors at the individual and organizational level. Model 1 is the bivariate model, confirming our initial observation of a positive (and significant) statistical association between years since adoption of HBR and health care managers’ subjective perception of innovativeness. The explained variance is modest (2.3%), which indicates that even if years since adoption is significant, first-line managers’ perception of innovativeness is largely a product of other factors. In model 2, we introduce participation in the collaborative HBR project from 2013 to 2015 as an independent variable. This variable turns out not to be statistically significant and adds no explanatory power. Controlling for individual factors (model 3) reduces the effect of our main independent variable markedly (no longer significant). Model 3 increases the explanatory power of the model significantly, to 14%. In particular, length of service in the organization has shown to have a significant impact on perception of innovativeness (Beta=0.32***), and higher education also shows a significant score (Beta=0.23**). Model 4 introduces variables at the organizational level. These factors do not add much to the conclusions drawn from model 3, which comports with our earlier observations (Table 5).
 |
Table 5 Multiple Linear Regression. Years Since Adoption of HBR (Left) and Subjective Perception of Innovativeness (Right) |
The main message from this analysis is that the observed statistical relationship between years since adoption of HBR and perception of innovativeness among first-line managers can be explained, in part, by differences in the health care managers’ length of service in the organization, as well as their higher education. After controlling for length of service in the organization and their educational level, first-line managers in municipalities that are “early adopters” or “innovators” in Rogers’12 terminology do not on average have a significantly stronger sense of innovativeness than others. Furthermore, it is interesting to observe that management education does not have any significant impact on subjective perception of innovativeness, and neither do any of the factors at the organizational level.
Discussion and Conclusion
The aim of the paper has been to explain the diffusion of HBR as an innovative model within the health care sector in Norwegian municipalities, and to shed light on the degree to which the adoption of HBR is associated with first-line managers’ perception of innovativeness in the health care sector. The paper contributes to research by relating first-line managers’ “subjective” perception of innovativeness to an “objective” conceptualization often used in diffusion studies of innovation, and by exploring what factors that may explain either.11,12 More than half of the Norwegian municipalities had adopted HBR as a model by the end of 2018, eight years after the first municipalities adopted the model and six years after the launch of the national collaborative project that aimed to support the introduction of HBR. It remains to be seen whether all Norwegian municipalities will adopt the model, as has been the case in Denmark,3 where HBR is mandated by law. In the literature on diffusion of innovations, the skills and motivation of the managers involved have been emphasized as one important facilitating factor for innovation.11 This paper has been particularly interested in investigating whether the municipalities that have adopted the model – and in particular the early adopters of the model – are more likely to have first-line managers who think of their organizations as innovative compared to municipalities that have not adopted the model or have adopted it later.
The analysis has shown a significant correlation between years since adoption of HBR and first-line managers’ subjective perception of innovativeness: early adoption of HBR is associated with a high score on perception of innovativeness in the managers’ own organization. The subsequent analysis revealed that a substantial part of the observed positive statistical relationship between early adoption of HBR and perception of innovativeness can be explained by other factors. In particular, the relationship can be explained by the first-line managers’ length of service in the organization and their educational level. A likely interpretation of this finding is that educational level and length of service are both positively associated with subjective perception of innovativeness and with the adoption of innovation. In other words, the analysis indicates that first-line managers’ perception of innovativeness does not in itself play a significant role in the diffusion of innovations, and it therefore also questions the role of first-line managers’ subjective perception of innovativeness in the municipal adoption of innovations. It has been established in the literature that having managers with higher education is important to the adoption of innovations,11,19 which is also confirmed in this analysis. A somewhat more surprising finding is the observation that the managers’ number of years employed in the organization (which we refer to as “maturity”) has a positive – and also relatively strong – effect on innovativeness. Our results indicate that having mature and stable personnel in key positions in the organization could be important factors for innovativeness. Other studies from the health sector have reported similar observations,19 which indicate that individuals who have reached a certain level of maturity in their professional life are more likely to be innovative as compared to individuals who are new in a profession and have less experience. Health care organizations are complex in terms of their professional and organizational structure, and such complexity presupposes maturity and experience among first-line managers. Furthermore, HBR involves complex user needs and is located in the user’s home, which presupposes a high degree of interdisciplinarity and collaboration between professionals. Such leadership models require a certain amount of experience and reflexivity.35
Another important result from the analysis is that the wealth of the municipality does not have an effect on innovativeness, measured neither as early adoption nor as subjective innovativeness. This is an interesting finding, and contrasts with the established assumption in research on innovation drivers that organizational wealth and capacity promote innovation.11 For example, a recent Danish study of HBR29 observed a negative statistical association between wealth and the adoption of HBR. In sum, this indicates that the relationship between early/late adoption of HBR and municipal finances is unclear and should be a focus in future research.
Possible limitations of the study are that non-responses in the survey are not equally distributed between the adopter categories, and in particular that non-adopters of HBR have a higher non-response rate than adopters. Some caution is therefore necessary when making inferences about statistical relationships. In self-administered surveys, there is also some risk for biased memory (eg years employed in organisation) and risk due to subjectivity (different understanding of abstract concepts, eg “collaboration”, “innovativeness” etc).
Ethical Approval
Review and approval from IRB or ethics committee was not required since the study did not carry out medical and health research according to the definitions in The Norwegian Act on medical and health research. Since the project collected personal data, the research project was notified to and assessed by the Norwegian Centre for Research Data (assessment number: 58358). The assessment documents that the research project processes personal data in accordance with data protection legislation. Informed consent was obtained from each participant at the opening page of the online questionnaire.
Funding
There were no sources of funding for this research.
Disclosure
Mrs Tilde Marie Bertelsen reports grants from Velux Foundation, during the conduct of the study. The authors report no conflicts of interest in this work.
References
1. Amdam J, Bergem R, Båtevik FO. Offentleg sektor i endring [Public Sector Under Change]. Scandinavian University Press (Universitetsforlaget); 2016.
2. Holmen AKT, Ringholm T. Innovasjon møter kommune [Innovation Meets Municipality]. Oslo: Cappelen Damm akademisk; 2019.
3. Bertelsen TM, Hansen MB. Hverdagsrehabilitering og velfærdsinnovation i ældreplejensorganisering [Home-Based Rehabilitation and Innovation in the Elder Care Organisation]. Aalborg Universitet; 2018.
4. Bersvendsen T. Effects of Home-Based Reablement: A Micro-Econometric Approach. 07 Media; 2020.
5. Hjelle KM, Tuntland H, Førland O, Alvsvåg H. Driving forces for home-based reablement; a qualitative study of older adults’ experiences. Health Soc Care Community. 2017;25(5):1581–1589. doi:10.1111/hsc.12324
6. Cochrane A, McGilloway S, Furlong M, Molloy D, Stevenson M, Donnelly M. Home-care“re-ablement” services for maintaining and improving older adults’ functional independence (protocol). Cochrane Database Syst Rev. 2013;11:1–2.
7. Bredland EL, Linge OA, Vik K. Det handler om verdighet: ideologi og praksis i rehabiliteringsarbeid [It’s About Dignity: Ideology and Practice in Rehabilitation Work].
8. Moe A, Brataas HV. Interdisciplinary collaboration experiences in creating an everyday rehabilitation model: a pilot study. J Multidiscip Healthc. 2016;9(1):173–182. doi:10.2147/JMDH.S103696
9. Førland O, Skumsnes R. Hverdagsrehabilitering – En oppsummering av kunnskap [Home-Based Rehabilitation – A Literature Review]. Oppsummering; 2016.
10. Vabø M, Vik K. Sammen om en aktiv hverdag. Hverdagsrehabilitering i Eigersund og Karmøy kommune – erfaringer og refleksjoner fra et forskningssamarbeid [Making an Active Every Day Life Together. Home-Based Rehabilitation in Eigersund and Karmøy Municipalities]. Oslo Metropolitan University - OsloMet: NOVA; 2017.
11. Bhatti Y, Olsen AL, Pedersen LH. Administrative professionals and the diffusion of innovations: the case of citizen service centres. Public Adm. 2011;89(2):577–594. doi:10.1111/j.1467-9299.2010.01882.x
12. Rogers EM. Diffusion of Innovations.
13. Report No. 47 to the Storting (2008–2009). The coordination reform — proper treatment – at the right place and right time. Oslo: Norwegian Ministry of Health and Care Services; 2009.
14. Report No. 29 to the Storting (2012–2013). Future care. Oslo: Norwegian Ministry of Health and Care Services; 2013.
15. Laberg T, Ness NE. Innføring av hverdagsrehabiliteringi norske kommuner [Introducing Home-Based Reablement in Norwegian Municipalities]. Ergoterapeuten. 2012.
16. Langeland E, Førland O, Aas E, et al. Modeller for hverdagsrehabilitering - en følgeevaluering i norske kommuner: effekter for brukerne og gevinster for kommunene? [Home-Based Rehabilitation Models – A Process Evaluation of Norwegian Municipalities: Effects for the Users and Gains for the Municipalities?]. Vol. nr. 6/2016. Bergen: Senter for omsorgsforskning, Vest; 2016.
17. Tuntland H, Ness NE. Hverdagsrehabilitering [Home-Based Reablement]. Oslo: Gyldendal akademisk; 2014.
18. Husebø AML, Storm M, Ødegård A, et al. Exploring social innovation (SI) within the research contexts of higher education, healthcare, and welfare services – a scoping review. Nord Soc Wor Res. 2021;12(1):72–110. doi:10.7577/njsr.3455
19. Yigit S, Aksay K. A comparison between generation X and generation Y in terms of individual innovativeness behavior: the case of Turkish health professionals. Int J Bus Adm. 2015;6:106.
20. Røhnebæk M, Lauritzen T. Kommunal innovasjon som oversettelse [Municipal Innovation as Translation]. Oslo: Cappelen Damm akademisk; 2019:193–208.
21. Berry F, Berry W. Innovation and Diffusion Models in Policy Research; In: Paul A. Sabatier (red.), Theories of the policy process. Westview Press. 2019:223–260.
22. Hansen M, Jakobsen M. Offentlig sektor innovation: hvad er det? Og hvad er værd at vide om det? [Public sector innovation: what is it? And what is worth knowing about it?]. Politica. 2013;45:243–249. doi:10.7146/politica.v45i3.69766
23. Walker RM. Internal and external antecedents of process innovation: a review and extension. Public Manag Rev. 2014;16(1):21–44. doi:10.1080/14719037.2013.771698
24. Scott WR. Institutions and organizations. Ideas, interests and identities: paperback: 360 pages Publisher: Sage (1995) language: English ISBN: 978-142242224. Management. 2014;17(2):136.
25. Camisón-Zornoza C, Lapiedra-Alcamí R, Segarra-Ciprés M, Boronat-Navarro MA. Meta-analysis of innovation and organizational size. Organ Stud. 2004;25(3):331–361. doi:10.1177/0170840604040039
26. Damanpour F, Sanchez‐Henriquez F, Chiu HH. Internal and external sources and the adoption of innovations in organizations. Br J Manag. 2018;29(4):712–730. doi:10.1111/1467-8551.12296
27. Dahl PS, Hansen KM. Diffusion of standards: the importance of size, region and external pressures in diffusion processes. Public Adm. 2006;84(2):441–459. doi:10.1111/j.1467-9299.2006.00011.x
28. Hansen M. Antecedents of organizational innovation: the diffusion of new public management into Danish local government. Public Adm. 2011;89:285–306. doi:10.1111/j.1467-9299.2010.01855.x
29. Bertelsen TM, Hansen MB, Bliksvær T, Lunde BV. Fra effektiv serviceproduktion til samskabelse: udbredelsen af et nyt styringsparadigme i dansk ældrepleje [From Effective Service Production to Co-Creation: The Dispersion of a New Management Paradigm in the Danish Elder Care Sector]. POLITICA Tidsskrift for politisk videnskab. 2021;53(3):280-299.
30. Roberts NC. Roberts: public entrepreneurship and innovation. Rev Policy Res. 1992;11(1):55–74. doi:10.1111/j.1541-1338.1992.tb00332.x
31. Damanpour F, Schneider M. Phases of the adoption of innovation in organizations: effects of environment, organization and top managers. Br J Manag. 2006;17(3):215–236. doi:10.1111/j.1467-8551.2006.00498.x
32. Kimberly JR, Evanisko MJ. Organizational innovation: the influence of individual, organizational, and contextual factors on hospital adoption of technological and administrative innovations. Acad Manag J. 1981;24(4):689–713.
33. Damanpour F, Schneider M. Characteristics of innovation and innovation adoption in public organizations: assessing the role of managers. J Public Adm Res Theory. 2009;19:106.
34. Krogh AH, Sørensen E, Torfing J. Samskabelse af innovative offentlige løsninger [Co-Creation of Innovative Public Solutions]. Vol. 2020. Oslo: Universitetsforlaget, cop.; 2020.
35. Lindland KM. Realisert ledelse av medarbeiderdrevet innovasjon i en kommunal kontekst [Managing collaborative innovation in a municipal context]. In: Holmen AKT, Ringholm T, editors. Innovasjon møter kommune [Innovation Meets Municipality]. Oslo: Cappelen Damm akademisk; 2019.
36. Totcheva CØ, Vedeler JS, Slettebø Å. Forutsetninger for vellykket sosial innovasjon i sykehjem: ledernes perspektiv – en kvalitativ intervjustudie [Prerequisites for successful social innovation in eldercare institutions – a qualitative study]. Nordisk Tidsskrift Helseforskning. 2019;15(1). doi:10.7557/14.4645
37. Akkerman SF, Bakker A. Boundary crossing and boundary objects. Rev Educ Res. 2011;81(2):132–169. doi:10.3102/0034654311404435
38. Damanpour F, Schneider M. Characteristics of innovation and innovation adoption in public organizations: assessing the role of managers. J Public Adm Res Theory. 2008;19(3):495–522. doi:10.1093/jopart/mun021
39. Benner P. From novice to expert. Excellence and power in clinical nursing practice. Am J Nurs. 1984;84(12):1479. doi:10.1097/00000446-198412000-00025
40. Willumsen E, Ødegård A. Samskaping: sosial innovasjon for helse og velferd [Co-Creation: Social innovation for Health and Welfare]. Oslo: Universitetsforlaget; 2020.
41. Ringdal K. Enhet og mangfold: samfunnsvitenskapelig forskning og kvantitativ metode [Unity and Diversity: Quantitative Methods in Social Sciences].
42. Raykov T, Marcoulides GA. An Introduction to Applied Multivariate Analysis. Hoboken: Taylor and Francis; 2012.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
