Back to Journals » Therapeutics and Clinical Risk Management » Volume 17
The Diagnostic Value of Fe3+ and Inflammation Indicators in the Death of Sepsis Patients: A Retrospective Study of 428 Patients
Received 12 November 2020
Accepted for publication 21 December 2020
Published 15 January 2021 Volume 2021:17 Pages 55—63
DOI https://doi.org/10.2147/TCRM.S291242
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Jia Wang, Junyu Wang, Bing Wei
Beijing Key Laboratory of Cardiopulmonary Cerebral Resuscitation, Capital Medical University, Emergency Medicine Clinical Research Center, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Bing Wei; Junyu Wang
Beijing Key Laboratory of Cardiopulmonary Cerebral Resuscitation, Capital Medical University, Emergency Medicine Clinical Research Center, Beijing Chao-Yang Hospital, Capital Medical University, No. 5 Jingyuan Road, Shijingshan, Beijing 100043, People’s Republic of China
Tel +86-10-51718602
Email [email protected]; [email protected]
Background: Studies have shown that a variety of blood inflammatory markers can be used to assess the criticality of patients with sepsis. In this study, the blood inflammatory factors related to the sepsis survival group and the death group were compared and analyzed, which can be used by clinicians to adjust sepsis patient treatment.
Methods: This study used retrospective methods to analyze the medical records of 428 patients with sepsis. The test of blood samples includes the patient’s age, gender, hospital stays, the concentration of procalcitonin (PCT), absolute neutrophil count (ANC), absolute lymphocyte count (ALC), neutrophil-to-lymphocyte ratio (NLR), D-dimer (DD), Fe3+, and hemoglobin (Hb) in the venous blood of patients with sepsis. The detection of PCT methods adopts the sandwich immunofluorescence (IF). ROC curve was used for the diagnosis and analysis of various factors of sepsis.
Results: Among all the patients with sepsis, 133 patients died, with a mortality rate of 31.07%. Analysis of related inflammatory indicators and the patient’s baseline parameters showed the patients age, the values of PCT, ANC, NLR, and DD in death group were statistically higher than those in survival group (all p values were < 0.05). However, the concentration of Fe3+ and ALC show an opposite trend between the two groups. Regression analysis results showed the patient’s gender, Fe3+, PCT, ANC, and DD are all independent prognostic factors for patients with sepsis. The results of the ROC curve of related diagnostic indicators show that DD has the best area under curve (AUC=0.700), the most sensitive index is ANC (74.44), and the most specific index is PCT (89.80). The results of the two-by-two combined diagnosis of the four indicators showed that the PCT+DD group had better AUC (0.748) and specificity (78.23), and the Fe3++DD group had the best sensitivity (75.89).
Conclusion: In this study, the patient’s gender and the inflammation-related markers of Fe3+, PCT, ANC, and DD can be used as independent risk factors affecting the prognosis of patients with sepsis. The combination of PCT+DD and Fe3++DD has high diagnostic value for patients with sepsis.
Keywords: sepsis, procalcitonin, Fe3+, D-dimer, immunocyte, diagnosis
Introduction
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection, which can lead to severe sepsis or septic shock.1 The patients often develop secondary acute organ dysfunction, severe sepsis, and hypotension that cannot be reversed by fluid resuscitation.2 Sepsis accounts for about 40% of the total number of patients admitted to the ICU ward, the mortality rate can be as high as 25%-40%, and the main causes of death are severe sepsis and septic shock.3 Timely diagnosis and treatment of sepsis is an important factor affecting the mortality of patients with sepsis. However, there is currently a lack of clinically specific indicators for determining infection, which are mainly based on the presence of infectious factors or clear infection foci, accompanied by non-specific indicators such as body temperature and white blood cell changes, or the existence of inversely inferred based on body temperature and white blood cell changes the possibility of infection. Generally, these factors can be affected by many factors, especially for ICU patients, and the factors affecting these two indicators may be diverse.
Biomarkers are a class of important substances that have been widely used in clinical assessment of diseases or injuries with the advancement of molecular biology in recent years. They can not only explore the mechanism of disease at the molecular level but also accurately and sensitively evaluate early tissue damage, and has its unique advantages to provide early warning and provide a good basis for clinical diagnosis. At present, there are about thousands of markers used in sepsis-related research, and among them, the most widely used and most well known is procalcitonin (PCT). PCT is one of the precursors of calcitonin, which has made great advantages in the early identification of bacterial infections and non-bacterial infections.4,5 During bacterial infections, especially severe infections, the blood levels not only increase significantly but also it is important to evaluate the severity of infection and know the prognosis and outcome of the disease. The level of PCT content in the blood is generally not affected by factors such as hormone status and treatment in the body, and the reliability is high. More and more studies have shown that PCT levels in the blood of patients with bacterial infections will increase, especially in patients with severe bacterial infections or sepsis.6,7 Therefore, in foreign clinical practice, PCT is often regarded as one of the sensitive indicators for the diagnosis of severe sepsis and is used in clinical diagnosis, treatment, and prognosis. The chelation of Fe3+ with serum transferrin can transport free iron ions. Apoferritin and Fe3+ form a serum ferritin (SF) complex, which is a storage form of iron.8 SF is an effective indicator for judging whether the body is iron-deficient or overloaded.9 Studies have shown that the transferrin level of patients with sepsis has a significant downward trend within 24 hours of onset. Therefore, predicting the concentration of Fe3+ can be used as a new biomarker for early diagnosis of sepsis. D-dimer (DD) is a specific product of fibrin monomer cross-linked by activated factor Ⅷ in the blood and then degraded by plasmin.10,11 It is considered to be a kind of indication of fibrinolysis process. Once harmful substances such as bacteria, viruses, endotoxins enter the blood, they can directly activate factor XII and initiate the endogenous coagulation pathway: the activated endogenous coagulation system can in turn activate the anticoagulation system, that is, the fibrinolytic system, so that DD rises.12 Severe pneumonia is often accompanied by systemic inflammation, which can induce and activate the coagulation system, and will further lead to the hyperfunction of the fibrinolytic system, leading to an increase in D-D.13 Studies have shown that the content of D-D in the blood increases significantly when inflammatory diseases occur in the body, and its concentration increases with the severity of inflammation. Therefore, D-D is often used as a measure of the severity of sepsis patients.14
In this study, patients were divided into survival group and death group according to the death of sepsis patients in the ICU, and compared the detection of PCT, D-D, Fe3+ in the blood of patients with inflammatory indicators for diagnosis of sepsis. To evaluate the application value of these factors in the diagnosis and prognosis of patients with sepsis.
Patients and Methods
Research Objects and Diagnostic Criteria
This study adopted a retrospective research method and selected 482 patients with sepsis in the emergency department, EICUm and ICU wards of Beijing Chao-Yang Hospital from January 2012 to June 2020. The patients were divided into two groups: 349 patients in the survival group and 133 patients in the death group. Sepsis diagnosis refers to the latest diagnostic criteria for sepsis and septic shock published in 2016 by the Journal of the American Medical Association, spesis3.0;1 Sepsis can be diagnosed if the Sequential Organ Failure Assessment (SOFA) score ≥2 points can be diagnosed as sepsis. Clinically, the bedside rapid SOFA score (respiratory rate ≥22 beats/min, change of consciousness, systolic blood pressure ≤100 mm Hg) can be performed to meet at least 2 items. After meeting the above criteria, assess whether the patient has organ dysfunction. This method saves clinical assessment time. Septic shock refers to patients with sepsis who still need to apply vasoactive drugs after adequate fluid resuscitation to maintain mean arterial pressure (MAP) ≥65mmHg and arterial blood lactic acid concentration > 2mmol/L. This study obtained the informed consent of all patients and their families, signed the informed consent form, and was approved by the hospital ethics committee.
Inclusion and Exclusion Criteria
The inclusion criteria of patients are as follows:1 patients who were older than 18 years old;2 patients whose sample collection time was less than or equal to 24 hours after the onset of onset to admission;3 no medication was applied before data collection. The exclusion criteria of patients are as follows:1 Certain diseases that cause the increase or decrease of transferrin, such as acute viral hepatitis, rheumatoid arthritis, primary renal disease, systemic lupus erythematosus, history of hemodialysis, combined Malignant tumors, etc.;2 Drug treatment has been applied before data collection;3 Patients whose clinical data is incomplete or are hospitalized for the second time;4 During treatment the patients who voluntarily give up.
Collection of Blood Samples
For the patients included in this study, 2 mL of venous blood was drawn, centrifuged for 10 minutes (3000 revolutions/min), and serum was collected for use. The sample is tested within 4 h; otherwise, it is stored in a refrigerator at −20°C.
Detection of Serum Ferritin Fe3+
Use Beckman’s AU5400 automatic biochemical analyzer, supporting reagents, and standard products to determine transferrin, the normal reference value is 1.7–3.4g/L.
D-Dimer Detection
It is determined by an automatic blood coagulation analyzer and supporting reagents. The reaction principle is a solid-phase double antibody sandwich method. The D-D contained in the sample to be tested can be captured by the D-D antibody on the membrane. A D-D monoclonal antibody-colloidal gold conjugate label, the label can be expressed as red spots, and the red intensity of the spots is proportional to the concentration of D-D in the sample. The red intensity can be measured by a quantitative reader to measure the concentration of D-D.15 Sample requirements: Use constitutive acid anticoagulant tube to draw blood, save plasma, fresh test, store in the refrigerator when not tested, not test within 24 hours, it should be stored in low temperature freezing. Detection of D-D:1 Take the clever kit from the cold storage, equilibrate at room temperature for at least half an hour, add 1.1 mL of D-D gold standard lyophilized product to the lyophilized product of D-D gold standard solution and shake it well;2 Lay the D-D reaction plate flat on the laboratory bench, and add 2 drops of D-D blocking solution to the reaction hole to make it completely infiltrate;3 Use a sterile tip to absorb 100ul organic acid Add anticoagulant plasma to the reaction plate. After it is completely infiltrated, add 2 drops of D-D washing solution;4 When the washing liquid is completely infiltrated, use a clean tip to accurately add 100ul of D-D colloidal gold solution;5 After the infiltration is complete, add 4 drops of D-D washing solution;6 Immediately read the absorbance (OD value) under the D-D item of the U2 gold standard quantifier, and calculate the D-D concentration in the sample.
PCT Detection
PCT is detected by semi-quantitative immunochromatography with German Brahms PCT-Q reagent. An anti-catacalcin monoclonal mouse antibody (tracer) labeled with colloidal gold and a polyclonal sheep anti-calcitonin antibody (solid phase) are used for detection. After 200μL of the patient’s sample is added to the detection hole, the tracer element binds to the PCT in the sample to form a labeled antigen-antibody complex. This complex moves through the area containing the detection zone by capillary action in the detection system. During this process, the labeled antigen-antibody complex binds to the solid-phase anti-PCT antibody to form a sandwich complex. When the PCT concentration is greater than or equal to 0.5ng/mL, the complex appears as a light red band, and the color intensity of the band is directly proportional to the concentration of PCT in the sample. The tracer that does not bind to PCT diffuses to the control strip area, where it is fixed, producing a very strong red band. The function of this detection system is determined by this control strip. After 30 minutes, compare with the PCT concentration color chart provided on the reference card. According to the reference value concentration range <0.5ng/mL, ≥0.5 ng/mL, ≥2ng/mL, ≥10ng/mL, they were rated as 1, 2, 3 and 4 points, respectively. The detection process of each index is strictly in accordance with the reagent instructions.
Statistical Methods
SPSS 25.0 statistical software package was used for statistical processing of the data in this study. Normally distributed measurement data are represented by mean ± standard deviation (X ± s), and skewed distribution is represented by median (interquartile range). Pairwise comparison of non-normally distributed data adopts the Kruskal–Wallis test method of non-parametric test. The ROC curve was used to analyze the diagnostic value of factors such as PCT and Fe3+ in sepsis. P<0.05 indicates that the difference is statistically significant.
Results
Baseline Data of Patients
A total of 482 patients with sepsis were included in this study. Among them, there were 133 patients in the death group, accounting for 31.07%; 295 patients in the survival group, accounting for 68.93%. There was no statistical difference in the gender and length of stay between the two groups of patients in the baseline data (all P values > 0.05). The age comparison between the two groups showed that the age of the death group was greater than that of the survival group, and the difference between the two was statistically significant (P=0.013). The test results of inflammatory cells and factors in the two groups of patients showed that the detection values of ANC, NLR, PCT, and DD in the death group were statistically higher than those in the survival group (all P<0.05, respectively). The detection results of Fe3+ and ALC were both lower than the expression of the survival group, and the difference was statistically significant (P<0.05); there was no difference in the expression of Hb between the two groups (P=0.534). See Table 1 for detailed results.
 |
Table 1 The Related Indicators of Two Groups of Patients |
The Results of Regression Analysis
The results of univariate regression analysis showed that the patient’s age, Fe3+, PCT, NLR, ANC, and DD concentrations were all influencing factors for the two groups of patients (Table 2). The results of multivariate analysis showed that the patient’s Gender, Fe3+, PCT, ANC, and DD were all independent factors affecting the survival of the patient (Table 3). In gender grouping, male sepsis patients are more likely to die after excluding other interfering factors; among the other four factors, only Fe3+ is negatively correlated with the patient’s death (B=−0.072, P=0.024); the expression of other indicators increases with the death of the patient was proportional (all B are +, all P are <0.05).
 |
Table 2 The Results of Univariate Regression Analysis |
 |
Table 3 The Results of Multivariate Regression Analysis |
The Diagnostic Value of Different Factors to Patients
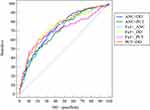
In the diagnostic analysis of the five significant factors of multivariate regression analysis, the results showed that DD has the largest area under the curve (AUC=0.700), ANC has the highest diagnostic ability (74.44%), and PCT has the highest specificity (89.80%), Fe3+ has the highest Youden index. According to the death and survival of the included patients as the sensitivity and specificity criteria of each factor. See Table 4 and Figure 1 for detailed results.
 |
Table 4 The Diagnostic Parameters of Five Indexes |
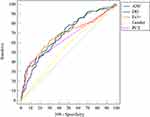 |
Figure 1 The diagnostic parameters of five indexes. Abbreviations: ANC, absolute neutrophil count; PCT, procalcitonin; DD, D-dimer. |
The Diagnostic Value of Pairwise Combination of Blood Indicators
Subsequently, we combined Fe3+, ANC, PCT, and DD in pairs and used them to diagnose death in sepsis patients. The results showed that the AUC and specificity of the PCT+DD combination were the highest (74.80% and 78.23%, respectively), and the Fe3++DD combination had the highest sensitivity and Youden index (75.89% and 41.35%, respectively). More detailed results ar show in Table 5 and Figure 2.
 |
Table 5 Diagnostic Value of the Combination of Two Factors |
Discussion
Sepsis is a disease in which pathogenic microorganisms or toxins produced by them are spread in the patient’s body through the blood circulatory system, which causes the body’s inflammatory response to disorder and leads to tissue and organ dysfunction.1 According to the results of foreign epidemiological studies, there are nearly 20 million people suffering from sepsis each year in the world, with a fatality rate of over 25%, making it the leading cause of death in intensive care units.16 The pathophysiological process of the onset of sepsis is extremely complex. We still have a long way to go to fully understand sepsis, especially the lack of effective treatment measures to reduce the morbidity and mortality of sepsis, then sepsis the early and mid-term differential diagnosis of disease is extremely important.
The discovery of new biomarkers in the early diagnosis of sepsis is particularly important to facilitate the identification of sepsis as soon as possible, and it is helpful to take effective treatment measures as soon as possible to reduce the mortality of patients with sepsis. Biomarkers can be used for the diagnosis of sepsis, disease staging, response to therapeutic intervention and prognostic evaluation. The blood culture examination of the body is a traditional method for diagnosing sepsis. It not only takes a long time but also has a low positive rate, which cannot be used in clinical diagnosis in a timely and effective manner. According to researches, PCT has better specificity and sensitivity than white blood cell count and neutrophil percentage in the diagnosis of infectious diseases. This study showed that the expression of neutrophils and the ratio of NLR in the death group were higher than those in the survival group (all P values were <0.01). However, when a patient with sepsis is in septic shock, the WBC count and body temperature cannot reflect the presence of bacterial infection in the patient. This limits the diagnostic value of neutrophils to a certain extent. Furthermore, PCT is not affected by immunosuppression and can well identify bacterial infections. PCT increases rapidly when bacterial infections occur in the patient’s body and decreases rapidly after the infection is controlled.17,18 PCT activity is stable and not easily affected by other factors. It has been used as a detection indicator for many diseases and has shown good clinical practicability. Compared with traditional laboratory indicators, PCT has the advantages of simple and fast response, good repeatability, high sensitivity, and specificity. These advantages can assist clinicians in the diagnosis and differential diagnosis of related infectious diseases. Therefore, PCT has received more and more attention from clinicians. However, the sensitivity and specificity of PCT in different studies are quite different.19 The diagnostic criteria recommended by the American Association of Chest Physicians/American Society of Critical Care Medicine (ACCP/SCCM) and the 2001 International Sepsis Conference’s diagnostic criteria for sepsis both proposed to include PCT and C-reaction Protein (CRP) is used as a diagnostic element. In the detection and analysis of many sepsis biomarkers, Suarez et al found that PCT is a good indicator for assessing the severity of infection in patients.20 Since then, many indicators have not made great breakthroughs in the treatment of sepsis, so it is still very necessary and practical to propose a new biomarker for the diagnosis and treatment of early sepsis. Assicot et al21 first found a significant increase in PCT in the serum of infected patients in 1993. PCT is regulated by the CALC-1 gene on the short arm of human chromosome 11. Under normal circumstances, the concentration of PCT in healthy people is less than 0.1ng/mL, which can hardly be detected in serum. However, when the concentration of PCT increases sharply after bacterial infection, it can reach a peak within 6–8 hours,22 up to 1000 ng/mL,23 and gradually return to normal after 24 hours, and it can persist for up to 7 days.24 The study of PCT in this study showed that the concentration of patients in the death group was higher than that in the survival group, and there was a statistical difference between the two groups (P<0.05), which was consistent with the study by Assicot et al, and the regression analysis showed that PCT was Independent risk factors affecting death of patients. In the study of the diagnostic value of PCT in patients with sepsis, PCT has the highest specificity (89.80%); this is consistent with the high specificity of PCT in clinical studies for sepsis caused by bacterial infection. Therefore, PCT can be used as a biomarker to diagnose sepsis and identify severe bacterial infections.
The high concentration of free iron (Fe3+) in cells has serious side effects on cells. An important regulator that regulates iron storage and metabolism is SF secreted by hepatocytes, macrophages, and Kupffer cells. When iron in the body increases, SF takes into iron and convert the divalent iron to trivalent iron for storage, to avoid the toxic effect of high concentration of Fe3+ in the cell; when the iron demand in the body increases and the free iron in the cell decreases, SF can release Fe3+ at any time for the body Required. Many diseases are related to iron deficiency and iron overload in the body. In these cases, the detection of Fe3+ levels can provide an important basis for the diagnosis and treatment of diseases. Some studies have confirmed that the reduction of Fe3+ can be seen in inflammation, malignant tumors, etc., which is considered to be related to iron metabolism disorders in these disease states. This study showed that the Fe3+ concentration in the death group was significantly lower than that in the survival group, and there was a statistical difference between the two groups (P<0.001). Regression analysis results show that Fe3+ is an independent risk factor that affects the death of patients. In the research on the diagnostic value of Fe3+ in patients with sepsis, Fe3+ has the highest Youden index (30.17%). This is consistent with the results obtained by Shanbhogue et al15 in observing the changes of serum iron in a group of patients with acute abdominal infection. They found that the preoperative serum iron of this group of patients was significantly lower than that of the normal control group. We believe that the decrease of Fe3+ in the death group may be due to the body’s stress response process. The lactoferrin released by granulocytes forms a lactoferrin-iron complex with iron. The liver cell receptor can recognize the lactoferrin molecule containing fucose residues in the complex, and quickly clear the lactoferrin-iron complex in the liver, leading to hypoferricemia. However, research by Lan et al showed that as the quartile of serum iron levels in patients with sepsis increased, a gradual increase in the risk of death at 90 days was observed. Although they stratified the serum iron concentration, they did not report on the overall study of serum iron and the prognosis of patients.25 Therefore, we believe that a decrease in Fe3+ can cause an increase in the mortality of patients with sepsis, and Fe3+ can be used as a diagnostic indicator of poor prognosis in patients with sepsis.
The increase in D-D levels in the body not only reflects the possibility of new thrombosis or thrombus dissolution in the body but also reflects the state of infection in the body. Severe pneumonia, especially pulse toxicosis, is often accompanied by systemic inflammatory reactions and releases a large number of inflammatory mediators. On the one hand, these inflammatory mediators cause vascular endothelial damage and thus initiate the clotting process. On the other hand, when shock occurs, blood fatigue can easily lead to micro-thrombosis. Formed to activate the fibrinolytic system and increase D-D. Studies have found that D-D increases significantly during severe infection, and it can be used as an indicator to evaluate severe pneumonia.26,27 In this study, the concentration of D-D in the death group was higher than that in the survival group, and there was a statistical difference between the two groups (P<0.01); and D-D can be used as an independent prognostic factor in patients with sepsis. Although the AUC of D-D is the largest (70.00%) of all factors, its sensitivity (68.75%) and specificity (60.64) are not the best.
A report in 1975 showed that men are more susceptible to post-traumatic infections.28 Later, more studies have shown that male’s gender and age are the main risk factors for infection and multiple organ failure after trauma and blood loss.29,30 Studies also show that women after traumatic injury, severe blood loss, and sepsis have significantly better prognosis.31,32 However, there are also retrospective analyses showing that female patients with infection or severe sepsis after trauma have a higher mortality rate.33,34 The results of this study show that male patients are more likely to die than female patients. This conclusion is consistent with more research. The reason for the gender difference in death may be that high levels of female sex hormones can reduce the pulmonary inflammation caused by severe blood loss in patients with sepsis, thereby reducing the mortality of patients.
We then superimposed the results of the multivariate analysis to show that the factors affecting sepsis was two-by-two to compare the different predictive values of the factors. The results showed that the AUC and specificity of the PCT+DD combination were the largest (74.80% and 78.23%, respectively), Fe3++DD combination has the highest sensitivity and Youden index (75.89% and 41.35%, respectively). Therefore, we conducted a comparative study on the detection of PCT, D-D, Fe3+ and related inflammatory indicators in the blood of sepsis patients in the survival group and the death group, and showed that the patient’s gender and inflammation related to Fe3+, PCT, ANC, and DD were related markers can be used as independent risk factors affecting the prognosis of patients with sepsis; in the diagnosis of the risk of death in patients with sepsis, the combination of Fe3++ DD has high diagnostic sensitivity, and the combination of PCT + DD has good diagnostic specificity.
Abbreviation
ALC, absolute lymphocyte count; ANC, absolute neutrophil count; DD, D-dimer; Hb, hemoglobin; IF, immunofluorescence; MAP, mean arterial pressure; NLR, neutrophil-to-lymphocyte ratio; PCT, procalcitonin; SF, serum ferritin; SOFA, Sequential Organ Failure Assessment.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was approved and approved by the ethics committee of Beijing Chaoyang Hospital, the informed consent of patients or family members was obtained, and patient information was strictly maintained. All patients provided written informed consent and compliance with the declaration of Helsinki.
Consent for Publication
Not applicable.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
2. Cornell TT, Wynn J, Shanley TP, et al. Mechanisms and regulation of the gene-expression response to sepsis. Pediatrics. 2010;125(6):1248–1258. doi:10.1542/peds.2009-3274
3. Du B, An Y, Kang Y, et al. Characteristics of critically ill patients in ICUs in mainland China. Crit Care Med. 2013;41(1):84–92. doi:10.1097/CCM.0b013e31826a4082
4. Cui N, Zhang H, Chen Z, Yu Z. Prognostic significance of PCT and CRP evaluation for adult ICU patients with sepsis and septic shock: retrospective analysis of 59 cases. J Infect Med Res. 2019;47(4):1573–1579. doi:10.1177/0300060518822404
5. Mewes JC, Pulia MS, Mansour MK, et al. The cost impact of PCT-guided antibiotic stewardship versus usual care for hospitalised patients with suspected sepsis or lower respiratory tract infections in the US: a health economic model analysis. PLoS One. 2019;14(4):e0214222. doi:10.1371/journal.pone.0214222
6. Go H, Nagano N, Katayama D, et al. Diagnostic accuracy of biomarkers for early-onset neonatal bacterial infections: evaluation of serum procalcitonin reference curves. Diagnostics. 2020;10(10):839. doi:10.3390/diagnostics10100839
7. Thorsted A, Nielsen EI, Friberg LE. Pharmacodynamics of immune response biomarkers of interest for evaluation of treatment effects in bacterial infections. Int J Antimicrob Agents. 2020;56(3):106059. doi:10.1016/j.ijantimicag.2020.106059
8. Wang D, Yu S, Zhang Y, et al. Caspase-11-GSDMD pathway is required for serum ferritin secretion in sepsis. Clin Immunol. 2019;205:148–152. doi:10.1016/j.clim.2018.11.005
9. Arcani R, Suchon P, Venton G, et al. Efficacy of intravenous iron therapy in non-anaemic iron-deficient patients with fatigue. Neth J Med. 2020;78(1):34–36.
10. Semeraro F, Ammollo CT, Caironi P, et al. D-dimer corrected for thrombin and plasmin generation is a strong predictor of mortality in patients with sepsis. Blood Transfus. 2020;18(4):304. doi:10.2450/2019.0175-19
11. Semeraro F, Ammollo CT, Caironi P, et al. Low D-dimer levels in sepsis: good or bad? Thromb Res. 2019;174:13–15. doi:10.1016/j.thromres.2018.12.003
12. Köhler J, Maletzki C, Koczan D, et al. The contact system proteases play disparate roles in streptococcal sepsis. haematologica. 2020;105(5):1424–1435. doi:10.3324/haematol.2019.223545
13. Yin S, Huang M, Li D, Tang N. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolysis. 2020;1. doi:10.1007/s11239-020-02105-8
14. Naderpour Z, Momeni M, Vahidi E, et al. Procalcitonin and D-dimer for predicting 28-day-mortality rate and sepsis severity based on SOFA score; a cross-sectional study. Bull Emerg Trauma. 2019;7(4):361. doi:10.29252/beat-070404
15. Shanbhogue L, Paterson N. Effect of sepsis and surgery on trace minerals. J Parenter Enteral Nutr. 1990;14(3):287–289. doi:10.1177/0148607190014003287
16. Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of disease study. Lancet. 2020;395(10219):200–211. doi:10.1016/S0140-6736(19)32989-7
17. Hoeboer SH, Alberts E, Hul IVD, et al. Old and new biomarkers for predicting high and low risk microbial infection in critically ill patients with new onset fever: a case for procalcitonin. J Infect. 2012;64(5):484–493. doi:10.1016/j.jinf.2012.01.002
18. Ramirez P, Garcia MA, Ferrer M, et al. Sequential measurements of procalcitonin levels in diagnosing ventilator-associated pneumonia. Eur Resp J. 2008;31(2):356–362. doi:10.1183/09031936.00086707
19. Wen N, Shi J, Wu J, Yang S. The application of PCT and CRP combined with 16s rRNA in the early diagnosis of neonatal septicemia. Int J Clin Exp Med. 2019;12(11):12861–12867.
20. Suarez-de-la-Rica A, Maseda E, Anillo V, et al. Biomarkers (procalcitonin, c reactive protein, and lactate) as predictors of mortality in surgical patients with complicated intra-abdominal infection. Surg Infect (Larchmt). 2015;16(3):346–351. doi:10.1089/sur.2014.178
21. Assicot M, Bohuon C, Gendrel D, et al. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993;341(8844):515–518. doi:10.1016/0140-6736(93)90277-N
22. Ruan L, Chen GY, Liu Z, et al. The combination of procalcitonin and C-reactive protein or presepsin alone improves the accuracy of diagnosis of neonatal sepsis: a meta-analysis and systematic review. Crit Care. 2018;22(1):1. doi:10.1186/s13054-018-2236-1
23. Miedema KGE, Bont ESJMD, Elferink RFMO, et al. The diagnostic value of CRP, IL-8, PCT, and sTREM-1 in the detection of bacterial infections in pediatric oncology patients with febrile neutropenia. Springer Open Choice. 2011;19:10.
24. Clarke AJ, Jacques TS, Galloway M, et al. ALK positive inflammatory myofibroblastic tumour of the pineal region. J Clin Pathol. 2005;58(9):981. doi:10.1136/jcp.2004.022947
25. Lan P, Pan KH, Wang SJ, et al. High serum iron level is associated with increased mortality in patients with sepsis. Sci Rep. 2018;8(1):1–7. doi:10.1038/s41598-018-29353-2
26. Schutte T, Thijs A, Smulders Y. Never ignore extremely elevated D-dimer levels: they are specific for serious illness. Neth J Med. 2016;74(10):443–448.
27. Wada Y, Kuzuhara A, Hanamura M, et al. Role of selectins on IgE-mediated skin reaction. Br J Pharmacol. 2000;131(8):1531–1536. doi:10.1038/sj.bjp.0703739
28. McGowan JE, Barnes MW, Finland M. Bacteremia at Boston City Hospital: occurrence and mortality during 12 selected years (1935–1972), with special reference to hospital-acquired cases. J Infect Dis. 1975;132(3):316–335. doi:10.1093/infdis/132.3.316
29. George RL, McGwin G, Windham ST, et al. Age-related gender differential in outcome after blunt or penetrating trauma. Shock. 2003;19(1):28–32. doi:10.1097/00024382-200301000-00006
30. Kher A, Wang M, Tsai BM, et al. Sex differences in the myocardial inflammatory response to acute injury. Shock. 2005;23(1):1–10. doi:10.1097/01.shk.0000148055.12387.15
31. Gannon CJ, Pasquale M, Tracy JK, McCarter RJ, Napolitano LM. Male gender is associated with increased risk for postinjury pneumonia. Shock. 2004;21(5):410–414. doi:10.1097/00024382-200405000-00003
32. George RL, McGwin G, Metzger J, et al. The association between gender and mortality among trauma patients as modified by age. J Trauma Acute Care Surg. 2003;54(3):464–471. doi:10.1097/01.TA.0000051939.95039.E6
33. Eachempati SR. Gender-based differences in outcome in patients with sepsis. Arch Surg. 1999;134(12):1342–1347. doi:10.1001/archsurg.134.12.1342
34. Sakr Y, Elia C, Mascia L, et al. The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care. 2013;17(2):R50. doi:10.1186/cc12570
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.