Back to Journals » Patient Preference and Adherence » Volume 14
The Development of a New Questionnaire to Measure the Burden of Immunoglobulin Treatment in Patients with Primary Immunodeficiencies: The IgBoT-35
Authors Jones GL, Williams K , Edmondson-Jones M, Prevot J, Drabwell J, Solis L, Shrimpton A, Mahlaoui N
Received 15 October 2019
Accepted for publication 12 June 2020
Published 3 September 2020 Volume 2020:14 Pages 1567—1584
DOI https://doi.org/10.2147/PPA.S234669
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Georgina L Jones,1 Kate Williams,2 Mark Edmondson-Jones,2 Johan Prevot,3 Jose Drabwell,3 Leire Solis,3 Anna Shrimpton,4 Nizar Mahlaoui5– 7
1Department of Psychology, School of Social Sciences, Leeds Beckett University, Leeds, UK; 2PAREXEL International, London, UK; 3International Patient Organisation for Primary Immunodeficiencies, Downderry, Cornwall PL11 3LY, UK; 4Clinical Immunology and Allergy Unit, Northern General Hospital, Sheffield Teaching Hospitals and NHS Foundation Trust, Sheffield, UK; 5French National Reference Center for Primary Immune Deficiencies (CEREDIH), Necker Enfants Malades University Hospital, Assistance Publique-Hôpitaux De Paris, Paris, France; 6Pediatric Immuno-Haematology and Rheumatology Unit, Necker Enfants Malades University Hospital, Assistance Publique-Hôpitaux De Paris, Paris, France; 7IPOPI Medical Advisory Board, Chair
Correspondence: Georgina L Jones
Department of Psychology, School of Social Sciences, Leeds Beckett University, Calverley Building, City Campus, Leeds, UK
Tel +44 113 8125106
Email [email protected]
Purpose: To describe the development and psychometric testing of a new questionnaire to measure the burden of immunoglobulin treatment (Ig) from the perspective of patients with primary immunodeficiencies (PID).
Patients and Methods: An online, cross-sectional survey was administered to PID patients across 10 countries (nine European and Canada) who were receiving either intravenous (IVIg) or subcutaneous (SCIg) immunoglobulin therapy. The range and distribution of the responses (ie, levels of missing data, floor and ceiling effects), exploratory factor analysis (using factor loadings of 0.4 or greater) and measures of internal consistency reliability (ie, Cronbach’s alpha coefficient, inter-item and item-total correlations) were used to identify the domain and item pool.
Results: In total, 472 patients completed the questionnaire, of which 395 were included in the analysis (32% underwent IVIg and 67% underwent SCIg). The final instrument contained 34 items across eight domains of treatment burden (time, organisation and planning, leisure and social, interpersonal relationships, employment and education, travel, consequences of treatment and emotional) and an additional Ig treatment burden global question at the end of the measure. All the scales achieved good internal reliability (Cronbach’s alpha coefficient ranged from 0.70 to 0.85) and, with the exception of one item exceeded the minimum threshold of 0.35 for item-total correlations. Treatment burden was lower than anticipated across the different treatment routes and countries, although overall was more burdensome for patients undergoing IVIg compared to SCIg treatment.
Conclusion: The IgBoT-35 appears to be a reliable, patient-generated questionnaire and may help to identify more individualised and preferred therapies for the PID patient when used in clinical practice. A new survey with a sample of US patients is currently being undertaken to further establish its validity and conceptual model. The overall Ig burden of treatment scores appeared to be low. PID patient preferences are important to guide treatment decisions and ensuring patients receive the right treatment at the right time.
Keywords: intravenous immunoglobulins, subcutaneous immunoglobulins, primary immunodeficiency, treatment burden, patient preference, quality of life
Plain Language Summary
In an age where minimally disruptive medicine is a key goal of healthcare delivery, it is important to identify any potential treatment burden from the patient’s perspective. The IgBoT-35 is a new questionnaire for people living with a primary immunodeficiency (PID) to self-report the burden of receiving immunoglobulin treatment. Patients' burden of immunoglobulin therapy may vary based on clinical and demographic characteristics, and patient preferences of treatment options including modes of administration, frequency, duration and experience. To develop the IgBoT-35, 395 patients from 10 countries (nine European and Canada) and undergoing either subcutaneous (67%) or intravenous (32%) administration completed an online survey. Psychometric tests were undertaken to identify the questionnaire’s final item pool and domain structure. This analysis identified eight areas of treatment burden: Time, Organisation and Planning, Leisure and Social, Interpersonal Relationships, Employment and Education, Travel, Consequences of Treatment, and Emotional. A question concerning patient’s perceived overall Ig treatment burden was also included. Although treatment burden was worse for patients undergoing intravenous compared to subcutaneous administration, it was generally lower than anticipated across the different treatment routes and countries. The IgBoT-35 provides a measure of Ig treatment burden from the patient’s perspective, for use in research or clinical practice. It is already translated and usable in the aforementioned 10 countries. Ig treatment burden appears generally low, potentially proving reassuring forPID patients facing subcutaneous and intravenous choices. IgBoT-35 data may help deliver more individualised and preferred therapies especially where non-adherence or poor satisfaction with Ig therapy is observed.
Introduction
Burden of treatment can be defined as the consequences of receiving treatment (these may be medication, therapies or other interventions).1,3 It describes the “work of being a patient” – everything the patient needs to do to treat and manage their illness, for example, undergoing tests and investigations, visiting doctors, adhering to treatment regimens and making lifestyle changes.4 It therefore helps us understand variations in healthcare utilization and adherence in different healthcare settings and clinical contexts.2 Burden of treatment is an important concept because it may negatively affect adherence to treatment, quality of life, disease management and healthcare outcomes such as hospitalisations and survival.5,6
One condition where treatment burden may be high is in primary immunodeficiency disorders (PIDs). These occur when the body’s immune response is impaired or absent which leads to increased susceptibility to infections. PIDs are caused by hereditary or genetic factors and represent a group of over 400 disorders with some occurring as often as one per 1,200–2,000 individuals.7 However, the disorders are generally defined as rare with some only occurring in one per million individuals.
Patients with PIDs need to monitor their health carefully and should take precautions to avoid infections, including maintaining personal hygiene, having a nutritious diet, and not smoking. Modern PID treatments help patients to live longer and healthier lives than before. Treatment depends on the type of PID but options include immunoglobulin (Ig) replacement therapy, granulocyte-colony stimulating factor, gamma interferon, polyethylene glycol-modified adenosine deaminase, stem cell transplantation, and gene therapy among others, these last two being curative, which is not the case of Ig replacement therapy which is a chronic lifelong supportive treatment.
However, Ig replacement therapy is the main treatment for most patients with antibody deficiencies and it can be administered either intravenously (directly into a vein) or subcutaneously (directly under the skin). Whilst it is generally accepted that this treatment can dramatically improve quality of life8,9 it may also be associated with a substantial treatment burden. Intravenous Ig treatment (IVIg) is generally administered in hospital and can be infused every two, three or four weeks lasting approximately two to four hours per visit. The precise length of infusion, however, will be dependent on dose and tolerance of the individual. Subcutaneous Ig treatment (SCIg) is typically administered in the home once a week or more frequently but can be administered in the hospital depending on patients’ individual needs.
Whilst there are numerous studies which have tried to measure the quality of life of patients with a PID,8,10 less attention has focused upon the burden of Ig treatment. The results of a recent systematic review to explore burden of Ig treatment in patients with PID revealed that ten different “health” questionnaires had been used to measure treatment burden.11 Most notable of these were the Life Quality Index (LQI) or a slightly modified version12,16 which is a condition-specific instrument developed specifically to measure IVIg treatment satisfaction for patients with a PID, and the Treatment Satisfaction Medication Questionnaire (TSMQ),17,18 which is a generic instrument that measures a patient’s satisfaction with treatment. Several other generic burden of treatment measures exists; however, none of these have been used in patients with a PID undergoing Ig treatment. This heterogeneity of different measures, subsequently measuring different outcomes does not enable direct comparison of Ig treatment-related burden to be easily quantified. A new Ig burden of treatment specific measure may therefore prove a useful measure for standardising the measurement of Ig treatment burden across future studies and as newer Ig therapies and modalities are developed.
The FDA has published guidance for the development of patient-reported outcome measures, especially those to be used in clinical trials.19 This describes an iterative process which has been adhered to as closely as possible during the development of the IgBoT questionnaire. The process of developing this new measure has also involved collaborations between an international team involving academic, industry and patient partners.
The development of the questionnaire involved four stages. Stage 1 involved a systematic review of the existing literature to understand what the burden of Ig therapy may be in adult patients with primary immunodeficiencies.11 This review identified the studies that measured the burden of Ig treatments on adult patients (aged 16 years and older) with primary immunodeficiencies (PID) and appraised and synthesised this evidence in relation to the different modes of Ig administration available and the instruments used. In Stage 2, semi-structured interviews with 30 patients diagnosed with a PID attending the Clinical Immunology and Allergy Unit (CIAU) in Yorkshire, UK, were undertaken (Jones et al 2020 under review). Patients receiving IVIg and SCIg at home or in hospital were included. An inductive [data-driven] thematic analysis approach was taken to prioritise patient accounts/concerns and identify the key concepts and themes.20
This resulted in a 112-item measure. A further 18 items were added based upon the findings from the International literature generated as part of stage 1 around Ig treatment burden. In stage 3, the face validity of the preliminary questionnaire was undertaken with an additional 14 patients with PID (who did not take part in the qualitative interviews) to understand patient’s perceptions of the item pool and response categories chosen. These were also recruited via the CIAU but they were not involved in the qualitative interviews. The 10-item QQ-10 was used to collect information on the patient’s views on the new tool.21 The QQ-10 is a measure of face validity, acceptability and utility of questionnaire use from the patient’s perspective and has been used in previous studies. In addition, a standard proforma consisting of 10 items was used to ask patients to comment on: 1) How they found the questionnaire generally, 2) Ease of use, 3) Content, 4) Language, 5) Relevance and 6) Missing items or areas not covered. Telephone and face to face meetings were also held with the large academic, clinical and PPI team to check the suitability and relevance of the item pool. This face validity exercise resulted in an initial 129-item questionnaire.
The aim of this study is to report on stage 4 of the developmental process. It involved undertaking a large patient survey using the questionnaire generated in stage 3 to i) reduce the length of the questionnaire, and identify the salient domains of Ig treatment burden and the scoring system of the resulting new shorter measure whilst also ii) using this shorter measure to explore if the burden of treatment varies according to the route of Ig administration, by country of residence that took part and by the age and gender of the patient groups.
Patients and Methods
Design
A 151-item questionnaire was administered in an online, cross-sectional survey across 10 countries. The 151 items comprise 1) the 129-item questionnaire generated in stage 3, 2) 18 demographic, PID and treatment-related questions and 3) four “dummy items” which were also included to check the scoring patterns of patient’s completing the questionnaire.
Recruitment and Data Collection
The 10 countries included nine European countries (United Kingdom, France, Germany, Italy, Poland, Sweden, Denmark, Norway and the Netherlands), and Canada. The survey was entered online using Survey Monkey. Ethical permissions were obtained from the Independent Ethics Committee (IEC) and the Institutional Review Board (IRB) according to national and international regulations where appropriate. These included: Germany (Uniklinik Freiburg Ethik komission), Canada (Schulman IRB), Norway (Regional Ethics Committee for South-Eastern Norway), UK (South East UK NHS Ethics Committee), and Italy (La segreteria del Comitato Etico, Università Federico II). For the Netherlands, France, Sweden, Poland and Denmark a detailed review of this study by an independent ethics board was not mandated by national nor regional guidelines.
Data collection only began in each country after acquisition of a written approval or favourable ethical opinion was obtained.
Translation and Linguistic Validation
The surveys were translated on the paper version and linguistically validated with the support of Mapi in accordance with the guidance of the ISPOR task force for translation and cultural adaptation.22 The translation procedure included the following steps: i) Conceptual analysis and definition, ii) Two forward and one backward translation, and iii) Cognitive debrief interviews with five PID patients in each study country. Following migration to Survey Monkey, all screens were also checked for accuracy of translation.
Sample Size
It was anticipated that considering a three to one item to respondent ratio as recommended, a sample size of 400 would be sufficient to undertake the factor analysis of the 129 items reported below. This was also thought to be sufficient as generally, a sample size of >300 is considered adequate.23
Recruitment
In order to achieve an approximate sample size of 400 patients, 450 patients were identified. Patients were invited to participate in the study by IPOPI and local national member organisations (NMOs) if they met the following inclusion criteria: they were 18 years of age and older and were currently receiving Ig therapy. The treatment had to be delivered at home or at the hospital and via the intravenous or subcutaneous route based on a medical or joint medical-patient decision. The administration route and location of where the infusion should be given was already done before the patient would decide on whether to take part in the survey.
IPOPI first contacted the study country NMOs in order to create awareness of the study and determine estimates for the number of eligible patients in each of the four groups (IVIg hospital/home or SCIg hospital/home). IPOPI collaborated with the NMOs to promote the study to doctors, the International Nursing Group for Immunodeficiencies (INGID), and national nursing associations. They also promoted the study using a variety of media, including articles, websites, social media, and/or brochures and requested that the NMOs communicated details of the study via their websites, newsletters, or social media. All advertising media was also submitted to the ethics committees for approval.
The NMOs were asked to perform the following: i) Identify and contact eligible patients to introduce the study and invite them to take part, ii) send interested and eligible patients an email containing a link to the online survey in their local language – this link also contained a unique country-specific identification number (created by PAREXEL). Only the NMO knew which identification number corresponded to which eligible patient (contact details) but did not have access to the answers provided by the patient to the survey, iii) assign interested and eligible patients with a unique country-specific identification number (provided to the NMO by PAREXEL). If the patient later consented to be contacted for follow-up questions about their survey responses, the NMOs could then use the identification number to identify them, and iv) provide PAREXEL with details of the number of interested and eligible patients who have been sent a link to the survey and their unique identification numbers. No identifiable data were collected from patients by PAREXEL, sponsor or the academic institutions and no details that the NMOs had collected during this process were shared with PAREXEL, the sponsor or the academic institutions involved in this research. Also, the NMO did not have access to the information provided by the patients to the survey, this information was only accessible by PAREXEL and linked to the unique country-specific identification number.
Recruitment was monitored to ensure patients were equally represented in each of the following groups: IVIg in hospital, IVIg at home, SCIg in hospital and SCIg at home. Study participants could withdraw from the study at any time by not completing the questionnaire or by requesting withdrawal from their NMO contact. If patients decided to withdraw, no new data were collected from them and they were not contacted again. However, the anonymous data collected before their withdrawal would still be used in analyses, reports, conference presentations, and academic journal publications.
Statistical Analyses
The data file was originally received in Excel. This was converted to SPSS v22. On SurveyMonkey, most of the 133 questionnaire items suitable for the psychometric analysis (the 129 items + the four dummy items) used a Verbal Rating Scale ranging between 1 = Never, 2 = Rarely, 3 = Sometimes, 4 = Often and 5 = Always. A small subset of items also included an additional “Not Applicable” response category (coded as 6). For the purposes of this analyses, the data were recoded from 0 to 5 (5 = Not Applicable) to support an eventual scoring algorithm of 0–100 (in line with most questionnaires). Only patients that gave consent to use their survey data were included in the final analysis.
Exploratory factor analysis (EFA), a method of classical test construction, was carried out which included the “not relevant” responses in the procedure. EFA is a statistical procedure which enables the underlying dimensions of an instrument to be estimated. It simplifies complicated sets of data into factors using methods such as principal component analysis (PCA), which is a technique used to reduce a large number of items on a questionnaire into a smaller number of dimensions by analysing the correlations between the individual items. Each factor that is produced is therefore an indication of the relationships between a set of variables.24 PCA using varimax rotation (orthogonal rotation), which attempts to identify interpretable dimensions was used. To test the adequacy of the sample size for undertaking factor analysis, the Kaiser Meyer-Olkin and Bartlett’s Test of Sphericity values were calculated. Values of 0.5 or greater and p<0.0001 are recommended, respectively.25
To extract the factors, corresponding eigenvalues greater than 1, scree plots and minimum factor loadings of 0.40 were selected.23,26 The following tests were also used to examine the domain structure and item pool of the instrument. Cronbach’s alpha reliability coefficient is the measure which is most frequently used for establishing the internal consistency reliability of a questionnaire (ie, the extent to which items within a scale are associated with each other or the homogeneity of the items) and was calculated in this study.27 Many different views have been expressed regarding what the minimum reliability coefficient should be for indicating the internal consistency reliability of a test. For example, Helmstadter28 postulated that a co-efficient of 0.5 or more was satisfactory whereas Carmines & Zeller29 and Streiner & Norman30 advocated that the alpha co-efficient of a scale should ideally exceed 0.8. However, in practice, an alpha value of 0.7 or more as proposed by Nunnally31 is most commonly accepted.30
Levels of missing data, floor and ceiling effects (ie, the percentage of patients who score at the bottom and the top of the scales), inter-item correlations, missing data and item-total correlations were also explored which follows good methodological guidelines for the development of questionnaires. The following thresholds were adopted as reasons for possible item redundancy: missing data at item level >5%;32 floor and ceiling effects >45% and/or a treatment ceiling of the “not applicable” answers exceeding 50% and inter-item correlations >0.3.33 Fifty percent of inter-item correlations also had to fall within the range 0.30 to 0.70.34
Item-total correlations can also be calculated to check the internal consistency reliability of a dimension. This is the extent to which there is a linear relationship between an item and its scale score which has been corrected for overlap.35 To correct for overlap the item which is to be correlated with the scale is omitted from the scale total. Recommended thresholds can vary between 0.25,32 0.3036 and 0.40 or more.33,37 For the purposes of this study, and given the large number of items that were included in the survey, a conservative correlation co-efficient estimate in between these values of 0.35 was adopted for indicating satisfactory item-total correlation. The methods employed were described in the study protocol (v1.4).
Following this analysis, the domain scores were then calculated. This was computed by summing the scores for each item in the domain, then dividing by the maximum score possible for the domain, and then multiplying by 100 to convert the domain score onto a scale of 0–100 (0 = no Ig treatment burden, 100 = maximum Ig treatment burden). Descriptive statistics (eg, means, medians, standard deviations, minimum and maximum values, interquartile ranges and 95% confidence intervals were then calculated for the sample as a whole and by country of completion. Finally, t-tests with Bonferroni correction were undertaken to see if there were any significant differences between the mean domain scores of those receiving IVIg compared to SCIg, males compared to females and those aged ±60 years old and an analysis of variance (ANOVA) with Bonferroni correction was undertaken to explore if domain scores varied significantly by country. Based on the availability of domain scores from nine countries, we estimated a Bonferroni corrected p-value of 0.005 to indicate statistically significant variation in domain score values by country.
Results
Four hundred and seventy-two patients started the questionnaire. However, of these 72 patients did not complete the question giving their consent to use the data, two patients had a duplicate ID and a further three did not give a treatment location. Therefore, a total of 395 questionnaires were eligible for inclusion in the analysis (83.7%) (Figure 1).
 |
Figure 1 Flowchart to show patient completion of the online survey. |
The demographics of the patient sample are shown in Table 1. With the exception of one patient whose Ig treatment was not reported, most patients were receiving SCIg treatment (266; 67%) compared to IVIg treatment (128; 32%) and more females (247; 63%) participated compared to males (147; 37%). The mean age of the sample was 45.9 years (sd=14.6; median=46.0; IQR=35.0–57.0). In terms of employment, most patients worked full-time (136; 35%); compared to part-time (63; 16%). The remainder reported their employment status as disabled (64; 16%); retired (63; 16%); student (31; 8%); self-employed (21; 5%); homemaker (6; 2%); unemployed (9; 2%); and missing (2; 1%). Clinical and Ig treatment characteristics are reported in Table 2.
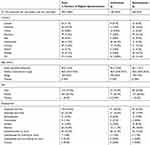 |
Table 1 Patient Characteristics by Ig Treatment Group |
 |
Table 2 Clinical Characteristics by Treatment Route |
Prior to undertaking the analyses, levels of missing data, floor and ceiling effects and answers to the not applicable questions were explored. From this analysis, 71 items were removed because they exceeded the minimum thresholds. However, although four items exceeded the 45% cut-off for floor and ceiling effects ie, “labour intensive”, “other illness worries”, “an unexpected reaction” and “time worries” because these were considered conceptually important based upon team meetings and the themes actively generated from the qualitative interviews they were kept in at this stage.
Following this only one dummy question remained which was also removed (“felt negative about my treatment”) because after checking the pattern of scoring with its twin question, the pattern of scoring was in the appropriate direction. The overall Ig burden item was also excluded. Given that most of the positively worded items had been removed, it was decided to also remove the remaining seven positively phrased items to avoid the complexities of possible recoding and interpreting negative correlations for potential users of the new measure in the future. Therefore, a total of 80 items were excluded leaving 53 items that were used in the first round of factor analysis. Following discussions within the clinical and statistical team, for the purposes of the factor analysis, those patients that answered “not applicable” to any item were recoded to 0 meaning “never”, rather than designated missing from the dataset. This was because the wording of the questions was such that a response of burden being “not applicable” was semantically comparable with an item “never” being burdensome.
An initial factor analysis was undertaken on the 395-patient sample. In the first instance, multicollinearity was explored to check which items did not appear to be correlated with any other variables or correlated too highly. After reviewing the correlation matrix, it was decided to remove a further two items (swelling and tight skin) because they appeared to be negatively correlated with many of the items. The analysis was then run again. Having removed these items, the Kaiser-Meyer Olkin value was 0.927 and the Bartlett’s test of Sphericity was significant (p<0.0001), thus indicating that the sample size was adequate.
From the data, 11 factors were extracted accounting for 63% of the variability in the data. However, only the first nine appeared meaningful accounting for 58% of the variability. These nine factors appeared to measure 1) time and organisational and planning burden (9 items), 2) leisure and social activities burden (6 items), 4) emotional burden (5 items), 5) travel burden (5 items), 7) interpersonal relationships and activities (6 items), 8) employment and education burden (3 items), and factors 3, 6 and 9 related to psychological consequences and physical consequences (eg, side effects) of treatment (11 items). Two items failed to load significantly within these nine factors (insurance and others understanding what going through) and so were omitted from the analysis.
It was decided that the first factor would be best separated into two domains. In the emotional burden domain, conceptually one item (“others worry”) was felt not to fit and so was removed from the analysis. Some additional potential items were also removed at this stage based upon conceptual reasoning (ie, considering the information generated from the systematic review and qualitative interviews). This resulted in a 34-item questionnaire, with eight domains plus an additional item relating to “global Ig treatment burden” which falls outside of the scored domains (Table 3).
 |
Table 3 Domain Structure, Item Pool and Reliability of the Domains Generated from the Exploratory Factor Analysis |
PCA was repeated on these 34 items and seven meaningful factors were identified which accounted for 61.7% of the variance. There was no change to the planned domain structure as described above (Table 3). All the inter-item correlations were positive, suggesting that the items are measuring the same underlying constructs, and 97% of the inter-item correlations fell within the range 0.30 to 0.70 (Nunnally, 1994). In addition, all the alpha values exceeded the minimum threshold of 0.70 suggesting acceptable levels for each of the domains (Table 3).
The purpose of the proposed IgBoT-35 instrument is to indicate the extent of self-reported Ig treatment burden on each item and domain measured. The raw scores for each IgBoT-35 item are reported in Table 4. Each scale was then standardised on a scale of 0–100. Scale scores for the sample overall are shown in Table 5. Descriptive statistics of the IgBoT-35 mean scores by country have been provided in graphical (Figure S1–9) and tabular form (Table S1).
 |
Table 4 Raw Data of the IgBoT-35 Items |
 |
Table 5 Mean Domain Scores for the IgBoT-35 for the Total Patient Sample |
For the overall sample overall, treatment burden appeared to be generally low across each item (Table 4) and domain (Table 5). Whilst the time burden was generally low across all countries, it was highest in France (mean: 45.4) and lowest in Sweden (mean: 21.5). Organisation and planning burden was low across all countries. It was highest in France (mean: 33.8) and lowest in Germany (mean: 16.9). Leisure/social burden was low across all countries. It was highest in France (mean: 51.4) and lowest in Norway (mean: 23.0). Interpersonal relationship burden was low across all countries. It was highest in France (mean: 40.2) and lowest in Italy (mean: 14.2). Employment and education burden was low across all countries. It was highest in France (mean: 39.5) and lowest in Sweden (mean: 9.2). Travel burden was low across all countries. It was highest in Poland (mean: 28.8) and lowest in Denmark (mean: 8.9). Consequences of treatment burden was low across all countries. It was highest in France (mean: 35.6) and lowest in Germany (mean: 23.3). Finally, the single item “Global Ig treatment burden” was low across all countries. It was highest in France (mean: 54.5) and lowest in Italy (mean: 24.1) (Figure S1–9 and Table S1). One-way ANOVA to test for differences in domain values between countries revealed that none were Bonferroni-significant (Tables S2–10).
In relation to Ig treatment route, burden was low across both IVIg and SCIg (Table 6). Despite this, with the exception of the emotional well-being domain, treatment burden was observed to be higher for those receiving IVIg compared to SCIg therapy, particularly in the three areas of leisure/social activities, interpersonal relationship, employment and education, and travel (P<0.005). Generally, mean IgBoT-35 domain scores were higher for women than men with the exception of the leisure/social domain and the employment and education domain, and significantly higher for women in the consequences of treatment domain (P<0.005). However, overall these differences were very small (eg, less than 3 points on some scales) (Table 7). In terms of age, the sample was categorised into those younger and older than 60 (Table 8). For all domains, mean IgBoT scores were higher in those aged younger than 60 years of age compared to those aged older than this and significantly worse in the time, interpersonal relationships, employment and education and emotional burden domains (P<0.005). Whilst overall the mean burden scores were generally lower than anticipated, they were worse for those on hospital compared to home treatment and significantly worse on the leisure and social, education and employment and travel domains (P<0.005) (Table 9).
 |
Table 6 Domain Summary Statistics by Administration Route (IVIG/SCIG) |
 |
Table 7 Domain Summary Statistics by Gender (Female/Male) |
 |
Table 8 Domain Summary Statistics by Age Group (<60/≥60) |
 |
Table 9 IgBoT-35 Domain Values by Location (Home versus Hospital Treatment) |
Discussion
The aim of this study was to develop the first Ig patient-generated burden of treatment questionnaire for patients living with a PID and to start to quantify the perceived impact of Ig treatment from PID patients receiving this therapy across Europe and Canada.
The psychometric analysis resulted in a questionnaire comprising eight domains and 34 items which covered various aspects of Ig related treatment burden: time (4 items), organisation and planning (5 items), leisure and social (5 items), interpersonal relationships (3 items), employment and education (3 items), travel (5 items), consequences of treatment (6 items), and emotional (3 items). Lastly, an additional Ig treatment burden global question was included at the end of the measure (n=35 items in total). The internal reliability of the questionnaire was high with all the scales exceeding the accepted alpha value of 0.70 for comparisons at a group level. The questionnaire also demonstrated acceptable levels of inter-item correlations and item-total correlations.
The dimensions produced on the questionnaire reflect the many areas of treatment burden that patients undergoing Ig therapy may experience. The finding that treatment burden was generally low across the different treatment routes and countries is supported by recent evidence generated from a systematic review of the international literature on Ig treatment burden for patients with a PID10 and a smaller, in-depth qualitative study to explore the concerns of 30 patients in the UK support this finding too (Jones et al, under peer review).
Whilst the treatment burden was lower than anticipated, the analysis by route of administration revealed higher scores (higher burden) in patients receiving intravenous therapy in all domains (including leisure and social, interpersonal, travel and education), the only exception was on the emotional burden domain. Similar findings have been observed in other published studies.11 However, further research is needed to determine if these differences in scores as measured on the new questionnaire are replicated and to explore what other factors may be driving these differences.
The finding that those aged under 60 reported more Ig treatment-related burden is perhaps not surprising, given that this cohort of patients are more likely to be in employment and have younger families, school and education commitments to organise their Ig therapy around. However, further work to explore age-related Ig treatment impacts is needed to understand, for instance, the impact of receiving Ig as a lifelong treatment. Overall, women reported more Ig burden across all the domains and on the global single item compared to their male counterparts with the exception of the leisure and social domain and employment and education domains. However, given that the differences across the domains overall were very small, more work is needed to explore these possible gender differences further.
In terms of psychometric robustness, the English version of the instrument was generated from qualitative work with UK patients, a systematic review and expert feedback and internal peer review with members of the international study team thus supporting the content validity of the measure. Face validity was also demonstrated in a smaller survey with UK patients reported elsewhere. Whilst this survey has substantially reduced the questionnaire, identified the domain structure, scoring algorithms and aspects of reliability, based upon the FDA guidance for the development of PROMS, there are still a number of other psychometric analyses to undertake.19 Therefore, a second online survey with patients undergoing Ig therapy in the US is currently being undertaken using this shorter measure. This study will be used to test the current model of the IgBoT-35 and reduce it further if appropriate. The data will also be used to evaluate the other psychometric properties of the questionnaire which are currently un-determined, such as aspects of construct and criterion validity using “a priori” hypotheses developed by the team. A comparison of the mean treatment scores are also planned to see if the levels of Ig treatment burden observed from this first survey are similar to those reported by patients in the US.
Limitations
There were some limitations to the study. Due to the need to translate the questionnaire into nine different languages, the format of some of the items changed based upon the outcome of the cognitive interviewing. The most important change was that on the initial paper version of the instrument, it was only planned to have the header question “because of my current Ig treatment, I have ….” at the top of each page. However, due to the nature of SurveyMonkey, this was changed so that this header was used at the start of each item. This made some of the items long and more challenging to read, for example, “because of my current Ig treatment, I have found that my Ig treatment takes up too much time.”
Given the extent of item reduction that was needed with this first survey, item reduction was undertaken cautiously and there is potentially scope for some more item redundancy. There may also be problems with the “consequence of treatment” domain as some of these items cross-loaded but this will be explored further in the new data set before confirming the final domain structure. It may be that this domain will be shortened or removed depending on the results from the next set of analyses.
The whole questionnaire (including the demographic and IgBoT questions) that was entered onto SurveyMonkey was long and included 151 items. There was evidence of questionnaire fatigue because missing data was more evident towards the end of the questionnaire but unfortunately, we did not record completion times. Ideally, more time and opportunity to validate the different language versions of the questionnaire prior to being migrated from the paper to electronic version would have been beneficial (beyond the five patients per country used by MAPI who undertook cognitive debrief interviews on the paper version before it was uploaded). However, the time frames for delivery of the study meant that a fuller in-depth cognitive interviewing and face validity exercise could not be undertaken.
Unfortunately, we do not know the lapse of time between the administration of the questionnaire and the administration of immunoglobulin. It is possible that proximity to receiving Ig treatment may have influenced the “severity” of participants responses. Everyone who participated was currently receiving Ig treatment at the time of survey completion and we have reported the mean, median and range for the amount of years spent on Ig therapy.
It was not possible for us to achieve the sample size needed to undertake the psychometric tests (in the study timeframe) without widening recruitment beyond the UK to include the additional nine countries. However, the sample size of patients for each country (eg, average 12 IV respondents per country) may not sufficiently reflect the whole population and we cannot exclude the role of recruitment bias in our findings. Firstly, it is possible that if we had recruited Ig participants via other means (eg, directly from hospitals rather than from the membership of local patient organisations), then differences in treatment burden may be observed, although it is currently unclear how membership of a patient organisation would affect the burden of treatment (eg, the need to travel to hospital).
Secondly, it was not possible to mitigate possible bias between countries. However, everyone included met the same inclusion and exclusion criteria and whilst there were some differences in the observed IgBoT-35 domain values by country, none were significant.
Despite these limitations, the study has resulted in the largest PID survey ever conducted across Europe and Canada to date and, whilst further validation and psychometric testing is required, it has also generated the first-ever Ig specific burden of treatment measure for this patient group, which is already translated and ready to use across 10 countries. Our research has also started to identify where possible Ig treatment burden may be present, and whilst further research is needed, our findings may help facilitate more personalised and minimally disruptive treatment for the PID patient which is a key goal of healthcare delivery. This international survey would not have been possible without the involvement of a combined and multidisciplinary team (comprising academic, industry, and PPI partners) and in particular the support of IPOPI and its NMOs to encourage and support recruitment. This information may be helpful to other teams seeking to undertake cross-cultural research in the field of patient-reported outcome measurement which is increasingly desired.
Conclusion
The IgBoT-35 appears to be a reliable, patient-generated questionnaire. A further survey is currently being undertaken in a new sample of US patients to test the conceptual model of the measure and undertake further tests of reliability and validity. Overall, treatment burden from both IVIg and SCIg appears lower than expected which is reassuring for both PID patients and their clinical teams. However, individual differences such as age and gender appeared to affect treatment burden and intravenous delivery of Ig may seem to have a bigger impact on patients’ work, social and leisure aspects. Therefore, ensuring the patient has the possibility of choosing the administration route of their treatment in collaboration with their treating physician is warranted to ensure that the treatment has the lesser impact on the patient’s daily life. The IgBoT-35 questionnaire, when used in research and clinical practice may help to better understand the support needs of PID patients facing Ig treatment choices and identify the ways in which Ig treatment modality is impacting upon the patient’s lives. This should enable the most appropriate personalized Ig treatment plan to be implemented more quickly, thus minimising the treatment burden for the PID patient.
Data Sharing Statement
The datasets generated during and/or analysed during the current study are not publicly available because they contain information that could compromise research participant privacy/consent. However, some data may be available from the corresponding author on reasonable request.
Acknowledgments
We are grateful to i) all the patients who gave their time to take part in this research, ii) Professor John Brazier for his contribution to the development of the study protocol, iii) Mia Malmenas from PAREXEL and Teresa Kauf formerly from Shire, a Takeda company for their support and contribution to the development and delivery of this study, iv) Dr Betschel, Dr Whitney Goulstone, Dr Børre Fevang, Dr Martin Van Hagen, Dr Martin Buckland, and Prof Claudio Pignata for their assistance with our ethics committee applications. The abstract of this paper was presented at the Advances in Patient Reported Outcomes: Integration and Innovation Conference, Leeds, UK, 13th June 2019 as an oral presentation with interim findings. The abstract has been published in the Journal of Patient-Reported Outcomes 2020, 4(Suppl 1):28.
Disclosure
GLJ has received a research grant from Baxalta US to undertake this work and received financial remuneration to attend two travel meetings to London as part of this studyand a grant from SHIRE outside the submitted work. KW and MEJ received financial remuneration to undertake some of the data analysis. JP and LS are staff members and JD is a Board member of IPOPI. IPOPI has previously received unrestricted grants from BAXALTA/SHIRE in support of IPOPI’s activities, outside the scope of the study. NM has received unrestricted education grants from BAXALTA FRANCE and then SHIRE FRANCE to support the research activities of the French National Reference Center for PID (CEREDIH). He also received financial remuneration for travel to speak at the SHIRE International Symposium in 2017 and an honorarium for speaking at this symposium. Ms Leire Solis reports grants provided from Takeda, during the conduct of the study; grants from Takeda, grants from CSL Behring, grants from Grifols, grants from Kedrion, grants from Octapharma, grants from Biotest, grants from LFB, grants from NBI, grants from PPTA, grants from RMS Medical Products, grants from KANE SpA, grants from ConvaTec, outside the submitted work. Mr Johan Prevot reports grants from Takeda, during the conduct of the study; grants from Takeda, grants from CSL Behring, grants from Grifols, grants from Kedrion, grants from Octapharma, grants from Biotest, grants from LFB, grants from NBI, grants from PPTA, grants from RMS Medical Products, grants from Cane SpA, grants from ConvaTec, outside the submitted work. Mrs Jose Drabwell reports grants provided to IPOPI from TAKEDA, during the conduct of the study; grants from CSL BEHRING, grants from GRIFOLS, grants from KEDRION, grants from OCTAPHARMA, grants from BIOTEST, grants from LFB, grants from NBI, grants from PPTA, grants from RMS MEDICAL PRODUCTS, grants from KANE SPA, grants from CONVATEC, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Sav A, Kendall E, McMillan SS, et al. ‘You say treatment, I say hard work’: treatment burden among people with chronic illness and their carers in Australia. Health Soc Care Community. 2013;21(6):665–674. doi:10.1111/hsc.12052
2. May CR, Eton DT, Boehmer K, et al. Rethinking the patient: using burden of treatment theory to understand the changing dynamics of illness. BMC Health Serv Res. 2014;14(1):1–11. doi:10.1186/1472-6963-14-281
3. Mair FS, May CR. Thinking about the burden of treatment. BMJ. 2014;349:g6680. doi:10.1136/bmj.g6680
4. Tran VT, Montori VM, Eton DT, Baruch D, Falissard B, Ravaud P. Development and description of measurement properties of an instrument to assess treatment burden among patients with multiple chronic conditions. BMC Med. 2012;10(1):68. doi:10.1186/1741-7015-10-68
5. Brod M, Hammer M, Christensen T, Lessard S, Bushnell DM. Understanding and assessing the impact of treatment in diabetes: the treatment-related impact measures for diabetes and devices (TRIM-diabetes and TRIM-diabetes device). Health Qual Life Outcomes. 2009;7:83. doi:10.1186/1477-7525-7-83
6. Pifferi M, Bush A, Di Cicco M, et al. Health-related quality of life and unmet needs in patients with primary ciliary dyskinesia. Eur Respir J. 2010;35(4):787–794. doi:10.1183/09031936.00051509
7. Chinn IK, Orange JS. Immunodeficiency disorders. Pediatr Rev. 2019;40(5):229LP- 242. doi:10.1542/pir.2017-0308
8. Espanol T, Prevot J, Drabwell J, Sondhi S, Olding L. Improving current immunoglobulin therapy for patients with primary immunodeficiency: quality of life and views on treatment. Patient Prefer Adherence. 2014;8:621–629. doi:10.2147/PPA.S60771
9. Gardulf A, Nicolay U. Replacement IgG therapy and self-therapy at home improve the health-related quality of life in patients with primary antibody deficiencies. Curr Opin Allergy Clin Immunol. 2006;6(6):434–442. doi:10.1097/01.all.0000246619.49494.41
10. Mozaffari H, Pourpak Z, Pourseyed S, Moin M, Farhoodi A. Health-related quality of life in primary immune deficient patients. Iran J Allergy Asthma Immunol. 2006;5:23–27.
11. Jones GL, Vogt KS, Chambers D, Clowes M, Shrimpton A. What is the burden of immunoglobulin replacement therapy in adult patients with primary immunodeficiencies? A systematic review. Front Immunol. 2018;9(JUL). doi:10.3389/fimmu.2018.01308
12. Daly PB, Evans JH, Kobayashi RH, et al. Home-based immunoglobulin infusion therapy: quality of life and patient health perceptions. Ann Allergy. 1991;67(5):504–510.
13. Nicolay U, Haag S, Eichmann F, Herget S, Spruck D, Gardulf A, Measuring treatment satisfaction in patients with primary immunodeficiency diseases receiving lifelong immunoglobulin replacement therapy. Qual Life Res. 2005;14(7):1683–1691. doi:10.1007/s11136-005-1746-x
14. Gardulf A, Nicolay U, Math D, et al. Children and adults with primary antibody deficiencies gain quality of life by subcutaneous IgG self-infusions at home. J Allergy Clin Immunol. 2004;114(4):936–942. doi:10.1016/j.jaci.2004.06.053
15. Vultaggio A, Azzari C, Milito C, et al. Subcutaneous immunoglobulin replacement therapy in patients with primary immunodeficiency in routine clinical practice: the VISPO prospective multicenter study. Clin Drug Investig. 2015;35(3):179–185. doi:10.1007/s40261-015-0270-1
16. Gardulf A, Borte M, Ochs HD, Nicolay U. Vivaglobin clinical study group. Prognostic factors for health-related quality of life in adults and children with primary antibody deficiencies receiving SCIG home therapy. Clin Immunol. 2008;126(1):81–88. doi:10.1016/j.clim.2007.06.009
17. Beauté J, Levy P, Millet V, et al. Economic evaluation of immunoglobulin replacement in patients with primary antibody deficiencies. Clin Exp Immunol. 2009;160(2):240–245. doi:10.1111/j.1365-2249.2009.04079.x
18. Jones CA, Rojavin M, Baggish JS. Patients with primary immunodeficiency receiving subcutaneous immune globulin Hizentra maintain health-related quality of life and treatment satisfaction in a multicentre extension study of efficacy, tolerability and safety. J Pharm Heal Serv Res. 2012;3(1):41–47. doi:10.1111/j.1759-8893.2011.00076.x
19. US Food and Drug Administration. Guidance for industry on patient-reported outcome measures: use in medical product development to support labeling claims. Fed Regist. 2009;74(235):65132–65133.
20. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi:10.1191/1478088706qp063oa
21. Moores KL, Jones GL, Radley SC. Development of an instrument to measure face validity, feasibility and utility of patient questionnaire use during health care: the QQ-10. Int J Qual Heal Care. 2012;24(5):517–524. doi:10.1093/intqhc/mzs051
22. Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Heal J Int Soc Pharmacoeconomics Outcomes Res. 2005;8(2):94–104. doi:10.1111/j.1524-4733.2005.04054.x
23. Field AP. Discovering Statistics Using SPSS: (And Sex, Drugs and Rock’n’roll). SAGE; 2005. Available from: https://books.google.co.uk/books?id=IY61Ddqnm6IC.
24. Kline P. A Handbook of Test Construction: Introduction to Psychometric Design. New York, NY, US: Methuen; 1986.
25. Kaiser HF, Rice J. Little Jiffy, Mark Iv. Educ Psychol Meas. 1974;34(1):111–117. doi:10.1177/001316447403400115
26. Stevens J. Applied Multivariate Statistics for the Social Sciences.
27. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. doi:10.1007/BF02310555
28. Helmstadter GC. Principles of Psychological Measurement. Appleton-Century-Crofts; 1964. Available from: https://books.google.co.uk/books?id=khHs5Zhz4JcC.
29. Carmines E, Zeller R. Reliability and Validity Assessment. 2455 Teller Road, Thousand Oaks California 91320 United States of America: SAGE Publications, Inc; 1979. doi:10.4135/9781412985642
30. Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to Their Development and Use. Oxford University Press; 1995. Available from: https://books.google.co.uk/books?id=8TYQAQAAMAAJ.
31. Nunnally JC. Psychometric Theory. McGraw-Hill; 1978. Available from: https://books.google.co.uk/books?id=WE59AAAAMAAJ.
32. Lamping DL, Schroter S, Marquis P, Marrel A, Duprat-Lomon I, Sagnier -P-P. The community-acquired pneumonia symptom questionnaire: a new, patient-based outcome measure to evaluate symptoms in patients with community-acquired pneumonia. Chest. 2002;122(3):920–929. doi:10.1378/chest.122.3.920
33. Hajjar ST. Statistical analysis: internal-consistency reliability and construct validity. Int J Quant Qual Res Methods. 2018;6(1):27–38.
34. Nunnally JC, Bernstein IH. Psychometric Theory.
35. Gandek B, Ware JE, Aaronson NK, et al. Tests of data quality, scaling assumptions, and reliability of the SF-36 in eleven countries. J Clin Epidemiol. 1998;51(11):1149–1158. doi:10.1016/S0895-4356(98)00106-1
36. Kline P. The Handbook of Psychological Testing. Routledge; 2000. Available from: https://books.google.co.uk/books?id=lm2RxaKaok8C.
37. Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychol Assess. 1995;7(3):309–319. doi:10.1037/1040-3590.7.3.309
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
