Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 9
The cost-utility of treating anemia with continuous erythropoietin receptor activator or Epoetin versus routine blood transfusions among chronic hemodialysis patients
Authors Maoujoud O, Ahid S, Cherrah Y
Received 9 September 2015
Accepted for publication 17 November 2015
Published 24 February 2016 Volume 2016:9 Pages 35—43
DOI https://doi.org/10.2147/IJNRD.S96027
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Omar Maoujoud,1,2 Samir Ahid,1 Yahia Cherrah1
1Research Team of Pharmacoepidemiology and Pharmacoeconomics, Medical and Pharmacy School, Mohammed V University, Rabat, 2Department of Nephrology and Dialysis, Military Hospital, Agadir, Morocco
Objective: The purpose of this study was to determine the cost-utility of treating anemic dialysis patients with continuous erythropoietin receptor activator (CERA) once monthly or Epoetin Beta (EpoB) thrice weekly compared with a reference strategy of managing anemia with red blood cell transfusion (RBCT).
Methods: Cost-utility analysis study design. Decision analysis model, National health care payer, over 1 year with the publicly funded health care system. Chronic hemodialysis patients with renal anemia were included. The outcome marker of this study was the incremental cost per quality-adjusted life-year (QALY) gained (incremental cost-utility ratio [ICUR]) of CERA or EpoB relative to RBCT.
Results: The total cost per patient (in US$) was estimated at $2,176.37, $4,107.01, and $4,356.69 for RBCT, CERA, and EpoB, respectively. The cost-utility ratio was calculated at 4,423.52, 6,955.50, and 7,406.38 $/QALY for RBCT, CERA, and EpoB, with an ICUR of CERA and EpoB in relation to RBCT at 19,606.40 and 22,466.09 $/QALY, respectively. In sensitivity analysis, the model was most sensitive to hospitalization costs, hospital stay, and annual number of RBCT units. Also, assuming utility and survival improvement with erythropoiesis stimulating agents use resulted in a decrease in ICUR at 13,429 $/QALY for CERA and 15,331 $/QALY for EpoB. In probabilistic sensitivity analysis, the main results of our model were unchanged; CERA and EpoB were more costly and more effective than RBCT below a threshold of 19,500 $/QALY. CERA was the best option for a willingness to pay over 19,500 $/QALY.
Limitations: Some model parameters were obtained from observational data, the comparator RBCT is not the standard of care.
Conclusion: Our study suggests that managing anemia in dialysis patient with CERA or EpoB may results in better outcomes with higher overall costs. Considering different assumptions, we found substantial variability in the estimates of the cost-utility and incremental of using CERA or EpoB.
Keywords: cost-utility, cost-effectiveness, anemia, dialysis, erythropoiesis stimulating agents, continuous erythropoietin receptor activator, epoetin
Introduction
Anemia is a common complication of chronic kidney disease (CKD) because of decreased kidney production of erythropoietin. It is associated with adverse clinical outcomes and poor health-related quality of life (QOL).1,2 Treatment of anemia before the advent of erythropoiesis stimulating agents (ESAs) relied on routine blood transfusions.2–4 Early studies demonstrated a reduction in transfusions needed and an improvement in QOL in chronic hemodialysis patients (CHP) after the introduction of ESA in the market, compared with managing anemia without ESAs.4,5 Therefore, ESAs in routine clinical practice diffused rapidly and became the standard option.6 The class of ESA includes the short-acting forms Epoetin Alpha and Epoetin Beta (EpoB), and the long-acting ones: darbepoetin and the pegylated erythropoietin continuous erythropoietin receptor activator (CERA).7 Understanding the relative cost-utility of those treatments is of importance to both clinicians and health care reimbursement authorities, as the acquisition costs of all ESAs are relatively high and are among the top drug expenditures of hospitals, health care payers, and providers.7–10 Although all of previous health economic studies focused their analysis on short-acting ESA, CERA as the last one to be introduced in clinical practice has not been well studied yet.1,7,9,11
The purpose of this study was to determine the cost-utility of treating dialysis patients with CERA once monthly or EpoB thrice weekly compared with a strategy of managing anemia without ESAs.
Patients and methods
Study design
We estimated the cost per quality-adjusted life-year (QALY) gained with treatment using two different ESAs to maintain hemoglobin level within the target 10.5–12 g/dL, compared with strategy of managing anemia without ESAs. A decision analytic model was constructed to model the cost and clinical outcomes in a cohort of Moroccan CHP. All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and/or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Treatment comparators
Three treatment strategies were compared: (1) CERA, (methoxy polyethylene glycol-EpoB; Mircera®; Hoffman-La Roche Ltd, Basel, Switzerland); (2) EpoB, (Recormon®; Hoffman-La Roche Ltd); and (3) management of anemia without ESAs (use of rescue red blood cell transfusions [RBCTs]).
Population and data sources
ESA requirement, efficacy, and costs
We used the study of Maoujoud et al12 to provide clinical and costing data for this model. Authors reported in this prospective observational study the cost-effectiveness of CERA once monthly in comparison with EpoB thrice weekly to maintain hemoglobin within the range 10.5–12 g/dL. The study was conducted in a cohort of 75 Moroccan CHP. In this study, patients who complied with the inclusion criteria were selected for a follow-up over two periods: the first period during 6 months (month −6 to 0); maintaining prior treatment with EpoB thrice weekly; the second for 6 months (month 0–6), after changing treatment to CERA once monthly. The cost-effectiveness analysis was conducted from the health care payer perspective; and applied decision analytic techniques; key model inputs included clinically effectiveness measures, which was measured by the clinical success rate of treatment, defined as the proportion of patients successfully maintaining Hb within the range of 10.5–12 g/dL, in the first period on EpoB and in the second period on CERA therapy, as well as drug acquisition costs for both treatments considered.
Iron use
Mean intravenous iron requirement in maintenance therapy with ESA was estimated according to two Moroccan studies Maoujoud et al12 and Benamar,13 which are in accordance with the recent data provided by the Dialysis Outcomes and Practice Patterns Study (DOPPS) reports.14 For our model, we adopted an average use of intravenous iron for in-center hemodialysis patients at 100–125 mg/month.
RBCT requirement
Transfusion requirement for patients not receiving ESAs was based on two Moroccan studies (Benamar et al15 and Bahadi et al16), also we considered for our analysis the data reported by Remak et al4 and Naci et al,17 according to those studies; the average number of RBCT/year needed was estimated in our model at 10 red blood cell units/year.
Quality of Life
QALY is the survival weighted by health-related QOL, it is calculated by multiplying survival with utility; which is a measure of the preference for a specific health outcome, and usually acts as a single marker of health-related QOL. Utility ranges from 0, representing the worst imaginable health, to 1, representing perfect health.7,18 Considering previous studies, there is a continuous improvement in QOL with the increase in Hb level using ESA,1,17,19 we determinate the QALYs in our model at three Hb ranges: low Hb range (9–10.5 g/dL), high Hb range (>12 g/dL), and intermediate Hb range (10.5–12 g/dL). For baseline analysis to obtain QALYs, survival was multiplied by utility at the three ranges. The utility estimate for dialysis patients treated with ESA was based on the published meta-analysis, randomized trials, and cohorts studies comparing different Hb levels achieved7,19,20 and from recent studies evaluating QOL in CHP.17 The average utility score for CHP treated with ESA and achieving Hb in the range 10.5–12 g/dL was estimated at 0.64,7,17,21–23 and at 0.63 for patients in the lower Hb range.3,7,22 As there is no evidence that utility scores continue to improve, once Hb level rise above 12.0, we considered only one utility score for all Hb above 12 g/dL at 0.65.3,7,20 For hemodialysis patients not receiving ESA, the mean Hb level was estimated by the Moroccan society of nephrology at 8.25 g/dL in the national registry of renal disease Magredial.24 Thus, we considered in our model this level of Hb; with a corresponding utility score at 0.54, considering previous studies that had evaluated the QOL in CHP receiving only RBCT.19,20,22,25
Mortality
Annual mortality in CHP treated with ESA in comparison with RBCT was based on two systematic reviews1,19 and a health economic evaluation of ESA in CKD.7 Annual mortality rates for each of the three Hb ranges in CHP receiving ESA and patients receiving RBCT were obtained from the same studies. For our model as reported in the meta-analysis of Tonelli et al19 and in the study of Naci et al,17 we considered that ESA use is associated with better survival in comparison with RBCT, and that mortality rate in the intermediate Hb level (10.5–12 g/dL) and low (<9–10.5 g/dL) is similar. Also, we integrate in our model the results of randomized controlled trials that demonstrated an increase in mortality with higher Hb level6,26–28 in comparison with low and intermediate ranges.
Hospitalization
Data relative to hospitalization in Moroccan hemodialysis patients receiving ESA were extrapolated from four observational studies.29–32 In the absence of RCT investigating the relationship between ESA use or Hb level, and the risk or the duration of hospitalization, we assumed in our model that there is no difference in hospital stay for the three Hb ranges, this assumption is comforted by previous studies.17,20,33 Hospitalizations in patients receiving RBCT only in the model were based on Moroccan observational data reported by Bahadi et al,16 and the studies of Remak et al4 and Naci et al;17 considering those reports, ESA use in CHP is associated with a decrease in hospitalization estimated at −37% in comparison with patients receiving RBCT. Baseline clinical, costs and assumptions are reported in Table 1.
Economic analysis
In our analysis, we adopted the perspective of the National health care payer in Morocco, for a time horizon of 1 year. So, for CERA and EpoB, we considered direct medical cost including ESA acquisition cost, iron usage, and hospitalization. For RBCT, we based our estimation on the hospital cost of one unit of transfused filtered red blood cells, including compatibility testing, cross-matching, and the infusion in day hospital. All costs were obtained from the prices approved by the Moroccan National Agency on Medical Insurance (ANAM), they were collected every 3 months, reported in Moroccan dirhams (MAD) then converted to US dollar ($) (in 2013; 1 US$ = 9,297 MAD). A discount rate of 3% was applied to both costs and utilities, all analyses were performed using TreeAge Pro 2015 (TreeAge Software, Williamstown, MA, USA).
Cost-utility analysis
In order to calculate costs, QALYs and increments associated with CERA, EpoB, and RBCT alone, a decision analysis model was constructed in TreeAge Pro 2015 (TreeAge Software). Key model inputs included for CERA, EpoB, and RBCT; medical costs, survival, and utilities depending on Hb levels. Model outputs were expected cost-utility ratio and the incremental cost-utility ratio (ICUR), which represent the additional cost and utility obtained, when CERA or EpoB is compared with the RBCT regime. As there is no official incremental cost-utility threshold for willingness to pay (WTP) in Morocco; being considered as ideal for the acceptance of a given health intervention, we compared ICUR with different hypothetical WTPs.
Sensitivity analysis
Given the fact that our model involves some uncertainties and assumptions, we performed one-way sensitivity analysis; by varying baseline estimates within a range of potentially reasonable values, particularly the number of hospitalizations, the mean length of hospital stay, ESA costs, utilities, and survival estimations. Also, probabilistic sensitivity analysis was conducted by a Monte Carlo simulation; to better test the overall uncertainty in our model. We varied the input parameters used in clinical effectiveness, utility, and cost estimates. A normal distribution was used for clinical parameters, and a log-normal distribution was applied to the cost estimates.
Results
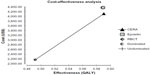
In Table 2, cost, QALYs, and incremental associated with CERA and EpoB administration, compared to treatment with RBCT, are summarized. The total cost per patient was estimated at $2,176.37, $4,107.01, and $4,356.69 for RBCT, CERA, and EpoB, respectively. In our model, ESA administration was associated with an increase in patients’ QOL by 0.1 QALYs per annum in average, compared to treatment with RBCT alone, with an incremental cost at $1,930.64 for CERA and $2,189.32 for EpoB. Therefore, the cost-utility ratio was calculated at 4,423.52, 6,955.50, and 7,406.38 $/QALY for RBCT, CERA, and EpoB, with an ICUR of CERA and EpoB in relation to RBCT at 19,606.40 and 22,466.09 $/QALY, respectively. The cost-utility diagram is resumed in Figure 1.
For the one-way sensitivity analysis, the inputs in the model were allowed to vary within clinically plausible ranges. Table 3 shows sensitivity of the base-case ICUR of CERA and EpoB relative to RBCT in different scenarios tested. The model was most sensitive to hospitalization costs, hospital stay, and annual number of RBCT units, any increase in those parameters resulted in a decrease in ICURs as reported in Table 3. Assuming utility and survival improvement with ESA use while all costs remained the same resulted in a decrease in ICUR at 13,429 $/QALY for CERA and 15,331 $/QALY for EpoB. Testing the hypothesis of equal mortality rate between ESA use and RBCT; only resulted in an ICUR at 20,878 $/QALY and 23,940 $/QALY, respectively. Decreasing the acquisition cost of CERA and EpoB by 25% resulted in ICUR at 11,911 $/QALY and 14,088 $/QALY, respectively.
The probabilistic sensitivity analysis was performed using a second-order Monte Carlo simulation, for this analysis, 10,000 simulated trials were run. The main results of our model were unchanged; CERA and EpoB therapy was always more costly and more effective than RBCT as shown in the scatter plots of Figures 2 and 3. A cost-effectiveness acceptability curve was also obtained from the simulation (Figure 4). This graph indicates the probability that the use of CERA and EpoB being cost-effective compared with RBCT at different levels of a maximum acceptable threshold for WTP. At all WTP thresholds below 19,500 $/QALY gained, RBCT was the cost-effective as compared with both ESAs, and a WTP at 19,666 $/QALY resulted in a probability that CERA was cost-effective at 65%. Over this threshold, CERA was always the best option.
Discussion
This cost-utility analysis shows that treating anemia in CHP with CERA or EpoB is associated with a substantial clinical benefit and results in significant additional cost relative to RBCT. Elaborate sensitivity analyses revealed that the health care payer should be willing to pay at least $19,666 per additional QALY for CERA to become cost-effective compared with a strategy without ESA use. In Morocco, there is no official adopted threshold value of the WTP; as almost all emerging countries. The World Health Organization consider an incremental cost per QALY gained or an incremental cost-effectiveness ratio of a medical intervention below one time of the gross domestic product (GDP) per capita as maximum cost-effective, between 1 and 3 times of GDP per capita as cost-effective, and more than 3 times of GDP per capita as not cost-effective.34 According to the World Bank,35 the 2013 Moroccan GDP per capita was estimated at $3,092, considering this value, a threshold of 9,276 $ would be adopted as maximum limit for a health procedure to be considered as being cost-effective; therefore, CERA and EpoB would be considered technically as not cost-effective in our model. But this is a misinterpretation of the main results of our study. Indeed, the comparison between ESA and RBCT in the management of anemia has been considered as counter-factual;17 considering the fact that the use of ESA as a treatment of anemia in dialysis patients is now unanimly considered as the standard of care;36–39 following international clinical practice guidelines for anemia management in CKD40 and Moroccan national guidelines,41 as RBCT is linked to transfusion-transmitted infections, immunologic sensitization complicating transplantation, and iron overload.1,2 In our model, it was mandatory to include RBCT as a reference procedure; because at our knowledge, this is the first cost-utility analysis of ESA including CERA.9,11 None of the previous cost-utility or cost-effectiveness studies had considered the last long-acting ESA for anemia in such population. Also, in Morocco, our study is the first to evaluate ESA at all. As reported recently by Schmid,9 there are few pharmacoeconomic studies evaluating the cost-utility of CERA; in 18 publications included in his analysis, only one study published as an abstract, reported data about the cost and QALY relative to CERA use in Brazilian dialysis patients;40 using a model of a hypothetical cohort of CHP treated with CERA or epoetin, the analysis showed that epoetin treatment was more cost-effective than CERA treatment. Unfortunately, it was not possible to compare this study with our results since the access was limited to an abstract. We evaluated the robustness of the main finding in extensive sensitivity analysis, and found that our model was sensitive to hospitalizations length and cost, number of RBCT units, and utility estimates. These parameters have been highlighted in previous studies as major drivers of cost variations among chronic dialysis patients.1,7,17,33 In addition, wherever uncertainty exists, we have make some assumptions favorable to RBCT, as we did not consider the costs relative to complications of blood transfusion, and hospitalization costs were based only on the minimum daily cost allowed by the National Agency of Medical Insurance without considering medications and investigation costs. Not surprisingly, when assuming higher costs of hospital stay per day, ESA use become more cost-effective, as reported in the systematic review of Ferguson et al.1 Our analysis has several strengths. This is the first cost-utility study of ESA in the management of anemia in CHP that consider CERA; to be published in peer-review journal. Also, our results are as close to real practice as possible; as CERA and EpoB doses, costs, and efficacy were derived from our previous prospective observational real-life study.12 Indeed, we have tried to deal with uncertainties and assumptions in our model with sensitivity analysis. Other economic evaluations did not fully test the assumptions though sensitivity analysis. There are some limitations to our study. Considering the lack of data on some epidemiological parameters such as mortality rate and utility scores in Moroccan hemodialysis patients, we based our analysis on results of randomized controlled trials and systematic reviews that have been conducted on this topic; to limit this potential bias. Also, our baseline estimates of hospitalizations rates and duration are based on some Moroccan retrospectives studies,15,16,24,29–31 for this reason, we have also consider the results of previous cohort studies and analysis conducted in other countries. We did not include indirect costs such as loss of productivity and travel costs. Given the fact that the perspective was that of a health care payer, and not a societal one, and in the absence of evidence that ESA use increases employment rates in hemodialysis patients. Makes it unlikely that adopting societal perspective would have changed our results.1,7,17,19,33 The results of our analysis have several potential implications for clinical practice, health policy, and futures research. Our study shows the cost-utility associated with CERA and EpoB in a clinical and market context close to real-life. Also, we believe that our analysis would inform policy makers about optimal planning relative to ESA use.
Conclusion
In conclusion, our study suggests that managing anemia in dialysis patient with ESA may results in better outcomes with higher overall costs. Considering different assumptions, we found substantial variability in the estimates of the cost-utility and incremental of using CERA or EpoB, nevertheless, our findings can help future investigators to design better cost-effectiveness and cost-utility studies.
Acknowledgments
The authors would like to thank Zouhair Oualim, Hocein Dkhissi, Mohamed Lisri, and Mohammed Asseraji on behalf of the Moroccan Society of Nephrology, for useful comments on earlier drafts of the manuscript.
Partial data from this manuscript have been presented as a poster at the World Congress of Nephrology, organized by the International society of nephrology: Cape Town, South Africa March 2015, poster number SAT-451.
Disclosure
The authors report no conflicts of interest in this work.
References
Ferguson T, Xu Y, Gunasekara R, et al. The cost effectiveness of erythropoietin-stimulating agents for treating anemia in patients on dialysis: a systematic review. Am J Nephrol. 2015;41(2):89–97. | |
Keown PA, Churchill DN, Poulin-Costello M, et al. Dialysis patients treated with Epoetin alfa show improved anemia symptoms: a new analysis of the Canadian Erythropoietin Study Group trial. Hemodial Int. 2010;14(2):168–173. | |
Clement FM, Klarenbach S, Tonelli M, Johnson JA, Manns BJ. The impact of selecting a high hemoglobin target level on health-related quality of life for patients with chronic kidney disease: a systematic review and meta-analysis. Arch Intern Med. 2009;169(12):1104–1112. | |
Remak E, Hutton J, Jones M, Zagari M. Changes in cost-effectiveness over time. The case of Epoetin Alfa for renal replacement therapy patients in the UK. Eur J Health Econ. 2003;4(2):115–121. | |
Bahlmann J, Schoter KH, Scigalla P, et al. Morbidity and mortality in hemodialysis patients with and without erythropoietin treatment: a controlled study. Contrib Nephrol. 1991;88:90–106. | |
Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med. 1998;339(9):584–590. | |
Clement FM, Klarenbach S, Tonelli M, Wiebe N, Hemmelgarn B, Manns BJ. An economic evaluation of erythropoiesis-stimulating agents in CKD. Am J Kidney Dis. 2010;56(6):1050–1061. | |
Burnier M, Douchamps JA, Tanghe A, et al. Less frequent dosing of erythropoiesis stimulating agents in patients undergoing dialysis: a European multicentre cost study. J Med Econ. 2009;12(2):77–86. | |
Schmid H. Cost-effectiveness of continuous erythropoietin receptor activator in anemia. Clinicoecon Outcomes Res. 2014;6:319–330. | |
Meguid El Nahas A, Bello AK. Chronic kidney disease: the global challenge. Lancet. 2005;365(9456):331–340. | |
Becker R, Dembek C, White LA, Garrison LP. The cost offsets and cost-effectiveness associated with pegylated drugs: a review of the literature. Expert Rev Pharmacoecon Outcomes Res. 2012;12(6):775–793. | |
Maoujoud O, Ahid S, Cherrah Y. Analyse coût-efficacité du CERA vs Epoetin beta dans le traitement de l’anémie chez les hémodialysés chroniques. 1er colloque national de pharmaco-épidémiologie et pharmaco-économie. Rabat, Morocco; 2013. | |
Benamar L. Traitement de la carence martiale en dialyse. 11th Congress of the Moroccan Society of Nephrology. Marrakech, Morocco; 2013. | |
Weiss G, Kronenberg F. Intravenous iron administration: new observations and time for the next steps. Kidney Int. 2015;87(1):10–12. | |
Benamar L, Rhou H, Ezzaitouni H. Hepatite virale c chez les hemodilayses chroniques au CHU de Rabat, prevalence et facteurs de risques. Med Maghreb. 2001;89:17. | |
Bahadi A, Maoujoud O, Zejjari Y, et al. [Diagnosis and evaluation of hepatitis C virus among haemodialysis patients]. East Mediterr Health J. 2013;19(2):192–199. | |
Naci H, de Lissovoy G, Hollenbeak C, et al. Historical clinical and economic consequences of anemia management in patients with end-stage renal disease on dialysis using erythropoietin stimulating agents versus routine blood transfusions: a retrospective cost-effectiveness analysis. J Med Econ. 2012;15(2):293–304. | |
Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis. 1987;40(6):593–603. | |
Tonelli M, Klarenbach S, Wiebe N, Shrive F, Hemmelgarn B, Manns B. Erythropoiesis-stimulating agents for anemia of chronic kidney disease: systematic review and economic evaluation. Technology Report no 106. Ottawa, Canada: Canadian Agency for Technology and Drugs in Health; 2008. | |
Tonelli M, Winkelmayer WC, Jindal KK, Owen WF, Manns BJ. The cost-effectiveness of maintaining higher hemoglobin targets with erythropoietin in hemodialysis patients. Kidney Int. 2003;64(1):295–304. | |
Manns B, Johnson JA, Taub K, Mortis G, Ghali WA, Donaldson C. Quality of life in patients treated with hemodialysis or peritoneal dialysis: what are the important determinants? Clin Nephrol. 2003;60(5):341–351. | |
CANEPO. Canadian Erythropoietin Study Group. Effect of recombinant human erythropoietin therapy on blood pressure in hemodialysis patients. BMJ. 1990;300:573–578. | |
Kaufman JS, Reda DJ, Fye CL, et al. Subcutaneous compared with intravenous epoetin in patients receiving hemodialysis. Department of Veterans Affairs Cooperative Study Group on Erythropoietin in Hemodialysis Patients. N Engl J Med. 1998;339(9):578–583. | |
Ramdani B. Insuffisance renale chronique terminale au maroc: enjeux economique. Registre MAGREDIAL, données préliminaires. 2012; Mars 2012: Agadir Maroc. | |
Asserraji M, Maoujoud O, Belarbi M, Oualim Z. [Epidemiological profile of end stage renal disease at the Military Hospital in Rabat, Morocco]. Pan Afr Med J. 2015;20:439. | |
Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355(20):2085–2098. | |
Pfeffer MA, Burdmann EA, Chen CY, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361(21):2019–2032. | |
Besarab A, Goodkin DA, Nissenson AR. The normal hematocrit study – follow-up. N Engl J Med. 2008;358(4):433–434. | |
Ezziani M, Najdi A, Mikou S, Hanin H, Arrayhani M, Houssaini TS. [Predictors of response to the CERA in chronic hemodialysis treatment-naive by erythropoiesis-stimulating agent]. Pan Afr Med J. 2015;20:331. | |
El Farouki MR, Bahadi A, Hamzi MA, Kabbaj D, Benyahia M. [Profile of chronic renal failure in diabetes at initiation of hemodialysis in the nephrology and dialysis service of the military hospital in Rabat, Morocco]. Pan Afr Med J. 2013;15:124. | |
Zemaraoui N, Maoujoud O, Belarbi M. La référence tardive au néphrologue des patients en insuffisance rénale chronique : fréquence et conséquences. Research. 2014;1:1255. | |
Ezziani M, Tazi El Pardya N, Mbarki H, Kabbali N, Arrayhani M, Sqalli Houssaini T. [Profil des patients hospitalisés en néphrologie en 2013]. Néphrol Thér. 2013;10(5):398. | |
Glenngard AH, Persson U, Schon S. Cost-effectiveness analysis of treatment with epoietin-alpha for patients with anaemia due to renal failure: the case of Sweden. Scand J Urol Nephrol. 2008;42(1):66–73. | |
World Health Organization. Making Choices in Health. WHO Guide to Cost-Effectiveness Analysis. 2003. Available from: http://www.who.int. | |
World Development Indicators (Morocco). The World Bank. 2013. Available from: http://www.worldbank.org/. | |
Akbari A, Clase CM, Acott P, et al. Canadian Society of Nephrology commentary on the KDIGO clinical practice guideline for CKD evaluation and management. Am J Kidney Dis. 2014;65(2):177–205. | |
Kliger AS, Foley RN, Goldfarb DS, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for anemia in CKD. Am J Kidney Dis. 2013;62(5):849–859. | |
Locatelli F, Barany P, Covic A, et al. Kidney disease: improving global outcomes guidelines on anaemia management in chronic kidney disease: a European Renal Best Practice position statement. Nephrol Dial Transplant. 2013;28(6):1346–1359. | |
Locatelli F, Nissenson AR, Barrett BJ, et al. Clinical practice guidelines for anemia in chronic kidney disease: problems and solutions. A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2008;74(10):1237–1240. | |
Silva FHCV, Vianna CMDM, Silva FVC. Cost-effectiveness of anemia treatment in dialysis patients in Brazil: ISPOR 3rd Latin America conference research abstract. Value Health. 2011;14(7):A570. | |
SMN, Moroccan Society of Nephrology Guidelines RBMP. ALD 17 (Insuffisance Renal Chronique Terminale), SMN, 2011. Available from: www.nephro-maroc.org. Accessed January 26, 2016. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.