Back to Journals » ClinicoEconomics and Outcomes Research » Volume 12
The Cost-Effectiveness of Universal Varicella Vaccination in Italy: A Model-Based Assessment of Vaccination Strategies
Authors Azzari C , Baldo V , Giuffrida S , Gani R , O'Brien E, Alimenti C, Daniels VJ , Wolfson LJ
Received 13 September 2019
Accepted for publication 16 February 2020
Published 8 June 2020 Volume 2020:12 Pages 273—283
DOI https://doi.org/10.2147/CEOR.S229685
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
C Azzari,1 V Baldo,2 S Giuffrida,3 R Gani,4 E O’Brien,5 C Alimenti,6 VJ Daniels,7 LJ Wolfson7
1Department of Health Sciences, University of Florence and Meyer Children’s University Hospital, Florence 50139, Italy; 2Hygiene and Public Health Unit Department of Cardiac Thoracic Vascular Sciences and Public Health University of Padua, Padua 35100, Italy; 3LHU Reggio Calabria, Reggio 89100, Calabria, Italy; 4Evidence Synthesis, Modeling & Communication, Evidera, London, UK; 5Evidence Synthesis, Modeling & Communication, Evidera, San Francisco, CA, USA; 6MSD Italy, Market Access, Roma, Italy; 7Center for Observational and Real-World Evidence, Merck & Co., Inc., Kenilworth, NJ, USA
Correspondence: LJ Wolfson
Merck & Co., Inc., Center for Observational and Real-World Evidence (CORE), 600 Corporate Drive, CRB-205, Kenilworth, NJ 08833, USA
Tel +1 267-305-0650
Email [email protected]
Background: In 2017, varicella vaccination became mandatory for all children in Italy, based on a two-dose schedule administered at 12– 15 months of age and 5 to 6 years of age. Varicella vaccines are available in different formulations (as a single vaccine or as a combination vaccine together with measles, mumps, and rubella) and are made by multiple manufacturers with different effectiveness profiles. This study calculates the cost-effectiveness of a range of varicella vaccination strategies to identify the optimal strategy for Italy.
Methods: A dynamic transmission cost-effectiveness model was applied in Italy to simulate the long-term (50 years) costs and outcomes associated with different varicella vaccination strategies. Five vaccination strategies were evaluated using the model: two doses of two different combination Measles-Mumps-Rubella-Varicella vaccines (either Vaccine A (MSD) [denoted QQVa] or Vaccine B (GSK) [denoted QQVb]); a first dose of a single Varicella vaccine followed by a second dose of a combination vaccine (either Vaccine C (MSD) followed by Vaccine A [denoted MQVa] or Vaccine D (GSK) followed by Vaccine B [denoted MQVb]); or no vaccine at all (NV). The model was adapted for Italy using publicly available Italian data and expert opinion.
Results: Over the 50-year time-horizon, in the absence of universal varicella vaccination, there would be 34.8 million varicella cases, 142 varicella-infection-related deaths, and € 23 billion in societal costs. The cost per capita from a societal perspective ranged from € 164.55 to € 392.18 with NV being the most expensive and QQVa the least expensive. The most effective strategy was QQVa, which resulted in a 66% decrease in varicella cases and 30% reduction in varicella-related deaths compared to NV strategy. QQVa led to a net saving in societal cost around € 13 billion compared to NV as the cost of vaccination was more than offset by the savings that resulted from the reduced burden of illness.
Conclusion: Varicella vaccination has a major impact on reducing varicella incidence, prevalence, and societal costs. This analysis supports the policy for universal varicella vaccination in Italy as the NV strategy was the most expensive and resulted in the poorest outcomes. QQVa offers the greatest benefits at the lowest cost and should be considered as a potential priority strategy for Italian population.
Keywords: varicella, vaccination, Italy, health-economics, cost-effectiveness, chickenpox, MMRV, varicella zoster virus
Background
Varicella is one of the most common infectious diseases in children and is caused by the varicella zoster virus (VZV). The annual worldwide incidence of varicella is estimated to range from 2 to 16 cases per 1000 persons, with the highest incidence observed in individuals under 15 years of age.1–3 Primary VZV infection is characterized by an incubation period ranging from 10 to 21 days, and is infectious via contact up to 5 days after the onset of symptoms.4 In most cases, varicella is a self-limited disease, and symptomatic treatment (with acetaminophen to control fever, lotions for pruritus, and fluid substitution to maintain hydration) is sufficient. Treatment with antivirals is recommended for patients at risk for severe disease (such as immunocompromised hosts and newborns whose mothers acquired infection around the time of delivery) and for people with VZV infection with virally mediated complications (e.g. ocular involvement, pneumonia, or encephalitis).5 Treatment of healthy children with varicella with oral acyclovir within 24 hrs of the onset of illness resulted in reduction in the severity of cutaneous and systemic signs and symptoms; however, it did not appear to reduce the rate of complications.6
The overall mortality rates due to varicella in the European Union/European Economic Area countries range from 0.01% to 5.4% among hospitalized cases of varicella per year.7 These are likely to be from immunocompromised individuals or individuals who acquired an initial infection later in life. An increased incidence of meningitis, encephalitis, and bacterial superinfection, usually due to Staphylococcus aureus or Streptococcus pyogenes, has been associated with varicella infection.8,9 Varicella can disseminate to the lungs causing pneumonia and severe respiratory symptoms and has also been associated with transient hepatitis.10,11 Although rare, hemorrhagic disease and nephritis are severe complications of varicella in both children and adults.12 As a consequence of these symptoms and complications, high levels of healthcare utilization including hospitalizations and ambulatory visits are associated with varicella.13,14 In addition, varicella and the associated complications can result in missed days at work for employees with varicella or caregivers of varicella patients.15
Live-attenuated VZV vaccines have been available since the 1980s for administration to children 12 months of age and older and have been proven to be safe and effective in preventing varicella. It was not licensed in the US until 1995 around which time it began to be used more widely. The implementation of routine childhood immunization programs for varicella has resulted in a dramatic decline in morbidity and mortality related to varicella.16–18 In the United States, since the introduction of the varicella vaccination program, the mortality rate for varicella decreased from 0.41 per million population (pre-vaccination program) to 0.05 per million population (post-vaccination program), hospitalizations due to varicella declined by 88% and ambulatory visits declined by 59%.14,19 These decreases were associated with significant cost savings ($5 for every $1 spent).16,20 Similarly, in Sicily and Canada, publicly funded vaccinations were shown to decrease in the rates of hospitalizations and burden of disease.21,22 Additional countries (e.g. Uruguay, Taiwan, Germany, Finland, and Australia) have added the varicella vaccine to their childhood immunization schedule, while others recommend the vaccine for specific risk groups such as immunocompromised people (e.g. individuals with forthcoming transplantation, chemotherapy, or immunosuppression), healthcare workers, and susceptible adolescents and adults. Reductions in varicella-specific mortality and morbidity have been observed in regions in Italy after the introduction of varicella vaccination.23
In 2017, universal varicella vaccination was initiated for all children in Italy on a two-dose schedule at 12–15 months of age and 5 to 6 years of age, following the experimental phase in eight regions that had begun in 2013.24 Varicella vaccines are available in different formulations (single or in combination with measles, mumps, and rubella [MMR] vaccines), are made by multiple manufacturers, and have different effectiveness and safety profiles. Consequently, public health experts in Italy must assess which vaccines will lead to the optimal vaccination strategy. Critical components to consider include when and how to introduce a new vaccine into a national immunization program, assessment of the current burden of disease, and the potential impact of the vaccine on epidemiology, and the cost-effectiveness and fiscal impact of vaccine introduction.25 In this analysis, we provide an assessment of four alternative varicella vaccination strategies (compared to not vaccinating) in consideration of the critical components mentioned above.
Methods
An age-structured deterministic, population level, dynamic transmission model was adapted for Italy to facilitate discussions about varicella vaccine choice.26 The model was implemented using Mathematica and uses a Maternal/Passive Immunity-Susceptible-Exposed-Infectious-Recovered-Susceptible (MSEIRS) structure to model the natural disease progression history of VZV, including herpes zoster reactivation. We assume the population is homogeneous over space and gender. We derive the contact mixing matrix assuming proportionate mixing, i.e., mixing between age groups is proportional to their activity level.27 The model estimates incidence of natural or wild-type as well as breakthrough (≥42 days post varicella vaccination) varicella, as well as associated hospitalizations and deaths. These outcomes are aggregated to estimate quality-adjusted life years (QALYs), along with indirect and direct medical costs over a 50-year time horizon.
Four vaccination strategies for Italy were evaluated in comparison to each other and to not vaccinating (NV). The first and second strategies were based on two doses of combination vaccines (utilizing either ProQuad® [Vaccine A] or Priorix-Tetra® [Vaccine B], denoted as strategy QQVa (i.e. Vaccine A followed by Vaccine A) and strategy QQVb (i.e. Vaccine B followed by Vaccine B), respectively. The third and fourth strategies required a first dose of a single varicella vaccine, administered at the same visit as receipt of the MMR vaccine, and a second dose being administered as a combination vaccine. Thus, the third strategy was Varivax® [Vaccine C] + MMR VaxPro® followed by Vaccine A (denoted MQVa), and the fourth was Varilrix® [Vaccine D] + Priorix® followed by Vaccine B (denoted MQVb). The first dose was assumed to be administered at the age of 13–15 months, and the second at the age of 5 to 6 years. Coverage for the first dose for QQVa and QQVb was assumed to be 85%; coverage for the first dose of MQVa and MQVb was assumed to be 81%, assuming that coverage for a single dose vaccine would be lower than for a combination vaccine; and coverage for the second dose was assumed to be 83% for all vaccination strategies. Uptake rates were based on coverage data for the MMR vaccine programs in Italy as reported by the World Health Organization, where coverage of the first dose was 85% and the second dose was 83%.28 In the analysis, we assume that the new vaccination strategies replace existing strategies simultaneously across Italy (i.e. there is no gradual roll-out program).
The parameter data used in the model were based on public health reports, peer-reviewed publications, and expert opinion. The model assumed a total population of 59,504,000, based on United Nations population data for Italy in 2015.29 The Italian-specific epidemiology parameters required for the varicella model are provided in Table 1. When developing the model, the population was segmented into the age-groups shown in Table 1.
 |
Table 1 Healthcare Resource Utilization and Cost Data |
The costs of the vaccines were estimated as 50% of the net maximum selling prices40 in Italy in 2018, according to Italian legislation on mandatory discounts to the NHS.41
All inpatients were assumed to receive a diagnostic test and three prescriptions of over-the-counter (OTC) treatments. We assumed all cases aged one to 64 years required at one outpatient visit with those aged under <1 year old or ≥65 years old required two. One percent of outpatients received diagnostic testing and 90% received either one (if aged one to 64 years) or three (if aged <1 or 65+ years) prescription or OTC treatments.
Marginal adverse event costs related to febrile seizures when combination vaccines were used as the 1st dose of MMR-containing vaccines were included and assumed to be the same for both QQVa and QQVb, based on several studies that indicated this a class effect among combination measles-mumps-rubella-varicella vaccines.42–44 This cost was estimated to be €0.60 per person vaccinated with MMRV, based on a rate of 1/2874 additional febrile seizures per person vaccinated with MMRV, versus MMR+V,45 assuming all febrile seizures were hospitalized46 and the cost per hospitalization was €1729 per case.47 An additional charge of €7.39 was included for the single vaccines to account for administration, delivery, and cold-chain costs associated with the use of varicella vaccine components separately as opposed to using it as part of the MMRV vaccine.38
Vaccine performance is characterized by an analogue of McLean-Blower (1995) framework using published parameterizations with varying approaches to parameter estimation (Table 2). Effectiveness (take and waning) for QQVa and MQVa were taken from a simple dynamic model26 based on Kuter 2004;47 for QQVb and MQVb, they were referenced from parameters reported in modeling papers based on Prymula 2014,49–52 and supported by recently published evidence in the extension of the Prymula trial.53,54 Importantly, this framework accounts for the significance of time since vaccination in modelling the force of infection and waning of vaccine-derived protection, which is critical to capturing actual vaccine impact. Recent meta-analyses55–57 examining various aspects of varicella vaccine effectiveness have not always accounted for this factor; those that do have found more differences between vaccines made by different manufacturers. A recent analysis in from Taiwan58 provides further real-world evidence in support of the differences in take and waning between Vaccines A and B.
 |
Table 2 Assumed Properties of Varicella Vaccines |
Utility values used to calculate QALYs are the same as those used in Wolfson et al 201926 and are based on the study by Littlewood et al,59 with different rates for individuals under and over 15, and rates among breakthrough varicella much lower than for natural or wild-type varicella. Both costs and QALYs were discounted at a rate of 3% per year.60 Costs were calculated from two perspectives: the payer perspective which included costs for inpatient and outpatient visits, treatments, diagnostic testing and vaccination; and the societal perspective which included costs from the payer perspective and productivity losses.
Incremental cost-effectiveness ratios (ICERs) were calculated as the ratio of the discounted incremental cost to the discounted incremental QALY per capita for the duration of the time horizon. When the incremental cost is lower and the incremental QALY higher, the ICER cannot be calculated and the alternative strategy is referred to as being “dominant” (i.e. less expensive and more effective). A dominant strategy is always the preferred health-economic strategy at any willingness-to-pay threshold as it is cost-saving (i.e. there is a net profit associated with use of the alternative strategy) and it improves quality of life.
Model Calibration
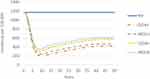
To simulate different vaccination strategies in the Italian population, age-specific contact rates and seroprevalence needed to be calibrated for the dynamic transmission model based on Italian annual population data,29 Italian annual fertility data54 and measured pre-vaccine era seroprevalence.42 The dynamic transmission model contact rates and seroprevalence were calibrated based on monotonized forms of both the population and seroprevalence data. That is, a monotonically decreasing smoothing function was applied to the Italian annual population data while preserving the Italian annual total population, while a monotonically increasing function was applied to the seroprevalence data. The calibrated data were then used as inputs for calculating the force of mortality which was then used as an input for the dynamic transmission model contact rates and seroprevalence. Proportionate mixing contact patterns were assumed, and the model calibration output (Figure 1) included in the model.61
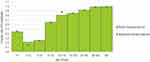 |
Figure 1 Pre-vaccine seroprevalence calibration based on data collected in Italy (2013–2014, data from 61). Abbreviation: VZV, varicella zoster virus. |
One-way deterministic sensitivity analyses (DSA) were undertaken to examine the impact of assumed variation of key local parameters on the costs associated with the different vaccination strategies. The DSA was approached by varying coverage assumptions (MMRV +10%, −15%), and the coverage gap between varicella containing vaccines (+5%, −25%); the percentage of cases requiring over-the-counter (OTC) drugs (± 20%); percent of cases requiring diagnostic testing (± 20%); cost of inpatient and outpatient care (± 20%); work days lost (± 20%); cost of work days lost (± 20%); and percent of cases requiring hospitalization or outpatient visit (± 20%). To assess the impact of overall uncertainty on the results, probabilistic sensitivity analyses (PSA) were undertaken by varying the parameters within confidence intervals. Of the 1000 PSAs run, 968 were suitable for inclusion. Further details of the parameters and probability distributions used in the PSA are provided in Supplementary Tables 1 and 2.
Results
The cumulative number of cases, hospitalizations, and deaths over the 50-year time horizon for each of the strategies is shown in Table 3. The most substantial differences are between NV and the vaccination strategies, where the number of cases falls between 52% and 66%, with the greatest fall associated with QQVa. Falls in hospitalizations are even greater (57% to 71%). Decreases in deaths are far less dramatic (20–30%) and may be due to a shift in the average age of infection to the older population. The change in annual incidence rate of varicella from initiation of strategy to the end of the 50-year time horizon is shown in Figure 2. Here we see a rapid initial decline in cases following the introduction of vaccination and deletion of the susceptible population. This is followed by a slow gradual increase in incidence as the susceptible population is supplemented with new births until a steady state is reached at around 50 years.
 |
Table 3 Burden of Disease for the Different Vaccination Strategies Over 50 Years |
The discounted costs per capita and the total costs over the 50-year time-horizon are shown in Table 4 for each of the strategies. The average discounted QALY per capita are also shown.
 |
Table 4 Health Economic Outcomes from the Base Case (All Costs and QALYs are Discounted) |
All strategies are cost-saving compared to no vaccine. However, QQVa is the most cost-saving and is more effective than all other strategies, therefore, is the preferred strategy. MQVa is the next least expensive vaccination strategy across the cost categories shown in Table 4, as well as the next best effective option. The least effective and most expensive option is NV, which is dominated by all vaccination strategies (i.e. it is the most expensive and least effective option).
The results from the DSA are shown in Figure 3. The key drivers affecting costs are the MMRV coverage and the coverage gap. Coverage has a large non-linear impact on incidence due to their influence on herd immunity. Herd immunity is an indirect benefit of vaccination whereby the number of infectious people can be depleted levels low enough to significantly reduce the transmission rate. Therefore, the incremental benefits of improved coverage can be substantial. The results are also sensitive to the percent of cases requiring hospitalization or outpatient visit.
The scatter plots from the PSA are shown in Figure 4. These support the deterministic results as they indicate QQVa and MQVa are cost-saving 100% of the time compared to NV, and QQVb and MQVb are costing-saving 82% of the time compared to NV.
 |
Figure 4 Incremental costs and QALYs vs NV generated from PSA (mean PSA values also shown). |
Discussion
The results from the model support the continuation of universal varicella vaccination in Italy. Not vaccinating against varicella is more expensive from both the societal and the healthcare payer perspectives. The results show quadrivalent vaccines as always more effective than monovalent vaccines. The QQVa strategy was the dominant strategy, and MQVb was the least effective and most expensive of the four examined vaccination strategies.
The dominance of the QQVa strategy over the other vaccine strategies results from a combination of factors, including vaccine efficacy and coverage. Administering a combination vaccine to infants likely leads to increased uptake, some parents may be hesitant to have more than one injection on 1 day and may fail to return for the missing dose. However, coverage is a major driver behind costs and outcomes even with coverage in the model ranging from 81% to 85%. Further improvements in coverage could lead to substantial improvements in outcomes.62
The treatment costs and loss of quality of life associated with febrile seizures were included in the model, given that febrile seizure has been a known, if rare adverse event associated with MMRV vaccines as a class.42–45
However, as the likelihood is relatively small and hospitalization costs low relative to varicella infection, these costs and loss of quality of life are more than offset by the benefits of vaccination.
The use of dynamic transition models to estimate the costs and benefits of vaccination strategies for infectious diseases is recommended by the World Health Organization where transmission is predominantly person-to-person, the vaccine reduces infectiousness, and the vaccinated population is important to reduce onwards transmission.63 Dynamic transmission models take into account the indirect benefits of vaccination resulting from lowering the probability of onward transmission, either through the reduction in susceptibility or the potential infectiousness in the uninfected population, also well known as the herd protection effect.64,65 This motivated our choice of a dynamic model framework to examine different vaccination strategies for varicella.
With the inclusion of vaccine failure rates and examining degree of protection and waning in detail, strategies differentiating by the types of vaccines in use can be separately examined in our model. As a result, our results enable policymakers to make informed decisions on subsequent questions related to vaccine choice, consideration of combination vaccines, and consequences of using different vaccines in terms of ease of implementation and uptake, healthcare costs and epidemiological outcomes.
An important aspect of dynamic transmission models is their calibration. An assumption of the dynamic transmission model is that population size is monotonically decreasing with age, and seroprevalence is monotonically increasing with age. New contact rates are then calibrated based on monotonized population and seroprevalence data. Using the calibrated contact rates, the model seroprevalence was derived. This ensured that the model can fit pre-vaccine-era varicella seroprevalence data, and the model is fitted to the data by adjusting contact rates and assuming proportionate mixing. In this case, non-monotonic Italian population data by age were monotonized using a smoothing function while preserving the overall population, and seroprevalence data were monotonized using a linear model starting at 10 years to a final time point of 40 years29,61,66 and used static population age distribution and population size for Italy with the assumption of proportionate mixing. This implementation may overestimate transmission in older people, and alternatives have been suggested, such as empirical or synthetic social contact matrices.30,67,68
The model was parameterized for the Italian setting using a range of data sources, including public reports, peer-reviewed articles, and data assumptions. Aggregating these types of data into a single model introduces uncertainty due to differences in the underlying assumptions associated with the different data.31,33,38 The key data assumptions were around diagnostic testing and treatment. The DSA indicated that the results were not highly sensitive to these. However, they were sensitive to the proportion of cases seeking treatment which is a major driver of costs.
The sensitivity analysis indicated that the results were most sensitive to coverage assumptions. Accurate prediction of coverage rates is a critical factor in proving the overall benefits and cost-effectiveness of vaccination. While epidemiology patterns are unpredictable, the assumptions in the model have been applied consistently across the different strategies, and the PSA and sensitivity analysis indicated that the results were robust under a range of different conditions.
The present study has a potential bias. Firstly, we considered that modifying the strategy from a quadrivalent to a monovalent varicella vaccine in the first vaccination results in a decrease of coverage of 4%. However, we did not consider that when vaccinations are administered by family pediatricians (as in Tuscany) this hypothesized decrease might be significantly reduced if even present. Secondly, there are limited data available comparing Varivax/ProQuad to Varilrix/Priorix-Tetra; however, first, Varivax and ProQuad are generally consider to be immunologically equivalent to each other, as are Varilrix and Priorix-Tetra; second, two head-to-head studies58,69 – one in an outbreak setting in Germany, one in real-word use in Taiwan – both show similar patterns in differences in effectiveness after a single dose as the way that we (and others)49,50,52,68 reflect take and waning in our models. Little is known about the performance of the effectiveness of the two-dose strategies involving Vaccine B and/or Vaccine D when used in long-interval settings, as all the recent clinical trial data51,53 are based on administration of the doses only 3 months apart, rather than several years apart. Data is available on the real-world effectiveness of both Varivax48 and ProQuad70 on long-interval schedules, with results consistent with how they are modelled in this study. However, in all cases, there is the possibility that the performance of any of these vaccines in the Italian epidemiological context could be different than has been seen in other settings, and hence, is a limitation of the study.
Conclusion
Varicella vaccination strategies in general have a major effect on varicella incidence, prevalence, costs, and quality of life. Vaccination provides immediate and long-term benefits to both the vaccinated and unvaccinated population. The model predicts that various two-dose vaccination strategies are cost-saving compared to no vaccination in Italy. The two-dose combination vaccine strategy QQVa is the dominant strategy as it is the most effective and least expensive compared to all other options and should be considered as a candidate for the optimal vaccination strategy for the Italian population.
Abbreviations
DSA, Deterministic sensitivity analysis; MMR, Measles, mumps and rubella; MSEIRS, Maternal/Passive Immunity-Susceptible-Exposed-Infectious-Recovered-Susceptible; MQVa, Vaccine C followed by Vaccine A; MQVb, Vaccine D followed by Vaccine B; NV, No vaccine; OCT, Over the counter; PSA, Probabilistic sensitivity analysis; QALY, Quality-adjusted life years; QQVa, Vaccine A; QQVb, Vaccine B; VZV, Varicella zoster virus®.
Acknowledgments
The authors would like to thank Tracey Weiss and Dana Brown for project management assistance and Matthew Pillsbury for critical review of the manuscript, all employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ USA.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The study was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. The authors take full responsibility for the scope, direction, and content of the manuscript, and have approved the submitted manuscript.
Disclosure
CA, VB, and SG report financial support from Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, RG and EOB are employees of Evidera, Modelling and Simulation, Inc, and participated in the study under contract to Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USAND (at the time of the study), VJD and LJW are employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, who may own stock and/or hold stock options in Merck & Co., Inc., Kenilworth, NJ, USA. The authors report no other conflicts of interest in this work.
References
1. Heininger U, Seward JF. Varicella. Lancet. 2006;368(9544):1365–1376. doi:10.1016/S0140-6736(06)69561-5
2. Sadzot-Delvaux C, Rentier B, Wutzler P, et al. Varicella vaccination in Japan, South Korea, and Europe. J Infect Dis. 2008;197(2):185–190. doi:10.1086/522163
3. Bardach A, Cafferata ML, Klein K, Cormick G, Gibbons L, Ruvinsky S. Incidence and use of resources for chickenpox and herpes zoster in Latin America and the Caribbean–a systematic review and meta-analysis. Pediatr Infect Dis J. 2012;31(12):1263–1268. doi:10.1097/INF.0b013e31826ff3a5
4. Czumbel I, Quinten C, Lopalco P, et al. Management and control of communicable diseases in schools and other child care settings: systematic review on the incubation period and period of infectiousness. BMC Infect Dis. 2018;18(1):199. doi:10.1186/s12879-018-3095-8
5. Gnann J. Varicella-zoster virus: atypical presentations and unusual complications. J Infect Dis. 2002;186(1):S91–S98.
6. Dunkle LM, Arvin AM, Whitley RJ, et al. A controlled trial of acyclovir for chickenpox in normal children. N Engl J Med. 1991;325(22):1539–1544. doi:10.1056/NEJM199111283252203
7. European Centre for Disease Prevention and Control. Guidance for Varicella Vaccination in the European Union; 2015.
8. Marchetti M, Kühnel UM, Colombo GL, Esposito S, Principi N. Cost-effectiveness of adjuvanted influenza vaccination of healthy children 6 to 60 months of age. Hum Vaccin. 2007;3(1):14–22. doi:10.4161/hv.3.1.3657
9. Choo PW, Donahue JG, Manson JE, Platt R. The epidemiology of varicella and its complications. J Infect Dis. 1995;172(3):706–712. doi:10.1093/infdis/172.3.706
10. Krugman S, Goodrich CH, Ward R. Primary varicella pneumonia. N Engl J Med. 1957;257(18):843–848. doi:10.1056/NEJM195710312571801
11. Gogos CA, Bassaris HP, Vagenakis AG. Varicella pneumonia in adults. A review of pulmonary manifestations, risk factors and treatment. Respiration. 1992;59(6):339–343. doi:10.1159/000196084
12. Preblud SR. Varicella: complications and costs. Pediatrics. 1986;78:4.
13. Galil K, Brown C, Lin F, Seward J. Hospitalizations for varicella in the United States, 1988 to 1999. Pediatr Infect Dis J. 2002;21(10):931–934. doi:10.1097/00006454-200210000-00009
14. Fangjun Z, Harpaz R, Jumaan A, et al. Impact of Varicella Vaccination on Health Care Utilization. JAMA. 2005;294(5):7.
15. Robert Koch-Institut. Empfehlungen der Ständigen Impfkommission (STIKO) Robert Koch-Institut. Epidemiol Bull. 2003;2003.
16. Davis MM, Patel MS, Gebremariam A. Decline in varicella-related hospitalizations and expenditures for children and adults after introduction of varicella vaccine in the United States. Pediatrics. 2004;114(3). doi:10.1542/peds.2004-0012
17. Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352(5):450–458. doi:10.1056/NEJMoa042271
18. Lopez A, Zhang J, Brown C, Bialek S. Varicella-related hospitalizations in the United States, 2000–2006: the 1-dose varicella vaccination era. Pediatrics. 2011;127(2):2. doi:10.1542/peds.2010-0962
19. Marin M, Zhang JX, Seward JF. Near elimination of varicella deaths in the US after implementation of the vaccination program. Pediatrics. 2011;128(2):214–220. doi:10.1542/peds.2010-3385
20. Lieu TA, Cochi SL, Black SB. Cost-effectiveness of a routine varicella vaccination program for US children. JAMA. 1994;271(5):375–381. doi:10.1001/jama.1994.03510290057037
21. Kwong JC, Tanuseputro P, Zagorski B, et al. Impact of varicella vaccination on health care outcomes in Ontario, Canada: effect of a publicly funded program? Vaccine. 2008;26(47):6006–6012. doi:10.1016/j.vaccine.2008.08.016
22. Amodio E, Tramuto F, Cracchiolo M, et al. The impact of ten years of infant universal varicella vaccination in Sicily, Italy (2003-2012). Hum Vaccin Immunother. 2015;11(1):236–239. doi:10.4161/hv.36157
23. Pezzotti P, Bellino S, Prestinaci F, et al. The impact of immunization programs on 10 vaccine preventable diseases in Italy: 1900–2015. Vaccine. 2018;36(11):1435–1443. doi:10.1016/j.vaccine.2018.01.065
24. Ministro della Salute. Le novità del decreto legge sui vaccini. 2017.
25. World Health Organization. Principles and Considerations for Adding a Vaccine to a National Immunization Programme from Decision to Implementation and Monitoring; 2014.
26. Wolfson LJ, Daniels VJ, Pillsbury M, et al. Cost-effectiveness analysis of universal varicella vaccination in Turkey using a dynamic transmission model. PLoS One. 2019;14(8):e0220921. doi:10.1371/journal.pone.0220921
27. Castillo-Chavez C, Hethcote HW, Andreasen V, Levin SA, Liu WM. Epidemiological models with age structure, proportionate mixing, and cross-immunity. J Math Biol. 1989;27(3):233–258. doi:10.1007/BF00275810
28. World Health Organization. WHO vaccine-preventable diseases: monitoring system 2018. Available from: http://apps.who.int/immunization_monitoring/globalsummary/countries?Countrycriteria%5Bcountry%5D%5B%5D=ITA.
29. Department of Economic and Social Affairs. Population Prospects: The 2017 Revision. United Nations: Population Division; 2017.
30. Fumanelli L, Ajelli M, Manfredi P, Vespignani A, Merler S. Inferring the structure of social contacts from demographic data in the analysis of infectious diseases spread. PLoS Comput Biol. 2012;8(9):e1002673. doi:10.1371/journal.pcbi.1002673
31. Agenzia Nazionale per i Servizi Sanitari Regionali. Tariffario Prestazioni Sanitarie Specialistiche Ambulatoriali - Visita Generale Agenzia Nazionale per i Servizi Sanitari Regionali; 2014.
32. Azzari C, Massai C, Poggiolesi C, et al. Cost of varicella-related hospitalisations in an Italian paediatric hospital: comparison with possible vaccination expenses. Curr Med Res Opin. 2007;12:2945–2954. doi:10.1185/030079907X242610
33. Trucchi C, Gabutti G, Rota MC, Bella A. Burden of varicella in Italy, 2001–2010: analysis of data from multiple sources and assessment of universal vaccination impact in three pilot regions. J Microbiol. 2015;64(11):1387–1394.
34. Morandi DI. Prestazioni specialistiche ambulatoriali Confronto tra le tariffe nazionale. Agenzia Nazionale per i Servizi Sanitari Regionali; 2014.
35. Boccalini S, Bonanni P, Bechini A. Preparing to introduce the varicella vaccine into the Italian immunisation programme: varicella-related hospitalisations in Tuscany, 2004-2012. Euro Surveill. 2016;21(24). doi:10.2807/1560-7917.ES.2016.21.24.30257
36. Ministero dell’Economia e delle Finanze. Libro verde della spesa pubblica 2007 - aggiornato con l’indice dei prezzi al consumo Ministero dell’Economia e delle Finanze. 2007.
37. Agenzia Nazionale per i Servizi Sanitari Regionali. Tariffario Prestazioni Sanitarie Specialistiche Ambulatoriali - Radiografia del torace di routine Agenzia Nazionale per i Servizi Sanitari Regionali. 2014.
38. Coudeville L, Brunot A, Giaquinto C, Lucioni C, Dervaux B. Varicella vaccination in Italy - an economic evaluation of different scenarios. PharmacoEconomics. 2004;22(13):839–855. doi:10.2165/00019053-200422130-00003
39. EuroStat. Retribuzioni e costo del lavoro. 2018.
40. Farmadati online database, Available from: https://www.farmadati.it/.
41. National Law N. 386/1974, included in the National Official Bulletin “GU Serie Generale n.225 del 29-08-1974”, art. N. 9, Link: https://www.gazzettaufficiale.it/eli/id/1974/08/29/074U0386/sg
42. Schink T, Holstiege J, Kowalzik F, Zepp F, Garbe E. Risk of febrile convulsions after MMRV vaccination in comparison to MMR or MMR+V vaccination. Vaccine. 2014;32(6):645–650. doi:10.1016/j.vaccine.2013.12.011
43. Ma S-J, Xiong Y-Q, Jiang L-N, Chen Q. Risk of febrile seizure after measles-mumps-rubella-varicella vaccine: a systematic review and meta-analysis. Vaccine. 2015;33(31):3636–3649. doi:10.1016/j.vaccine.2015.06.009
44. Kowalzik F, Faber J, Knuf M. MMR and MMRV vaccines. Vaccine. 2018;36(36):5402–5407. doi:10.1016/j.vaccine.2017.07.051
45. Gabutti G, Kuhdari P, Ferioli S, Trucchi C. Hospital admissions for seizure in Italy: a decennial retrospective analysis with a special focus on the burden in the pediatric age. Neurol Sci. 2015;36(9):1667–1673. doi:10.1007/s10072-015-2230-1
46. Christensen H, Trotter CL. Modelling the cost-effectiveness of catch-up ‘MenB’ (Bexsero) vaccination in England. Vaccine. 2017;35(2):208–211. doi:10.1016/j.vaccine.2016.11.076
47. Supplemento Ordinario n.8 alla Gazzetta Ufficiale n.23 - Tariffe delle prestazioni di assistenza ospedaliera per acuti - Convulsioni e cefalea. 2012
48. Kuter B, Matthews H, Shinefield H, et al. Ten Year Follow-up of Healthy Children Who Received One or Two Injections of Varicella Vaccine. Pediatr Res. 2004;23(2):132–137.
49. Holl K, Sauboin C, Amodio E, Bonanni P, Gabutti G. Coverage, efficacy or dosing interval: which factor predominantly influences the impact of routine childhood vaccination for the prevention of varicella? A model-based study for Italy. BMC Public Health. 2016;16(1):1103. doi:10.1186/s12889-016-3738-x
50. Ouwens MJNM, Littlewood KJ, Sauboin C, et al. The impact of 2-dose routine measles, mumps, rubella, and varicella vaccination in France on the epidemiology of varicella and zoster using a dynamic model with an empirical contact matrix. Clin Ther. 2017;37(4):816–829. doi:10.1016/j.clinthera.2014.12.017
51. Prymula R, Riise Bergsaker M, Esposito S, et al. Protection against varicella with two doses of combined measles-mumps-rubella-varicella vaccine versus one dose of monovalent varicella vaccine: a multicentre, observer-blind, randomised, controlled trial. Lancet. 2014;383(9925):1313–1324. doi:10.1016/S0140-6736(12)61461-5
52. Sauboin C, Holl K, Bonanni P, et al. The impact of childhood varicella vaccination on the incidence of herpes zoster in the general population: modelling the effect of exogenous and endogenous varicella-zoster virus immunity boosting. BMC Infect Dis. 2019;19(1):126. doi:10.1186/s12879-019-3759-z
53. Povey M, Henry O, Riise Bergsaker MA, et al. Protection against varicella with two doses of combined measles-mumps-rubella-varicella vaccine or one dose of monovalent varicella vaccine: 10-year follow-up of a Phase 3 multicentre, observer-blind, randomised, controlled trial. Lancet Infect Dis. 2019;19(3):287–297. doi:10.1016/S1473-3099(18)30716-3
54. Quinn HE, Gidding HF, Marshall HS, et al. Varicella vaccine effectiveness over 10 years in Australia; moderate protection from 1-dose program. J Infect. 2019;78(3):220–225. doi:10.1016/j.jinf.2018.11.009
55. Zhu S, Zeng F, Xia L, He H, Zhang J. Incidence rate of breakthrough varicella observed in healthy children after 1 or 2 doses of varicella vaccine: results from a meta-analysis. Am J Infect Control. 2018;46(1):e1–e7. doi:10.1016/j.ajic.2017.07.029
56. Yin M, Xu X, Liang Y, Ni J. Effectiveness, immunogenicity and safety of one vs. two-dose varicella vaccination: a meta-analysis. Expert Rev Vaccines. 2018;17(4):351–362. doi:10.1080/14760584.2018.1433999
57. Marin M, Marti M, Kambhampati A, Jeram SM, Seward JF. Global varicella vaccine effectiveness: a meta-analysis. Pediatrics. 2016;137(3):e20153741. doi:10.1542/peds.2015-3741
58. Cheng H, Chang L, Lu C, Huang L. Epidemiology of breakthrough varicella after the implementation of a universal varicella vaccination program in Taiwan, 2004–2014. Sci Rep. 2018;8(1):1. doi:10.1038/s41598-018-35451-y
59. Littlewood KJ, Ouwens MJ, Sauboin C, Tehard B, Alain S, Denis F. Cost-effectiveness of routine varicella vaccination using the measles, mumps, rubella and varicella vaccine in France: an economic analysis based on a dynamic transmission model for varicella and herpes zoster. Clin Ther. 2015;37(7):830–841. doi:10.1016/j.clinthera.2015.01.006
60. Attema AE, Brouwer W, Claxton K. Discounting in economic evaluations. PharmacoEconomics. 2018;36(7):745–758. doi:10.1007/s40273-018-0672-z
61. Gabutti G, Rota MC, De Donno A, et al. Sero-epidemiology of VZV infection in Italy: impact evaluation of extensive vaccination. Epidemiol Prev. 2014;38(6):57–61.
62. World Health Organization. Weekly epidemiological record 2014
63. World Health Organization. Guide for Standardization of Economic Evaluations of Immunization Programmes; 2008.
64. Centers for Disease Control and Prevention. Direct and Indirect Effects of Routine Vaccination of Children with 7-Valent Pneumococcal Conjugate Vaccine on Incidence of Invasive Pneumococcal Disease–United States, 1998–2003; 2005.
65. Drolet M, Bénard É, Boily M-C, et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2015;15(5):565–580. doi:10.1016/S1473-3099(14)71073-4
66. Department of Economic and Social Affairs. Birth by Age of Mother - World Population Prospects: 2017 Revision. United Nations: Population Division; 2017.
67. Hoang TV, Coletti P, Melegaro A, et al. A systematic review of social contact surveys to inform transmission models of close contact infections. BioRxiv. 2018.
68. van Hoek AJ, Melegaro A, Gay N, Bilcke J, Edmunds WJ. The cost-effectiveness of varicella and combined varicella and herpes zoster vaccination programmes in the United Kingdom. Vaccine. 2012;30(6):1225–1234. doi:10.1016/j.vaccine.2011.11.026
69. Spackova M, Wiese-Posselt M, Dehnert M, Matysiak-Klose D, Heininger U, Siedler A. Comparative varicella vaccine effectiveness during outbreaks in day-care centres. Vaccine. 2010;28(3):686–691. doi:10.1016/j.vaccine.2009.10.086
70. Giaquinto C, Gabutti G, Baldo V, et al. Impact of a vaccination programme in children vaccinated with ProQuad, and ProQuad-specific effectiveness against varicella in the Veneto region of Italy. BMC Infect Dis. 2018;18(1):103. doi:10.1186/s12879-018-3017-9
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.