Back to Journals » Clinical Ophthalmology » Volume 8
The comparison of intravitreal triamcinolone and bevacizumab in patients with macular edema secondary to branch retinal vein occlusion
Authors Gokce G, Sobaci G, Durukan AH, Erdurman FC
Received 29 November 2013
Accepted for publication 18 December 2013
Published 7 February 2014 Volume 2014:8 Pages 355—362
DOI https://doi.org/10.2147/OPTH.S58468
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Gokcen Gokce,1 Gungor Sobaci,2 Ali Hakan Durukan,2 Fazil Cuneyt Erdurman3
1Department of Ophthalmology, Sarikamis Military Hospital, Kars, Turkey; 2Faculty of Medicine, Department of Ophthalmology, Gulhane Military Medical Academy, Ankara, Turkey; 3Department of Ophthalmology, Canakkale Military Hospital, Canakkale, Turkey
Purpose: This study was conducted to compare the efficacy and safety of intravitreal triamcinolone acetonide (IVTA) and intravitreal bevacizumab (IVB) in the treatment of macular edema related to branch retinal vein occlusion (BRVO), using the new optical coherence tomography parameters.
Material and methods: The medical records of 62 patients (IVTA n=26; IVB n=36) with macular edema secondary to BRVO and at least 12 months follow-up between 2007 and 2011 were evaluated by within-group and inter-group comparisons.
Results: Both groups were similar in terms of demographic characteristics (P>0.05). Best corrected visual acuity (BCVA) improvement and central subfoveal thickness (CST) reduction were significantly higher in the IVTA group at only the third month (P<0.05). In nonischemic BRVO, while BCVA improvement was significantly higher in the IVTA group at the third and sixth months (P<0.05), no significant difference was found in CST reduction at all visits (P>0.05). In ischemic BRVO, no significant difference was found in BCVA improvement at all visits, but CST reduction was significantly higher in the IVTA group at the first and third months. Logarithmic optical coherence tomography change (LogOCTc) and relative change in retinal thickness (RCRT) showed the same levels of significance in the comparisons. Relative change in retinal thickening (RCRTing) was more valuable compared to the other parameters in the subgroup analyses.
Conclusion: There was no difference between groups at the 12th month. IVTA was more efficient than IVB in regard to BCVA improvement in nonischemic BRVO in the early follow-up. IVTA made significant retinal thinning compared to IVB in ischemic BRVO in the early period. RCRTing and LogOCTc are important parameters used to monitor the response to treatment in BRVO. Because of the similar levels of significance, RCRT and LogOCTc can be used interchangeably.
Keywords: branch retinal vein occlusion, bevacizumab, macular edema, triamcinolone
Introduction
The most common cause of vision loss during branch retinal vein occlusion (BRVO) is the development of macular edema (ME) at any stage of the disease. Currently there is no effective and commonly accepted treatment method for BRVO-related ME, although limited benefits were reported with grid laser photocoagulation.1 Anti-vascular endothelial growth factor agents and corticosteroids compete with each other in the treatment of BRVO, as they do in many other retinal diseases. Although studies have tried to demonstrate the advantages or disadvantages of each treatment type, no clear conclusion has been reached.2,3
The purpose of this study was to compare the efficacy and safety of intravitreal triamcinolone acetonide (IVTA) and intravitreal bevacizumab (IVB) in the treatment of ME related to BRVO, to provide a framework for the future treatment of patients.
Materials and methods
We conducted a retrospective study of consecutive patients at our clinic who had been treated off-label with intravitreal drugs triamcinolone or bevacizumab for BRVO-related ME and who were followed-up for at least 12 months between 2007 and 2011.
This study adhered to the tenets of the Declaration of Helsinki. It was approved by the Ethical Committee of Gulhane Military Medical Academy and informed consents had been obtained from the patients. We included patients who had best corrected visual acuity (BCVA) worse than 0.09 logarithm of minimal angle of resolution (LogMAR) unit and/or central subfoveal thickness (CST) of at least 300 μm with leakage on fluorescein angiography (FA) secondary to BRVO-related ME, who were treated with one of the intravitreal drugs (IVTA or IVB), and who had regular follow-ups during the 12 months after treatment. Patients were excluded from the study if they had initial findings or medical history of a) amblyopia, b) previous treatment of macular lesion including ME of other etiologies, c) chronic ME of 6 months duration or more, d) macular ischemia at a distance greater than a 6 clock-hour sector of the optical disc diameter from the foveal center on FA,4 e) anterior or other posterior segment disease that presumably affects BCVA and/or CST, f) ME in both eyes, g) previous laser photocoagulation either focal/grid, or panretinal within 3 months of the injection, h) BRVO with active neovascularization needing laser photocoagulation at first presentation, i) intraocular surgery during the previous 3 months, j) glaucoma, or k) switch to other drug(s) and/or laser because of unresponsiveness to the initial drug treatment during 12-month follow-up period.
All patients underwent a thorough ophthalmic examination including Goldmann aplanation tonometry, FA (Heidelberg Retinal Angiogram-2; Heidelberg Engineering GmBH, Dossenheim, Germany) and optical coherence tomography (OCT) (Stratus III OCT™; Carl Zeiss Meditec AG, Jena, Germany) at presentation to the hospital. These were repeated at each visit, except that FA was performed when needed. ME was defined as an OCT-based CST of at least 300 μm with leakage on FA.
Patients meeting both the inclusion and the exclusion criteria were divided into two groups according to the intravitreal drug used: IVTA (4 mg/0.1 mL – Kenacort®-A 40; Bristol-Myers Squibb, New York, NY, USA) injections; and IVB (1.25 mg/0.05 mL – Avastin®; Genentech, Inc., South San Francisco, CA, USA) injections. Injection techniques are detailed elsewhere.1,2 Treatments were repeated in patients with a lack of visual and anatomical stability at the control examinations, a one-row or more decline in BCVA, a CST value at or above 300 μm as measured by OCT, an increase in subretinal fluid accumulation that decreased during follow-ups, or presence of any leakage on FA. Retreatments were performed on an as-needed basis. At the first monthly control examination, for the patients with CST values <250 μm or BCVA values higher than 0.09 LogMAR unit, the minimum interval for a new control or deciding a new injection was 12 weeks for IVTA and 6 weeks for IVB; all other patients underwent monthly control examinations. Patients with no improvement in BCVA or with no reduction or with an increase in CST values despite three injections were considered to be treatment-resistant (defined as decrease in BCVA >0.1 LogMAR unit of initial LogMAR-Visual Acuity [VA] and increase in CST >0.1 log unit of initial LogOCT), and they were not given new injections with the same agent.
Patients were evaluated as belonging to the ischemic group if they had capillary perfusion defects larger than five optical disc diameters at presentation.5 The OCT scans of patients were performed using the Stratus III OCT™ in the Macular Thickness Map mode. The CST was recorded as the center point thickness provided by the Stratus software. Scans with resolutions >7 were considered for evaluation. A mean of two successive examinations performed by the same examiner were taken into consideration as CST.
The primary outcome measure was the change in BCVA measured by the Snellen chart 1 month, 3 months, 6 months, and 12 months after the treatment. Snellen values were converted to LogMAR equivalent. The secondary evaluation criterion was the variation in CST values. The following parameters were selected for evaluation:6
- CST: The distance between the inner limiting membrane and the retinal pigment epithelium within an area of 1 mm2 in the central region
- Retinal thickening (RT): Obtained by subtracting the CST value from the normal value (212±20 μm) identified in studies conducted using Stratus III OCT™7
- Absolute change in retinal thickness (ACRT) = pretreatment CST – CST at the month of control
- Relative change in retinal thickness (RCRT) = ([pretreatment CST – CST at the month of control]/pretreatment CST) ×100%
- Relative change in retinal thickening (RCRTing) = ([pretreatment CST – CST at the month of control]/pretreatment RT) ×100%
- Logarithm of central macular thickness (LogOCT): the logarithm of the CST value obtained with base 212, which is the average of the normal population;8 (If CST =212, then LogOCT =0)
- Logarithmic OCT change (LogOCTc) = LogOCT at the month of control – pretreatment LogOCT.
For visual acuity comparisons within the groups, changes in LogMAR values compared to those obtained pretreatment values were used (LogMAR-VAc = LogMAR-VA at the month of control – pretreatment LogMAR-VA).
In statistical comparisons, the normal distribution was checked using the Kolmogorov–Smirnov test. The chi-square and/or Fisher’s exact tests were used for discrete variables. The Mann–Whitney U test was administered for continuous variables. The Wilcoxon test was used to compare dependent groups. The Spearman correlation test was used for correlation analysis. SPSS for Windows (Version 16.0.1; SPSS Inc., Chicago, IL, USA) was used for the statistical analysis, and P<0.05 was considered significant.
Results
Sixty-two consecutive patients who had been treated off-label with intravitreal drugs triamcinolone (26 patients) and bevacizumab (36 patients) were analyzed in this study. The demographic and clinical characteristics of the patients were not significantly different between groups (P>0.05) (Table 1).
Within-group response to treatment
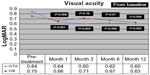
Monthly averages of BCVA values in the group that received IVTA are shown in Figure 1. Significant increase was observed in the BCVA level in all months after injection compared to the initial level (P<0.01). Monthly averages of BCVA values in the group that received IVB are also shown in Figure 1. Significant increase in BCVA levels in months 1, 6, and 12 compared to the initial level (P<0.05) was observed; however, the better BCVA in month 3 observed in this group was not statistically significant. Because the BCVA level in month 3 was lower than the level measured in month 1, the mean BCVA values obtained in months 6 and 12 were found to be significantly higher compared to the value in month 3 (P<0.05).
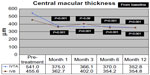
The monthly averages of CST values in the group that received IVTA are shown in Figure 2. A significant decrease in all months compared to the pretreatment CST values was observed (P<0.001). The value obtained in month 12 was significantly lower than that measured in month 6 (P=0.01). The monthly average CST values in the group that received IVB are also shown in Figure 2. A significant decrease in months 1, 6, and 12 compared with the pretreatment CST values was observed (P<0.001). Importantly, the CST in month 3 was significantly increased compared with month 1 (P=0.01). Correspondingly, the average CST values obtained in months 6 and 12 were significantly lower than the CST value measured in month 3 (P<0.01).
Comparison of the response to treatment between groups
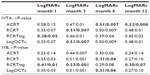
When eyes were compared according to the change in BCVA levels and CST parameters, a larger decrease in CST values and a larger increase in BCVA levels in all months were observed in the IVTA group compared to the IVB group. The differences in all CST parameters and the BCVA level were found to be significant compared to pretreatment values (P<0.05) only in month 3 (Table 2).
Comparison of the response to treatment in patients with nonischemic BRVO
When nonischemic eyes were compared (within groups) according to the change in BCVA level from the pretreatment, a statistically significant increase was observed in the visual acuity of the IVTA group in all months (P=0.01). In contrast, a significant increase was observed only in months 6 and 12 for the eyes that underwent IVB (P<0.05). According to the change in CST parameters from pretreatment values, a statistically significant decrease in CST was observed in the IVTA group in all months. In the IVB group, a significant decrease in CST was observed in all of the follow-ups except for month 3 (P<0.01).
When the groups were compared (between groups) according to the change in the BCVA level from the pretreatment level, a larger increase in the BCVA level was observed in the IVTA group. This difference was significant in months 3 and 6. According to the change in CST compared with the pretreatment level, the IVTA group was observed to have a larger decrease in CST in all months, but this change was not significant in any follow-ups (P>0.05).
Comparison of the response to treatment in patients with ischemic BRVO
When patients with ischemic BRVO were compared (within groups) according to the change in BCVA levels from the pretreatment levels, a statistically significant increase (P=0.01) was observed in the visual acuity of the IVTA group in month 1. In contrast, in the eyes that underwent IVB, no significant increase was observed at any of the follow-ups; only the increase in visual acuity in month 1 was close to significance (P=0.05). According to the change in CST values from the pretreatment levels, a statistically significant decrease (P<0.01) in CST was observed in the IVTA group in all months. In contrast, the decrease in CST obtained in the IVB group was not significant at any of the follow-ups.
When eyes were compared (between groups) according to the amount of change in BCVA levels from pretreatment levels, a larger increase in BCVA in all months was observed in the IVTA group, but this difference was not significant at any of the follow-ups (P>0.05). According to the change in CST parameters from the pretreatment levels, the IVTA group was observed to have a larger decrease in CST in all months. This change was significant for all parameters in month 3 and for all parameters except RCRTing in month 1 (P<0.05).
Injection numbers
The average injection number was significantly higher in the IVB-injected group (P<0.001) (Table 1).
Correlation between the variations in BCVA and CST
The correlation of the monthly variation in BCVA levels and CST parameters showed that in the IVTA group, RCRTing had the highest correlation in month 1, whereas LogOCTc and RCRT had the highest correlation in month 3, and ACRT was prominent thereafter. In the IVB group, RCRTing had the highest correlation values in months 1, 3, and 12, and LogOCTc and RCRT had the highest correlation values in month 6. Although a better correlation pattern was observed in the IVB group compared to the IVTA group in months 1 and 3, the IVTA group exhibited a better pattern in months 6 and 12. However, the correlation coefficients (r values) of groups were found to be low (Table 3).
Intravitreal injection-related complications
According to Goldmann applanation tonometry measurements performed within a week of injection, the average intraocular pressure (IOP) level was found to be 26.12 mmHg in the IVTA group and 17.11 mmHg in the IVB group (P<0.001). The IOP level increased to ≥30 mmHg (P=0.001) in 26.9% of the patients in the IVTA group and to ≥21 mmHg in 53.8% of the same group (P=0.007). The patients with an IOP level >30 mmHg were given topical medication to keep the IOP level under control, but three patients (11%) developed glaucoma as detected by clinical examination. Three patients with an IOP level >40 mmHg were required to receive systemic antiglaucomatous treatment. The IOP level did not increase to 30 mmHg in any patient in the IVB group. The highest value measured was 28 mmHg in this group. In the IVB group, 19.4% of the patients were observed to have IOP levels ≥21 mmHg. No glaucoma development was observed in the patients in the IVB group.
At the final follow-up examination, 23.1% of the patients in the IVTA group were found to have developed a cataract. This percentage was 5.6% in the IVB group (P=0.05).
Discussion
With the recent widespread use of IVTA and IVB to treat ME associated with BRVO, the comparison of these agents has become important for clinicians. Most of the studies conducted thus far have failed to show which of the two agents is more effective. This study aimed to compare the effectiveness of IVTA and IVB and also aimed to determine the necessary parameters of OCT, which is the primary test to evaluate the effectiveness of treatment.
There are many variable results from different sources regarding the treatment of ME due to BRVO with IVTA injection.9–15 In our study, we found an increase in BCVA levels of 0.19 LogMAR in month 1, 0.23 LogMAR in month 3, 0.22 LogMAR in month 6 and 0.24 LogMAR in month 12 in patients treated with IVTA. All values were found to be statistically significant with respect to pretreatment values. In our study, an increase of BCVA obtained with 4 mg IVTA in month 6 was found to be equal to the gain obtained with 20 mg IVTA in the study of Jonas et al,10 which included only nonischemic BRVO cases, and was found to be higher than the gain obtained with 4 mg in month 5 in the study of Lee et al.14 In our study, increases of 0.20 LogMAR in month 1, 0.30 LogMAR in months 3 and 6, and 0.31 LogMAR in month 12 were achieved in patients with nonischemic BRVO. These increases were statistically significant in all follow-up months. The values of our month 3 results for the nonischemic group were found to be similar to those of Cheng and Wu9 and greater than those of Jonas et al.10 Increases of 0.19 LogMAR in month 1, 0.18 LogMAR in month 3, 0.15 LogMAR in month 6, and 0.19 LogMAR in month 12 were observed in patients with ischemic BRVO. Of these results, only the increase obtained in month 1 was significant with respect to the pretreatment levels and was found to be higher than that in the ischemic group of Chen et al.15
In two studies of BRVO cases treated with IVB, the BCVA value increased from 0.5 to 0.2 LogMAR at the end of a 12-month follow-up.16,17 According to the study of Jaissle et al,16 a 39% decrease in CST at the end of month 10 and an increase of 0.3 LogMAR with IVB was reported. In another study, Kondo et al17 observed an increase in BCVA of 0.27 LogMAR at month 12 and a 47% decrease in CST with an average of 2 IVB injections. However, with an average of 2.83 injections, an average increase in BCVA of 0.12 LogMAR at the end of month 12 and a decrease in CST of 17.6% were observed in our study. Gutiérrez et al18 observed a significant increase of 0.53 LogMAR in month 6 compared to the pretreatment value and a 31.7% decrease in CST. With IVB, an increase of 0.08 LogMAR in month 6 and a decrease in CST of 17.6% were observed in our study and the observed increase in BCVA and the decrease in CST with respect to pretreatment values in the IVB group were found to be lower than in the other studies on this subject.
In many studies comparing IVB and IVTA treatment in ME due to BRVO, no significant differences were observed between the groups. According to Guthoff et al,19 the BCVA level in the IVB group was found to be significantly higher than in the IVTA group in month 2. However, this difference was not significant, even though the IVB group had higher levels at the final follow-up. In the study of Byun et al,3 similar to the study of Cheng et al,2 no significant differences in BCVA and CST values were observed between the two groups in month 12. Considering the risks caused by the increased cost and number of injections, IVTA was found to be superior.3 In our study, significant difference in BCVA and CST was observed in month 3 in favor of IVTA, but similar to these studies, no significant difference was found at the final follow-up. When the same comparison was performed in nonischemic BRVO patients, a significant difference in BCVA levels was observed in months 3 and 6. The changes in CST were not found to be significant at any of the follow-ups. In ischemic BRVO, no significant difference was observed in BCVA between the two groups, but the amount of change in CST was found to be significant in the first 3 months. Additionally, a continuous increase in visual acuity in subsequent follow-ups as a result of repeated injections after the increase obtained in the first month was observed in both IVB- and IVTA-injected BRVO patients. Accordingly, we agree with the hypothesis of Hsu et al,20 which suggests that a better response could be obtained in the following months (unless a response was achieved during the first months) with IVB treatment in patients with Central Retinal Vein Occlusion. However, we think that the theory of Hsu et al20 may be valid for BRVO.
In our study, parameters of OCT that were not used in previous studies of BRVO groups but that were defined recently in the treatment of diabetic ME were also correlated with changes in BCVA. Although OCT parameters of ACRT and RCRT have been used in previous BRVO studies, our study added the LogOCTc, RT, and RCRTing parameters. The purpose of using these parameters was to analyze the obtained anatomical and functional success more objectively. Chan and Duker21 suggested the use of RCRTing in the evaluation of ME associated with any type of retinal disease. In a study that evaluated diabetic ME with OCT, this parameter was used to assess the degree of approximation to normal for retinal thickening (not retinal thickness) after treatment.6 In the same study, RCRTing yielded unstable results when the pretreatment level of RT was lower. Therefore, when the pretreatment CST value was relatively low, ACRT was used due to its stability, and when this value was high, RCRTing was considered to be more appropriate to use. Normal CST values in the selected population are required for the measurement of RT and RCRTing. Because these values may vary according to age, sex, and race, the normal values determined in studies may not be appropriate for every population. Accordingly, the measurement of LogOCT was also included in our study. All of the studies on LogOCT were performed in patients with ME due to diabetic retinopathy.8 Thus, our study is the first study using LogOCT to assess ME due to BRVO. The main advantage of LogOCT is its compatibility with LogMAR, because the calculation methods are the same.
All of the OCT parameters were used in the correlation analysis of the change in BCVA in our study. However, different results were obtained between the two groups in the correlation analysis of the change in BCVA. The RCRTing was the most highly correlated with BCVA change in the IVB group, in months 1, 6, and 12. In the IVTA group, RCRTing became prominent in month 1, whereas LogOCTc and RCRT were prominent in month 3, and ACRT was prominent thereafter. Contrary to the literature, we think that the sensitivity and specificity of the OCT parameters defined for the follow-up of diabetic ME are not only related to the initial CST value but also to the applied treatment. Without separation into subgroups, all CST parameters displayed a consistent level of statistical significance in our study. However, this consistency deteriorated when the calculations were performed according to subgroups, such as ischemic–nonischemic. RCRTing was more valuable compared to the other parameters in the subgroup analyses. Therefore, this parameter appeared to be more valuable in the subgroup analyses in which the numbers decreased.
In our study, a remarkable observation was made, namely, that LogOCTc and RCRT showed the same levels of significance in the comparisons (Table 2). Despite the different formulas used in the calculations, because the same P-value was achieved with these two parameters, they can be used as alternatives to one another in independent intergroup analyses of CST changes in retinal diseases.
Complications due to intravitreal injections have always been a subject of debate in the comparison of the efficacy of treatment agents. In many studies, it appears that IVTA results in more complications compared to IVB. Guthoff et al19 found that the posttreatment IOP level was >30 mmHg in 60% of patients treated with IVTA. Chen et al22 reported that the IOP level was >21 mmHg in 32% of the BRVO patients treated with IVTA. In IVTA-treated patients, an IOP level of ≥30 mmHg was observed in 26.9% and an IOP level of ≥21 mmHg was observed in 53.8% in our study. With antiglaucomatous treatment, control levels were achieved in all patients, with IOP levels ≥30 mmHg; therefore, no patient required filtration surgery. However, the development of open-angle glaucoma was observed in three patients injected with IVTA. After IVB treatment, an IOP level >30 mmHg was not observed in any of the cases, and an IOP level of ≥21 mmHg was observed in 19.4%.
Cataract development is an important complication related to IVTA injection and was reported in 24% of BRVO patients by Guthoff et al.19 Chen et al22 reported a 28% rate of development of cataract after IVTA. In our study, the rate of cataract development was found to be 23.1% in the IVTA group. After IVB injection, a 5.6% rate of cataract development was observed.
The main weaknesses of our study included failure to provide complete ideal randomization, due to the retrospective nature of our study, and the fact that the socioeconomic levels of the patients may have influenced the timing and method of treatment. However, we think that these weaknesses, which may affect our results, are minimized by including a sufficient number of cases and by applying broad exclusion criteria for the study. We did not obtain significant differences between the groups according to demographic and clinical characteristics of patients. The indications for treatment and follow-up were utilized by the same experts for 4 years, the same application criteria and doses were used and the FA and OCT used for follow-ups were performed by the same team with the same devices. These other factors increase the strength of our study.
Duration of ME might be a possible risk factor that can be taken into account meaningfully when deciding on a course of treatment. However duration of ME is part of a patient’s history-dependent data and obtaining reliable and definite data may be influenced by the socioeconomic levels of the patients. Thus, we did not obtain data regarding the exact duration of ME in each patient. We excluded the patients with chronic ME of ≥6 months duration by checking their recordings and history instead.
Another weakness in our study design is the fact that a time domain OCT unit was used. The main limitations of time domain OCT include slow acquisition speed and lower resolution. Spectral domain OCT machines provide better images but they take a longer time to obtain useful data. A recent study by Hatef et al23 showed that both stratus OCT and spectral domain OCT demonstrated high intraclass repeatability. The main advantage of spectral domain OCT over the stratus OCT was found to be in its ability to obtain images with more detail and detect small changes in the normal anatomy of the retina.23 It was stated that stratus OCT can obtain reliable and useful clinical data about the progression and regression of the ME. Using the same device with the same mode for all patients at all visits was the main advantage for overcoming this possible weakness in our study.
Conclusion
IVTA was more effective than IVB in the early period, but no significant difference between groups was found at the final visit. IVTA induced significant retinal thinning compared to IVB in ischemic BRVO in the first 3 months. Higher IOP levels and cataract development have to be seriously considered in IVTA injections in BRVO. RCRTing and LogOCTc are important parameters used to monitor the response to treatment in BRVO. Because of the similar levels of significance, RCRT and LogOCTc can be used interchangeably. Other treatment modalities like ranibizumab or combination of IVTA and IVB should also be considered in the treatment of BRVO-related ME.
Disclosure
The authors report no conflicts of interest in this work. No financial support was received for this submission.
References
The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984;98(3):271–282. | |
Cheng KC, Wu WC, Chen KJ. Intravitreal triamcinolone acetonide vs bevacizumab for treatment of macular oedema secondary to branch retinal vein occlusion. Eye (Lond). 2009;23(11):2023–2033. | |
Byun YJ, Roh MI, Lee SC, Koh HJ. Intravitreal triamcinolone acetonide versus bevacizumab therapy for macular edema associated with branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2010;248(7):963–971. | |
Finkelstein D. Ischemic macular edema. Recognition and favorable natural history in branch vein occlusion. Arch Ophthalmol. 1992;110(10):1427–1434. | |
Branch Vein Occlusion Study Group. Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. A randomized clinical trial. Arch Ophthalmol. 1986;104(1):34–41. | |
Browning DJ, Glassman AR, Aiello LP, et al. Diabetic Retinopathy Clinical Research Network. Optical coherence tomography measurements and analysis methods in optical coherence tomography studies of diabetic macular edema. Ophthalmology. 2008;115(8):1366–1371, 1371. e1. | |
Chan A, Duker JS, Ko TH, Fujimoto JG, Schuman JS. Normal macular thickness measurements in healthy eyes using Stratus optical coherence tomography. Arch Ophthalmol. 2006;124(2):193–198. | |
Ferris FL, Miller KM, Glassman AR, Beck RW. Diabetic Retinopathy Clinical Research Network. A proposed method of logarithmic transformation of optical coherence tomography data for use in clinical research. Ophthalmology. 2010;117(8):1512–1516. | |
Cheng KC, Wu WC. Intravitreal triamcinolone acetonide for patients with macular edema due to branch retinal vein occlusion. Kaohsiung J Med Sci. 2006;22(7):321–330. | |
Jonas JB, Akkoyun I, Kamppeter B, Kreissig I, Degenring RF. Branch retinal vein occlusion treated by intravitreal triamcinolone acetonide. Eye (Lond). 2005;19(1):65–71. | |
Krepler K, Ergun E, Sacu S, et al. Intravitreal triamcinolone acetonide in patients with macular oedema due to branch retinal vein occlusion: a pilot study. Acta Ophthalmol Scand. 2005;83(5):600–604. | |
Ozkiris A, Evereklioglu C, Erkilic K, Dogan H. Intravitreal triamcinolone acetonide for treatment of persistent macular oedema in branch retinal vein occlusion. Eye (Lond). 2006;20(1):13–17. | |
Ozkiris A, Evereklioglu C, Erkiliç K, Ilhan O. The efficacy of intravitreal triamcinolone acetonide on macular edema in branch retinal vein occlusion. Eur J Ophthalmol. 2005;15(1):96–101. | |
Lee H, Shah GK. Intravitreal triamcinolone as primary treatment of cystoid macular edema secondary to branch retinal vein occlusion. Retina. 2005;25(5):551–555. | |
Chen SD, Lochhead J, Patel CK, Frith P. Intravitreal triamcinolone acetonide for ischaemic macular oedema caused by branch retinal vein occlusion. Br J Ophthalmol. 2004;88(1):154–155. | |
Jaissle GB, Leitritz M, Gelisken F, Ziemssen F, Bartz-Schmidt KU, Szurman P. One-year results after intravitreal bevacizumab therapy for macular edema secondary to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2009;247(1):27–33. | |
Kondo M, Kondo N, Ito Y, et al. Intravitreal injection of bevacizumab for macular edema secondary to branch retinal vein occlusion:results after 12 months and multiple regression analysis. Retina. 2009;29(9):1242–1248. | |
Gutiérrez JC, Barquet LA, Caminal JM, et al. Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to retinal vein occlusion. Clin Ophthalmol. 2008;2(4):787–791. | |
Guthoff R, Meigen T, Hennemann K, Schrader W. Comparison of bevacizumab and triamcinolone for treatment of macular edema secondary to branch retinal vein occlusion in a pair-matched analysis. Ophthalmologica. 2010;224(5):319–324. | |
Hsu J, Kaiser RS, Sivalingam A, et al. Intravitreal bevacizumab (avastin) in central retinal vein occlusion. Retina. 2007;27(8):1013–1019. | |
Chan A, Duker JS. A standardized method for reporting changes in macular thickening using optical coherence tomography. Arch Ophthalmol. 2005;123(7):939–943. | |
Chen CH, Chen YH, Wu PC, et al. Treatment of branch retinal vein occlusion induced macular edema in treatment-naïve cases with a single intravitreal triamcinolone or bevacizumab injection. Chang Gung Med J. 2010;33(4):424–435. | |
Hatef E, Khwaja A, Rentiya Z, et al. Comparison of time domain and spectral domain optical coherence tomography in measurement of macular thickness in macular edema secondary to diabetic retinopathy and retinal vein occlusion. J Ophthalmol. 2012;2012:354783. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.