Back to Journals » OncoTargets and Therapy » Volume 11
The clinical feasibility of flexible bronchoscopy interventional therapy in patients with central airway stenosis and respiratory failure caused by malignancy
Authors Wang J, Yang Y, Zha W, Zhang X
Received 30 May 2018
Accepted for publication 3 October 2018
Published 1 November 2018 Volume 2018:11 Pages 7709—7714
DOI https://doi.org/10.2147/OTT.S175825
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sanjeev K. Srivastava
Jiwang Wang,1,* Yang Yang,2,* Wangjian Zha,1 Xiuwei Zhang2
1Department of Respiratory and Critical Care Medicine, The First Affiliated Hospital of Nanjing Medical University, Nanjing 210029, Jiangsu, China; 2Department of Respiratory Medicine, Jiangning Hospital Affiliated to Nanjing Medical University, Nanjing 211100, Jiangsu, China
*These authors contributed equally to this work
Objective: The aim of this study was to investigate the clinical effects and feasibility of using flexible bronchoscopy intervention in cases of malignancy that causes central airway stenosis and respiratory failure.
Methods: The clinical data of patients who were admitted to the Department of Respiratory Medicine at the First Affiliated Hospital of Nanjing Medical University and underwent treatment of a malignant tumor with central airway stenosis and respiratory failure by flexible bronchoscopy from February 2010 to May 2013 were analyzed using a retrospective method. The age, gender, location, extent of airway stenosis, interventional therapy, efficacy, and complications for 12 patients were collected and analyzed using the SPSS 13.0 software.
Results: After interventional therapy, the dyspnea index for all the patients improved significantly, and compared with before treatment, the difference was statistically significant (t=13.40, P<0.01). Eleven patients with respiratory failure were corrected, and only one patient was treated via tracheal intubation with mechanical ventilation. There were no severe complications, such as massive hemorrhaging or cardiac arrest in any case.
Conclusion: Flexible bronchoscopy interventional treatment for central airway stenosis and respiratory failure caused by malignant tumors is an effective and safe method. It should be applied in clinical work.
Keywords: flexible bronchoscopy, malignant tumors, central airway, respiratory failure, interventional treatment
Introduction
The central airway refers to the trachea, carina, left and right main bronchus, and the middle section of the bronchus, and it is the main channel for releasing gases from the body. Central airway stenosis refers to the narrowing of the airway due to diseases causing airway lesions occurring in the trachea, the main bronchus, and the right medial segment,1 and this includes both benign and malignant lesions.2,3 The causes of malignant central airway stenosis are the metastasis of lung cancer, esophageal cancer, kidney cancer, etc.4 Patients with central airway stenosis are often in critical condition, and if they do not receive timely treatment, this condition leads to death.5 Therefore, the diagnosis and treatment of central airway stenosis are important for saving patients’ lives and improving their quality of life.
The treatment of malignant central airway stenosis includes surgical treatment or bronchoscopic interventional surgery. For patients who can be radical cured, surgical treatment should be the first choice. However, the application of surgical treatment is limited by unknown etiology, critical condition, tumor metastasis, and long airway stenosis. Bronchoscopic interventional surgery can effectively alleviate the central airway obstruction, improve the quality of life, and give patients the opportunity to undergo further radiotherapy and chemotherapy. In foreign countries, the rigid bronchoscopy is the most common choice for respiratory interventional therapy.6–9 However, the rigid bronchoscopy has not been widely utilized and popularized in China.10 Thus, it is necessary to explore the safety and effectiveness of flexible bronchoscopy for a timely and effective intervention in patients.
In this study, 12 patients with central airway stenosis and respiratory failure caused by malignancy malignant tumors were treated with flexible bronchoscopy interventional therapy. This technique achieved good success, and the results are reported below.
Materials and methods
Patients
The clinical data of 12 patients (6 males and 6 females) with central airway stenosis and respiratory failure caused by malignant tumors who were treated with flexible bronchoscopy interventional therapy (BF260, 1T260; Olympus Corporation, Tokyo, Japan) in the Department of Respiratory Medicine of the First Affiliated Hospital of Nanjing Medical University from February 2010 to May 2013 were retrospectively analyzed. Their average age was 58±9 years. This study included four cases of primary tracheal tumor (including two cases of squamous cell carcinoma and two cases of adenoid cystic carcinoma), seven cases of a postoperative recurrence of esophageal cancer infiltrating the central airway, and one case of esophageal cancer after radiotherapy stenosis. The operators are rich in clinical experience. In the 12 patients, 11 had type I respiratory failure and one had type II respiratory failure (Table 1).
Central airway obstruction is generally classified into three categories depending on whether the tumor is purely intraluminal, intraluminal, or mixed. If the tumor is confined to the airway lumen (intraluminal), it is considered “intrinsic” compression. On the other hand, if the tumor is obstructing the airway due to mass effect and there is no intraluminal component, it is called “extrinsic” compression (intraluminal). The majority of central airway obstruction falls into the final “mixed” category, being that there are elements of both intrinsic and extrinsic involvement. With respect to the “mixed” category, the tumor often originates adjacent to the airway and erodes through the airway wall invading the lumen.
Methods
Besides the necessary testing, all patients also underwent chest CT-airway three-dimensional imaging (Figure 1) in order to understand the site and length of the stenosis and the relationship with the large vessels. Some of the patients (stenosis site or the patency of distal side of bronchus was unknown) also received thin bronchoscopy (Figure 2). According to the severity of the patient’s condition and the type of stenosis, we selected from a clamp, balloon dilatation, freezing, high-frequency electrocautery, argon plasma coagulation (APC), and an airway stent for the comprehensive intervention.11–17 Interventional treatment was performed during general anesthesia using a laryngeal mask airway. There was one case of high-frequency electrocautery, one case of airway stent placement, one case of clamp combined balloon dilatation, one case of frozen joint high-frequency electrocautery, one case of high-frequency electrocautery combined with APC, two cases of balloon dilatation combined with APC and airway stent placement, and five cases of high-frequency electrocautery combined with airway stent placement. Two or more combined treatments accounted for 83.3%. In the process of intervention, suction was used to clean up the airway sputum and other secretions. During the operation, stop the operation when the pulse oxygen is less than 90% and the operation was performed again until the oxygenation is elevated.
  | Figure 1 Three-dimensional imaging of the airway showing significant stenosis in the middle of the trachea and atelectasis in the lower left part of the lung. |
  | Figure 2 Flexible bronchoscopy showed obstructive stenosis of the trachea. |
- High-frequency electrocautery: For valve or membranous stenosis, needle electrocautery is used for rapid removal. APC (with output power of 30–50 W and 0.8–1.6 L/min volume flux of Argon gas) was applied to the base of the lesion. Intermittent cauterization is appropriate (3–10 seconds per time), and the carbonized solidified tissues were timely cleaned using biopsy forceps.
- Airway stent placement: According to the length and diameter of the stenosis segment measured by preoperative chest CT and bronchoscopy, airway stents (Micro-Tech, Nanjing, China) of different lengths, diameters, and types were selected. The length of the selected scaffold should exceed 5–10 mm of the length of the narrow section. The bronchoscope enters the trachea through the laryngeal mask (4# for man, 3# for woman; Well Lead Medical Co., Ltd., Guangzhou, China), cleans up the secretion of the lesion area, and places the guide wire through the bronchial working hole. The guide wire was retained, and the bronchoscope was replaced with an ultrafine bronchoscope (2.8 mm inside diameter, BF-C30; Olympus Corporation). Pushers with metal stents are fed into the trachea along the guidewire, placed in the best position under the direct vision of the bronchoscope, and then withdrawn from the guidewire and the pusher.
- Balloon dilatation: The balloon catheter (Boston Scientific Corporation, Marlborough, MA, USA) was delivered through the working hole of the bronchoscope to the stenosed trachea or the stent with poor distension, and the balloon catheter is protruded at both ends of the stenosis or in the stent. Water was injected into the balloon with a gun pump, and the injection pressure was 3–8 atm (usually increases from low to high, 1 atm=101.325 kPa). The balloon remained bulged for 30–60 seconds each time. Each balloon will remain inflated for 30–60 seconds.
- Carbon dioxide freezing: Freezing treatment machine (K300) was purchased from Kooland, Beijing, China. The source of refrigeration is liquid carbon dioxide. The metal head of the flexible frozen probe (diameter is 1.9–2.3 mm) was placed on the surface of the object or pushed into the object, and frozen for 10–40 seconds. In the freezing process, the probe and the adhesive object are taken out together under freezing condition.
Statistical analysis
The data were analyzed using the SPSS 13.0 software (SPSS Inc., Chicago, IL, USA). Measurement data were expressed as mean ± SD, and the paired t-test was used to compare the efficacy before and after treatment. The data were considered statistically significant when P≤0.05.
Results
Clinical effects
After the above-mentioned single or multiple interventional therapies were performed, 12 patients’ cough, sputum, shortness of breath, and other clinical symptoms were shown to be significantly relieved before discharge. The partial pressure of oxygen was markedly increased, and the airway diameter was significantly larger than before treatment. According to Myer-Cotton classification, the degree of stenosis in all patients was grade III before treatment, and the degree of stenosis was grade I after treatment. It is supplemented in Table 1.
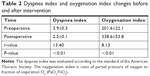
Index observations
The dyspnea index was evaluated according to the standard of the American Thoracic Society. The oxygenation index is ratio of partial pressure of oxygen to fraction of inspiration O2 (PaO2/FiO2). In the 12 patients, the dyspnea index was reduced from 3.9±0.3 points to 2.2±0.1 points after the interventional treatment (P<0.01; Table 2). After the operation, the oxygen device of nine patients (75%) could be completely removed within 24 hours, and PaO2 was above 70 mmHg (1 mmHg=0.133 kPa). Two cases were given nasal catheter oxygen, and their PaO2 was maintained above 75 mmHg. Only one case had to receive a tracheal intubation ventilation treatment (after the laryngeal mask was removed), and the ventilator was removed after 3 days. The oxygenation index was significantly improved from the preoperative level of 201.6±2.1 to 338.6±53.8 (P<0.01; Table 2). Airway obstruction was improved in all patients, and the survival time was longer than 3 months (Table 3).
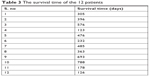  | Table 3 The survival time of the 12 patients |
Complications
Eleven patients with respiratory failure were corrected, and only one patient was treated with mechanical ventilation. All operations were completed successfully, and no patients experienced a massive hemorrhage, cardiac arrest, or other serious complications during the intervention.
Discussion
Malignancies are one of the most common causes of central airway stenosis.6,18 Severe obstruction can lead to pulmonary atelectasis and infection, hypoxemia or respiratory failure, and can cause asphyxia and other life-threatening conditions.19 With the increase in the incidences of bronchial lung cancer, the number of patients with central airway stenosis caused by malignant tumors has increased. Because patients have severe airway stenosis and respiratory failure (some patients are in advanced stage of tumor), the surgical risk for them is very high or the operation opportunity has been lost. It is imperative to improve the respiratory status of the patients in time and effectively, so as to gain time for follow-up treatment. Outside of China, the rigid bronchoscope is most commonly used for respiratory interventional therapy to timely and effectively open the airway,6–9 while the use of this type of bronchoscope is uncommon in China, and our hospital did not have rigid bronchoscope. In addition, there is a lack of doctors who can operate hard mirrors skillfully. The patient’s condition is extremely serious and might suffocate at any time. At that time, it is more important to save patients’ lives on time. In this study, flexible bronchoscopy interventional treatment in 12 patients with central airway stenosis and respiratory failure caused by malignant tumors achieved excellent results, proving to be a simple and effective way for most hospitals in China.
Because patients with central airway stenosis and respiratory failure caused by malignant tumors are in critical condition, it is important to choose a suitable and effective method of anesthesia during respiratory intervention. Since the use of the rigid bronchoscope with general anesthesia is uncommon in China, general anesthesia using a laryngeal mask airway for interventional treatment was a simple and economical method.10,20 General anesthesia is often used for patients with tracheal stenosis lesions, especially for the upper tracheal stenosis. Patients with left and right main bronchial stenosis and respiratory failure can also use a larynx mask airway for general anesthesia. In the 12 cases, the interventional therapy was successfully performed under general anesthesia with a laryngeal mask airway without any incidents.
In central airway stenosis, especially in a complex airway stenosis, the combined application of various treatment methods in intervention therapy is very effective.21,22 At present, the commonly used airway interventional treatment technologies are mainly the high-frequency electric knife, APC, freezing, airway stent placement, and balloon dilatation. However, all the above-mentioned technologies have their range of applications, characteristics, and limitations. Therefore, different treatment methods were selected in this study according to the type, location, degree, and length of the airway stenosis.15 Because the 12 patients had malignant tumors and were critically ill, the treatments for rapid ablation of tumor tissue and expansion of airway could be chosen. Using freezing, drawing, and other methods to remove necrosis and secretions in the airway, the respiratory function of the lung tissue could be rapidly recovered, and the respiratory failure could be effectively corrected, which could achieve the effect that drugs cannot achieve. When the second stenosis occurs, it is necessary to use APC or electrocautery to recanalization.
However, flexible bronchoscopy intervention therapy was unsafe for patients with central airway stenosis caused by pulmonary metastasis of renal cell carcinoma. There is a risk of massive bleeding, but enhanced CT examination before operation can effectively prevent the occurrence of this condition.
Conclusion
The flexible bronchoscopy intervention therapy in patients with central airway stenosis and respiratory failure caused by malignant tumors is an effective, simple, economical, and safe technique, and it is worthy of clinical application in the absence of rigid bronchoscopy.
Ethical statement
This study has been approved by the ethics committee of the First Affiliated Hospital of Nanjing Medical University. Before collecting clinical data from the patient, we informed them of our research purposes, and written informed consent was obtained. We advised that their data were for scientific purposes only, and the patients’ information were anonymous in order to protect the health, safety, and privacy of the patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Wahidi MM, Herth FJ, Ernst A. State of the art: interventional pulmonology. Chest. 2007;131(1):261–274. | ||
Gorden JA, Ernst A. Endoscopic management of central airway obstruction. Semin Thorac Cardiovasc Surg. 2009;21(3):263–273. | ||
Cosano Povedano A, Muñoz Cabrera L, Cosano Povedano FJ, et al. Endoscopic treatment of central airway stenosis: five years’ experience. Arch Bronconeumol. 2005;41(6):322–327. Spanish. | ||
Zhang H, Wang GF. Reatment of malignant central airway stenosis. Chin J Front Med Sci. 2014;6(2):19–21. | ||
Li LY. Etiology and pathophysiological changes of central airway stenosis. Chin J Tubercul Respir Dis. 2003;26(7):387–388. | ||
Jeon K, Kim H, Yu CM, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol. 2006;1(4):319–323. | ||
Beamis JF. Interventional pulmonology techniques for treating malignant large airway obstruction: an update. Curr Opin Pulm Med. 2005;11(4):292–295. | ||
Theodore PR. Emergent management of malignancy-related acute airway obstruction. Emerg Med Clin North Am. 2009;27(2):231–241. | ||
Colt HG, Harrell JH. Therapeutic rigid bronchoscopy allows level of care changes in patients with acute respiratory failure from central airways obstruction. Chest. 1997;112(1):202–206. | ||
Wang T, Zhang J, Wang J, et al. Interventional bronchoscopy with the use of mechanical ventilation by larynx mask or tracheal intubation under general anesthesia. Zhonghua Jie He He Hu Xi Za Zhi. 2011;34(10):739–742. Chinese. | ||
Vorasubin N, Vira D, Jamal N, Chhetri DK. Airway management and endoscopic treatment of subglottic and tracheal stenosis: the laryngeal mask airway technique. Ann Otol Rhinol Laryngol. 2014;123(4):293–298. | ||
Al-Ayoubi AM, Bhora FY. Current readings: the role of stenting in tracheobronchial disease. Semin Thorac Cardiovasc Surg. 2014;26(1):71–75. | ||
Ortiz R, Dominguez E, De La Torre C, et al. Early endoscopic dilation and mitomycin application in the treatment of acquired tracheal stenosis. Eur J Pediatr Surg. 2014;24(1):39–45. | ||
Jeong BH, Um SW, Suh GY, et al. Results of interventional bronchoscopy in the management of postoperative tracheobronchial stenosis. J Thorac Cardiovasc Surg. 2012;144(1):217–222. | ||
Wang JW. Interventional treatment and strategy of central type airway malignancy. Chin J Clin. 2012;19(2):356–373. | ||
Bolliger CT, Mathur PN, Beamis JF, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J. 2002;19(2):356–373. | ||
Jin FG, Li WP. Diagnosis and interventional procedure of central airway stenosis. Med Philos. 2008;29(22):7–9. | ||
Zhao W, Yang Z, Chen LA. Etiological diagnosis and treatment of central airway obstruction: report of 40 cases and review of the literature. Zhonghua Jie He He Hu Xi Za Zhi. 2011;34(8):590–594. Chinese. | ||
Wang JW. Treatment of Asphyxiating Tracheal Stenosis (Three Cases) by flexible bronchoscopy intervention with use of mechanical ventilation by larynx mask or tracheal intubation under general anesthesia. Chin J Tubercul Respir Dis. 2012;35(7):545–547. | ||
Wang JW. Intervention with flexible bronchoscopy in patients with respiratory failure caused by tracheal stenosis. Chin J Emerg Med. 2013;22(5):521–525. | ||
Jin FG, Fu EQ, Xie YH, et al. The application of combined interventional procedures for the management of intractable central airway stenosis. Zhonghua Jie He He Hu Xi Za Zhi. 2010;33(1):21–24. Chinese. | ||
Chhajed PN, Somandin S, Baty F, et al. Therapeutic bronchoscopy for malignant airway stenoses: choice of modality and survival. J Cancer Res Ther. 2010;6(2):204–209. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.