Back to Journals » Journal of Pain Research » Volume 14
The Central Response of Electroacupuncture on Trigeminal Neuralgia Based on Resting-State Functional Magnetic Resonance Imaging: A Protocol for a Pre-Experimental, Single-Centre, Randomized, Controlled Trial
Authors Tang D, Zhang X, Xu Y, Dai L, Sun J, Hu H , Jiang H, Jin P , Chen L, Fang J
Received 17 August 2021
Accepted for publication 30 September 2021
Published 20 October 2021 Volume 2021:14 Pages 3321—3331
DOI https://doi.org/10.2147/JPR.S334078
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Houman Danesh
Ding Tang,1 Xufen Zhang,1 Yani Xu,1 Linglin Dai,1 Jianlan Sun,1 Hantong Hu,2 Huangwei Jiang,3 Ping Jin,3 Lifang Chen,2 Jianqiao Fang4
1The Third Clinical Medical College of Zhejiang Chinese Medical University, Hangzhou, Zhejiang, People’s Republic of China; 2Department of Acupuncture, The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, Zhejiang, People’s Republic of China; 3Department of Radiological, The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, Zhejiang, People’s Republic of China; 4The Third Clinical Medical College of Zhejiang Chinese Medical University, Key Laboratory of Acupuncture and Neurology of Zhejiang Province, Hangzhou, Zhejiang, People’s Republic of China
Correspondence: Lifang Chen
Department of Acupuncture, The Third Affiliated Hospital of Zhejiang Chinese Medical University, No. 219 Moganshan Road, XiHu District, Hangzhou, Zhejiang, 310005, People’s Republic of China
Email [email protected]
Jianqiao Fang
Zhejiang Chinese Medical University, NO. 548 Binwen Road, Binjiang District, Hangzhou, Zhejiang, 310053, People’s Republic of China
Email [email protected]
Objective: To verify the efficacy of electroacupuncture (EA) on classical trigeminal neuralgia (CTN), and to observe the brain functional status of patients with CTN and the intervention effects of EA on brain function by resting-state functional magnetic resonance imaging (rs-fMRI).
Methods and Analysis: Thirty CTN patients will be randomly divided into EA combined with carbamazepine group and carbamazepine group in 2:1 ratio by using a random number table. Patients in EA combined with carbamazepine will receive EA treatment and carbamazepine for four weeks. The carbamazepine group will only receive carbamazepine treatment. VAS (visual analogue scale), HAMA (Hamilton Anxiety Scale), HAMD (Hamilton Depression Scale) and SF-36 (short form 36 health survey) will be performed before, after four-week treatments and at three-month follow-up in CTN patients. Six CTN patients will be randomly selected from EA combined with carbamazepine group and carbamazepine group, respectively, before treatment, and twelve paired healthy participants will be recruited at the same time. The twelve CTN patients will be scanned by rs-fMRI before and after treatment, and the healthy participants will be scanned by rs-fMRI only at baseline. Regional homogeneity (ReHo) and amplitude of low-frequency fluctuation (ALFF) analysis will be carried out to compare the dysfunctional brain regions between CTN patients and healthy participants, as well as the differences between two groups of patients with CTN after treatment.
Trial Registration: ChiCTR-1900027873.
Keywords: electroacupuncture, trigeminal neuralgia, pre-experimental, fMRI, randomized controlled trial, protocol
Introduction
Classical trigeminal neuralgia (CTN) is a common neuropathic pain characterized by electrical pain sensations, which is developing without apparent cause other than neurovascular compression. Its incidence rate is estimated to range between 4.3 and 8 per 100,000, the average age of onset is (63±16) years old, the ratio of men to women is about 1:1.6. One of the main causes of its burden is that it causes severe pain, sometimes described as excruciating, typically, the attacks are sudden and abrupt, with the pain sensation arising only from one or more trigeminal nerve branches.1 As CTN progresses, the pain often becomes more prolonged and severe. Eventually, it can lead to psychosocial distress because it negatively impacts daily activities and quality of life (QOL).2 It is a hot spot in the field of pain research because of its severe pain and its huge influence on patients’ daily life. Carbamazepine is the first-line medicine for CTN, but its long-term use is prone to addiction, drug resistance, and adverse drug reactions, resulting in poor long-term effect.3–5 Surgical interventions such as microvascular decompression (MVD), percutaneous radiofrequency rhizotomy (PRR), percutaneous glycerol rhizotomy (PGR), percutaneous balloon compression (PBC), and stereotactic radiosurgery (SRS), including gamma knife radiosurgery (GKRS) or CyberKnife, have certain efficacy but possess risks for complications and may in some cases be associated with a high risk. In MVD, the main complication is postoperative trigeminal nerve deficit which may lead to facial weakness, hearing loss, cerebellar infarct or hematoma, and Cerebro-Spinal Fluid (CSF) leak. PRR damages small unmyelinated pain fibers contributing to adverse effects. Higher temperatures may be associated with the rate of hypesthesia. PBC and SRS have a high risk of hypesthesia.6,7
In China, acupuncture has been practiced since 2000 BC as a treatment for a variety of diseases according to the “meridian theory” as described in the Yellow Emperor’s Classic of Internal Medicine.8 According to the consensus panel report of the National Institutes of Health (NIH), acupuncture can effectively treat postoperative dental pain,9 acupuncture has experienced significant growth in popularity and usage in the United States.10 Electroacupuncture (EA), as a development of acupuncture, allows stimulation of a larger area around acupoints for a shorter time. Furthermore, it is quite easy to identify and quantify stimulation parameters such as intensity, duration, and frequency,11 but the mechanisms underlying these effects remain to be clarified, EA may modulate inflammatory pain by affecting the entire nervous system, including the central nervous system (CNS), the peripheral nervous system (PNS), the immune system as well as endocrine system.12
In the past few years, a lot of clinical studies have reported that acupuncture is favorable in treating trigeminal neuralgia (TN). Gao 13 found that acupuncture can serve as an alternative treatment for patients with idiopathic trigeminal neuralgia (ITN) to improve cognitive function as well as QOL. Ichida14 concluded that ITN can be treated with acupuncture since it has analgesic effects on ITN and the associated secondary myofascial pain. Zhang15 found primary trigeminal neuralgia (pTN) patients can benefit from triple punctures significantly with few side effects.
Hu16 analyzed 33 randomized, controlled trials (RCTs) according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines, he concluded that all current scientific evidence is limited, because most RCTs included were of low methodological quality, current available evidence is of poor or very poor quality. Thus, acupuncture in treating pTN cannot be robustly assessed by research. For the validity of the outcomes, large-scale, long-term RCTs must be conducted by using rigorous methods.
Functional magnetic resonance imaging (fMRI) studies on the central pathogenesis of TN have shown that there are dysfunction in many brain regions, which are mainly manifested in the imbalanced brain networks related to pain perception and regulation, emotion management and so on. Wang17 discovered low-frequency BOLD signals in trigeminal pain are distributed in a characteristic spatiotemporal pattern. Yuan18 concluded that several brain regions involved with pain modulation and perception were found to show abnormal spontaneous brain activity in ITN patients, including the cerebellum, cingulate cortex, insula, etc. Xiang19 found CTN is linked to altered neuronal networks in various brain regions such as cerebellum, temporal gyrus, occipital gyrus, etc. They all imply that CTN affects cerebral function to some extent.
fMRI-based studies of the central mechanism of acupuncture analgesia previously have shown that acupuncture can alleviate pain by regulating the imbalance and integrating the connections of brain function. Yu20 concluded that acupuncture could alleviate pain in Parkinson’s Disease (PD) patients through modulation of both sensory-discriminative and emotional related brain regions. Yan21 showed that different changes are observed in degree centrality (DC) patterns in patients with chronic shoulder pain (CSP) after treatment at contralateral or ipsilateral Tiaokou (ST 38). Shi22 demonstrated that acupuncture stimulation resulted in widespread deactivation in patients with chronic acute low back pain (ALBP), affecting the limbic system, pain state, and default mode network (DMN), as well as activating the attentional and sensory systems. However, currently, there are no fMRI-based studies on the central analgesic mechanism of acupuncture for TN.
In this study, we might find (1) EA can alleviate the pain symptoms of CTN patients effectively during the acute stage. (2) EA can achieve the analgesic effect by regulating the imbalance of brain functional network in CTN patients. (3) The imbalance of brain functional network in CTN patients and the regulating effect of EA on CTN patients may be related to the brain regions of pain perception and regulation, emotion management, memory and cognition which can be detected by fMRI, such as cerebellum, limbic lobe, frontal gyrus, etc.
To sum up, we need to solve the following problems: (1) At present, there is no ideal treatment plan for CTN. (2) Domestic and abroad reports show that acupuncture treatment of CTN can significantly alleviate pain, make the “trigger point” disappear, and the long-term effect of EA on CTN is remarkable, but there is no strong objective evidence. (3) There is no study on acupuncture treatment for CTN based on whole-brain fMRI study.
The team of Professor Fang Jianqiao has been studying the efficacy and mechanism of acupuncture analgesia for many years. Previously, Dr. Sun Jing had published a study protocol in MEDICINE titled Electroacupuncture therapy for change of pain in classical trigeminal neuralgia. In contrast, there are several differences between this protocol and Dr. Sun’s protocol: (1) fMRI will be introduced into clinical trials of EA treatment for CTN, it will provide further objective basis for the efficacy, immediate effect, cumulative effect and long-term effect of EA on CTN. (2) In addition to recruiting CTN patients, we will recruit healthy participants to investigate the imbalance in the brain network of CTN patients by comparing the fMRI images of CTN patients and healthy participants. (3) Considering the pain degree of CTN, in order to enhance the patient’s compliance, we will adopt positive control, non-equivalent randomized control design, and there will be no placebo group in this protocol.
Thus, we conduct this well-designed, single-centre, randomized controlled clinical trial to assess the EA effects on CTN based on fMRI analysis and behavioral scales evaluation.
Materials and Methods
Study Design
The study is a pre-experimental, single-centre, randomized controlled, outcome assessor-blinded clinical trial, and it was approved by the Ethics Committee of The Third Affiliated Hospital of Zhejiang Chinese Medical University. In order to obtain a more definite result, we expanded the sample size from 16 to 30, and prolonged the study period. Thirty CTN participants recruited from Zhejiang Province will be randomly divided into EA combined with carbamazepine group and carbamazepine group in 2:1 ratio by using a random number table, respectively, six patients will be selected from each group before treatment. Twelve paired healthy participants will be recruited at the same time. The results of brain fMRI scanning will be compared to trace the location of specific dysfunctional brain regions. Data for the assessment will be collected at baseline, 4-week treatment, and 3-month follow-up in two groups of CTN patients, and data in healthy group will be collected only at baseline.
This study protocol was developed according to the Standard Protocol Items: Recommendations for Intervention Trials (SPIRIT) 2013,23 which is supplied in Supplementary File 1. Chinese Clinical Trial Registry (ChiCTR) has registered this trial. The trial flow chart is summarized in Figure 1 and Table 1.
 |
Table 1 Trial Schedule |
Study Methods
Participant Recruitment
This study will recruit subjects from all over the province. Wechat and hospital posters will be used to advertise our study. Eligibility of CTN patients and healthy participants will be assessed by physicians using the criteria described below. Informed consent will be obtained once eligible patients agree to participate in the study.
Ethical Considerations
Prior approval from the ethics committee will be obtained prior to the beginning of this study. The patient’s privacy will be protected, all participants will be assigned to treatment and examination only after signing their informed consent.
Randomization and Blinding
Randomization will be done by Microsoft Excel 2020 software in the study. This list of generated random numbers will be printed, divided into small pieces, separated and sealed in sequentially numbered envelopes. The special screeners will preserve the envelopes, and they will open the envelope when each participant is included so the group information can be gathered. After that, the subjects will be informed whether they would be in the EA combined with carbamazepine group or carbamazepine group. The outcome assessors and data analysts are all blinded.
Participants and Populations
Inclusion Criteria for CTN Patients
Inclusion Criteria for Healthy Participants
Twelve age-matched healthy participants with similar age, sex, weight, and educational background will be immediately recruited to pair the CTN patients. In addition to the above four criteria, healthy participants must also meet the following criteria: physical fitness (no major illness history, no genetic history, no mental, emotional disorders, no acute or chronic pain disease, no cognitive impairment, no brain dysfunction or diseases, etc.), no history of fainting, no contraindication for receiving MRI scanning, and agree to participate in the study and complete the treatment and examination as required.
Exclusion Criteria
Interventions and Comparison
The baseline period is two weeks, the treatment period is four weeks, and the follow-up is three months. The pain score will be recorded once a day and performed at baseline (week 0). Before treatment, the average data of the past two weeks will be assessed. After treatment, the average data of the week 4 will be taken. During the follow-up, the average data of the last two weeks will be taken. fMRI will be performed in two groups of CTN patients at baseline (week 0), four weeks after the treatment, and three months at the follow-up. fMRI will be performed in healthy group only at baseline. To make sure CTN patients and healthy participants have no contraindication for receiving MRI scanning, all of them should receive MRI scanning before the study.
EA Treatments
For EA, filiform stainless steel needles (size 0.18 × 25mm, 0.25 × 40 mm, Huatuo brand, manufactured by Suzhou Medical Appliance in Suzhou, Jiangsu Province, China) will be inserted. Instruments of EA will be unified by Hans acupoint neural stimulator (HANS-200A, manufactured by Nanjing Jisheng Medical Technology Co. Ltd.). The acupuncture intervention and comparison conforms to the Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA) 2010,24 which is supplied in Supplementary File 2. The EA protocol will be performed by acupuncturists with a master’s degree and at least five years of experience in the field.
The Position and Function of Acupoints
In accordance with the 2006 People’s Republic of China National Standard (GB/T 12346-2006) “Acupoints names and positioning”, the locations and indications of acupuncture acupoints are detailed in Table 2.
 |
Table 2 Locations and Indications of Acupuncture Acupoints |
Acupuncture Acupoints
Main acupoints: The affected side of Si-bai (ST2), Di-cang (ST4), Xia-guan (ST7).
Adjunct acupoints: Pain in the 2nd branch will be treated with Quan-liao (SI18), pain in the 3rd branch will be treated with Jia-che (ST6), and A-shi-xue (Pain in the 2nd or 3rd branch, two acupuncture points will be selected from the 2nd branch or 3rd branch, respectively).
Main acupoints and adjunct acupoints are local acupoints.
Distal acupoints: The 2 sides of He-gu (LI4) and Wai-guan (TE5).
Manipulation
By using tiny needles (0.18 × 25mm) we will stimulate local points with shallow row needling based on the distribution of the nerves in trigeminal neuralgia. It is important to perform acupuncture gently, and acupuncture should be no deeper than 5mm. The hand should not touch on the trigger points (these are the pain-sensitive places that light touch can trigger severe pain, like the tiff, cheek, nose, and so on). The doctor should consult with the patient to determine the trigger position (never needle or touch the trigger points). Distal points He-gu (LI4) and Wai-guan (TE5) will be stimulated with 0.25 × 40mm needle (depth of 25–35mm). After the patient has a feeling of acid distention (“get Qi”), the reducing method of twirling and lifting-inserting will be applied. In the treatment, if the patient feels pain badly, the distal acupoints can be needled first with the reducing method until it soothes the pain, local acupoints will be needled next.
EA Parameters
The adjunct acupoints of Xia-guan (ST7) and Quan-liao (SI18) or Jia-che (ST6) and Xia-guan (ST7) will receive EA treatment, using the Hans acupoint neural stimulator. In addition, EA will be applied to the distal acupoints at He-gu (LI4) and Wai-guan (TE5). A diluted wave of 2/100Hz will be used as the EA parameter, the treatment time is 60 minutes, and the current intensity is comfortable for subjects.
Frequency, Duration, and Time
Treatment will be provided three times a week, four weeks continuous intervention, and a total of 12 sessions.
Carbamazepine Treatments
Two groups of CTN patients will take the same dose of carbamazepine tablets (Deliduo, Beijing Novartis Pharmaceutical CO. LTD.). 200mg orally twice a day, continue taking for four months (in the treatment and follow-up periods).
Healthy Group
There will be no treatment specifically designed for the healthy group.
Outcome Measures
Primary Outcome Measure
The primary outcome measure is the Visual Analogue Scale (VAS). VAS scores range from no pain on the left to the worst possible pain on the right by measuring the distance from the left side of the mark to the edge.25
Secondary Outcome Measures
The secondary outcome will be the emotional state and QOL.
Emotional State
Hamilton Anxiety Scale (HAMA) and Hamilton Depression Scale (HAMD) will be used to assess emotional state.
The HAMA has 14 symptom-defined elements that address both psychological and somatic symptoms, scores range from 0 (no problem) to 4 (severe) with each item.26
The HAMD-17 is viewed as the “gold standard” of depression evaluations and consists of 17 questions that serve as a point of reference for more recently developed scales.27 The total score is interpreted differently according to different recommendations (eg, 0–7 = normal; 8–13 = mild depression; 14–18 = moderate depression; 19–22 = severe depression and ≥23 = very severe depression).28
Quality of Life
The QOL will be assessed by the Short Form 36 Health Survey (SF-36). It is an instrument widely used to measure Health-Related Quality of Life. The SF-36 measures eight scales with 36 questions. Scores range from 0 to 100 for each scale, the higher the score, the better the life quality.29
The above measurements, including VAS, HAMA, HAMD and SF-36 will be performed at baseline, after four-week treatments and at three-month follow-up in CTN patients.
rs-fMRI Examination and Data Analysis
The rs-fMRI experiments will be conducted using a 1.5 Tesla clinical scanner (GE Medical Systems, LLC) in the Department of Radiology. During the MRI scan, all subjects will be instructed to lie supine, keep their heads still using foam pads and straps, with their eyes closed, stay awake, avoiding structured thinking to ensure rest. Try to avoid painful episodes for about 6min during the resting-state scanning. Every subject will take routine whole brain MRI sequence scans first, including scout scan, conventional transverse section T2WI to exclude intracranial space-occupying lesion and cerebrovascular diseases. High resolution three-dimensional T1-weighted imaging will be performed with a multi-echo magnetization-prepared rapid gradient-echo (T1-weighted MPRAGE) sequences with the following parameters:sagittal slices = 176, time to repetition (TR) = 1900ms, time to echo (TE) = 2.45ms, time to inversion (TI) = 900ms, field of view (FOV) = 256 × 256mm2, thickness/gap = 1.0/0 mm, acquisition matrix = 256 × 256, flip angle (FA) = 9°.
The resting-state scanning sequence is based on blood oxygenation level-dependent (BOLD) principle, using an echo-planar imaging (EPI) sequences with the following parameters: axial slices = 33, TE = 40ms, TR = 3000ms, thickness = 5.0mm, gap = 1mm, FOV = 240 × 240mm2, FA = 90°, acquisition matrix = 64×64, and 200 volumes, each fMRI scan will last 384 seconds. After the data is collected, the cooperation situation of each subject will be asked and recorded in time.19,30–38
rs-fMRI Data Pre-Processing
Image preprocessing will be conducted by Statistical Parametric Mapping (SPM12, http://www.fil.ion.ucl.ac.uk/spm) and the Resting-State fMRI Data Analysis Toolkit (REST, http://www.restfmri.net) on Matlab (MathWorks, Inc., Natick, MA, USA). Data pre-processing will be accomplished by SPM12: 1) remove the previous 10 unstable time points of the data; 2) time correction of the remaining time points; 3) spatial head motion correction; 4) all the subjects’ images will be spatially standardized, and re-sampled to a voxel size of 3 × 3 × 3mm3; 5) remove linear drift; 6) removal of the covariates of head motion parameters and cerebrospinal-fluid signal covariates; 7) remove the effects of high-frequency noise by band-pass filtering (0.01–0.08 Hz).19,30–38
The Regional Homogeneity (ReHo) Calculation
ReHo measuring the short-distance functional connectivity at voxel-level with Kendall’s coefficient of concordance (KCC) is described in the following formula: 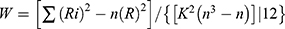 , which was calculated from the consistency of the time series between each individual hormone and its 26 closest neighbors in the brain region. By calculating the KCC value of each given Voxel, the KCC diagram or ReHo diagram of each subject can be obtained. smReHo will be obtained by dividing the average KCC value of the whole brain into the KCC value of each voxel. Finally, we will smooth with a Gaussian kernel of 6 mm full-width at half-maximum (FWHM) to reduce noise.19,39
, which was calculated from the consistency of the time series between each individual hormone and its 26 closest neighbors in the brain region. By calculating the KCC value of each given Voxel, the KCC diagram or ReHo diagram of each subject can be obtained. smReHo will be obtained by dividing the average KCC value of the whole brain into the KCC value of each voxel. Finally, we will smooth with a Gaussian kernel of 6 mm full-width at half-maximum (FWHM) to reduce noise.19,39
The Amplitude of Low-Frequency Fluctuation (ALFF) Calculation
The ALFF algorithm assumed that the low frequency BOLD signals in resting-state brain has its physiological signification. It uses the average of the amplitudes of all the frequencies in a certain frequency band (0.01 ~ 0.08 Hz) to characterize the spontaneous activity of a voxel which reflects the level of the spontaneous activity of each voxel at rest on the view of energy point. First, using a Gaussian kernel of 8 mm FWHM for spatial smoothing. Next, a Fast Fourier Transform (FFT) will be applied to convert each voxel’s time series into the frequency domain, the area under the peak of the power spectrum is considered as the signal energy, and then the square root of this area value represents the amplitude of the signal oscillation, the ALFF value will be obtained by extracting the oscillation amplitude in the frequency range from 0.01 to 0.08Hz. To improve normality of the ALFF, we will perform M-transform. mALFF will be accomplished by dividing ALFF value of the whole brain into ALFF value of each voxel.17,40
Twelve randomly selected patients with CTN will receive rs-fMRI scanning of the whole brain at baseline, after four-week treatments, and at three-month follow-up. Twelve paired healthy participants will receive rs-fMRI examination only at baseline.
Incidence of Adverse Events
The investigators will record and assess all adverse events (AEs) reported by the participants at each visit point. Researchers should immediately contact the principal investigator and ethics committee in case of serious AEs. They will decide if the participant should be removed from the study.
Participants who suffer harm will be compensated.
AEs associated with acupuncture might include fainting, stuck needle, bent needle, broken needle and hematoma.
Carbamazepine-related AEs commonly include nervous system symptoms such as dizziness, ataxia, lethargy and fatigue, water retention and hyponatremia, sometimes rashes, urticaria, pruritus, toxic epidermal necrolysis syndrome, Stevens-Johnson Syndrome, behavioral disorders in children, severe diarrhea, lupus-like syndrome, rare glandular diseases, arrhythmias, atrioventricular block, myelosuppression, central nervous system poisoning, allergic hepatitis, hypocalcemia, osteoporosis, renal poisoning, peripheral neuritis, acute urinary purple disease, embolic vasculitis, allergic pneumonia, acute intermittent porphyria, hypothyroidism, granulocytopenia, thrombocytopenia, aplastic anemia, toxic hepatitis.
Quality Control
An expert panel of acupuncture, neurology, iconography, statistics, and methodology experts reviewed and revised the trial protocol before the study started. The members of the research team are required to take part in a series of training to make certain that they fully understand the research protocol and standard operating procedures. As a means of improving patients’ compliance, compensation and health education are also considered. If the pain is unbearable and seriously interferes with patients’ daily life during the study, patients can take carbamazepine 0.2g once daily after a meal. Medications or other analgesic methods used for emergency pain relief should be recorded with time and dosage.
Data Management
The researchers will be required to fill in the Case Report Form (CRF) with the data collected in accordance with the requirements of the study programme. After the study is finished, the researchers will submit to data management center the complete and signed CRF of all the selected patients in the study. The consistency of case report data collected from the research will be checked, and data queries for inconsistent data will be sent to doctors for clarification.
Statistical Analysis
Based on the intention-to-treat (ITT) principle, an independent statistician will verify the effectiveness and safety of the intervention. Values missing from the dataset will be imputed using last-observation-carried-forward method.
The measurement data will be expressed by mean ± standard deviation. VAS, HAMA, HAMD, and SF-36 will be analyzed by repeated measures analysis of variance (ANOVA). For enumeration data, Chi-square test will be used. All the statistical tests are double-sided, P ≤ 0.05 is considered as statistically significant.
For ReHo analysis and ALFF analysis, 2-sample-t-tests will be conducted within the CTN patients and healthy participation before treatment, as well as EA combined with carbamazepine group and carbamazepine group before and after treatment. Paired t-tests will be performed between two groups of CTN patients before and after treatment to evaluate the ReHo and ALFF difference, P ≤ 0.05 is used to indicate a significant difference.
Statistical software: ReHo analysis and ALFF analysis will adopt REST software, SPSS 25.0 will be used to analyze the remaining data.
Discussion
Current conventional therapies may provide some modest relief from pain on the CTN, including drugs, surgery, and other adjuvant methods.6,41 In spite of that, it is challenging to treat with patients who are poorly compliant with medications and therapies, and the treatments also can entail significant cost to patients and society. Traditional Chinese medicine (TCM) recognizes CTN as a type of facial pain that has been discussed for thousands of years in ancient TCM literatures. Especially acupuncture has a significant impact on treating this disease in TCM, but evidence-based medicine does not demonstrate conclusive evidence that acupuncture treatment can treat CTN.16,35 In this study, we intend to fill that knowledge gap by investigating the effects of acupuncture combined with EA under the fMRI clinical research paradigm.
With rs-fMRI, BOLD signals can be acquired in the resting state and, indirectly, used to identify the specific brain regions that are activated. In ReHo, neuronal activity is analyzed between a given voxel and its adjoining voxels at rest to account for differences in local brain activity. Potential problems with synchronization and coordination in spontaneous neuronal activity are indicated by ReHo values. rs-fMRI techniques such as ALFF, which reveal spontaneous static state brain activity, can be used to analyze and evaluate intrinsic fluctuations in brain signals. This parameter has been proven to be a valuable indicator of spontaneous nerve activity intensity.
This study has several strengths. First, it is a well-designed RCT to evaluate the clinical effectiveness of EA on CTN patients. Second, it is a preliminary study to see how EA affects brain function in CTN patients based on fMRI, no research has been reported till now. Clinical effectiveness of EA in treating CTN may be demonstrated in this study. Additionally, the study attempts to assess how EA impact brain function in CTN patients.
As a pre-experimental, single-centre trial, not only the low incidence of CTN but also the pain degree of CTN, considering the ethical issues, in order to enhance the patients’ compliance, we will adopt positive control design, CTN patients will be randomly divided into EA combined with carbamazepine group and carbamazepine group in 2:1 ratio with a non-equivalent randomized control design. If the results of this study prove the absolute effectiveness of EA in the treatment of CTN, we will further expand the sample size in the later multi-centre clinical trial and consider adding the placebo group.
In summary, this protocol describes the steps involved with a single-centre, randomized, controlled trial that intend to preliminarily observing the brain region localization and functional status of CTN patients and the intervention effect of EA treatment on brain functional activity of CTN patients, this study will measure the ReHo and ALFF throughout the whole brain with rs-fMRI.
It is expected that this study will provide evidence in this field and establish a solid foundation for future, large-scale, multi-centre clinical trials. Moreover, identifying an integrated modality of EA for treating CTN will be of great importance for clinical practice.
Study Limitations
A potential limitation is that only twelve patients can be selected for fMRI study due to limited funds and the low incidence of CTN. It is hoped that some valuable conclusions can be drawn through this preliminary experimental study, which will lay a foundation for future study.
Trial Status
Participant enrollment is started from December 2019. Due to the expanded sample size and the COVID-19 outbreak, it is expected that the enrollment process and the study can be completed by the end of December 2021. Twenty CTN patients and ten healthy participants have been recruited till now.
Data Sharing Statement
All data will be available upon reasonable request.
Ethics and Dissemination
All procedures in the study will be conducted in accordance with the “Declaration of Helsinki (version 19 October 2013)”. The protocol for the study has been approved by institutional review board and ethics committee of the Third Affiliated Hospital of Zhejiang Chinese Medical University (permission number: ZSLL-KY-2019-029-01). The results of the study will be published in a peer-reviewed journal. Patients will also be able to access the results via Wechat or by telephone.
Consent
A consent form will be provided to each enrolled participant after he/she received detailed information about the study procedures, possible risks, and their rights.
Acknowledgments
We appreciate the effort and help from all of those involved in this trial.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study is funded by The Third Affiliated Hospital of Zhejiang Chinese Medical University. This work is also supported by the programme of the Provincial Administration of Traditional Chinese Medicine of Zhejiang (NO. 2018ZY008), and the funder will not have a role in the conduction or interpretation of this trial, or in any decision to publish the results.
Disclosure
The authors declare that they have no competing interests.
References
1. Arnold M. Headache classification committee of the International Headache Society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
2. Melek LN, Smith JG, Karamat A, et al. Comparison of the neuropathic pain symptoms and psychosocial impacts of trigeminal neuralgia and painful posttraumatic trigeminal neuropathy. J Oral Facial Pain Headache. 2019;33(1):77–88. doi:10.11607/ofph.2157
3. Di Stefano G, Truini A. Pharmacological treatment of trigeminal neuralgia. Expert Rev Neurother. 2017;17(10):1003–1011. doi:10.1080/14737175.2017.1370375
4. Ono Y, Shimo T, Shirafuji Y, et al. Drug-induced hypersensitivity syndrome caused by carbamazepine used for the treatment of trigeminal neuralgia. Case Rep Dent. 2016;2016:4605231.
5. Yuan M, Zhou HY, Xiao ZL, et al. Efficacy and safety of gabapentin vs. carbamazepine in the treatment of trigeminal neuralgia: a meta-analysis. Pain Pract. 2016;16(8):1083–1091. doi:10.1111/papr.12406
6. Bick SKB, Eskandar EN. Surgical treatment of trigeminal neuralgia. Neurosurg Clin N Am. 2017;28(3):429–438. doi:10.1016/j.nec.2017.02.009
7. Gubian A, Rosahl SK. Meta-analysis on safety and efficacy of microsurgical and radiosurgical treatment of trigeminal neuralgia. World Neurosurg. 2017;103:757–767. doi:10.1016/j.wneu.2017.04.085
8. Zhou W, Benharash P. Effects and mechanisms of acupuncture based on the principle of meridians. J Acupunct Meridian Stud. 2014;7(4):190–193. doi:10.1016/j.jams.2014.02.007
9. Acupuncture. NIH consensus statement; 1997:1–34.
10. Austin S, Ramamonjiarivelo Z, Qu H, et al. Acupuncture use in the United States: Who, where, why, and at what price? Health Mark Q. 2015;32(2):113–128. doi:10.1080/07359683.2015.1033929
11. Comachio J, Oliveira Magalhaes M, Nogueira Burke T, et al. Efficacy of acupuncture and electroacupuncture in patients with nonspecific low back pain: study protocol for a randomized controlled trial. Trials. 2015;16(1):469. doi:10.1186/s13063-015-0850-7
12. Yuan L, Mingxiao Y, Fan W, et al. Mechanism of electroacupuncture on inflammatory pain: neural-im mune-endocrine interactions. JTCM. 2019;39(5):740–749.
13. Gao J, Zhao C, Jiang W, et al. Effect of acupuncture on cognitive function and quality of life in patients with idiopathic trigeminal neuralgia. J Nerv Ment Dis. 2019;207(3):171–174. doi:10.1097/NMD.0000000000000937
14. IChida MC, Zemuner M, Hosomi J, et al. Acupuncture treatment for idiopathic trigeminal neuralgia: a longitudinal case-control double blinded study. Chin J Integr Med. 2017;23(11):829–836. doi:10.1007/s11655-017-2786-0
15. Zhang Y-P, Wang Y, Xia W-G, et al. Triple puncture for primary trigeminal neuralgia: a randomized clinical trial. Curr Med Sci. 2019;39(4):638–644. doi:10.1007/s11596-019-2085-4
16. Hu H, Chen L, Ma R, et al. Acupuncture for primary trigeminal neuralgia: a systematic review and PRISMA-compliant meta-analysis. Complement Ther Clin Pract. 2019;34:254–267. doi:10.1016/j.ctcp.2018.12.013
17. Wang Y, Xu C, Zhai L, et al. Spatial-temporal signature of resting-state BOLD signals in classic trigeminal neuralgia. J Pain Res. 2017;10:2741–2750. doi:10.2147/JPR.S143734
18. Yuan J, Cao S, Huang Y, et al. Altered spontaneous brain activity in patients with idiopathic trigeminal neuralgia: a resting-state functional MRI study. Clin J Pain. 2018;34(7):600–609. doi:10.1097/AJP.0000000000000578
19. Xiang CQ, Liu WF, Xu QH, et al. Altered spontaneous brain activity in patients with classical trigeminal neuralgia using regional homogeneity: a resting-state functional MRI study. Pain Pract. 2019;19(4):397–406. doi:10.1111/papr.12753
20. Yu SW, Lin SH, Tsai CC, et al. Acupuncture effect and mechanism for treating pain in patients with Parkinson’s disease. Front Neurol. 2019;10:1114. doi:10.3389/fneur.2019.01114
21. Yan CQ, Huo JW, Wang X, et al. Different degree centrality changes in the brain after acupuncture on contralateral or ipsilateral acupoint in patients with chronic shoulder pain: a resting-state fMRI study. Neural Plast. 2020;2020:5701042. doi:10.1155/2020/5701042
22. Shi Y, Liu Z, Zhang S, et al. Brain Network Response to Acupuncture Stimuli in Experimental Acute Low Back Pain: an fMRI Study. Evid Based Complement Alternat Med. 2015;2015:210120. doi:10.1155/2015/210120
23. Chan AW, Tetzlaff JM, Gotzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. doi:10.1136/bmj.e7586
24. Hugh Macpherson AW, Cummings M, Jobst K, Rose K, Niemtzow, R. Standards for reporting interventions in controlled trials of acupuncture: the STRICTA recommendations. Acupunct Med. 2002;20(1):22–25. doi:10.1136/aim.20.1.22
25. Hantong H, Lifang C, Xiaofei J, et al. Effect of herb-partitioned moxibustion on pain and quality of life in women with endometriosis: a protocol for a randomized clinical trial. J Tradit Chin Med. 2019;40(2):324–332.
26. Thompson E. Hamilton Rating Scale for Anxiety (HAM-A). Occup Med. 2015;65(7):601. doi:10.1093/occmed/kqv054
27. Carneiro AM, Fernandes F, Moreno RA. Hamilton depression rating scale and Montgomery-asberg depression rating scale in depressed and bipolar I patients: psychometric properties in a Brazilian sample. Health Qual Life Outcomes. 2015;13(1):42. doi:10.1186/s12955-015-0235-3
28. Melzer J, Rostock M, Brignoli R, et al. Preliminary data of a HAMD-17 validated symptom scale derived from the ICD-10 to diagnose depression in outpatients. Forsch Komplementmed. 2012;19(4):191–196. doi:10.1159/000342018
29. Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725. doi:10.1177/2050312116671725
30. Bao C, Liu P, Liu H, et al. Different brain responses to electro-acupuncture and moxibustion treatment in patients with Crohn’s disease. Sci Rep. 2016;6(1). doi:10.1038/srep36636.
31. Bao C, Wang D, Liu P, et al. Effect of electro-acupuncture and moxibustion on brain connectivity in patients with Crohn’s disease: a resting-state fMRI study. Front Hum Neurosci. 2017;11:000559. doi:10.3389/fnhum.2017.00559
32. Long X, Liu F, Huang N, et al. Brain regional homogeneity and function connectivity in attenuated psychosis syndrome -based on a resting state fMRI study. BMC Psychiatry. 2018;18(1):383. doi:10.1186/s12888-018-1954-x
33. Miller RL, Pearlson G, Calhoun VD. Whole brain polarity regime dynamics are significantly disrupted in schizophrenia and correlate strongly with network connectivity measures. PLoS One. 2019;14(12):e0224744. doi:10.1371/journal.pone.0224744
34. Ni MF, Huang XF, Miao YW, et al. Resting state fMRI observations of baseline brain functional activities and connectivities in primary blepharospasm. Neurosci Lett. 2017;660:22–28. doi:10.1016/j.neulet.2017.09.014
35. Sun J, Li R, Li X, et al. Electroacupuncture therapy for change of pain in classical trigeminal neuralgia. Medicine. 2020;99(16):e19710.
36. Tsai YH, Yuan R, Patel D, et al. Altered structure and functional connection in patients with classical trigeminal neuralgia. Hum Brain Mapp. 2018;39(2):609–621. doi:10.1002/hbm.23696
37. Zhang J, Cai X, Wang Y, et al. Different brain activation after acupuncture at combined acupoints and single acupoint in hypertension patients: an rs-fMRI study based on ReHo analysis. Evid Based Complement Alternat Med. 2019;2019:1–10.
38. Zhang Y, Mao Z, Pan L, et al. Frequency-specific alterations in cortical rhythms and functional connectivity in trigeminal neuralgia. Brain Imaging Behav. 2019;13(6):1497–1509. doi:10.1007/s11682-019-00105-8
39. Yan J, Li M, Fu S, et al. Alterations of dynamic regional homogeneity in trigeminal neuralgia: a resting-state fMRI study. Front Neurol. 2019;10:1083. doi:10.3389/fneur.2019.01083
40. Chen Y, Xiang CQ, Liu WF, et al. Application of amplitude of low frequency fluctuation to altered spontaneous neuronal activity in classical trigeminal neuralgia patients: a resting state functional MRI study. Mol Med Rep. 2019;20(2):1707–1715.
41. Wiffen PJ, Derry S, Moore RA, Kalso EA. Carbamazepine for chronic neuropathic pain and fibromyalgia in adults Cochrane Database Syst Rev. 2014;4:CD005451. doi:10.1002/14651858.CD005451.pub3
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

