Back to Journals » Psychology Research and Behavior Management » Volume 15
The Causal Effects of Anxiety-Mediated Social Support on Death in Patients with Chronic Heart Failure: A Multicenter Cohort Study
Authors Yan J, Tian J , Yang H, Han G, Liu Y, He H, Han Q, Zhang Y
Received 23 August 2022
Accepted for publication 2 November 2022
Published 8 November 2022 Volume 2022:15 Pages 3287—3296
DOI https://doi.org/10.2147/PRBM.S387222
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Igor Elman
Jingjing Yan,1 Jing Tian,1,2 Hong Yang,1 Gangfei Han,2 Yanling Liu,1 Hangzhi He,1 Qinghua Han,2 Yanbo Zhang3,4
1Department of Health Statistics, School of Public Health, Shanxi Medical University, Taiyuan, People’s Republic of China; 2Department of Cardiology, The First Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China; 3Shanxi Provincial Key Laboratory of Major Diseases Risk Assessment, Shanxi Medical University, Taiyuan, People’s Republic of China; 4Shanxi University of Chinese Medicine, Taiyuan, People’s Republic of China
Correspondence: Yanbo Zhang, Shanxi Provincial Key Laboratory of Major Diseases Risk Assessment, Shanxi Medical University, No. 56 South Xinjian Road, Taiyuan, Shanxi Province, 030001, People’s Republic of China, Tel +86 3543985051, Email [email protected] Qinghua Han, Department of Cardiology, The First Hospital of Shanxi Medical University, No. 85 South Jiefang Road, Taiyuan, Shanxi Province, 030001, People’s Republic of China, Tel +86 3100113031, Fax +86 3514867146, Email [email protected]
Background: Chronic heart failure (CHF) affects more than 3.8 million people worldwide. There is a paucity of studies focusing on psychosocial issues in CHF patients. This study aimed to investigate the association of social support, mental adjustment and death to exploring whether mental adjustment could mediate the relationship.
Methods: From May 2017 to June 2021, we conducted a multicenter clinical study to collect 1552 patients data. The Patient Report Outcome (PRO) scale were disseminated to collect information in the physical, psychological, social and therapeutic domains of patients. Marginal structural model was used to investigate the association of social support and CHF death, and the role of mental adjustment in their mediation.
Results: The direct effect of social support accounted for 44.76% of the total effect. High social support (≥ 14 points) reduced mortality by 46.3% (RR=0.537, P=0.027), medium social support (11– 14 points) reduced mortality by 45.3% (RR=0.547, P=0.042). Anxiety (effect percentage: 24.63%) and appetite-sleep quality (effect percentage: 30.61%) played a mediating role between social support and death in CHF patients. In women, aged > 75 years, divorced or widowed patients were most prone to anxiety due to inadequate support (RR=0.519, P=0.019; RR=0.403, P=0.002; RR=0.413, P=0.041). Family care and socioeconomic assistance significantly reduced the risk of death (RR=0.689, P=0.040; RR=0.584, P=0.012).
Conclusion: Social support can reduce patient mortality, especially family care and social economic assistance. The elderly, female, divorced or widowed patients are more likely to cause mental illness due to inadequate social support.
Keywords: chronic heart failure, social support, marginal structural model, mediation analysis
Background
Chronic Heart Failure (CHF) is a progressive and disabling disease. Affected by the aging population, the number of patients with CHF has reached 60 million worldwide.1 Although the current treatment methods for patients with CHF have been greatly improved, the rehospitalization and mortality rates of patients with CHF remain high.2,3 The 1-year rehospitalization and mortality rates of patients with CHF are 44% and 17%, respectively and the 5-year mortality rate is 42.3%.4 Poor prognosis of heart failure (HF) causes heavy mental and economic burdens to patients, families, and society.2,5 Reducing the risk of death in patients with HF remains a crucial social issue.
The ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure (2021) clearly state that in addition to biological risk factors,3 the development of HF is influenced by several social factors. The stress-buffering hypothesis suggests that social support can moderate the association between stress and health outcomes, and social factors play an extremely important role in health outcomes.6,7 In recent years, although the risk factors of CHF have been well researched, few studies have investigated the social protective factors of patients. In addition, there may be a complex relationship between social support and psychological status. Social support may buffer patients’ anxiety, depression, and other adverse psychological conditions and improve patients’ prognosis.8,9 However, there are still no studies that adequately address these concerns. Therefore, this study focused on the causal role of social support in reducing the mortality of patients with CHF and the potential mechanism (mediating effect) of anxiety, depression, and other psychological domains related manifestations.
Notably, the causal relationship of validation usually requires a clinical cohort study. Owing to the extensive follow-up period, treatment transfer and time-dependent confounding factors inevitably exist, leading to causal effect estimation error; this may affect the efficiency of the study and may cause selection bias.10 The traditional statistical analysis method can not solve these problems effectively.11 Marginal structure model is a classical method in causal inference, which can effectively deal with time-varying confounding factors and transfer problems and more accurately explore the real effects among variables.12 Therefore, this study used the patient report outcome scale for patients with CHF to collect patient information from the physiological, psychological, social, and therapeutic domains, by building a marginal structural model to analyze the causal effect of social support to cardiac death, the mediating effect of anxiety, depression, and other psychological domains.
Methods
Study Population
Between May 2017 and June 2021, we conducted a multi-center longitudinal cohort study in Shanxi, China (the First Hospital of Shanxi Medical University; Shanxi Cardiovascular Hospital; Bethune Hospital) [ChiCTR2100043434; ChiCTR2100043337]. According to the strict inclusion and exclusion criteria (Table 1), 1552 patients with a definite diagnosis of CHF were included in the study, and a cohort of patients with CHF was constructed. CHF-PROM scale was used to collect patients’ data (Table 2). According to their baseline social support scores, patients were categorized into four groups: I (Low social support group/non-exposed group, 0–9), II (Mild social support group, 9–11), III (Medium social support group, 11–14), and IV (High social support group, ≥14). Thereafter, CHF-PRO information and outcome event information of patients were obtained in 1, 3, and 6 months and then followed up every 6 months thereafter. The investigation conforms with the principles outlined in the Declaration of Helsinki, and written informed consent for participation was obtained from all patients.
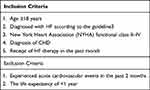 |
Table 1 Participant Inclusion and Exclusion Criteria |
 |
Table 2 The Structural Frame of CHF-PROM |
The inclusion and exclusion criteria are listed in Table 1.
Measurement of Variables
Chf-Prom
In this study, the CHF-PROM,13 which is suitable for Chinese people, was used for data collection. The scale was divided into four fields, 12 dimensions, and 57 items. Each item was divided into 0–4 points, representing the frequency of social support: never (0), less than once a month (1), 1–3 times a month (2), once a week (3), and more than once a week (4).
To facilitate patients’ understanding, the scale involves the method of combining positive and negative scoring. The positive scoring results are kept unchanged in the calculation. The item with the negative score is calculated as 4 minus the item score, and the final score of each item is between 0–4. The higher the score, the better the health status. The specific structures are listed in Table 2. The results of Cronbach’s α coefficients for each dimension show that the scale has good reliability (Figure 1).
 |
Figure 1 Cronbach α coefficients of each dimension. |
Social Support
The social support score was calculated from five items in the PRO scale: SOY1 (family care and communication), SOY2 (relatives’ and friends’ care and communication), SOY3 (colleagues’ care and communication), SOC4 (social and economic assistance), and SOC5 (actively seeking help from the society). The overall score of social support was calculated by summing up the five items, with a possible total score of 20 points. We then categorized the score into four groups according to level of social support based on the distribution of scores in the patients: I (Low social support group, 0–9), II (Mild social support group, 9–11), III (Medium social support group, 11–14), and IV (High social support group, ≥14).
Covariates
Covariates such as demographics (age, gender, occupation, educational attainment, marital status, etc.), cardiac comorbidity (arrhythmic, hypertension, valvular heart disease, and diabetes mellitus), physiology domain (somatization, appetite, sleep independence), psychology domain (anxiety, depression, fear, paranoia), society domain (support, utilization), and treatment domain (compliance, satisfaction, effect of drug) were included. Age was grouped according to the World Health Organization’s (WHO) age classification criteria (≤60, 60–75, ≥75).
Outcome Variable
The primary study endpoint was defined as cardiovascular death (HF-related, sudden, stroke-related, and any other cardiovascular death) during the follow-up.
Statistical Analysis
Missing Values
All the data in this paper were collected one to one by professionally trained members of the research team, so there were a few missing variables. For non-time-varying covariates, the mean was used to estimate the missing values. For the PRO scale, the mean values of two similar follow-up time points were used to fill in the missing values. Two-sided tests were used for all statistical analyses, and the significance level was set at 0.05.
Data Analysis
Sample size estimation was performed using PASS 15 software. The mortality was estimated to be 0.5 in group I (low social support), 0.4 in group II, 0.35 in group III, and 0.3 in group IV. We used the following settings: power = 0.9, alpha = 0.05, and alternative hypothesis = two-sided test. Considering a 10% loss to follow-up rate, the final total sample was estimated to be 1500. We collected data from 1652 people. According to the deduction of lost follow-up patients (n =83), 1469 people were finally included in the model analysis.
The data was arranged, processed, and analyzed using the SPSS 25 software. First, continuous variables were described using means with standard deviations for data with normal distribution, medians and interquartile range for non-normally distributed variables, and numbers and percentages for categorical variables. According to the distribution of variables, the analysis of variance (ANOVA), chi-squared test, and Wilcoxon rank-sum test were used to compare the differences in each parameter between the four groups.
Second, the multiple mediation marginal structural model was used to analyze the risk ratios of social support to cardiac death in patients with CHF and test the potential mediating role of physiological and psychological domains. We used the Directed Acyclic Graph (DAG) for mediator variable selection (Figure 2).
Finally, the subgroup analyses and item analysis of different populations to provide a basis for personalized social intervention for patients with CHF.
In each marginal structural model, we used ordered logistic regression to calculate the stable inverse probability weights for each sample (the weights were truncated at the 95th percentiles and normalized to reduce the influence of outliers).
Results
From the baseline information distribution of CHF patients with different social support levels, there were significant differences in age and marital status distributions. The age of patients with low social support was significantly higher than that of those with high social support (72.4 vs 68.36, 65.8, 67.39, P=0.004). The proportion of divorced and widowed patients with low social support was significantly higher than that of patients with high social support (20.1% vs 15.0, 12.2%, 17.4%, P=0.047). There were no gender differences among the groups (P=0.716). The comorbidity distribution of the patients was similar, as shown in Table 3.
 |
Table 3 Baseline Characteristics by Level of Social Support |
Table 4 shows the following results: the risk of death was 0.537 times higher in grade IV social support patients than in grade I social support patients, with a risk reduction of 46.3% (RR=0.537, 95% CI: 0.310–0.931, P=0.027); the risk of death in patients with social support III was 0.547 times higher than that in patients with low social support, with a 45.3% reduction (RR=0.547, 95% CI: 0.306–0.979, P=0.042).
 |
Table 4 Multiple Mediation Analysis |
The direct effect of social support accounted for 44.76% of the total effect, and the mediating effects of appetite and sleep accounted for 30.61% of the total effect. In other words, social support can improve patients’ appetite and sleep state, and, thus, reduce the occurrence of death events (RR=0.433, 95% CI: 0.264–0.709, P<0.001). The mediating effect of patients’ anxiety symptoms accounted for 24.63% of the total effect of social support, which could improve patients’ anxiety symptoms and reduce the occurrence of death events (RR=0.510, 95% CI: 0.365–0.711, P<0.001). The mediating effect was statistically significant.
According to the subgroup analyses results in Figure 3, patients with CHF aged over 75 years were the most sensitive to social support (RR=0.764, P=0.019), and this patient group was also the most prone to anxiety due to insufficient social support (RR=0.403, P=0.002). Patients younger than 60 years of age were most likely to develop appetite and sleep disorders and accelerate the occurrence of outcome events due to insufficient social support (RR=0.212, P=0.005). For female patients, anxiety symptoms are apparent when social support is insufficient and will significantly affect the occurrence of end-point events (RR=0.519, P=0.019). Divorced or widowed patients are more likely to experience mental illness (anxiety) because of inadequate social support (RR = 0.413, P=0.041).
 |
Figure 3 Subgroup analysis. Abbreviations: SOC, social support; APS, appetite-sleep quality; ANX, Anxiety. |
Figure 4 shows the death risk analysis of each item in the dimension of social support. The results showed that financial support had the strongest effect on mortality in patients with CHF. Compared with patients with no or low financial support, the mortality risk of patients with high financial support was 58.4% (RR=0.584, P=0.012). In addition, family care had the next highest effect on reducing death in patients with CHF. The mortality risk of patients with high levels of family care was 68.9% lower than that of patients with low levels of family care. We did not observe significant effects of social support from neighbors, relatives, co-workers, or actively sought social support on the risk of death in patients with HF.
 |
Figure 4 Item analysis. |
Discussion
We prospectively investigated the causal effect between social support and the risk of death in patients with CHF in a 5-year follow-up cohort. The main findings of this study are as follows. (1) The results of the marginal structural model analysis showed that more social support was significantly associated with a reduced risk of death in patients with CHF, and anxiety, appetite-sleep quality played a mediating role; (2) patients with CHF over 75 years old who are females, divorced, and widowed need to pay more attention to the mental health problems (anxiety) caused by insufficient social support; and (3) among the forms of social support, family care and economic support are the most important.
This study found that there was a causal relationship between social support and death in patients with CHF, and anxiety and appetite and sleep played a mediating role in the relationship. From the statistical perspective of causality argument, the estimation of causality in the real world is usually based on randomized controlled trial (RCT), which strictly controls the trial conditions and adopts the method of randomization and grouping, which can effectively control confounding bias.14 However, the development of RCT still needs a lot of human and material support and strict ethical review, which is difficult to carry out in conventional research centers and general hospitals.15 Strict experimental conditions also bring adverse effects, affecting the extrapolation of results. The correct causal inference model can be used to verify the causal relationship more accurately under the condition of controlling all kinds of confounding. Edge structure model is a kind of more mature causal inference model, it by logistic model is used to estimate probability, and uses the estimation method for inverse probability weighting of the stable weight, build a virtual crowd, the virtual crowd, the distribution of confounding factors and the corresponding processing factor levels are independent of each other, achieve the goal of similar randomized, At this time, the risk assessment of the virtual population can obtain the unbiased analysis of the effect assessment of treatment factors, and solve the phenomenon of time-dependent confounding and treatment transfer in the follow-up process of cohort data.12 In this study, based on the cohort data of CHF patients, we assigned Low social support, mild social support, medium social support and high social support groups at baseline, carried out regular follow-up of patients in the four groups for up to 5 years, and constructed the marginal structure model. It has proved the causal relationship between different degrees of social support and the death of CHF patients and the potential mechanism (mediating) effect of anxiety and other psychological conditions. This analysis and research method has the same idea as many other articles, which can ensure the reliability of the research results.16–18
From the perspective of social medicine and social psychology, prolonged chronic diseases may break the life balance of individuals. When the coping mechanism is ineffective, individuals live with depression, anxiety, sleep disorders, and other symptoms.8,19–21 One possible mechanism in this association is the buffering effect of social support. The buffering hypothesis proposes that social support is only (or mainly) related to health when stressful life events occur.22 This hypothesis predicts that social support will protect individuals against the potential negative impact of stress events by changing the perception of negative events, enhancing one’s sense of self-respect, self-confidence, and self-efficacy, transfer of coping resources, thereby promoting health-related behavior changes that protect anxiety and depression, and improving appetite and sleep state of patients.23–25 In the absence of a clinical diagnosis, psychological symptoms of patients with CHF are often unnoticed and untreated, causing adverse effects on symptom treatment and health outcomes of patients.26 Careful attention by clinical medical workers is recommended to recognize early and mild anxiety symptoms of patients with HF. Additionally, appropriate attention and psychological support to patients’ symptoms to prevent and reduce the anxiety symptoms of patients is necessary to improve the overall treatment effect, treatment compliance of patients, and reduce treatment cost.
The final item analysis results show that family care, communication, and social economic assistance are particularly important for patients. According to the present literature, patients with low socioeconomic status are more likely to receive a less comprehensive management solution from rural hospitals.27–29 Poorer survival and social status may be important factors leading to the deterioration of health outcomes. Social support for patients through economic assistance will help reduce adverse outcomes, and support through family communication may improve the mental health of patients.
Strengths
Based on the biopsychosocial medicine model, this study comprehensively analyzed the causal effects of social support and its items on adverse outcome events in patients with CHF and adjusted the effect size of social support by considering the mediating roles of physiological and psychological domains using data from a prospective cohort study. In addition, a subgroup analysis was conducted for patients of different ages, sexes, and marital statuses. The results are helpful in providing personalized social intervention for different subgroups of patients and improving the prognosis of patients.
Limitations
As the patients were more sensitive to economic situations, only the frequency of aid was counted in the social and economic aid part of this study’s item analysis, and the specific value of financial aid could not be collected. Therefore, the influence of different amounts of financial aid on the outcome could not be accurately determined. Unmarried patients accounted for a very low proportion of the study’s cohort, and no endpoint events occurred in the group with high social support. To ensure the accuracy of the effect estimation, unmarried people were not included in this study; thus, the results may not apply to unmarried people.
Conclusion
Social support can reduce patient mortality, especially family care and social economic assistance. Elderly, female, divorced, or widowed patients should also have attention given to their psychological status (anxiety). Patients younger than 60 years of age with decreased appetite and sleep should receive timely social support to prevent the occurrence of adverse events.
Data Sharing Statement
The raw data that support the findings of this study are available on request from the corresponding author ([email protected]). The data are not publicly available due to privacy or ethical restrictions.
Ethics Approval and Consent to Participate
The investigation conforms with the principles outlined in the Declaration of Helsinki, and written informed consent for participation was obtained from all patients. This project was approved by the Ethics Committee of Shanxi Medical University and registered in the Chinese Clinical Trial Registry.
Acknowledgments
We are grateful for the cooperation of Shanxi Cardiovascular Hospital.
Funding
This research is supported by a grant from the National Natural Science Foundation of China (grant no: 81872714, 82103958) and Shanxi Provincial Science and Technology Achievements Transformation Project (grant no: 201903D321104).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Olano‐Lizarraga M, Wallström S, Martín‐Martín J, Wolf A. Causes, experiences and consequences of the impact of chronic heart failure on the person´s social dimension: a scoping review. Health Soc Care Community. 2022;30(4):e842–e858. doi:10.1111/hsc.13680
2. Groenewegen A, Rutten FH, Mosterd A, et al. Epidemiology of heart failure. Eur J Heart Fail. 2020;22(8):1342–1356.
3. Mcdonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–3726.
4. Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol. 2016;13(6):368–378.
5. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Rev Esp Cardiol. 2016;74(10):1037–1147.
6. Miao Jonasson J, Hendryx M, Shadyab AH, et al. Social support, social network size, social strain, stressful life events, and coronary heart disease in women with type 2 diabetes: a cohort study based on the women’s health initiative. Diabetes Care. 2020;43(8):1759–1766.
7. Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676–684.
8. Ibarra-Rovillard MS, Kuiper NA. Social support and social negativity findings in depression: perceived responsiveness to basic psychological needs. Clin Psychol Rev. 2011;31(3):342–352.
9. Park M, Cuijpers P, van Straten A, et al. The effects of psychotherapy for adult depression on social support: a meta-analysis. Cognit Ther Res. 2014;38(6):600–611.
10. Bailly S, Pirracchio R, Timsit JF. What’s new in the quantification of causal effects from longitudinal cohort studies: a brief introduction to marginal structural models for intensivists. Intensive Care Med. 2016;42(4):576–579.
11. Osranek M, Bursi F, Bailey KR, et al. Left atrial volume predicts cardiovascular events in patients originally diagnosed with lone atrial fibrillation: three-decade follow-up. Eur Heart J. 2005;26(23):2556–2561.
12. Williamson T, Ravani P. Marginal structural models in clinical research: when and how to use them? Nephrol Dial Transplant. 2017;32(suppl_2):i84–i90.
13. Xue J. Development and Evaluation of PRO Scale for Chronic Heart Failure. Shanxi Medical University; 2012.
14. Cook JA, Hislop J, Adewuyi TE, et al. Assessing methods to specify the target difference for a randomised controlled trial: DELTA (Difference ELicitation in TriAls) review. Health Technol Assess. 2014;18(28):1–175.
15. Ravani P, Palmer SC, Oliver MJ, et al. Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol. 2013;24(3):465–473.
16. Chang SC, Glymour M, Cornelis M, et al. Social integration and reduced risk of coronary heart disease in women: the role of lifestyle behaviors. Circ Res. 2017;120(12):1927–1937.
17. Rathbun AM, Shardell MD, Stuart EA, et al. Pain severity as a mediator of the association between depressive symptoms and physical performance in knee osteoarthritis. Osteoarthritis Cartilage. 2018;26(11):1453–1460.
18. Darabi Z, Najafi F, Safari-Faramani R, Salimi Y. Controlled direct effect of psychiatric disorders on cardiovascular disease: evidence from a large Kurdish cohort. BMC Cardiovasc Disord. 2020;20(1):501.
19. Hasan K, Sevda K, Mustafa Ç. Suicide risk in chronic heart failure patients and its association with depression, hopelessness and self esteem. J Clin Neurosci. 2019;68:51–54.
20. Morikawa M, Okada T, Ando M, et al. Relationship between social support during pregnancy and postpartum depressive state: a prospective cohort study. Sci Rep. 2015;5:10520.
21. Webster J, Nicholas C, Velacott C, et al. Quality of life and depression following childbirth: impact of social support. Midwifery. 2011;27(5):745–749.
22. Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol. 1988;7:269–297.
23. Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ. 1999;318:1460–1467.
24. Orth-Gomér K, Johnson JV. Social network interaction and mortality. A six year follow-up study of a random sample of the Swedish population. J Chronic Dis. 1987;40:949–957.
25. Oman D, Kurata JH, Strawbridge WJ, Cohen RD. Religious attendance and cause of death over 31 years. Int J Psychiatry Med. 2002;32:69–89.
26. Sony J, Sebastian Justin C, George A. Depression and congestive heart failure: are antidepressants underutilized? Eur J Heart Fail. 2003;5:399–400.
27. Philbin EF, Dec GW, Jenkins PL, et al. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol. 2001;87(12):1367–1371.
28. Rathore SS, Masoudi FA, Wang Y, et al. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the national heart failure project. Am Heart J. 2006;152(2):371–378.
29. Simpson L, Owens PL, Zodet MW, et al. Health care for children and youth in the United States: annual report on patterns of coverage, utilization, quality, and expenditures by income. Ambul Pediatr. 2005;5(1):6–44.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

