Back to Journals » Drug Design, Development and Therapy » Volume 17
The Benefits of Molnupiravir Treatment in Healthcare Facilities Patients with COVID-19
Authors Cheng SL, Wang PH , Chang CY, Wang HH, Wang CJ, Chiu KM
Received 8 October 2022
Accepted for publication 9 January 2023
Published 19 January 2023 Volume 2023:17 Pages 87—92
DOI https://doi.org/10.2147/DDDT.S392708
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Manfred Ogris
Shih-Lung Cheng,1,2 Ping-Huai Wang,1 Cheng-Yu Chang,1 Hsu-Hui Wang,1 Chung-Jen Wang,1 Kuan-Ming Chiu2,3
1Department of Internal Medicine, Far Eastern Memorial Hospital, New Taipei City, 220, Taiwan; 2The Graduate Institute of Medicine, Yuan-Ze University, Taoyuan City, Taiwan; 3Division of Cardiovascular Surgery, Far Eastern Memorial Hospital, New Taipei City, 220, Taiwan
Correspondence: Kuan-Ming Chiu, Division of Cardiovascular Surgery, Far Eastern Memorial Hospital, No. 21, Section 2, Nanya S. Road, Banqiao District, New Taipei City, 220, Taiwan, Tel +886-2-89667000, Email [email protected]
Background: Molnupiravir (MOL) is an oral antiviral medication that has recently been treated for COVID-19.
Objectively: We perform a prospective and observational study to elucidate the efficacy and safety of MOL in healthcare patients with COVID-19.
Materials and Methods: A observational, non-randomized study of patients diagnosed with COVID-19 in 46 healthcare facilities and treated with MOL started within 5 days after the onset of signs or symptoms. We recorded data for all patients, including demographic data, clinical features, and symptoms. Treatment response was classified into cure, stable, hospitalization and death. Multivariate analysis was performed with stepwise logistic regression for hospitalization and death risk factors.
Results: In total, 856 patients were diagnosed as having COVID-19 and treated with MOL during the study period. Of those, 496 patients (57.9%) were cured, 256 patients (29.9%) in stable condition, 104 patients (12.2%) hospitalized, and 22 patients (2.6%) died, respectively. There was significant effectiveness (87.8%) in COVID-19 patients using MOL. Multivariate analysis was performed to confirm the risk factors for hospitalization and death and included elder age (> 80 years old) (odds ratio (OR) 2.2, 95% confidence interval (CI): 1.1– 6.9), old cerebrovascular accident (CVA) (OR=4.1, 95% CI: 1.3– 9.9), the presence of diabetes mellitus (DM) (OR=2.6, 95% CI: 1.2– 9.1) and chronic respiratory diseases (OR=2.4, 95% (CI): 1.3– 8.1).
Limitations: This is an observational study, neither randomized study nor control group study.
Conclusion: Initial treatment with MOL has the treatment benefits and is well tolerated for patients with COVID-19 in healthcare facilities. Older age, old CVA, DM, and chronic respiratory diseases were independent risk factors for hospitalization and mortality. The results demonstrate there are important clinical benefits of MOL beyond the reduction in hospitalization or death for these patients with more comorbidities in Taiwan.
Keywords: molnupiravir, COVID-19, healthcare facility, clinical benefit, hospitalization, comorbidity
Introduction
COVID-19 infection is currently affected among the general population in the world. This disease was first documented in Wuhan (China) in December 2019 and is due to SARS-CoV-2 (2019-nCoV) virus. COVID-19 symptoms included high body temperature, general malaise, sore throat, cough, shortness of breath, low energy status. In most infected people, the symptoms are mild, but in the elderly or those with multiple comorbidities it may complicate with severe pneumonia, acute respiratory distress syndrome, multi-organ failure, and death.1 Adequate vaccines’ administration is important for the prevention of severe COVID-19 development or mortality; however, the effective antiviral medications to combat this disease are not currently available. Patients with immunocompromised diseases could not be fully protected though got vaccinated, and existing vaccines may not be good protection against new SARS-CoV-2 variants.2,3 Remdesivir, a new antiviral agent, has been demonstrated that there were beneficial effects in antiviral treatment4 ; however, some studies have not documented its effectiveness on coronavirus therapy. Most important, the drug is expensive and can just be administered intravenously in a hospital facility.4–6 For convenience and popularity, there is the need to develop simple oral anti-virus drugs available in most patients with COVID-19 infection.
Three are new oral antiviral medications developed and have documented clinical effectiveness in recent studies. Among these oral medications, molnupiravir (MOL), a new orally active RdRp inhibitor with a excellent pharmacokinetic character, has demonstrated to have its ability to interfere SARS-COV-2 replication, and reduce viral load.4 MOL has the unique agent with the isopropyl ester prodrug of the ribonucleoside analogue β-D-N4-hydroxycytidine (NHC).7 Previous studies have found that MOL is an effective interfere of coronavirus replication with an EC50 in the micromolar concentration7–9; the benefit of this antiviral agent has been shown in animal studies.7,10,11 One report showed that a greater proportion of viral clearance achievement was observed in subjects administered with MOL vs placebo.12 Moreover, MOL has well demonstrated promising treatment efficacy and safety profiles in previous clinical studies and trials. Studies have documented that MOL has the efficacy with the near 50% risk reduction of hospitalization or mortality in non-hospitalized patients infected with mild-to-moderate COVID-19 disease severity who have underlying comorbidities and risk factors for poor prognosis. Besides, the safety was similar between the study and placebo group (adverse events: 35% and 40%, respectively), as was the incidence of drug-related adverse events (12% and 11%, respectively).13 Another oral medication, fluvoxamine, a selective serotonin reuptake inhibitor and σ-1 receptor agonist,14 has potential benefits of early non-hospitalized patients’ treatment of COVID-19 in previous trials.15–17 However, there was no significant clinical effectiveness in hypoxemia prevention, reduced emergency department visit, hospitalization rate, or mortality associated with coronavirus.18 Paxlovid is another promising agent with SARS-CoV-2 protease inhibitor antiviral therapy, specifically designed to be administered orally.19 Their recent trial had showed that Paxlovid can reduce the 89% risk of hospitalization or mortality rate.19 In the clinical practice, however, Paxlovid has some limitations including many drug interactions and is not administered in patients using nasogastric (NG) tube feeding.
Assessment of drugs administered of the COVID-19 management protocols has been documented.20 These protocols are very practical even with the development and approval of several vaccines. These recommendations were instructed to aid home isolation, bed rest, dietary supplements, and additionally the administration of antipyretic, steroids, and antiviral drugs. As we know, many COVID-19 patients with comorbidity, bed-ridden status and NG tube feeding in the healthcare facilities and may have been poorer outcome if these patients without suitable oral anti-viral agents. Besides, there were few studies to elucidate the treatment benefits for MOL in patients lived healthcare facilities. The aim of the study will evaluate the effectiveness of using MOL in these facilities in Taiwan.
Methods
Study Design and Population
This is a prospective and observational study. All patients infected with COVID-1 were admitted in the healthcare facilities. These patients have received third COVID-19 vaccination. The confirmed diagnosis of COVID-19 infection was based on rapid antigen test with positive results. The equipment and facilities of rapid antigen tests were used: 1) SD BIOSENSOR Rochi, 2) GenBody Inc, and 3) Abbott® Laboratories. Patients were SARS-CoV-2 infection that had performed rapid antigen test-confirmed no more than 3 days earlier. Besides, onset of signs or symptoms less than 3 days, at least one sign or symptom of COVID-19 and physicians would receive MOL therapy (800mg/day) 5 days’ treatment course after confirmation diagnosis via video consultation. All medical records were reviewed and analyzed. Ethical approval from the hospital (IRB number: 111247-E, approval by the institutional review board, Far Eastern Memorial Hospital), and informed consents from all study subjects were obtained. The study follows the rules of the Declaration of Helsinki.
There were 1035 patients with COVID-19 infection enrolled and treated with MOL in 46 health-care facilities and 856 patients completed the survey and analyzed from May 2022. All these patients did not use ventilator support. There were only 102 patients (11.9%) with oxygen demand using oxygen cannula. The demographics of patients were as follows: average age was 78.4 ± 25.8 years, male was 521 (60.8%) and female was 335 (39.2%).
Evaluation of Therapeutic Effects
All patients were received with MOL therapy after confirmation COVID-19 diagnosis. The assessment parameters including COVID-19 symptoms, daily vital signs, oxygenation status. Caregivers in facilities should report patients’ COVID-19 signs and symptoms through day 28 after MOL therapy. Clinical improvement and deterioration of coronavirus’ symptoms and signs were defined as any reduction and worsening, respectively, compared with baseline symptoms’ severity. The time to sustained improvement of symptoms or signs was defined as the number of days from the initial therapy (the first of 5 consecutive days) to resolution or alleviation (without symptoms or signs relapse by day 28) and the time to deterioration of clinical symptoms or signs as the number of days from treatment (the first of 5 consecutive days) to the days of symptoms worsening. Patients should be hospitalized if symptoms progressed, poor oxygenation, and unstable vital signs. The effectiveness for MOL treatment was classified into three groups including cure group, stable group, and hospitalization group. The definition of cure group is without symptoms and without viral replication that is negative antigen test, and no need for hospitalization; stable group should be divided into three groups including no viral replication but symptom presence, prolonged viral replication with or without symptoms and no need for hospitalization; hospitalization group is symptoms got worse and need for hospitalization.
Statistical Analysis
Continuous variables are recorded as mean and standard deviation (SD). Descriptive statistics for demographics and patient’s characteristics, comorbidities and clinical outcomes are provided. ANOVA multiple comparisons, using Tukey’s HSD (honest significant difference) tests, were performed between users of different parameters for all clinical outcomes. Chi-square tests of independence and ANOVA F-tests were done for each parameter. All statistical analyses were performed using SAS® version 9.4 (Windows NT version, SAS Institute, Inc., Cary, NC, USA) and R (version 3.4.2; R Foundation for Statistical Computing, Vienna, Austria). A two-tailed P-value less than 0.05 was taken as significance.
Results
The aim of the study is to evaluate the effectiveness and benefit for MOL treatment. The cure group after MOL therapy was 496 (57.9%) and stable group was 256 (29.9%). There were 104 hospitalized patients (12.1%) because sustained symptoms still progressed. After hospitalization, 22 patients (2.6%) died due to multiple organ failure and septic shock. Eighty-two patients (9.6%) were improved and discharge after hospitalization. The average time for symptoms and signs resolution was 7.9 ± 3.6 days, and time for diseases progression was 2.2 ± 1.9 days. The recovery time for symptoms resolution was slow in cure and stable groups; however, patients needed to be hospitalized were still deteriorated in the second to third days though early administration MOL therapy. Most important, most patients were cured and in a stable condition to prevent critical illness development after early MOL prescription.
The characteristics of MOL treated patients with different groups are analyzed in Table 1. Patients still needed to receive hospitalized treatment included more elder years (84.4± 23.7), and more underlying comorbidities including old cerebrovascular accident (CVA), diabetes mellitus (DM) and respiratory diseases. There were significant statistical differences in elder age and three comorbidities compared with cure and stable group patients. Healthcare COVID-19 patients with elder age, CVA, DM and lung diseases would develop severe pneumonia and diseases.
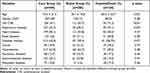 |
Table 1 Demographic Characteristics of the COVID-19 Patients with Diverse Groups |
Multivariate analysis was performed to find the risk factors for developing severe illness (hospitalization/death). After adjusting parameters for sex, medications, significant risk factors including elder age (>80 years old) (odds ratio (OR) 2.2, 95% confidence interval (CI): 1.1–6.9), old cerebrovascular accident (CVA) (OR=4.1, 95% CI: 1.3–9.9), the presence of diabetes mellitus (DM) (OR=2.6, 95% CI: 1.2–9.1) and chronic respiratory diseases (OR=2.4, 95% (CI): 1.3–8.1) were identified (Table 2).
 |
Table 2 Multi-Variate Analysis of Risk Factors for Hospitalization in Health-Care Patients with COVID-19 Infection |
There were few adverse effects or events during the MOL treatment course (day 1 to day 5) and evaluation time (day 28). These adverse effects included mild diarrhea (1.2%) and skin rash (0.9%). The administration of MOL was relatively safe and effective.
Discussion
This was first study in Taiwan to evaluate the effectiveness for MOL treatment with COVID-19-infected patients in healthcare facilities. The dominating SARS-CoV-2 genotypes were Omicron two subtype (BA.1 and BA.2) in Taiwan in 2022. Early administration of anti-viral agents’ treatment was very essential to avoid COVID diseases progression, and our result demonstrated that there was an 87% cure and stable conditions among patients who received MOL, suggesting that early control of viral replication prevented progression to severe illness and death. In a recent study, initial treatment with MOL reduced the risk of hospitalization or death in at-risk, unvaccinated adults with Covid-19.21 Therefore, MOL has excellent effectiveness of treatment with these patients who lived in healthcare facilities.
There were some limitations for Paxlovid administration in our study patients. First, among patients who lived at a healthcare facility, there were multiple renal and hepatic impairment. It is difficult to adjust medications dosage. Second, multiple drugs would interrupt Paxlovid absorption and patients had taken many drugs for underlying comorbidities. It should pay more attention to these drug–drug interactions. Third, there were more NG tube replacement in our patients. Paxlovid was not administered via NG tube. However, MOL did not have the aforementioned limitations. In our patients, there were near 80% patients with NG tube in healthcare facilities. MOL is a very suitable oral form anti-viral agent for these patients in healthcare facilities. In the past studies, MOL is also the oral, direct-acting antiviral shown to be highly effective at reducing nasopharyngeal SARS-CoV-2 infectious virus and viral RNA and has a favorable safety and tolerability profile.22,23
In our study, we mentioned that patients with elder age, old CVA, DM and respiratory diseases would develop critical illness in COVID-19 infection. Many review articles had elucidated these risk factors for mortality in patients with COVID-19 infection.24–28 These risk factors included older age (≥65 years), male gender, hypertension, CVDs, diabetes, chronic obstructive pulmonary disease (COPD), high D-Dimer titles, malignancies, etc were associated with greater risk of death from COVID-19 infection. It is also reasonable that patients would progress the COVID-19 infection due to underlying conditions (relative immunocompromised), poor cough function and sputum expectoration clearance ability. These findings could help clinicians find patients with poor prognosis at an early stage, and we also should more pay attention to these patients with high-risk factors and close monitor clinical courses.
There were some limitations in our study. First, it is not a randomized study and there is no placebo group. All COVID-19 patients need to be treated. Second, not all patients lived in healthcare facilities could survey and evaluate treatment responses completely. Therefore, there were still 179 patients who did not finish all monitors. Third, this is a clinical and observational study. No viral titer loading, or experimental studies were performed.
In conclusion, this is a first study to confirm the treatment effectiveness and safety using MOL in patients who lived in healthcare facilities with COVID-19 infection. Ninety percent of the patients prevented the development of critical illness, and only 1% have mild adverse effects. Risk factors to develop severe illness include elder age, old CVA, DM and respiratory diseases. MOL is well effective in COVID-19 infection and prevent to progress critical illness. Further studies should be performed to confirm the efficacy of the combined two anti-viral agents and the potential genetic risks for MOL.
Acknowledgments
This study was supported by grants from the Far Eastern Memorial Hospital FEMH-2021-C-20.
Author Contributions
Dr Cheng: study design, correct the study data, draft the manuscript. Dr Wang, Dr Chang: correct the data. Dr Chiu: organize the study. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no competing interests in this study.
References
1. Rufaida MT, Kedwai I, Ahsan F, Shamim A, Shariq M, Parveen S. A dossier on COVID-19 chronicle. J Basic Clin Physiol Pharmacol. 2021;33(1):45–54.
2. Imran M, Kumar Arora M, Asdaq SMB, et al. Discovery, development, and patent trends on molnupiravir: a prospective oral treatment for COVID-19. Molecules. 2021;26(19):5795. doi:10.3390/molecules26195795
3. Christie A, Mbaeyi SA, Walensky RP. CDC interim recommendations for fully vaccinated people: an important first step. JAMA. 2021;325(15)::1501–1502. doi:10.1001/jama.2021.4367
4. Vitiello A, Troiano V, La Porta R. What will be the role of molnupiravir in the treatment of COVID-19 infection? Drugs Ther Perspect. 2021;37(12):572–579. doi:10.1007/s40267-021-00879-2
5. Ferner RE, Aronson JK. Remdesivir in covid-19. BMJ. 2020;369:m1610. doi:10.1136/bmj.m1610
6. Vitiello A, Ferrara F, Porta R. Remdesivir and COVID-19 infection, therapeutic benefits or unnecessary risks? Ir J Med Sci. 2021;190(4):1637–1638. doi:10.1007/s11845-020-02482-2
7. Menéndez-Arias L. Decoding molnupiravir-induced mutagenesis in SARS-CoV-2. J Biol Chem. 2021;297(1):100867. doi:10.1016/j.jbc.2021.100867
8. Zhao J, Guo S, Yi D, et al. A cell-based assay to discover inhibitors of SARS-CoV-2 RNA dependent RNA polymerase. Antiviral Res. 2021;190:105078. doi:10.1016/j.antiviral.2021.105078
9. Agostini ML, Pruijssers AJ, Chappell JD, et al. Small-Molecule antiviral β-d- N 4-Hydroxycytidine inhibits a Proofreading-Intact coronavirus with a high genetic barrier to resistance. J Virol. 2019;93(24):e01348–19. doi:10.1128/JVI.01348-19
10. Rosenke K, Hansen F, Schwarz B, et al. Orally delivered MK-4482 inhibits SARS-CoV-2 replication in the Syrian hamster model. Nat Commun. 2021;12(1):2295. doi:10.1038/s41467-021-22580-8
11. Sheahan TP, Sims AC, Zhou S, et al. An orally bioavailable broad-spectrum antiviral inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice. Sci Trans Med. 2020;12(541):eabb5883. doi:10.1126/scitranslmed.abb5883
12. Fischer W, Eron JJ, Holman W, et al. Molnupiravir, an oral antiviral treatment for COVID-19. medRxiv. 2021;1:548.
13. Mahase E. Covid-19: molnupiravir reduces risk of hospital admission or death by 50% in patients at risk, MSD reports. BMJ. 2021;375:n2422. doi:10.1136/bmj.n2422
14. Calusic M, Marcec R, Luksa L, et al. Safety and efficacy of fluvoxamine in COVID-19 ICU patients: an open label, prospective cohort trial with matched controls. Br J Clin Pharmacol. 2021;88(5):2065–2073. doi:10.1111/bcp.15126
15. Seftel D, Boulware DR. Prospective cohort of fluvoxamine for early treatment of coronavirus disease 19. Open Forum Infect Dis. 2021;8(2):ofab050. doi:10.1093/ofid/ofab050
16. Lenze EJ, Mattar C, Zorumski CF, et al. Fluvoxamine vs. placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial. JAMA. 2020;324(22):2292–2300. doi:10.1001/jama.2020.22760
17. Reis G, Dos Santos Moreira-Silva EA, Silva DCM, et al. Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial. Lancet Glob Health. 2022;10(1):e42–e51. doi:10.1016/S2214-109X(21)00448-4
18. Bramante CT, Huling JD, Tignanelli CJ, et al. Randomized Trial of Metformin, Ivermectin, and Fluvoxamine for Covid-19. N Engl J Med. 2022;387:599–610. doi:10.1056/NEJMoa2201662
19. Pfizer’s novel COVID-19 oral antiviral treatment candidate reduced risk of hospitalization or death by 89% in interim analysis of Phase 2/3 EPIC-HR study; 2021. Available from: https://www.pfizer.com/news/press-release/press-release-detail/pfizers-novel-covid-19-oral-antiviral-treatment-candidate.
20. Elekhnawy E, Negm WA, El-Sherbeni SA, Zayed A. Assessment of drugs administered in the Middle East as part of the COVID-19 management protocols. Inflammopharmacology. 2022;30(6):1935–1954. doi:10.1007/s10787-022-01050-7
21. Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients. N Engl J Med. 2022;386(6):509–520. doi:10.1056/NEJMoa2116044
22. Lee CC, Hsieh CC, Ko WC. Molnupiravir-A Novel Oral Anti-SARS-CoV-2 Agent. Antibiotics. 2021;10(11):1294. doi:10.3390/antibiotics10111294
23. Fischer W, Eron JJ, Holman W, et al. Molnupiravir, an Oral Antiviral Treatment for COVID-19. medRxiv. 2021;17:21258639.
24. Parohan M, Yaghoubi S, Seraji A, Javanbakht MH, Sarraf P, Djalali M. Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Aging Male. 2020;23(5):1416–1424. doi:10.1080/13685538.2020.1774748
25. Xiang G, Xie L, Chen Z, et al. Clinical risk factors for mortality of hospitalized patients with COVID-19: systematic review and meta-analysis. Ann Palliat Med. 2021;10(3):2723–2735. doi:10.21037/apm-20-1278
26. Rahman MM, Bhattacharjee B, Farhana Z. Age-related risk factors and severity of SARS-CoV-2 infection: a systematic review and meta-analysis. J Prep Med Hyg. 2021;62(2):E329–E371.
27. Silverio A, Di Maio M, Citro R. Cardiovascular risk factors and mortality in hospitalized patients with COVID-19: systematic review and meta-analysis of 45 studies and 18,300 patients. BMC Cardiovasc Disord. 2021;21(1):23. doi:10.1186/s12872-020-01816-3
28. Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21(1):855. doi:10.1186/s12879-021-06536-3
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
