Back to Journals » Journal of Asthma and Allergy » Volume 16
The ATLAS ASMA Study: Assessing the Impact of Asthma on Patients’ Life – The Spanish Patients’ Perspective
Authors Dominguez-Ortega J , Plaza V , Nieto A, Delgado Romero J, Ancochea J , Mejia N, Pastor M, Blanco-Aparicio M
Received 2 February 2023
Accepted for publication 5 April 2023
Published 3 May 2023 Volume 2023:16 Pages 461—471
DOI https://doi.org/10.2147/JAA.S404525
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Javier Dominguez-Ortega,1 Vicente Plaza,2 Antonio Nieto,3 Julio Delgado Romero,4 Julio Ancochea,5– 7 Natalia Mejia,8 Mariano Pastor,9 Marina Blanco-Aparicio10
1Department of Allergy, La Paz University Hospital, Institute for Health Research (IdiPAZ), Madrid, Spain; 2Department of Respiratory Medicine, Hospital de la Santa Creu i Sant Pau, Instituto de Investigación Biomédica Sant Pau, Barcelona, Spain; 3Pediatric Pulmonology and Allergy Unit, Hospital Universitari i Politècnic La Fe, Health Research Institute La Fe, Valencia, Spain; 4Allergology Clinical Management Unit, Hospital Virgen Macarena, Sevilla, Spain; 5Pneumology Department, Instituto de Investigación Sanitaria de La Princesa, Madrid, Spain; 6Pneumology Department, Facultad de Medicina, Universidad Autónoma de Madrid, Madrid, Spain; 7Centro de Investigación en Red de Enfermedades Respiratorias (CIBERES), Instituto de Salud Carlos III (ISCIII), Madrid, Spain; 8Medical Department, Novartis Farmacéutica, Barcelona, Spain; 9Fundación Española de Asociaciones de Pacientes Alérgicos y con Enfermedades Respiratorias (FENAER), Madrid, Spain; 10Pneumology Department, A Coruña University Hospital, A Coruña, Spain
Correspondence: Javier Dominguez-Ortega, La Paz University Hospital, Institute for Health Research (IdiPAZ), Madrid, Spain, Tel +34 616 719 390, Email [email protected]
Purpose: ATLAS ASMA described the psychosocial impact of asthma on patients’ daily life from patients’ perspectives (in terms of impaired personal and intimate relationships, sleep quality, leisure time, daily activities, and others) in Spain. Secondary objective includes description of time since diagnosis, expectations, and satisfaction of patients about disease, treatment and medical assistance received, adherence to treatment, perceived control of asthma, and health-related quality of life.
Patients and Methods: This was a cross-sectional, observational study, based on a self-administered online survey for adult patients (≥ 18 years) with asthma. Patients with asthma diagnosis of any type and severity who voluntarily participated in the survey through a web link were included consecutively. In the present manuscript, only adult patients’ data are included.
Results: A total of 132 adults with asthma were included. Moderate/severe asthma constituted 59.1% of the patients (females 71.2%). Overall, most relevant areas affected due to asthma were leisure activities (67.0%) and the quality/quantity of sleep (52.3%). Moderate/severe patients perceived some degree of impairment in work, school, or at home due asthma more frequently vs mild patients (55.2% vs 10.9%). Poorly controlled asthma (ACT≤ 19) was reported in 41 (70.7%) and 10 (21.7%) moderate/severe and mild patients (p< 0.000), respectively. Mild patients obtained higher mean (SD) Mini-AQLQ score than moderate/severe asthma patients (5.6 [1.0] vs 4.3 [1.1], p< 0.000), likewise higher significant results for every individual dimension. Most patients cited little limitation to intense efforts (20.5%). Half of the patients mentioned needing more information about asthma. Topics those patients like to have more information were difficulties that may can have and legal topics (78.6%), asthma evolution (78.6%), secondary effects or issues related to the treatment (61.9%) and legal topics (61.9%).
Conclusion: The study reported important insights on psychosocial impact of asthma on patients’ daily life from patients’ perspectives along with health determinants in asthma-related health outcomes, sociodemographic and psychosocial factors.
Keywords: patient survey, psychosocial impact, health-related quality of life, healthcare resources utilization, Asthma Control Test, Mini-AQLQ
Introduction
Asthma in adults is characterized with accelerated deterioration of lung function and increase the risk of fixed air flow obstruction.1 It is one of the most common chronic, non-communicable diseases associated with bronchial hyper-responsiveness and varying degree of airflow obstruction.2,3 Asthma in adults is known for female predominance, uncommon remission, and unusual mortality.4
On these grounds, asthma is considered a major global public health concern that involves a significant economic burden (for both children and adults), accounting for high morbidity and mortality in severe cases.1 Concretely, asthma is ranked 16th among the leading causes of years lived with disability and 28th among the leading causes of disease burden globally.5 Almost 300 million individuals are suffering from asthma worldwide, and it is likely that a further 100 million may be affected by 2025.5 Asthma affects nearly more than 20% of individuals in developed countries and around 3–5% in developing and underdeveloped countries.6 In Spain, prevalence among adults and children is reported to be 5% and 10%, respectively, accounting for more than 3 million people living with asthma.7 In recent decades, there has been an increase in asthma cases. The factors like industrialization and modern lifestyle have contributed significantly to this increased asthma burden.8,9
In addition, healthcare professionals (HCPs) and patients perceive asthma in a significantly different way.10 Clinicians can focus more on control, assessed by the presence of symptoms and use of medication, exacerbations and/or validated questionnaires such as Asthma Control Test (ACT). Whereas for patients, quality of life and impact on their work activities aspects are very important. Understanding the patient’s perspective may help HCPs to optimize therapies and improve asthma control.11,12 Understanding patients’ perspective can support physicians, other HCPs, and health institutions to structure and prioritize patient needs and management. Several questionnaires have been validated in asthma to assess health-related QoL (HRQoL) such as ACT and Mini Asthma Quality of Life Questionnaire (AQLQ).13 Even though many online patient surveys have been carried out, a study including the objective assessment of asthma control by ACT and assessment of quality of life by validated questionnaire has not been carried out. In addition, asthma assessment approach should also appraise other qualitative aspects of asthma (such as impact on daily activities, social impact, expectations about the future, etc.) to determine factors that are important for patients.14 The functional limitation that is linked with asthma, particularly the ability to perform activities of daily living, is a very important aspect, which in cases of severe asthma can affect 85% of patients and results in loss of labor productivity.15
The study was conducted to describe the psychosocial impact of asthma on patients’ daily life from patients’ perspectives, in terms of impaired personal and intimate relationships, sleep quality, leisure time, daily activities, and other relevant aspects. The study also describes the time since diagnosis, time from the onset of symptoms to diagnosis, time since diagnosis to treatment initiation, and type of HCPs who diagnosed the asthma. Additionally, the study evaluates direct and indirect use of healthcare resource use (HCRU), expectations and satisfaction of patients, treatment and medical assistance received, adherence to treatment, perceived control of asthma, and HRQoL. Taken together, the current study collected information about some scarcely investigated dimensions of patients’ perspective, through a structured survey. So far, no other studies in Spain have aimed to cover the multidimensional factors impacting daily life of patients with all asthma spectrum, ranging from mild to severe, from their own perspective.
Materials and Methods
Study Design and Setting
The main objective was to describe the psychosocial impact of asthma on patients’ daily life from patients’ and caregivers’ perspective, in terms of impaired personal and intimate relationships, sleep quality, leisure time, daily activities and other relevant aspects. Other secondary study objectives were i) to describe the time since diagnosis, time from the onset of symptoms to diagnosis, time since diagnosis to treatment initiation and type of HCP who diagnosed the asthma (patient pathway). ii) To describe direct and indirect use of resources and iii) psychological impact of asthma in adult patients. iv) To describe expectations and satisfaction of patients about disease, treatment and medical assistance received. v) To describe the adherence to treatment and the perceived control of asthma. vi) To evaluate the HRQoL and vii) describe the opinion of patients about the information received about the disease and main sources of information consulted.
ATLAS ASMA was a cross-sectional observational study based on a self-administered online survey for patients with asthma in Spain. In the present manuscript adult (18–75 years) patients’ outcomes are included. The study included patients with diagnosis of any type and severity of asthma. The number of patients were distributed in 2 groups according to disease severity: patients with mild asthma and patients moderate/severe asthma. Asthma diagnosis and severity (mild, moderate, and severe) were self-reported.
Participants were included consecutively as they proactively participated in the survey through the link indicated in the promotion. Before starting the survey, participants give their consent and verified that they met all the selection criteria. The study included patients who reported their asthma diagnosis and its severity.
The study was conducted according to the Declaration of Helsinki. Protocol and survey were approved by the Ethical and Clinical Research Committee of the Clinic hospital of Barcelona, with the ethics approval number HCB/2020/1376. Patients who agreed to participate and to abide by data privacy policy were included in the study survey.
Survey Development
The survey was created and endorsed by a scientific committee formed by asthma experts (physicians, investigators, and health economics experts) with large experience in the design of surveys. The study objectives were assessed using validated questionnaires/scales (ACT and Mini-AQLQ).
Participation in the online survey was completely voluntary and the online survey participants were anonymized, through the survey platform. The data collection duration was from 27th January 2021 to 31st July 2021. The survey participants were the ones who, if interested in the information provided through advertising channels (such as patients’ associations, scientific and medical associations, google add words, radio, press, etc.), decided to participate by accessing to the web link.
Study Variables
Psychosocial Impact on Daily Life
This primary endpoint was measured as the percentage of patients who perceived limitations in different aspects of life and required help to do these activities and the patients who identify themselves with each feeling within the society.
Secondary Endpoints
- Sociodemographic and clinical characteristics: Baseline sociodemographic and clinical features of mild and moderate/severe patients were assessed.
- Time and patient pathway: Time since diagnosis, elapsed time from the onset of symptoms to the diagnosis, time since diagnosis to treatment initiation, and type of HCPs who diagnosed the asthma were captured.
- Direct and indirect resource use: Direct health resources were assessed in terms of medical visits, hospitalizations, emergency visits, patients currently on treatment for asthma, patients receiving maintenance, rescue/relief or both type of medication. Direct non-healthcare resources were measured in terms of transport and need for a formal and/or informal caregiver, hours per month, and cost per month. Indirect resources (work productivity loss) were also assessed.
- Social and psychological impact: Psychological impact of asthma was measured in terms of emotional affectation and impact on personality traits (patience, concentration, self-confidence, irritability, etc.).
- Expectations and satisfaction: Expectations related to disease, expectations at the time of diagnosis about the future of respiratory symptoms and treatment benefits and satisfaction with treatment and medical assistance were reported.
- Adherence: Patients’ adherence to treatment (patients who stopped taking the treatment/following the treatment) and perceived asthma control were also assessed.
- Asthma HRQoL assessment: HRQoL was assessed by Mini-AQLQ.
- Opinion of patients about the information received, main sources of information consulted and opinion about telemedicine.
Sample Size & Statistical Analysis
The main study objective consisted of a descriptive analysis of many numerical and categorical endpoints. Therefore, the sample size has been calculated based on statistical criteria, using the criterion of maximum indeterminacy (when the percentage of one category in a categorical variable is expected to be around 50%). This sampling technique is a method of taking a small ratio of observation from a large population to get information of those large populations from the sampled observation by using some statistical techniques.16
The statistical analysis was performed by using Statistical Analysis System (SAS) Enterprise Guide 7.14. The description of all the variables was made for the total and for each subgroup based on severity of asthma (mild or moderate/severe). Sociodemographic and clinical characteristics of the participants were described. The mean, standard deviation (SD), median, quartiles (Q1 and Q3), minimum and maximum for describing continuous variables were used. The number and percentage of patients per response category were used to describe the categorical variables. No imputation of missing values was done for any variable. Counts (ie, number of visits or Mini-AQLQ scores, among others) were treated as continuous variables.
Results
Sociodemographic and Clinical Characteristics
A total of valid 132 adult patients with asthma were analyzed for this study. Moderate/severe asthma represented 59.1% (78) of the patients. Overall, mean age (SD) was 43.3 (13.1) years, and significantly higher for moderate/severe asthma patients (45.7 [12.6] years) than mild patients (39.8 [13.1] years). More than 70% (94) of the patients were females (mild 66.7% vs moderate/severe 74.4%) (Table 1).
 |
Table 1 Sociodemographic and Clinical Characteristics of Patients with Asthma |
Psychosocial Impact of Asthma on Patients
Overall, 59 (67.0%) patients mentioned leisure activities to be the most relevant area affected due to asthma. As far as feeling within society is concerned, 36 (40.9%) patients feel that they were limited in their activities due to asthma. Thirty-seven (35.6%) adults reported some degree of impairment in performing at work, school, or home in the past 4 weeks. In terms of difficulty in breathing due to asthma, 29 (37.2%) patients mentioned some degree of impairment. Thirty-six (46.2%) patients reported some limitations to intense efforts (mild asthma 18.4% vs moderate/severe asthma 72.5%), 28 (35.9%) patients reported some degree of impairment to perform moderate efforts. When talking about limitations in social activities, 17 (21.8%) patients mentioned some degree of impairment. As for limitations in work tasks, 16 (20.5%) patients mentioned that they experienced some degree of impairment (Table 2).
 |
Table 2 Psychosocial Impact of Asthma on Daily Life of Patients |
Times and Patient Pathway of Asthma
Even though the mean (SD) time for first symptoms of asthma to diagnosis was lower with mild asthma (1.7 years [2.9]) than moderate/severe asthma (2.9 years [4.8]), the mean (SD) time for asthma diagnosis was higher with mild asthma, ie, 21.2 (12.6) years in comparison to 18.9 (4.8) years in moderate/severe asthma. The specialty who gave maximum asthma diagnosis was pneumologist, in 39 (39.3%) patients (Table 3).
 |
Table 3 Times and Patient Pathway in Asthma |
Use of Direct and Indirect Resources
A mean (SD) of 2.5 (3.6) scheduled visits, 0.8 (1.8) crisis/episode visits, and overall, 3.3 (4.8) visits to professionals were reported in the last 4 months. Adults with moderate/severe asthma (4.3 [5.2]) had significantly higher total mean (SD) visits to the medical personnel than mild asthma (2.1 [4.2]) (p=0.001). Primary healthcare family doctor was the most visited professional with mean (SD) visits of 1.2 (2.3), mostly by patients with moderate/severe asthma (mild asthma 0.8 [1.8] vs moderate/severe asthma 1.6 [2.6]) (p=0.016).
A total of 13 (14.8%) patients had an emergency in the last year. The mean (SD) number of emergency visits was 2.0 (1.3) (mild asthma 1.5 [0.7] vs moderate/severe asthma 2.1 [1.4]).
One (2.4%) and 12 (26.1%) patients with mild asthma and moderate/severe asthma, respectively, reported help of caregiver without economic benefits (p=0.002). The mean (SD) time doing assistance was 1.9 (0.9) hours/day and 4.5 (2.5) days/week.
In case of loss of work productivity of informal caregiver and other expenditures, 4 (9.5%) and 17 (37.0%) patients with mild asthma and moderate/severe asthma, respectively, reported other expenses related to asthma (p=0.003). Mean of €/month for additional expenses were 9.0 (8.5) for mild asthma and 97.1 (118.5) €/month for moderate/severe asthma (Tables S1–S7).
Expectation and Satisfaction to the Treatment
Most of the mild asthma patients, ie, 23 (62.2%) and 17 (42.5%) of moderate/severe asthma patients did not expect evolution of respiratory issues since asthma diagnosis because they did not have enough asthma information (p=0.026). Regarding expected results for treatment, 21 (56.8%) of mild asthma patients and 27 (67.5%) for moderate/severe asthma patients were expecting to improve a lot.
Nineteen (51.4%) patients with mild asthma were quite satisfied with the treatment, while fifteen (37.5%) moderate/severe asthma patients were in the same category (satisfied p=0.0183). Only 6 (15.0%) moderate/severe asthma patients were unsatisfied.
Treatment Adherence and Asthma Control
Thirty-two (36.8%) patients declared that they stopped taking treatment on any occasion in the last month. The main reasons were that it was forgotten (20 [62.5%]) and that the patient thought that the treatment was not needed (10 [31.3%]). Thirty-six (41.4%) patients (51.4% in mild asthma and 34.6% in moderate/severe asthma) reported no effort or discomfort in taking the treatment, while 29 (33.3%) reported little effort or discomfort. Overall, 87 (87.9%) patients followed the treatment daily, in crisis or both. Fifty-two (96.3%) of the moderate/severe asthma patients followed the treatment in comparison to 35 (77.8%) patients with mild asthma (p=0.005).
Mean (SD) ACT score (used for assessing asthma control) was 18.7 (4.8) points. A total of 51 (49.0%) patients reported ACT cut-off ≤19 points (poorly controlled) (Figure 1).
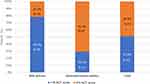 |
Figure 1 Asthma control in patients. Abbreviations: ACT, Asthma Control Test; N, Number of patients. |
HRQoL
The mean score (SD) in the Mini-AQLQ was 5.0 (1.2) points, with the environmental stimuli dimension being the dimension with a lower score (worse HRQoL). The patients with mild asthma obtained higher scores than the patients with moderate/severe asthma, 5.6 vs 4.3 in the global score, respectively (Figure 2).
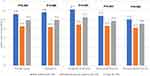 |
Figure 2 HRQoL of patients with asthma. Abbreviations: HRQoL, Health-related quality of life; Mini-AQLQ, Mini Asthma Quality of Life Questionnaire. |
Opinion of Patients About the Information Received and Main Sources of Information Consulted
The most common topics on which information was received in the last 6 months by a doctor or nurse to adults were: available social benefits or assistance (70 [83.3%]), limitations that may have due to asthma (35 [41.7%]), and evolution of asthma (32 [38.1%]). The responses were similar in both patients with mild and moderate/severe asthma.
Forty-two (50%) patients mentioned needing more information about asthma. Topics on which patients like to have more information were: difficulties that may can have and legal topics (33 [78.6%]), asthma evolution (33 [78.6%]), secondary effects or issues related to the treatment (26 [61.9%]) and legal topics (26 [61.9%]). The principal source to consult information about asthma was consult to doctor.
Discussion
ATLAS ASMA study is among the very few studies that provide valuable insights on the perceptions, HCRU and humanistic burden of adult population with asthma in Spain. The significance of this study increases manifold, considering the current scenario of COVID-19 pandemic that has directly impacted continuum of care of patients with asthma.17–19
Several social and environmental factors associated with negative health outcomes in asthma patients are well established.20 Our study reported higher proportion of women among patients with asthma. This finding, which is in line with other studies, suggest that there is a higher prevalence in adult women.21,22 Male predominance is usually observed from infancy or early childhood until 16 years of age.23,24 Population sample in our study was with high educational status which contradicts other studies in which the effect of a lower socioeconomic level is associated with worse control and other asthma factors. But it can be attributed to the survey characteristic of the study that requires online access.
An evident psychosocial impact of asthma on patients in both patients (mild and moderate/severe asthma) is demonstrated. Moderate/severe asthma patients seemed more psychosocially affected than those with mild asthma. Asthma control and asthma exacerbations can be influenced by factors, such as the presence of comorbidities, anxiety, and abnormal body mass index affect.25,26
We have observed a higher use of public vs private services in patients with asthma as National Health System provides easier and free access to hospital specialists than in other parts of the world.27 This helps us to determine a pattern of healthcare use. Patients with moderate/severe asthma had higher use of both hospitalizations and ambulances, and days of use of these services. Asthma prevalence is higher in high-income countries and it has been associated with significant economic and HRQoL burden.28 A real-world study from Europe (11 countries) on economic cost of persistent asthma among adults (30–54 years) estimated that the mean total cost per patient was €1583 and which was largely driven by indirect costs (62.5%). The expected total cost in the adult population of European countries was €4.3 billion (€19.3 billion when extended to the whole European population aged from 15 to 64 years).29
In the current study, emotional affectation was reported by patients with mild asthma and moderate/severe asthma. Correlation between anxiety and nervousness and the release of stress hormones are associated with the increased severity of asthma which indicates that regardless of the level/type of asthma, the symptoms altered. Feeling of frustration and worry are also important (led to release of corticosteroids in the body) and present in patients with asthma, but not with the same intensity as anxiety. These findings are in line with reports of worse outcomes for patients with asthma and comorbid depression or anxiety. These findings also suggest improved screening for and management of anxiety and nervousness in patients with asthma.30
Irrespective of the severity of asthma, adherence to treatment is very important. Better adherence is associated with stronger treatment benefits and inadequately treated asthma is related with poor symptom control and lower/bad performance at work and other social situations.31 In the study, clinicians reported that less than 50% of asthma medications are taken as prescribed. A greater adherence was observed with the increase in asthma severity. This was also observed in other studies that related perception of severity with adherence.31 In terms of asthma control, there is an apparent inverse pattern: greater the severity of asthma, lower the asthma control. This study allows to gather information on the perception of adherence in the middle of several psychosocial and environmental changes due to the pandemic.
There are different potential limitations to this study. The main one is the low recruitment of patients. A sample size of 882 patients was estimated for a percentage of 50%, with a 95% confidence interval (CI) of ±3.3 percentage units. In this way, the continuous variables were estimated with an accuracy of 0.066 SD. Considering that around 10% of patients might not produce evaluable data, the number of adult patients with asthma had to be included were approximately 987 patients (mild asthma 20% of sample [197 patients] and moderate/severe asthma 80% [790 patients]). However, the study experienced low recruitment and discontinuation of the recruitment because COVID-19 pandemic reduced face-to-face visits and the possibility of adequately explaining the purpose of the survey and the importance of their participation. The information about the study and the access link to the survey were published in different media so that interested patients could participate and complete the questions. Despite the measures that were taken to try to ensure the access to the survey, it was not possible to reach more population. One more limitation was related with the source of information, participants can be influenced by the effect of memory and by their subjectivity. Finally, the method of patient recruitment may lead to a study sample not representative of the overall population with asthma in Spain. Firstly, there is a risk that only patients with computer skills and Internet access might accept to participate. Secondly, there is also the risk that most patients could come from patients’ associations, being better informed and therefore likely to have better disease control. In addition, asthma diagnosis and severity classification (mild, moderate, and severe) were made by the patient/family member, and therefore physician conformation was not performed. However, even while considering these limitations, the present findings constitute the first real-world evidence study showing the importance from a patient’s perspective of the asthma humanistic burden and its associated HCRU in Spain.
Conclusion
ATLAS ASMA study has obtained important findings on asthma-related health outcomes, such as sociodemographic, social, and psychosocial impact on daily life, cost of care in the healthcare system (measured through direct and indirect HCRU), patients’ adherence to treatment, perceived asthma control, and HRQoL. Also, the impact of asthma on health determinants seems to be greater in moderate/severe patients compared to mild patients. The study highlights that the best way to understand how the patient experiences the disease and its consequences is through their own perspective.
Acknowledgments
We thank all the centers and investigators who have collaborated in the study. Also, we thank IQVIA, Carmen Barrull, and Sukanya Ghildiyal for providing medical writing and editorial assistance with this manuscript.
Funding
This study was funded by Novartis Farmacéutica, S.A.
Disclosure
Vicente Plaza: In the last three years, Dr Plaza received honoraria for speaking at sponsored meetings from AstraZeneca, Boehringer-Ingelheim, Chiesi, Gebro, GSK and Sanofi. Received help assistance to meeting travel from AstraZeneca and Chiesi. Act as a consultant for AstraZeneca, Gebro, GSK, Novartis, Teva and Sanofi. And received funding/grant support for research projects from a variety of Government agencies and not-for-profit foundations, as well as AstraZeneca and Chiesi, personal fees from Luminova. Dr Javier Dominguez-Ortega and Dr Antonio Nieto reports personal fees from NOVARTIS, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Dharmage SC, Perret JL, Custovic A. Epidemiology of asthma in children and adults. Front Pediatr. 2019;7:246. doi:10.3389/fped.2019.00246
2. Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018;391(10122):783–800. doi:10.1016/S0140-6736(17)33311-1
3. GEMA 5.2. Spanish Guideline for the Management of Asthma 2022; 2022. Available from: www.gemasma.com.
4. Trivedi M, Denton E. Asthma in children and adults-what are the differences and what can they tell us about asthma? Front Pediatr. 2019;7:256. doi:10.3389/fped.2019.00256
5. Global Asthma Network. The global asthma report; 2018.
6. Holgate ST, Thomas M. Chapter 7 - Asthma. In: O’Hehir RE, Holgate ST, Sheikh A, editors. Middleton’s Allergy Essentials. Elsevier; 2017:151–204.
7. Cisneros -CD-CR, Marina N, Melero C, et al. Accreditation of specialized asthma units for adults in Spain: an applicable experience for the management of difficult-to-control asthma. J Asthma Allergy. 2017;10:163–169. doi:10.2147/JAA.S131506
8. Nunes C, Pereira AM, Morais-Almeida M. Asthma costs and social impact. Asthma Res Pract. 2017;3(1):1. doi:10.1186/s40733-016-0029-3
9. Wieringa MH, Vermeire PA, Van Bever HP, Nelen VJ, Weyler JJ. Higher occurrence of asthma-related symptoms in an urban than a suburban area in adults, but not in children. Eur Respir J. 2001;17(3):422–427. doi:10.1183/09031936.01.17304220
10. Simpson AJ, Honkoop PJ, Kennington E, et al. Perspectives of patients and healthcare professionals on mHealth for asthma self-management. Eur Respir J. 2017;49(5):1601966. doi:10.1183/13993003.01966-2016
11. Horne R, Price D, Cleland J, et al. Can asthma control be improved by understanding the patient’s perspective? BMC Pulm Med. 2007;7(1):8. doi:10.1186/1471-2466-7-8
12. van der Molen T, Fletcher M, Price D. Identifying patient attitudinal clusters associated with asthma control: the European REALISE survey. J Allergy Clin Immunol Pract. 2018;6(3):962–971. doi:10.1016/j.jaip.2017.10.007
13. F-j G-B, de la Fuente-Cid R, Tafalla M, Nuevo J, Caamaño-Isorna F. Factors associated with health-related quality of life in adults with asthma. A cross-sectional study. Multidiscip Respir Med. 2012;7(1):32. doi:10.1186/2049-6958-7-32
14. Haughney J, Barnes G, Partridge M, Cleland J. The living and breathing study: a study of patients’ views of asthma and its treatment. Prim Care Respir J. 2004;13(1):28–35. doi:10.1016/j.pcrj.2003.11.007
15. Stubbs MA, Clark VL, McDonald VM. Living well with severe asthma. Breathe. 2019;15(2):e40–e9. doi:10.1183/20734735.0165-2019
16. Bhattacherjee A. Social science research: principles, methods, and practices; 2012.
17. Gao YD, Ding M, Dong X, et al. Risk factors for severe and critically ill COVID-19 patients: a review. Allergy. 2021;76(2):428–455. doi:10.1111/all.14657
18. Izquierdo JL, Almonacid C, González Y, et al. The impact of COVID-19 on patients with asthma. Eur Respir J. 2020;2020:2003142.
19. Skevaki C, Karsonova A, Karaulov A, Xie M, Renz H. Asthma-associated risk for COVID-19 development. J Allergy Clin Immunol. 2020;146(6):1295–1301. doi:10.1016/j.jaci.2020.09.017
20. Toskala E, Kennedy DW. Asthma risk factors. Int Forum Allergy Rhinol. 2015;5(Suppl 1):S11–S6. doi:10.1002/alr.21557
21. Leynaert B, Sunyer J, Garcia-Esteban R, et al. Gender differences in prevalence, diagnosis and incidence of allergic and non-allergic asthma: a population-based cohort. Thorax. 2012;67(7):625–631. doi:10.1136/thoraxjnl-2011-201249
22. Postma DS. Gender differences in asthma development and progression. Gend Med. 2007;4:S133–46. doi:10.1016/S1550-8579(07)80054-4
23. SIDRIA (Italian Studies on Respiratory Disorders in Childhood and the Environment). Asthma and respiratory symptoms in 6–7 yr old Italian children: gender, latitude, urbanization and socioeconomic factors. Eur Respir J. 1997;10(8):1780–1786. doi:10.1183/09031936.97.10081780
24. Sunyer J, Antó JM, Kogevinas M, et al. Risk factors for asthma in young adults. Spanish Group of the European Community Respiratory Health Survey. Eur Respir J. 1997;10(11):2490–2494. doi:10.1183/09031936.97.10112490
25. Baptista-Serna L, Rodrigo-Muñoz JM, Mínguez P, et al. Anxiety and body mass index affect asthma control: data from a prospective Spanish cohort. J Allergy Clin Immunol Pract. 2022;10(3):863–6.e1. doi:10.1016/j.jaip.2021.10.013
26. Domínguez-Ortega J, Luna-Porta JA, Olaguibel JM, et al. Exacerbations among patients with asthma are largely dependent on the presence of multimorbidity. J Investig Allergol Clin Immunol. 2022;33. doi:10.18176/jiaci.0816
27. Health Management. Overview of the Spanish healthcare system 2010; 2010. Available from: https://healthmanagement.org/c/it/issuearticle/overview-of-The-spanish-healthcare-system.
28. Serebrisky DWA, Wiznia A. Pediatric asthma: a global epidemic. Ann Glob Health. 2019;85(1):6. doi:10.5334/aogh.2416
29. Accordini S, Corsico AG, Braggion M, et al. The cost of persistent asthma in Europe: an international population-based study in adults. Int Arch Allergy Immunol. 2013;160(1):93–101. doi:10.1159/000338998
30. Munoz FA, Benton LD, Kops SA, Kowalek KA, Seckeler MD. Greater length of stay and hospital charges for severe asthma in children with depression or anxiety. Pediatr Pulmonol. 2020;55(11):2908–2912. doi:10.1002/ppul.25061
31. De Smet BD, Erickson SR, Kirking DM. Self-reported adherence in patients with asthma. Ann Pharmacother. 2006;40(3):414–420. doi:10.1345/aph.1G475
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
