Back to Journals » Patient Preference and Adherence » Volume 8
The association of smoking with medical treatment adherence in the workforce of a large employer
Authors Sherman BW , Lynch W
Received 17 January 2014
Accepted for publication 4 March 2014
Published 16 April 2014 Volume 2014:8 Pages 477—486
DOI https://doi.org/10.2147/PPA.S60927
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Bruce W Sherman,1–3 Wendy D Lynch4,5
1Employers Health Coalition, Inc., Canton, OH, USA; 2Department of Medicine, Case Western Reserve University School of Medicine, Cleveland, OH, USA; 3Sherman Consulting Services, LLC, Burlington, MA, USA; 4Lynch Consulting, Ltd, Steamboat Springs, CO, USA; 5Altarum Institute, Ann Arbor, MI, USA
Purpose: Prior descriptive epidemiology studies have shown that smokers have lower compliance rates with preventive care services and lower chronic medication adherence rates for preventive care services in separate studies. The goal of this study was to perform a more detailed analysis to validate both of these findings for current smokers versus nonsmokers within the benefit-covered population of a large US employer.
Patients and methods: This study involved the analysis of incurred medical and pharmacy claims for employee and spouse health plan enrollees of a single US-based employer during 2010. Multivariate regression models were used to compare data by active or never-smoker status for preventive care services and medication adherence for chronic conditions. Analysis controlled for demographic variables, chronic condition prevalence, and depression.
Results: Controlling for demographic variables and comorbid conditions, smokers had significantly lower cancer screening rates, with absolute reductions of 6%–13%. Adherence to chronic medication use for hypertension was also significantly lower among smokers, with nearly 7% fewer smokers having a medication possession ratio of ≥80%. Smokers were less adherent to depression medications (relative risk =0.79) than nonsmokers (P=0.10). While not statistically significant, smokers were consistently less adherent to all other medications than nonsmokers.
Conclusion: Current smokers are less compliant with recommended preventive care and medication use than nonsmokers, likely contributing to smoking-related employer costs. Awareness of these care gaps among smokers and direct management should be considered as part of a comprehensive population health-management strategy.
Keywords: tobacco, chronic condition management, disease management, health care utilization and costs, employer health benefits
Introduction
Tobacco use is associated with substantial societal cost. Higher health care costs result from smoking-related medical conditions, including chronic obstructive lung disease, lung cancer, heart disease, impaired wound healing, and premature births, among others.1 Tobacco use has also been associated with lost productivity, the cost of which is, within the United States, comparable in magnitude to the incremental cost increase associated with tobacco-related conditions.1
Yet not all of the health care costs associated with tobacco use appear to be a direct consequence of smoking-related illness. Evidence suggests that the health care utilization patterns of smokers may differ from those of nonsmokers and may contribute to greater medical costs as a result. Specifically, although some analysis has suggested that smokers may be less likely to have a primary care physician,2 a recent study found no difference between smokers and nonsmokers in utilization of office visits.3 A similar effort evidenced no significant difference in primary care utilization between smokers and nonsmokers, but did, however, find increased specialist visit rates among smokers.4 Some of the observed findings may be due to differences in prevalence rates of medical conditions among smoking and nonsmoking subpopulations in these studies, some of which did not control for demographic and comorbid health concerns. Despite the heterogeneity of analytic methodologies, there appears to be a general consensus that smokers exhibit behavioral differences in their utilization of many types of health care services.
More specifically, these findings imply that smokers may be more reactive in their approach to care. Addressing this consideration, prior research has evaluated the impact of smoking status on use of preventive care and chronic condition management. Available data suggest that smokers are less compliant with recommended cancer screening5 and immunizations6 and have lower disease-specific medication adherence for chronic conditions.7,8 However, these earlier descriptive studies failed to incorporate depression as a potential confounder, which is particularly important given that depression is known to be more prevalent in smokers than in nonsmokers.3,9
Depressive symptoms are associated with reduced compliance with recommended self-care10,11 and medication adherence,10–12 along with increased health care costs.10,13 Little is known, however, about the confounding effect of depression on utilization of specific health care services among smokers.
For employers, the cost of workforce tobacco use is substantial. Employers may face incrementally higher expenditures associated with tobacco-related health conditions,14,15 as well as added costs associated with lost productivity,3,16 workers’ compensation,17 and disability.3,15 Additionally, employers may experience costs related to increased fire risk, maintenance of indoor air quality, and cleaning associated with smoke residue.15
In addition to a greater prevalence of tobacco-related illness and associated costs among smokers in commercially insured populations, prior studies indicate that health care utilization patterns may differ between smokers and nonsmokers. In cross-sectional studies, smokers have been shown to have higher hospitalization rates.3,4,15 Emergency department use among smokers has been variable, with studies showing both greater emergency department utilization3 and equal utilization4 compared with nonsmokers. Comparisons of outpatient physician-visit utilization by smokers and nonsmokers have also yielded mixed results.3,4,14
Accordingly, this study was designed to evaluate the impact of smoking status on preventive care and disease-specific preventive care utilization, including medication adherence, in the adult health plan enrollees of a single employer. In order to more effectively characterize the independent impact of smoking on medical treatment compliance, depression was evaluated as a confounding variable.
Methods
Study design
This is a single-year, cross-sectional analysis using a medical and pharmacy claims database created for a single, large US employer with a national smoke-free workplace policy at the time the study data were collected. The database linked medical and pharmacy utilization and costs between 2008 and 2010, as well as health risk assessment data from 2009 and 2010. The analysis was limited to a comparison of current smokers and never-smokers. Because there was no available measure of the duration since smoking cessation in this population, it was not feasible to treat the former-smoker group as a homogenous population. As a result, former smokers were excluded from analysis.
Setting
Subjects in this study were employees of a large, multinational company headquartered in the Midwestern United States. This employer has created a longitudinal, integrated database through Truven Health Analytics (Ann Arbor, MI, USA), which includes annual survey information about health and health risks (using the University of Michigan health assessment18) as well as medical, pharmacy, workers’ compensation, absence, and presenteeism data. The health risk survey comprises a series of questions regarding individual lifestyle attributes, including smoking, physical activity, nutrition, stress, and other components, to which employees and spouses respond. Individuals submitting their completed assessment then receive an individualized report, describing opportunities for lifestyle improvement. Data for all survey takers is de-identified, and then aggregated and shared with the employer, who can then use the information to develop worksite or other lifestyle behavior-improvement programs to address the most prevalent concerns. This dataset has been described previously in a comparative analysis of health and productivity costs among smokers and nonsmokers.3
Data sources
Benefit eligibility, medical and pharmaceutical claims, and survey data containing smoking status for the study population were extracted from the employer’s database. The time period for all data was January 1, 2010 to December 31, 2010. The health risk survey (from University of Michigan),18 administered to employees as a voluntary part of the benefits enrollment process during 2010, included a question about smoking status. These data were combined into a comprehensive analytic file.
Selection criteria
The study population consisted of employees and spouses/partners, aged 18 to 64 years, who were continuously enrolled in company medical coverage during 2010, and who had also completed the 2010 survey, providing a valid indication of smoking status. Employees were included in the analysis if they were actively working during the study period, were on a leave of absence, or had left employment and were directly paying for employer-provided health insurance during the study period.
Demographic variables
Demographic descriptors were available from enrollment files, employment files, and survey responses. These included age and sex, ethnicity (classified as Caucasian or other), income, and educational achievement (college degree or not). Subsequent references to demographic variables include all the aforementioned, including income and education. Missing values for race, income, and education were replaced by the mean value in the sample of employees. Depending on the analysis, imputed data was required for 2.2% to 3.6% of individuals. Because of the low numbers, no sensitivity analysis was performed.
Definition of smoking status
Smoking status was determined based on self-reported smoking status from two sources: benefit enrollment information and the annual survey. As part of the benefit enrollment process, individuals were required to declare current smoking status in order to be eligible for a nonsmoking premium discount. The health assessments were utilized to identify prior smokers who responded affirmatively to the question: “How would you describe your cigarette smoking habits?” The response options were “still smoke”, “used to smoke”, and “never smoked”. Nonsmokers were identified as those who responded negatively to both the survey question as well as the benefit enrollment smoking status question. Smokers were identified as those who responded affirmatively to either the benefit enrollment question or the health assessment question. There was a nearly 97% concordance among the individual responses recorded from the two data sources. The number of cigarettes smoked on a daily basis was not included as a variable in this analysis, as this information was not reliably available. Respondents who considered themselves prior smokers were excluded from further analysis.
Definition of chronic conditions
Asthma, hypertension, diabetes, and coronary artery disease (CAD) were selected for inclusion in this study due to sufficient prevalence rates to permit statistical analysis. Individuals with these conditions were identified in accordance with proprietary Truven Health claims review algorithms, using medical and pharmacy services claims data (International Classification of Diseases, Ninth Revision [ICD-9] and Current Procedural Terminology codes, and National Drug Code codes, respectively). Other chronic conditions were excluded from analysis due to low prevalence rates.
Individuals with depression were identified as those who received facility or professional services provided under medical coverage that were reported on a claim with a principal diagnosis of depression (indicated as an ICD-9 code of 296.2X, 296.3X, or 311.XX).
Outcomes
Health care compliance measures of cancer screening were assessed in comparison to the age and sex-specific recommendations from the US Preventive Service Task Force.19 Prescription medication adherence for individuals with the identified chronic conditions was measured as the medication possession ratio (MPR), reported as the percentage of individuals with an MPR >80% for the identified medication or medication class. The MPR is a commonly used method to estimate patient adherence with prescribed medications, and reflects the number of days of supplied medications divided by the total number of days during the study period.20
Chronic illness measures studied were extracted from the Healthcare Effectiveness Data and Information Set21 and included: depression (acute and continuation treatment rates and medication adherence), hypertension (medication adherence), and asthma (medication adherence). Because of the low number of individuals with CAD, outcome measures included the presence of recommended prescriptions. In total, 14 outcomes (four screening measures and ten medication and adherence measures) were studied. The definitions for each of these measures, derived from the Healthcare Effectiveness Data and Information Set, and implemented by Truven, are shown in Table 1.
Analyses
To estimate the independent effect of smoking status on compliance with recommended cancer screenings and MPR, several types of analyses were conducted. To adjust for population differences between smokers and nonsmokers, several covariates were included in analyses of those eligible for each compliance outcome measure. Demographic variables (shown in Table 2) included age, sex, geographic region of residence, education level (secondary school versus higher than secondary school), income (< USD50,000/year versus ≥ USD50,000/year), union membership status, ethnicity (Caucasian versus non-Caucasian), and health plan type (preferred provider organization versus high-deductible health plan). Additionally, differences in relative prevalence and severity of comorbidities were controlled using the Charlson Comorbidity Index (CCI).22 The CCI provides a statistically reliable method for quantifying the 10-year predicted mortality of 22 common chronic conditions and is used as a basis for comparison and controlling of populations with a range of chronic conditions in terms of prevalence and severity. Finally, depression was included as a covariate, in accordance with the above diagnostic approach.
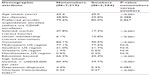  | Table 2 Population demographics for smokers and nonsmokers in the study population |
All statistical analyses were performed using Stata software (StataCorp LP, Release 12.1; College Station, TX, USA). Basic differences between groups were compared using t-tests (means) and chi-square (percentages). Logistic regression models were estimated to derive the marginal impact of each variable on screening and MPR outcomes. Regression risk analysis or method of recycled predictions23 was used to adjust the relative risks. Three sets of models were tested: one with only smoking as a predictor of outcomes; one with smoking along with demographic and CCI variables; and one with smoking, depression, and demographics along with CCI. A P-value of <0.05 was considered significant.
The relative risk of screening and adherence rates by smokers compared to nonsmokers were calculated as the percent of smokers divided by the percent of nonsmokers exhibiting the behavior. Confidence intervals and P-values were estimated using bootstrapping with 5,000 repetitions. For measures with small patient numbers (especially beta blocker with myocardial infarction), some models failed to converge, resulting in a smaller number of actual repetitions. However, none of those relative risks was significant. Confidence intervals shown were based on the percentile method and bias-corrected using Stata 12.1 (bstat command).
Results
After applying inclusion and exclusion criteria, 9,613 employees and spouses were eligible for the analyses. Of these, 2,394 were smokers (25%) and 7,219 (75%) were nonsmokers.
Population demographics of the two groups, smokers and nonsmokers, are shown in Table 2. While similar in sex distribution, benefit plan selection, and depression prevalence, smokers differed significantly from nonsmokers in other attributes. Smokers were older (45.0 years versus 43.4 years; P<0.001), and a higher percentage of smokers than nonsmokers were Caucasian (90.5% versus 84.1%; P<0.001). A lower percentage of smokers had attended college (42.4% versus 66.2%; P<0.001) or earned over USD50,000 per year (39.7% versus 60.4%; P<0.001).
Smokers had a higher prevalence of measured health conditions than nonsmokers. The CCI was significantly higher among smokers compared with nonsmokers (0.27 versus 0.22; P=0.001). Using eligibility for treatment or adherence metrics as indicators of prevalence (Table 3), smokers had significantly higher rates of treatment for depression (P<0.05), CAD (P<0.01), and previous myocardial infarction (P<0.001). Smokers and nonsmokers were similar in their rates of use of hypertension and asthma medications. Nonsmokers had significantly higher rates of treatment for diabetes (P<0.05). Due to their higher age, significantly more smokers were eligible for prostate, breast, and colorectal cancer screenings.
A small portion of the population was treated for depression (4.9%). Depression was not a significant predictor in any of the multivariate logit models predicting screening and adherence. Because depression did not contribute and results did not differ substantively from other models, only models without depression are reported.
Coefficients for logit models are shown in Table 4. Models for asthma and CAD had insufficient cases to run valid models. Controlling for demographics and CCI, smoking status (never-smokers versus current smokers) was a significant predictor of all cancer screening rates and hypertension adherence. Smoking was not a significant predictor of depression or diabetes medication adherence.
Of the covariates, age, region, salary, and plan type were significant factors in most models. Higher age groups were more likely to have recommended preventive screenings and higher medication adherence, except in the case of cervical cancer screening. Salary was positively associated with several outcomes. Living in the Midwestern US region was associated with higher rates of all outcomes, with the exception of a much lower likelihood of having prostate cancer screening. Union membership was the only demographic variable not significant in any models.
Adjusted relative risks for all outcomes are shown in Table 5. Smokers were less likely to receive recommended care and less likely to be adherent to medications in all instances. For all outcomes having 1,000 or more cases, smokers were significantly less likely to have recommended preventive care or an MPR >80%. Of those taking depression medications, smokers had a relative risk of 0.79 of being compliant (P=0.10) compared to nonsmokers. The relative likelihood that smokers had recommended cancer screenings were consistently between 0.82 and 0.85 that of nonsmokers. Other relative risks ranged from 0.72 to 0.96.
  | Table 5 Adjusted RRs for study outcomes of smokers and nonsmokers |
Discussion
In this study, current smokers were found to have significantly lower rates of compliance with recommended cancer screening as well as lower medication adherence for some of the identified chronic conditions. Importantly, the observed findings persisted despite adjustment for age, sex, ethnicity, income level, educational achievement, and comorbid conditions. Our results are consistent with prior studies4,6–8,12,24 showing lower compliance rates among smokers. Notably, although depression was more prevalent among smokers, it was not a significant factor in these results. Smokers were less compliant with all recommended screenings and medications, although results for conditions for which fewer than 500 patients were eligible for the metric were not significant. To our knowledge, this is the first study of treatment compliance among smokers that has incorporated this degree of statistical rigor.
Depression as a confounding factor
In our analysis, depression had no significant independent impact on treatment adherence, despite its established association with smoking and its direct association with reduced treatment adherence, as described earlier in this paper. The lack of confounding impact may be explained in part by the use of medical and pharmacy claims data for depression diagnosis, which may underestimate the overall prevalence rate based on self-reported depression. Prior research suggests that the prevalence of self-reported depression may be significantly greater than that derived from claims data.25 It is difficult to determine whether individuals with self-reported but untreated depression may have mild symptoms that are insufficient to cause them to access the health care system. Alternatively, it may be that, because smokers appear less likely to utilize the health care system, those with untreated depression may have more clinically significant symptoms.
Smoking status findings and potential explanations
While not specifically measured in this study, there are at least three possible explanations as to why smokers may have low compliance with recommended medical care. First, smokers may avoid regular contact with the health care system to minimize exposure to perceived pressure to stop smoking. However, in our prior analysis of this study population, no significant difference in ambulatory care clinician visit frequency was observed among smokers compared with nonsmokers, even following adjustment for demographic factors.3 Second, smokers may not want to be reminded about the development of smoking-related health complications, and avoidance of regular medical contact minimizes this possibility. However, these two scenarios appear unlikely, since smokers might then be anticipated to have comparable medication adherence to nonsmokers – a finding that was not observed in this study.
The third and perhaps most likely explanation is that, because smokers are already engaged in a known unhealthy lifestyle behavior, it may be easier for them to rationalize low compliance rates with recommended care on the basis of their at-risk lifestyle.26 In essence, smoking may provide an excuse or justification for other unhealthy practices. In a prior analysis of the same population, we found that smokers had significantly fewer primary care visits and a higher use of emergency department services.3 When considered in combination with the results from this study, the collective findings of lower rates of recommended cancer screening, lower medication adherence, and an apparently more reactive approach to health care utilization are consistent with this hypothesis.
Implication of results related to population health management
There are two important implications that can be inferred from our findings. First, these results suggest that the incremental increases in health care costs observed among smokers in some studies4,15 but not others3,27 may reflect two counteracting elements. First, tobacco-related illness may contribute to greater health care expenditure among smokers, along with a more symptom-driven approach to health care use. Offsetting these increased costs is the suboptimal compliance with recommended preventive care and medication use as observed in this study, the result of a more “reactive” use of health care services among smokers. While cross-sectional studies have not consistently demonstrated higher health care costs among smokers, it is possible that the observed suboptimal care compliance in this group may result in significantly greater associated health care costs if evaluated over time and in older populations. Accordingly, a compelling opportunity exists to better understand health care utilization and cost drivers among smokers, so as to more effectively target health management interventions to address the identified gaps in care.
Second, the health care implications resulting from poor adherence with recommended treatment are well established, and include suboptimal chronic condition management, increased hospitalization rates, and generally higher health care costs.28–31 The finding of decreased treatment compliance among smokers with chronic conditions enhances the importance of directly assessing and managing this issue in this patient population.
Smoking cessation is already recognized as a high-value preventive care service32 and, as such, is viewed as a priority in recent health care reform legislation. Health plan benefits for smoking cessation services are included among services requiring no out-of-pocket costs for non-grandfathered benefit plan enrollees, in accordance with the Patient Protection and Affordable Care Act.33 In apparent recognition of this value, the recent final rules regarding benefit incentives for wellness programs provide plan sponsors the opportunity to incorporate an incentive of up to 50% of the total annual health care cost of a single employee as an inducement for smoking cessation.34 The findings from this study provide additional support for the value of smoking cessation efforts.
Limitations
There are a number of limitations to this study. Our findings reflect the results of a single employer, and may not be generalizable to other business sectors. Importantly, this study includes only individuals (employees and their associated spouses) who were receiving commercial insurance benefits during the period of data collection and excluded individuals over the age of 65 years. It is unclear if the study findings can be generalized to other defined age, sex, and/or ethnicity subgroups.
As observed, the prevalence rates for the chronic conditions studied here are lower than might be anticipated in comparison to that seen among the general population. While these findings may be a result of a healthier workforce, it is also possible that the algorithms used to establish prevalence rates may have underestimated the total number of cases of each chronic condition.
While a conservative approach to measurement of condition prevalence rates adds credibility to the methodology, it may reduce the number of individuals identified with a condition (false negatives) or who are eligible for a specific metric. While the overall sample size was large, the small number of such individuals in specific subgroups may have limited the ability to reliably detect differences between smokers and nonsmokers.
Additionally, the identification of smoking status included in the study originated from self-reported data collected in the context of health assessment completion. Given the reduction in cost for nonsmokers, there may have been an incentive to falsely report smoking status. However, this may have been partially mitigated, since two different sources were being used to identify smokers. As such, while a majority of the workforce completed the health assessment, this population may not necessarily represent the findings from the broader employee population, thereby introducing a risk of self-selection bias into the study. Additionally, this study design does not account for elements of benefit design that may have impacted health care utilization. However, these were applied consistently across the entire workforce, and would not have been expected to selectively adversely impact either the smoker or nonsmoker population.
Further, use of MPR as a basis for establishing treatment adherence has inherent limitations. These include concerns related to changes in therapy, dose-splitting, medication sharing, and medication purchase outside the existing pharmacy benefit program, each of which may affect the measured MPR. Finally, an understanding of the primary and secondary preventive care utilization habits of former smokers would have provided additional insight into the interpretation of our findings. The inability to identify recent versus long-ago quitters made it impossible to gather reliable information about former smokers. Additional research is needed to better characterize both the nature and time course of treatment compliance changes that occur among individuals who are successful in their smoking cessation efforts.
Conclusion
Analysis of cancer screening and compliance with recommended pharmacy care among health beneficiaries of a single large employer revealed significantly lower rates of recommended care among smokers relative to nonsmokers. In addition to smoking-related illness, health care costs associated with smokers may also arise from lower rates of compliance with recommended care. Employers and other stakeholders seeking to more effectively manage population health and health care cost drivers should incorporate consideration of these research findings into their strategic planning.
Acknowledgments
Employers Health Coalition, Inc. (EHCI) received payment from Pfizer, Inc., for this research. Wendy D Lynch (Lynch Consulting, Ltd) received payment from EHCI as an independent contractor for supplemental analytics support and manuscript preparation. Bruce W Sherman (Sherman Consulting Services) received payment from EHCI as an independent contractor for study design and manuscript preparation while also serving as the EHCI medical director. Special thanks to Truven Health, Inc. for their role in providing the statistical analysis. Truven Health, Inc., received payment from EHCI as an independent contractor for performing statistical analysis related to the research.
Disclosure
Dr Sherman is currently a member of the speaker bureaus for Abbott, Merck, and Pfizer. He has recently participated in advisory board meetings on behalf of Novo Nordisk, Merck, Eisai, Genentech, Bayer, and Allergan. He serves on the scientific advisory board for Humana, and has received research funding from Sanofi and Pfizer. His recent speaking engagements with Pfizer have included unbranded presentations regarding the employer cost of smoking and value-based benefit design. Dr Lynch has received speaking honoraria from multiple pharmaceutical firms, employer coalitions, and health insurance companies in the past. She is currently receiving consulting fees from Teladoc and Eliza Corporations who may, among other services, encourage patients to quit smoking. Dr Lynch (Lynch Consulting, Ltd) received payment from EHCI as an independent contractor for supplemental analytics support and manuscript preparation. Dr Sherman (Sherman Consulting Services) received payment from EHCI as an independent contractor for study design and manuscript preparation while also serving as the EHCI medical director. This study was funded by a research grant from Pfizer for the statistical analysis (provided by Thomson Reuters/Truven) and manuscript preparation. The authors report no other conflicts of interest in this work.
References
Centers for Disease Control and Prevention (CDC). Smoking-attributable mortality, years of potential life lost, and productivity losses – United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228. | |
Hughes MC, Hannon PA, Harris JR, Patrick DL. Health behaviors of employed and insured adults in the United States, 2004–2005. Am J Health Promot. 2010;24(5):315–323. | |
Sherman BW, Lynch WD. The relationship between smoking and health care, workers’ compensation, and productivity costs for a large employer. J Occup Environ Med. 2013;55(8):879–884. | |
Bertakis K, Azari H. The influence of obesity, alcohol abuse, and smoking on utilization of health care services. Fam Med. 2006; 38(6):427–434. | |
Lemon S, Zapka J, Puleo E, Luckmann R, Chasan-Taber L. Colorectal cancer screening participation: comparisons with mammography and prostate-specific antigen screenings. Am J Public Health. 2001;91(8):1264–1272. | |
Pearson WS, Dube SR, Ford ES, Mokdad AH. Influenza and pneumococcal vaccination rates among smokers: data from the 2006 Behavioral Risk Factor Surveillance System. Prev Med. 2009;48:180–183. | |
Aggarwal B, Mosca L. Lifestyle and psychosocial risk factors predict non-adherence to medication. Ann Behav Med. 2010;40:228–233. | |
Laforest L, Denis F, Van Ganse E, et al. Correlates of adherence to respiratory drugs in COPD patients. Prim Care Respir J. 2010;19(2):148–154. | |
Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284(20):2606–2610. | |
Ciechanowski P, Katon W, Russo J. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–3285. | |
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. | |
Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–511. | |
Goetzel RZ, Anderson DR, Whitmer RW, Ozminkowski RJ, Dunn RL, Wasserman J; Health Enhancement Research Organization (HERO) Research Committee. The relationship between modifiable health risks and health care expenditures. An analysis of the multi-employer HERO health risk and cost database. J Occup Environ Med. 1998;40:843–854. | |
Centers for Disease Control and Prevention (CDC). Annual smoking-attributable mortality, years of potential life lost, and economic costs – United States, 1995–1999. MMWR Morb Mortal Wkly Rep. 2002;51(14):300–303. | |
Javitz HS, Zbikowski SM, Swan GE, Jack LM. Financial burden of tobacco use: an employer’s perspective. Clin Occup Environ Med. 2006;5(1):9–29, vii. | |
Bunn WB 3rd, Stave GM, Downs KE, Alvir JM, Dirani R. Effect of smoking status on productivity loss. J Occup Environ Med. 2006;48(10):1099–1108. | |
Musich S, Napier D, Edington DW. The association of health risks with workers’ compensation costs. J Occup Environ Med. 2001;43(6):534–541. | |
Health Risk Appraisal (HRA) [webpage on the Internet]. Ann Arbor, MI: University of Michigan Health Management Research Center; 2011 [modified November 19, 2012; cited September 23, 2012]. Available from: http://www.hmrc.umich.edu/content.aspx?pageid=19&fname=hra.txt. Accessed March 6, 2014. | |
Recommendations [webpage on the Internet]. Rockville, MD: US Preventive Services Task Force; 2010. Available from: http://www.uspreventiveservicestaskforce.org/recommendations.htm. Accessed September 14, 2013. | |
Blandford L, Dans PE, Ober JD, Wheelock C. Analyzing variations in medication compliance related to individual drug, drug class, and prescribing physician. J Manag Care Pharm. 1999;5:47–51. | |
National Committee for Quality Assurance. NQF Measures. Available from: http://www.ncqa.org/LinkClick.aspx?fileticket=p6Oa24wNQ6Y%3d&tabid=59&mid=1604&forcedownload=true. Accessed March 21, 2014. | |
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. | |
Kleinman LC, Norton EC. What’s the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009;44(1):288–302. | |
Jorm LR, Shepherd LC, Rogers KD, Blyth FM. Smoking and use of primary care services: findings from a population-based cohort study linked with administrative claims data. BMC Health Serv Res. 2012;12:263–272. | |
Collins JJ, Baase CM, Sharda CE, et al. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J Occup Environ Med. 2005;47(6):547–557. | |
Looijmans-van den Akker I, van den Heuvel PM, Verheij TJ, van Delden JJ, van Essen GA, Hak E. No intention to comply with influenza and pneumococcal vaccination: behavioural determinants among smokers and non-smokers. Prev Med. 2007;45:380–385. | |
Horwitz JR, Kelly BD, DiNardo JE. Wellness incentives in the workplace: cost savings through cost shifting to unhealthy workers. Health Aff (Millwood). 2013;32(3):468–476. | |
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. | |
Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff (Millwood). 2011;30(1):91–99. | |
National Council on Patient Information and Education. Enhancing Prescription Medication Adherence: A National Action Plan. National Council on Patient Information and Education; 2007. Available from: http://www.talkaboutrx.org/documents/enhancing_prescription_ medicine_adherence.pdf. Accessed August 28, 2013. | |
World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. Available from: http://www.who.int/entity/chp/knowledge/publications/adherence_full_report.pdf?ua=1. Accessed August 28, 2013. | |
Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31(1):52–61. | |
Title IV – prevention of chronic disease and improving public health: subtitle A – modernizing disease prevention and public health systems. In: The Patient Protection and Affordable Care Act. US Department of Health and Human Services; 2010. Available from: http://www.hhs.gov/healthcare/rights/law/title/iv-prevention-of-chronic-disease.pdf. Accessed August 28, 2013. | |
Incentives for nondiscriminatory wellness programs in group health plans. In: Federal Register. United States Federal Register, Vol 78, No 106, June 3, 2013. Available from: http://webapps.dol.gov/FederalRegister/PdfDisplay.aspx?DocId=26880. Accessed August 28, 2013. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



