Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
The Association Between Eosinophil Variability Patterns and the Efficacy of Inhaled Corticosteroids in Stable COPD Patients
Authors Yoon JK, Lee JK , Lee CH, Hwang YI , Kim H , Park D , Hwang KE, Kim SH , Jung KS, Yoo KH , Ra SW , Kim DK
Received 22 April 2020
Accepted for publication 9 July 2020
Published 31 August 2020 Volume 2020:15 Pages 2061—2070
DOI https://doi.org/10.2147/COPD.S258353
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Jung-Ki Yoon,1 Jung-Kyu Lee,2 Chang-Hoon Lee,1 Yong Il Hwang,3 Hyunkuk Kim,4 Dongil Park,5 Ki-Eun Hwang,6 Sang-Heon Kim,7 Ki-Suck Jung,3 Kwang Ha Yoo,8 Seung Won Ra,9 Deog Kyeom Kim2,10
1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul, Republic of Korea; 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Republic of Korea; 3Department of Internal Medicine, College of Medicine, Hallym University Sacred Heart Hospital, Anyang, Republic of Korea; 4Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Busan, Republic of Korea; 5Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Republic of Korea; 6Department of Internal Medicine, Wonkwang University, School of Medicine, Iksan, Republic of Korea; 7Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Republic of Korea; 8Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Republic of Korea; 9Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Republic of Korea; 10Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Republic of Korea
Correspondence: Deog Kyeom Kim
Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Republic of Korea
Tel +82-2-870-2228
Fax +82-2-831-0714
Email [email protected]
Introduction: Blood eosinophils are a predictive marker for the use of inhaled corticosteroids (ICS). However, there is concern over whether a single measure of blood eosinophils is sufficient for outlining a treatment plan. Here, we evaluated the association between variability in blood eosinophils and the effects of ICS in stable COPD cohorts.
Methods: COPD patients in the Korean COPD Subtype Study and the Seoul National University Airway Registry from 2011 to 2018 were analyzed. Based on blood eosinophils at baseline and at 1-year follow-up, the patients were classified into four groups with 250/μL as a cutoff value: consistently high (CH), consistently low (CL), variably increasing (VI), and variably decreasing (VD). We compared rates of acute exacerbations (AEs) according to ICS use in each group after calibration of severity using propensity score matching.
Results: Of 2,221 COPD patients, 618 were analyzed and a total of 125 (20%), 355 (57%), 63 (10%), and 75 (12%) patients were classified into the CH, CL, VI, and VD groups, respectively. After calibration, we found that ICS users tended to have a lower AE rate in the CH group (RR 0.41, 95% CI 0.21– 0.74) and VI group (RR 0.45, 95% CI 0.22– 0.88), but not in the CL group (RR 1.42, 95% CI 1.08– 1.89) and VD group (RR 1.71, 95% CI 1.00– 2.96).
Conclusion: More than one-fifth of patients had an inconsistent blood eosinophil level after the 1-year follow-up, and the AE-COPD rate according to ICS differed based on variability in eosinophils. Regular follow-up of blood eosinophils is required for COPD patients.
Keywords: COPD, eosinophils, inhaled corticosteroids, acute exacerbations of COPD, COPD treatment
Plain Language Summary
Recent clinical trials have shown that the blood eosinophil count predicts greater preventive effects of inhaled corticosteroids (ICS) on exacerbations of COPD. However, studies comparing blood eosinophil count at baseline and follow-up showed moderate variability in the counts. Nonetheless, no research has evaluated the correlation between eosinophil variability and the effects of ICS. Here, we merged two large Korean COPD cohorts (n=2221) and assessed the correlation between blood eosinophil variability and the response to ICS on acute exacerbations in 618 of these patients after the calibration of severity.
Twenty-two percent of COPD patients had a significant change in blood eosinophils during 1-year follow-up. Responses to ICS were markedly different between patients with higher eosinophil counts and those with lower eosinophil counts. However, ICS were also beneficial for the patients who had lower eosinophil counts at baseline but higher eosinophil counts at 1-year follow-up. Moreover, ICS were not beneficial for the patients who had higher eosinophil counts at baseline but lower eosinophil counts at 1-year follow-up. Based on our analysis, 40% of ICS users with higher eosinophil counts at baseline received ICS unnecessarily and 16% of non-ICS users with lower eosinophil counts at baseline did not receive ICS which might be beneficial.
We conclude that a single measure of blood eosinophils may not be sufficient for predicting the preventive effects of ICS on exacerbations. Considering that measurement of eosinophil counts is relatively easy, regular follow-up of the blood eosinophil count is required for COPD patients.
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogeneous disease characterized by persistent respiratory symptoms and limited airflow. Reducing the frequency of exacerbations is one of the main therapeutic goals, as acute exacerbation reduces the patient’s quality of life and accelerates the decline in lung function.1 Inhaled corticosteroids (ICS) are a key treatment option for severe COPD patients to prevent exacerbations.1,2 However, the response to ICS varies because of the heterogeneous nature of COPD, and those who do not respond to ICS may suffer from side effects, such as an increased risk for pneumonia, without experiencing benefits.3 Therefore, the need to identify an appropriate biomarker for selecting ICS has been emphasized.1
Eosinophils are involved in the immune response to hypersensitivity diseases and parasitic infection but also in tissue remodeling and the adaptive immune response.4 Airway inflammation due to eosinophil is an important pathophysiology of patients with asthma, and recent studies suggest that it also has a crucial role in COPD. As in other eosinophilic diseases, multiple post hoc analyses of randomized controlled trials for COPD have shown that higher blood eosinophil counts predict greater ICS preventive effects of ICS on exacerbations.5–9
Although new evidence has been used to update the guidelines for eosinophil counts,1,2 questions have been raised about the repeatability of blood eosinophil counts, particularly in patients with a high eosinophil count.10 There are many possible reasons for high eosinophil count other than eosinophilic COPD, such as a food or drug allergy. Moreover, peripheral blood eosinophil counts vary daily,11 leading to concerns about using a single measure of eosinophils as a predictive marker for ICS use. Recent reports12–14 show moderate variability in blood eosinophil counts ranging from 6 months to 3 years. However, no study has investigated the correlation between eosinophil variability and the effects of ICS. Here we analyzed the preventive effects of ICS on exacerbations according to variability in eosinophils in two stable COPD cohorts.
Materials and Methods
Study Participants
We enrolled COPD patients from two large COPD cohorts in South Korea. One cohort was from the Korean COPD Subtype Study (KOCOSS), the largest nationwide multi-center prospective observational cohort study in South Korea (NCT02800499).15 The Seoul National University Airway Registry (SNUAR) is another multi-center prospective observational cohort study by three university-affiliated hospitals in South Korea (NCT02527486). This cohort includes the same criteria for COPD as the KOCOSS, that is, post-bronchodilator forced expiratory volume in 1s (FEV1)/forced vital capacity <0.7 and ever smoker.
Patients with the following criteria were excluded: the follow-up period <6 months; baseline white blood cell count >12,000/μL or C-reactive protein >5 mL/dL, which might suggest a hidden infection or inflammation; and receipt of systemic steroids.
Surveys on symptoms and acute exacerbation (AE) were conducted at the time of enrollment and every 3 or 6 months. Moderate AE was defined as a patient visiting the outpatient clinic earlier than the expected date or taking antibiotics or steroids because of aggravated symptoms. Severe AE was defined as being admitted to or visiting the emergency room because of aggravated symptoms. The medications including ICS were collected at the time of enrollment based on what the physicians prescribed at each institute. All patients were classified into four groups based on serum eosinophil counts at baseline and 1-year follow-up: consistently high (CH) if both levels of eosinophils at baseline and 1-year follow-up were ≥250/μL, consistently low (CL) if both levels were <250/μL, variably increasing (VI) if the baseline eosinophil count was <250/μL and the eosinophil count of 1-year follow-up was ≥250/μL, and variably decreasing (VD) if the baseline eosinophil count was ≥250/μL and the eosinophil count at 1-year follow-up was <250/μL. In addition, the cutoff values of blood eosinophils (100, 150, 200, and 300/μL) other than 250/μL were also used and analyzed separately.
Statistical Methods
The chi-square test or Fisher’s exact test and Student’s t test or the Mann–Whitney test were used for categorical and continuous variables, respectively. We used 1:1 propensity score matching (the nearest neighbor method) with age, sex, smoking, FEV1/FVC, FEV1, the modified Medical Research Council (mMRC) dyspnea scale, and history of exacerbations for each group to create matched samples according to ICS use. A negative binominal regression model was used for the AE rate at the first-year of follow-up period. All analyses were performed with R Studio version 3.4.3.16
Results
Of the 2,385 and 448 patients registered in the KOCOSS and SNUAR cohorts, 2,221 patients had COPD and 618 patients were eligible for inclusion in the study (Figure 1). Blood eosinophil counts at baseline and 1-year follow-up were moderately correlated (intraclass correlation coefficient [ICC] = 0.55; Figure 2). To evaluate the impact of eosinophil variability on clinical outcomes, we divided the 618 patients into four groups based on their eosinophil counts at baseline and 1-year follow-up. A total of 125 (20%) patients had persistently high eosinophil counts (≥250/μL) at baseline and 1-year follow-up and were classified as the CH group, whereas 355 (57%) patients had persistently low eosinophil counts (<250/μL) and were classified as the CL group. About 22% of eligible patients showed variable blood eosinophil counts from baseline to the 1-year follow-up: 63 (10%) patients’ eosinophil counts increased (VI group), and 75 (12%) patients’ eosinophil counts decreased (VD group; Figure 2)
 |
Figure 1 Flowchart of participants. |
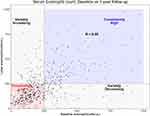 |
Figure 2 Correlation between blood eosinophil counts at baseline and 1-year follow-up. Dash line stands for 250/μL. |
High blood eosinophil counts were more variable than low counts. Of the patients with initial blood eosinophil counts ≥250/μL, 38% (75/200) had a decrease in blood eosinophil count (<250/μL) at the 1-year follow-up. By contrast, of the patients with initial blood eosinophil counts <250/μL, 15% (63/418) showed increased eosinophil counts (≥250/μL) at the 1-year follow-up.
The mean age of the patients was 68.6 years, and 97% of the patients were male. On average, each patient had a 46 pack-year smoking history, and 72% of patients were current smokers at the time of enrolment. The mean blood eosinophil count at baseline was 225/μL. About 27% of patients did not use any long-acting inhalers, whereas 40% of patients were used ICS. The mean FEV1 after bronchodilator use was 1.60 L (62%), ranging from 0.51 to 3.23 L (21–133%; Figure S1 in Supplementary Information). The incidence of moderate to severe exacerbations in the past year and during the 1-year follow-up was 23% and 29%, respectively. No differences in characteristics were detected among the four groups (Table 1).
 |
Table 1 Baseline Characteristic of Study Population Classified with Eosinophil Variability |
According to COPD guidelines, ICS are used by patients with severe COPD or if the COPD is not controlled by long-acting bronchodilators.1,2 Thus, ICS users in this study tended to have more severe COPD than nonusers (Table 2). Therefore, the severity of COPD of users and nonusers of ICS had to be calibrated to compare the preventive effects of ICS for exacerbations only. Propensity score matching with age, sex, height, smoking status, FEV1/FVC, FEV1, mMRC dyspnea scale, and a history of exacerbations was performed between ICS users and nonusers (Table 2).
 |
Table 2 Characteristics of Study Population Between ICS Users and Nonusers Before and After Propensity Score Matching |
The AE rates of patients in the CH group were significantly lower in ICS users than in nonusers Table 3 Figure 3). By contrast, the AE rate of patients in the CL group was higher in ICS users than nonusers (RR 1.42, 95% CI 1.08–1.89). It is interesting that patients in the VI group showed a similar pattern to patients in the CH group (RR 0.45, 95% CI 0.22–0.88), and patients in the VD group showed a similar pattern to patients in the CL group (RR 1.71, 95% CI 1.00–2.96). Overall, ICS users tended to have slightly more AE events than nonusers, but this difference was not significant (RR 1.09, 95% CI 0.89–1.34).
 |
Table 3 The Acute Exacerbation Rates of COPD in ICS Users and Nonusers According to Eosinophil Cutoffs |
 |
Figure 3 Eosinophil variability and the effect of ICS on acute exacerbation rate. |
Blood eosinophil changes between baseline and 1-year follow-up varied in ICS users and nonusers, but this difference was not significant (Figure 4), which suggests that eosinophil variability is not related to ICS use itself.
 |
Figure 4 Comparison of eosinophil change between ICS user and nonusers. |
Discussion
The importance of the blood eosinophil count as a predictive marker for the use of ICS in patients with COPD has been emphasized. However, variability in eosinophils has been observed, resulting in concerns over whether a single measure of eosinophils is sufficient to determine a treatment plan. Landis et al13 reported that the ICC of repeated blood eosinophil counts at 1-year follow-up was 0.64. However, Yun et al14 showed that the ICC of at 3-year follow-up in the ECLIPSE study was only 0.57. Southworth et al12 reported that the ICC at 2-year follow-up was 0.87 and emphasized that a lower eosinophil count is more stable over time than a higher one, a fact that was also reported in a population-based study.10 In this study, the ICC was at 1-year follow-up was 0.55, relatively lower than in previous studies. Given the potential factors which may affect eosinophil variability, such as a parasite infection, or food or drug allergies,4 the ICC can differ depending on geographic location or ethnicity.
Even with relatively lower ICCs in these two Korean cohorts consisting of stable patients with COPD, 78% of eligible patients were in either the CH or CL group. In addition, there were the preventive effects of ICS on exacerbations in patients with consistently high eosinophil counts (CH group) but not in patients with consistently low eosinophil counts (CL group). However, the remaining 22% of eligible patients had different eosinophil counts during the year. It is interesting that the responses to ICS also differed between the VI and VD groups. Patients in the VI group who had a low eosinophil count at baseline and a high eosinophil count after 1 year, showed the same beneficial effects of ICS as patients in the CH group. According to the epidemiological data in this study, if clinicians decide not to use ICS based on a single measure of blood eosinophil at baseline, 16% (39 of 240) of patients will delay the use of ICS. By contrast, patients in the VD group, who had a high eosinophil count at baseline but a low eosinophil count after 1 year, showed no effects of ICS. If clinicians decide to use ICS based only on blood eosinophil level at baseline, 40% (29 of 72) of patients will use ICS unnecessarily, which suggests a single eosinophil count cannot be a marker for selecting ICS in patients with COPD. Given that checking the blood eosinophil count is relatively easy, and improper use of ICS is critical for COPD patients, regular follow-up of the eosinophil count is required, although the remaining 78% (244 of 312) of patients do not need a follow-up count.
Regular follow-up of the blood eosinophil count seems to be required, in particular for patients with a high blood eosinophil count at baseline, but it is impossible to determine the optimal time interval or the number of eosinophil measurements sufficient to determine ICS use. Post hoc analyses of the IMPACT trial showed that two blood eosinophil measurements within a 2-week interval did not provide additional information to predict ICS response.17 No trial has considered the effects of ICS on long-term changes in eosinophil count. Additional study is required to optimize the follow-up period.
Using different cutoffs for blood eosinophil count changed the number of patients in each group (Table 4). A lower cutoff classified more patients in the CH group and fewer patients in the CL group. However, non-eosinophilic COPD patients with marginally high eosinophil counts would be classified into the CH group with too low of a cutoff, and the response to ICS in those patients would hamper that for eosinophilic COPD patients. For example, if the cutoff for the blood eosinophil count is set to 100/μL, ICS might not be beneficial for patients in the CH group (Figure S2 in Supplementary Information). However, if one applies too high a cutoff, such as 300/μL, eosinophilic COPD patients with marginally low eosinophil counts would be classified into the CL group, and the response to ICS would be diluted. The ideal cutoff seems to depend on the correlation between the baseline and follow-up eosinophil count; therefore, further study with more patients, a longer follow-up period, and ethical considerations are required.
 |
Table 4 Changes of Eosinophil Variability According to Eosinophil Cutoffs |
Recently, it revealed that serum eosinophil at admission can be used as prognostic factors of other clinical outcomes including readmission rate and time to first COPD-related readmission.18,19 Similar to the response to ICS in this study, eosinophil variability and measurement timing of eosinophil might affect predicting other clinical outcomes and further evaluation is required.
As systemic steroids lower blood eosinophil levels, ICS may also lower blood eosinophil levels. Kreindler et al20 reported that ICS have only limited effects on the blood eosinophil count. The change in the mean of blood eosinophil count from baseline to 1-year follow-up was slightly lower in ICS users than nonusers and was not significant (−8/μL vs −16/μL, p-value = 0.497). Given that 40% of the patients were ICS users and that there were fewer patients in the VI group than in the VD group, ICS might affect the blood eosinophil count, but the total effects would be minimal, and it may not be a challenge to determine the cutoff for the blood eosinophil count in patient with COPD.
Conclusions
ICS reduce exacerbations in patients with COPD and a consistently high eosinophil level but not the patients with a consistently low eosinophil level. One-fifth of patients showed significantly varying eosinophil counts during the 1-year follow-up, and the response to the ICS differed according to the variability in the eosinophil count. Therefore, regular follow-up of the blood eosinophil count is required for patients with COPD.
Abbreviations
AE, acute exacerbation; CH group, consistently high eosinophil group; CI, confidence interval; CL group, consistently low eosinophil group; FEV1, forced expiratory volume in one second; ICC, intraclass correlation coefficient; ICS, inhaled corticosteroid; KOCOSS, Korean COPD Subtype Study; mMRC, the modified Medical Research Council; SNUAR, Seoul National University Airway Registry; RR, relative risk; VD group, variably decreasing eosinophil group; VI group, variably increasing eosinophil group.
Ethics Approval and Informed Consent
The written informed consent was obtained from all study participants. The study was approved by the institutional review board (IRB) at each center: Seoul National University Hospital IRB, Catholic Medical Center Central IRB, Yonsei University Wonju College of Medicine IRB, Severance Hospital IRB, Soon Chun Hyang University Cheonan Hospital IRB, Ajou University Hospital IRB, Hallym University Dongtan Sacred Heart Hospital IRB, Hallym University Chuncheon Sacred Heart Hospital IRB, Hallym University Pyeongchon Sacred Heart Hospital IRB, Hanyang University Guri Hospital IRB, Konkuk University Hospital IRB, Konkuk University Chungju Hospital IRB, Hallym University Kangdong Sacred Heart Hospital IRB, Hallym University Kangnam Sacred Heart Hospital IRB, Seoul National University Boramae Medical Center IRB, Korea University Guro Hospital IRB, Korea University Anam Hospital IRB, Dongguk University Gyeongju Hospital IRB, Dong-A University Hospital IRB, Gachon University Gil Medical Center IRB, Gangnam Severance Hospital IRB, Kyung Hee University Hospital at Gangdong IRB, Kangbuk Samsung Hospital IRB, Kangwon National University Hospital IRB, Kyungpook National University Hospital IRB, Gyeongsang National University Hospital IRB, Pusan National University Hospital IRB, Soon Chun Hyang University Bucheon Hospital IRB, Seoul National University Bundang Hospital IRB, CHA Bundang Medical Center, CHA University IRB, Asan Medical Center IRB, Inje University Ilsan Paik Hospital IRB, Eulji General Hospital IRB, Samsung Medical Center IRB, Ulsan University Hospital IRB, Soon Chun Hyang University Seoul Hospital IRB, Yeungnam University Hospital IRB, Ewha Womans University Mok-dong Hospital IRB, Inha University Hospital IRB, Chonbuk National University Hospital IRB, and Jeju National University Hospital IRB.
Acknowledgments
A part of this study was presented at the poster discussion session in the European Respiratory Society International Congress 2019, Madrid, Spain.
Disclosure
All authors have no conflicts of interest to report.
References
1. Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164. doi:10.1183/13993003.00164-2019
2. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–582. doi:10.1164/rccm.201701-0218PP
3. Crim C, Calverley PM, Anderson JA, et al. Pneumonia risk in COPD patients receiving inhaled corticosteroids alone or in combination: TORCH study results. Eur Respir J. 2009;34(3):641–647. doi:10.1183/09031936.00193908
4. Kita H. Eosinophils: multifaceted biological properties and roles in health and disease. Immunol Rev. 2011;242(1):161–177. doi:10.1111/j.1600-065X.2011.01026.x
5. Bafadhel M, Peterson S, De Blas MA, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018;6(2):117–126. doi:10.1016/S2213-2600(18)30006-7
6. Pascoe S, Barnes N, Brusselle G, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med. 2019;7(9):745–756. doi:10.1016/S2213-2600(19)30190-0
7. Calverley PMA, Tetzlaff K, Vogelmeier C, et al. Eosinophilia, frequent exacerbations, and steroid response in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;196(9):1219–1221. doi:10.1164/rccm.201612-2525LE
8. Siddiqui SH, Guasconi A, Vestbo J, et al. Blood eosinophils: a biomarker of response to extrafine beclomethasone/formoterol in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;192(4):523–525. doi:10.1164/rccm.201502-0235LE
9. Cazzola M, Rogliani P, Calzetta L, Matera MG. Triple therapy versus single and dual long-acting bronchodilator therapy in COPD: a systematic review and meta-analysis. Eur Respir J. 2018;52(6):1801586. doi:10.1183/13993003.01586-2018
10. Oshagbemi OA, Burden AM, Braeken DCW, et al. Stability of blood eosinophils in patients with chronic obstructive pulmonary disease and in control subjects, and the impact of sex, age, smoking, and baseline counts. Am J Respir Crit Care Med. 2017;195(10):1402–1404. doi:10.1164/rccm.201701-0009LE
11. Spector SL, Tan RA. Is a single blood eosinophil count a reliable marker for “eosinophilic asthma?”. J Asthma. 2012;49(8):807–810. doi:10.3109/02770903.2012.713428
12. Southworth T, Beech G, Foden P, Kolsum U, Singh D. The reproducibility of COPD blood eosinophil counts. Eur Respir J. 2018;52(1):1800427. doi:10.1183/13993003.00427-2018
13. Landis SH, Suruki R, Hilton E, Compton C, Galwey NW. Stability of blood eosinophil count in patients with COPD in the UK clinical practice research datalink. Copd. 2017;14(4):382–388. doi:10.1080/15412555.2017.1313827
14. Yun JH, Lamb A, Chase R, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141(6):2037–2047 e2010. doi:10.1016/j.jaci.2018.04.010
15. Lee JY, Chon GR, Rhee CK, et al. Characteristics of patients with chronic obstructive pulmonary disease at the first visit to a pulmonary medical center in Korea: the Korea COPD subgroup study team cohort. J Korean Med Sci. 2016;31(4):553–560. doi:10.3346/jkms.2016.31.4.553
16. R: A Language and Environment for Statistical Computing [Computer Program]. Version 3.4.3. Vienna, Austria: R Foundation for Statistical Computing; 2017.
17. Bafadhel M, Barnes N, Bourke S, et al. Analysis of IMPACT: is one blood eosinophil count measurement sufficient to predict ICS treatment response in COPD?
18. Belanger M, Couillard S, Courteau J, et al. Eosinophil counts in first COPD hospitalizations: a comparison of health service utilization. Int J Chron Obstruct Pulmon Dis. 2018;13:3045–3054. doi:10.2147/COPD.S170743
19. Li Q, Larivee P, Courteau J, et al. Greater eosinophil counts at first COPD hospitalization are associated with more readmissions and fewer deaths. Int J Chron Obstruct Pulmon Dis. 2019;14:331–341. doi:10.2147/COPD.S187375
20. Kreindler JL, Watkins ML, Lettis S, Tal-Singer R, Locantore N. Effect of inhaled corticosteroids on blood eosinophil count in steroid-naive patients with COPD. BMJ Open Respir Res. 2016;3(1):e000151. doi:10.1136/bmjresp-2016-000151
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
