Back to Journals » Patient Preference and Adherence » Volume 14
The Association Among Medication Beliefs, Perception of Illness and Medication Adherence in Ischemic Stroke Patients: A Cross-Sectional Study in China
Authors Ruksakulpiwat S , Liu Z, Yue S, Fan Y
Received 18 October 2019
Accepted for publication 21 December 2019
Published 13 February 2020 Volume 2020:14 Pages 235—247
DOI https://doi.org/10.2147/PPA.S235107
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Video abstract presented by Suebsarn Ruksakulpiwat.
Views: 808
Suebsarn Ruksakulpiwat,1,2 Zhaojun Liu,1 Shihong Yue,1 Yuying Fan1,2
1The Second Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang Province, People’s Republic of China; 2College of Nursing, Harbin Medical University, Harbin, Heilongjiang Province, People’s Republic of China
Correspondence: Yuying Fan
The Second Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang Province, People’s Republic of China; College of Nursing, Harbin Medical University, 157 Baojian Road, Nangang Distinct, Harbin 150086, Heilongjiang Province, People’s Republic of China
Tel +86 13603630368
Email [email protected]
Purpose: To examine the association and the mediating effect among medication beliefs, perception of illness, and medication adherence in ischemic stroke patients.
Patients and Methods: This is a cross-sectional study, 306 ischemic stroke patients recruited from The Second Affiliated Hospital of Harbin Medical University, China between June 2018 and October 2018. The Beliefs about Medications Questionnaire (BMQ) was used to assess a patient’s beliefs about medication. The Brief Illness Perceptions Questionnaire (BIPQ) was used to rapidly determine the cognitive and emotional representation of ischemic stroke. Self-reported adherence was assessed using the Medication Adherence Report Scale (MARS). Logistic regression analysis, Pearson correlations, and mediation analysis were used to evaluate the association and mediating effects among medication beliefs, perception of illness, and medication adherence.
Results: Overall, 220 (65.48%) participants were non-adherent to their ischemic stroke medications. Non-adherent patients had greater stroke severity (p = 0.031) compared to adherent patients. After adjusting for demographic characteristics, specific concern (odds ratio [OR]: 0.652, 95% confidence interval [CI]: 0.431 to 0.987, p-value [P] = 0.043), and the perception of illness (overall score) (OR: 0.964, 95% CI: 0.944 to 0.985, P = 0.001) were significantly associated with medication adherence in ischemic stroke patients. The mediation analysis showed the significant indirect effects of specific concern, general overuse, and general harm. It suggested that some impacts of medication beliefs have been mediated on medication adherence.
Conclusion: Perceived concern about adverse effects of medicines and perception of illness have an influential impact on self-reported medication adherence in ischemic stroke patients. To enhance adherence, patients’ beliefs about medication and perceptions of their disease should be reconsidered. Future work should investigate interventions to influence patient adherence by addressing concerns about their ischemic stroke medications and the perception of the disease.
Keywords: ischemic stroke patients, medication beliefs, perception of illness, medication adherence
Introduction
Strokes are a leading cause of mortality and disability worldwide. In 2016, the global prevalence of strokes was 80.1 million cases, with 5.5 million deaths from strokes, and 13.7 million people experiencing a first stroke, resulting in 116.4 million Disability-Adjusted Life Years lost due to stroke, showing a trending increase in strokes.1
China, the world’s largest population, has 1.4 billion people. Every year, China sees 2.5 million new stroke patients. The annual stroke mortality rate is 1.6 million, approximately 157 per 100,000, surpassing heart disease to become the leading cause of death and disability. Strokes cause almost 116 deaths per 100,000 people living in metropolises and 111 deaths per 100,000 people living in rural areas.2,3 Northeast China has the highest incidence (486 per 100,000), whereas in southern China, the incidence is significantly lower (136 per 100,000).4 Heilongjiang province, which is in the northeast of China, has the highest incident rate. It is six times higher than Guangxi province in the south of China, with a mortality rate nine times higher. In Harbin, the capital city of Heilongjiang, the incidence and mortality of stroke were the highest among 12 cities and 22 rural areas in 21 provinces, with a prevalence secondary to Beijing.5
Patients with a history of stroke have a 30% to 43% risk of recurrence within five years.6 The mortality rate in the first stage of stroke recurrence is 56.2%. Therefore, the prevention of recurrence is essential to reducing the severity and mortality of this disease.7 In China, details on stroke recurrence prevention strategies are scarce. More studies are needed to examine the effectiveness of all stroke recurrence prevention efforts at the national level.4
Currently, taking medication regularly is a way to prevent the recurrence of strokes. However, stroke patients do not typically maintain regular medicine habits. Many factors contribute to regular medicine habits, such as financial constraint, family support, several doses, knowledge about the medicine, perception of illness, and medication beliefs.8–10
Medication beliefs and the perception of illness are a direct consequence of the patient’s intention and decisions regarding medicine intake, resulting in consistent consumption behavior. The common-sense model of self-regulation reveals that an adaptive response to illness depends on the belief or perception of the sickness of the person.11 In addition to the perception of illness, medication beliefs are essential factors affecting the patient’s decision about the medicine.12 Research on the perception of illness in hypertensive patients also found that patients who aware of their disease being chronic are more likely to take medication to control or prevent more severe illness.13
In China, patient perceptions of injustice correlated to the costs of care and conflicts of interest, inadequate physician practice, and health systems factors contributed to the patient-physician mistrust, the trust between healthcare providers and patients has been diminished, various patients suspected their personal need and questioned the necessity of their treatment, which is associated with non-adherence.14,15 Moreover, they may not consult their health care providers about the treatment they receive. It is possible that this may cause uncertainty about the prescribed medicine, the perceived illness, and medication adherence.15
This study aims to investigate the association and the mediating effect among medication beliefs, perception of illness, and medication adherence in ischemic stroke patients.
Materials and Methods
Design, Settings, and Sample
In this cross-sectional study, questionnaire data have been merged with clinical data from The Second Affiliated Hospital of Harbin Medical University, Harbin, China. The questionnaire consisted of multiple-choice, single-item scale, and Likert scale questions designed to assess patient’s demographic data, the cognitive and emotional representation of ischemic stroke, patient beliefs about ischemic stroke medication, and medication adherence. Participants were invited to take part in the study by the healthcare professionals, according to inclusion criteria, upon hospital admission during the study period.
A recent meta-analysis showed a small-to-moderate effect resulting from psychological beliefs on adherence to medicine across 94 studies, with a total sample size of 25,072 and an average sample size of 266.15,16 Therefore, the sample size for the current study was set at no smaller than 300. The inclusion criteria specified patients who had a clinical diagnosis of ischemic stroke from a healthcare professional (according to The American ICD-10-CM version, diagnosis code ICD-10:I63.902), who were on any ischemic stroke preventative medication and who provided informed consent. Exclusion criteria specified patients who had concurrent diagnoses of any condition profoundly affecting cognition (e.g., schizophrenia, dementia), who could not complete the questionnaire, and/or who had declined to participate.
Patient Involvement
We acknowledged that patients in the hospital – and especially those in the stroke unit – were likely to be elderly and/or have multiple physical constraints. Therefore, before the study started, 30 people (including healthcare providers and patients) were asked to complete the questionnaire. This was done in order to assess whether Chinese patients would easily understand the Chinese versions of the questionnaires; this arrangement was also made to provide help, as healthcare professions could instruct respondents on how to complete the questionnaire and/or explain the meaning of an item when difficulty arose.15 After this process, we found that the comments were entirely positive. Only a few words needed to improve; for example, in The Brief Illness Perception Questionnaire (BIPQ) question 1, instead of using “How much does your illness affect your life?”, patients more readily understand the intent of the inquiry when we replaced “illness” with “ischemic stroke”.
Measurements
Personal Information Inquiries and Health Records
Demographic information included admission date, hospital number, age, gender (as “Men” or “Woman”), score on the Chinese version of The National Institute of Health Stroke Scale (NIHSS),17 education (as “Literacy”, “Primary school”, “Middle school”, “High school or college” or “University or above”), occupation (as “Farmer”, “Worker”, “Housewife or unemployment”, “Retirement”, “Healthcare professional”, “Civil service”, or “Teacher”), duration of disease (whether patients have has ischemic stroke “less than 1 year”, “1–5 years” or “more than 5 years”), and payment methods (whether patients use “Self-supporting commercial”, “A new rural cooperative medical system”, “Urban medical insurance” or “Commercial medical insurance”).
Brief Illness Perceptions Questionnaire (BIPQ)
The BIPQ is a nine-item questionnaire designed to quickly evaluate the cognitive and emotional representation of an illness.18 It uses a single-item scale approach to assess perceptions on a 0–10 response scale. For example, question 1 (How much does your ischemic stroke affect your life?), a score of 0 = “no affect at all”, whereas a score of 10 = “severely affects my life”. The overall score was calculated as the sum of reversed scores of question 3 (How much control do you feel you have over your ischemic stroke symptoms?), question 4 (How much do you think your treatment can prevent your ischemic stroke?), and question 8 (How much do you think you know about ischemic stroke?) and the score of questions 1,2,5,6, and 7. Therefore, a higher overall BIPQ score indicates that the patient views the illness as more dangerous.19 The BIPQ includes five items for cognitive representation of illness perception: consequences, timeline, personal control, treatment control, and identity, two items on emotional representation: concern and emotions, and one item on illness comprehensibility: perceived cause of illness. According to existing literature,20 the question on illness comprehensibility involves qualitative analysis, therefore, it was not used in our study. For this questionnaire, the general word “illness” was replaced by the name of a particular illness: “ischemic stroke.” The BIPQ has been tested in several illness groups and shows reliability and validity. Good test-retest reliability (Pearson correlations 0.24–0.73) has also been demonstrated.21 The Chinese BIPQ has acceptable intercorrelation and test-retest reliability, with a Cronbach’s alpha of 0.538 to 0.757.22
Beliefs About Medications Questionnaire (BMQ)
The BMQ was designed to assess cognitive representation regarding medication in four dimensions: specific necessity, specific concerns, general overuse, and general harm.23,24 All 18 questions were scored on a 5-point Likert scale (1=strongly disagree, 2=disagree, 3=uncertain, 4=agree, 5=strongly agree). The mean for the item score was then calculated as the sum of each item score divided by the number of items. For example, the mean score for specific necessity = (N1+N2+N3+N4+N5)/5, and the mean score for general harm = (N1+N2+N3+N4)/4). Subscales were excluded for individuals with one or more answers missing from the total score of the corresponding BMQ.15,20 Validity and reliability have been confirmed by previous studies.24 For the Chinese version, the Cronbach’s α coefficients of the necessity dimension and concerns dimension were 0.813 and 0.706, respectively, and the test-retest reliability coefficients were 0.743 and 0.786, respectively.25
The Medication Adherence Self Report Scale (MARS)
We used the five-item version of the MARS to evaluate adherence to ischemic stroke medication.26 The MARS consists of five general statements about non-adherent behavior on a 5-point Likert scale (1=always, 2=often, 3=sometimes, 4=rarely, 5=never). The MARS is internally reliable (Cronbach’s alpha across four studies, 0.68 to 0.86), with exceptional test-retest reliability (r=0.97).27 The Chinese version of MARS demonstrated good internal consistency (Cronbach’s α coefficient was 0.87), content validity (content validity index was 1.00), and criterion-related validity (r=0.77, P=0.01).28 The consequence variable was calculated as the total score on the MARS-5. Previous studies performed sensitivity analyses using MARS scores 20 or 21 as the cut-off for non-adherence.20 Therefore, in our study, we used MARS scores of 20 as the cut-off point (scores < 20 define as non-adherence).
Data Collection
Patients who had a clinical diagnosis of ischemic stroke who were able to answer questions were invited by the healthcare professionals to take part in the study when they were admitted to the hospital during the study period. When patients had comorbidity, they were only included for the condition for which they were hospitalized.15 After information was provided verbal consent obtained, participants were asked to complete a questionnaire that took approximately 15 to 20 mins.
Data Analysis
Differences existed in the baseline characteristics as well as in the medication beliefs and perception of illness between adherent and non-adherent patients. We assessed these using chi-square and t-tests as appropriate.
The corresponding effect size used to describe the size of the difference in mean values between adherence and non-adherence relative to the standard deviation was calculated using Cohen’s d, which was computed as the difference between two mean values divided by the pooled standard deviation as follows: effect size =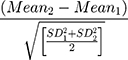 , where
, where
SD1 is the standard deviation of group 1 (non-adherence) and SD2 is the standard deviation of group 2 (adherence). The literature showed that cutoffs and percent overlap between the groups for small, medium, and large effect size, at 0.20 (85%), 0.50 (67%) and 0.80 (53%), respectively.29
The adjusted characteristic of ischemic stroke patients according to medication adherence and the adjusted association between medication beliefs and the perception of illness with medication adherence were assessed using a logistic regression analysis. The first model included medication beliefs. The second model encompassed the perception of illness (overall score) and demographic information. For the final model, we combined medication belief, each of the domains of the perception of illness, and demographic information. Pearson correlations were used to examine the relationships between BMQ, BIPQ, and MARS.
For mediation analysis, we used the “PROCESS” Procedure for the Statistics Package for the Social Sciences (SPSS) Version 3.3, written by Andrew F. Hayes.30 In evaluation of the significance of indirect effects, we applied 5000 bootstraps to estimate 95% Cl. As in previous studies, in order to avoid a collinearity problem that could diminish the indirect effects, we separately analyzed the indirect effect of medication belief mediators in the association between the perception of illness and medication adherence.31 We adopted the strategy proposed by Preacher and Hayes to evaluate our pathway and followed four necessary steps to assess mediation.32,33 Step 1: association between the perception of illness and medication adherence (Path c=X →Y; total effect); step 2: association between the perception of illness and medication belief mediators (Path a=X → M); step 3: association between medication belief mediators and medication adherence (Path b=M → Y); and step 4: association between the perception of illness and medication adherence after controlling for medication belief mediators (Path c’=direct effect). The mediation analyses were controlled for all characteristics of ischemic stroke patients. Statistical analyses were performed using IBM SPSS Statistics V. 20.0.
Results
Participants
Between June 2018 and October 2018, there were 336 ischemic stroke patients in the study. Of those patients, 30 (8.9%) missed the questionnaire completely (three patients with incomplete BMQ, four patients with unfinished BIPQ, three patients with inadequate MARS, and 20 with missing clinical data), resulting in an ultimate analytical sample size of 306 (91.1%).
Table 1 shows the characteristics of ischemic stroke patients using MARS. The mean age of patients was 63.47±10.20 years. 57.8% were men, while 36.3% had a middle school education. 34%, 35%, and 25.8% had been diagnosed with ischemic stroke for less than one year, one to five years, and more than five years respectively; most of the respondents were workers (29.4%) making use of urban medical insurance (48.7%). Overall, 220 (65.48%) participants were non-adherent to their ischemic stroke medications. Non-adherent patients had greater severity of a stroke (P = 0.031) compared to adherent patients (NIHSS scores ≤ 4: mild impairment, NIHSS scores 5–14: mild to moderate impairment).34 Adherent and non-adherent participants did not vary in terms of age, gender, education, occupation, duration of disease, or payment methods (P > 0.05 for all evaluations).
 |
Table 1 Characteristics of Ischemic Stroke Patients |
Unadjusted Comparison of Perception of Illness and Medication Beliefs According to Medication Adherence
Table 2 contains the replies to the BIPQ and the BMQ. In the responses to the BIPQ, non-adherent patients stated that strokes had a greater effect on their lives (P = 0.000; Cohen’s d = 0.62), believed that the illness would continue for a longer time (P = 0.001; Cohen’s d = 0.41), and had experienced more stroke symptoms (P = 0.000; Cohen’s d = 0.60), moreover, non-adherent participants reported being more concerned about strokes (P = 0.002; Cohen’s d = 0.38), and also more emotionally affected by the ailment (P = 0.000; Cohen’s d = 0.48). However, there was no significant difference between adherent and non-adherent patients in the score distribution of items measuring patient personal control (P = 0.218; Cohen’s d = 0.16), treatment control (P = 0.863; Cohen’s d = 0.02), and patient comprehensibility (P = 0.719; Cohen’s d = 0.05).
 |
Table 2 An Unadjusted Comparison of the Perception of Illness and Medication Beliefs According to Medication Adherence |
In the responses to the BMQ, non-adherent patients expressed more concern about the harmful effects of their use of medicines (P = 0.000; Cohen’s d = 0.64). Likewise, they had more perceived notions that doctors overuse or put too much trust in medicines (P = 0.000; Cohen’s d = 0.51) and that stroke medicine could negatively affect their lives (P = 0.000; Cohen’s d = 0.45). Alternatively, there were no significant differences between adherent and non-adherent patients the Specific Necessity dimension (P = 0.344; Cohen’s d = 0.12).
Adjusted Comparison of Perception of Illness and Medication Beliefs According to Medication Adherence
The results of the multivariate analysis showed that variables contributing to medication adherence included education (equal to the university level or above) (odds ratio [OR]: 4.589, 95% confidence interval [CI]: 1.062–19.823, p-value [P] = 0.041) and the duration of disease (more than five years) (OR: 2.355, 95% CI: 1.131–4.903, P = 0.022) (supplementary data 1).
In Table 3, we evaluated the association of four dimensions of medication beliefs with medication adherence, adjusted the comparison of the perception of illness (overall score) and demographic factors according to medication adherence. Then we consecutively adjusted for the first model and eight domains of the perception of illness with demographic factors.
 |
Table 3 Adjusted Comparison of Perception of Illness and Medication Beliefs According to Medication Adherence |
Model 1 measured the association of four dimensions of medication beliefs (evaluated by BMQ) with medication adherence alone. Adherent participants diagnosed with ischemic stroke reported significantly lower scores regarding positive statements about their medicines-specific concern (OR: 0.574, 95% CI: 0.405 to 0.813, P = 0.002). That is, when the patient has a significant concern about the harmful effects of the use of their medicines, they are more likely to report non-adherence.
In their responses on the perception of illness (Model 2) as evaluated by BIPQ, the perception of ischemic stroke was significantly associated with medication adherence (OR: 0.964, 95% CI: 0.944 to 0.985, P = 0.001). This means that when the patient has greater negative perceptions about the disease, it was significantly associated with non-adherence.
Our final model (Model 3), which included medication beliefs, each of the domains of the perception of illness, and characteristics of ischemic stroke patients, showed an insignificant influence on the associations observed in Model 1. The results for specific concerns slightly changed the statistical significance (OR: 0.652, 95% CI: 0.431 to 0.987, P = 0.043). However, the results regarding each of the domains of the perception of illness have lost statistical significance (P > 0.05 for all evaluations).
The Pearson Correlation Between BMQ, BIPQ, and MARS
The correlation between BMQ, BIPQ and MARS is shown in Table 4. Specific necessity was significantly related to specific concern (r = 0.147, P < 0.05, n = 306) and general overuse (r = 0.188, P < 0.01, n = 306). There was also a significant association between specific concern and general overuse, general harm, BIPQ, and MARS (r = 0.438, 0.382, 0.305 and −0.317, respectively, P < 0.01, n = 306). General overuse was also correlated with general harm, BIPQ, and MARS (r = 0.492, 0.215 and −0.404, respectively, P < 0.01, n = 306). Likewise, general harm was significantly related to BIPQ and MARS (r = 0.174 and −0.368, P < 0.01, n = 306). Overall, the Pearson correlation coefficient was −0.278 (P < 0.01) for BIPQ and MARS. These results indicate that as MARS decreased, specific concern, general overuse, general harm and BIPQ increased, and specific necessity did not.
 |
Table 4 Correlation Matrix for the Different Scales Used to Test BMQ, BIPQ, and MARS. Pearson Correlation Coefficient (p-value) |
Testing the Mediation Role of Medication Belief Mediators
The results of the mediation analyses are shown in Table 5. The significant indirect effects of specific concern (M2) (a*b = −0.027, 95% Cl: −0.044 to −0.014), general overuse (M3) (a*b = −0.026, 95% Cl: −0.044 to −0.011), and general harm (M4) (a*b = −0.017, 95% Cl: −0.034 to −0.003) suggest that some of the impact of medication belief on medication adherence is mediated through these pathways [Figure 1]. To clarify, for the specific concern (M2) path, for every unit of increase in the perception of illness, M2 increases by 0.019 (P < 0.001) units and, for every unit increase in M2, medication adherence decreases by 1.418 (P < 0.001) units. Finally, every unit of increase in the perception of illness indirectly causes 0.027 (95% Cl: −0.044 to −0.014) units decrease in medication adherence. For the general overuse (M3) path, for every unit of increase in the perception of illness, M3 increases by 0.014 (P < 0.001) units, and for every unit increase in M3, medication adherence decreases by 1.957 (P < 0.001) units. Finally, every unit of increase in the perception of illness indirectly causes 0.026 (95% Cl: −0.044 to −0.011) units decrease in medication adherence. For the general harm (M4) path, for every unit of increase in the perception of illness, M4 increases by 0.009 (P < 0.05) units, and for every unit of increase in M4, medication adherence decreases by 1.841 (P < 0.001) units. Every unit of increase in the perception of illness indirectly causes 0.017 (95% Cl: −0.034 to −0.003) units decrease in medication adherence. Among the overall participants, the significant total effect (c) of the perception of illness on medication adherence was −0.086 (SE = 0.021, P = 0.000).
 |
Table 5 The Effect of Medication Belief Mediators (M) in the Association Between the Perception of Illness (X) and Medication Adherence (Y) |
Discussion
In this cross-sectional study, we discovered that more severe ischemic stroke was a significant association with poor adherence. Moreover, we found that medication beliefs impact medication adherence and are mediated by factors such as patient concerns about the medication, and the belief that doctors overuse medications. The information in this study can help design clinical practice interventions to prevent instances of non-adherence.
Further studies are needed because medication adherence is a tremendously important factor in decreasing mortality, morbidity, and medical costs in chronic diseases.35 Many healthcare providers have become increasingly conscious of medication adherence research.36 A qualitative study of 180 stroke patients revealed that adherent patients reported remembering to take medicines and looking for support both from parents and health professionals. Furthermore, they understand the consequence of non-adherence and believe their medicines provide more help than harm.37 Moreover, a predictive study of ischemic stroke patients showed that medication beliefs could best predict medication adherence (b = 0.415, P < 0.05), followed by illness perception (b = −0.293, P < 0.05).38 A longitudinal study of 180 stroke survivors found that younger patients who had increased specific concern about medications, reduced cognitive functioning, and low perceived benefit of medication reported poor adherence.39 Our research on a majority of elderly subjects with ischemic stroke found that concern about medications and illness perception were important predictors of non-adherence.
Over 65% of our study participants were classified as non-adherent. This was consistent with the medication adherence study in 535 participants over the age of 40 years who had at least one stroke or transient ischemic stroke (TIA) in the previous five years. The result showed that a great proportion of participants (67%) with likely Posttraumatic Stress Disorder (PTSD) were nonadherent to medications.40 Moreover, our research was also consistent with the medication adherence research in chronic obstructive pulmonary disease (COPD) patients in the United States, which found that almost 60% of participants were non-adherent to their COPD regimen, highlighting the extent of this problem across a diverse setting.41 The significance of our study is emphasized by the fact that the majority of our participants had high stroke severity [Table 1]. Therefore, adequate exposure to the healthcare providers and an opportunity to learn and practice appropriate self-management behaviors should be provided for the patients.41,42
The adjusted results showed that specific concern and the perception of illness (overall score)—that is, when the patient has a more significant concern about the harmful effects of their use of medicines and greater negative perceptions about the disease—were significantly associated with non-adherence. Our finding was consistent with a recent study that showed that adherent stroke, diabetes mellitus, rheumatoid arthritis, and chronic obstructive pulmonary disease patients had significantly fewer concerns about medicines.15,20,41 Moreover, a predictive study found that increased specific concerns about medication can predict poor adherence.39 A study in hypertensive patients revealed that general harm and general overuse of medicines were not significantly correlated with adherence or prediction for a large group of medication adherent patients.43 Likewise, general overuse and general harm were not associated with medication adherence in our research. It can be interpreted that usually, in Chinese society, if there is a minor ailment, a patient will use general medicines that can be purchased without having to travel to the hospital for treatment. However, with these convenient access channels, all patients can simply buy prescriptions for themselves beyond the necessity, such as Traditional Chinese Medicine (TCM) which can create the belief that they are not worried about taking prescribed medicine.44,45 The perception of ischemic stroke (overall score) was significantly associated with medication adherence in our results, which consistent with the predictive study in Thailand that showed that illness perceptions were significantly associated with and could predict medication adherence.38
The study of key barriers to medication adherence in survivors of strokes and transient ischemic attacks revealed that the low perceived need for medications (the necessity of medicine) was not associated with medication adherence (OR: 1.230, 95% CI: 0.790 to 1.910, P = 0.36).46 Likewise, the perception of the necessity of medicine (specific necessity) was not associated with medication adherence in our analysis (OR: 0.848, 95% CI: 0.575 to 1.250, P = 0.405) [Model 3 in Table 3]. Therefore, it may be appropriate to study belief about the necessity of ischemic stroke medications in China. The previous study revealed that numerous Chinese patients questioned the necessity of the individual treatment they received.15 Notably, older and chronic patients are skeptical of western doctors,44 making them averse to compliance with western medicine (including ischemic stroke medications). Compared to western treatment, Chinese people believe Traditional Chinese Medicine (TCM) to have more benefits in terms of lower side effects, more options, psychological comfort, and an increase in the quality of the relationship between patients and healthcare providers.45 Thus, the point estimate about the necessity of the individual prescription among Chinese people could be due to opportunity, and further studies are needed to explore this finding further.
In the correlation analysis, Table 4 shows that specific necessity was not significantly correlated with general harm in our research. This was supported by a cross-sectional study in China.15 Pearson correlation coefficients between specific necessity and general harm in stroke, diabetes mellitus, and rheumatoid arthritis patients were not significantly associated. Moreover, our results also found that the MARS score for ischemic stroke patients was negatively associated with a specific concern. This result is also supported by a cross-sectional survey of 485 chronically ill patients (hypertension, musculoskeletal disease, diabetes type 2 and cardiac insufficiency), which found that MARS scores were negatively correlated with BMQ-concerns. Thus, chronically ill patients with fewer concerns about the side effects of their medicine tended to be more adherent.47 In our study, the total MARS scores were significantly correlated with the perception of ischemic stroke (BIPQ overall score). However, according to previous research, the full MARS scores were generally not significantly associated with the BIPQ scores.48
While bivariate relationships between medication beliefs, perception of illness, and medication adherence have been identified, the multifaceted relationship among them has not been explained. Another important finding in our study is that medication belief mediates the perception of ischemic stroke and medication adherence. The assessment of a mediating effect could help understand how the perception of illness affects medication adherence through medication belief. Patients are likely to develop non-adherence if they have a higher disease congruence and more extensive disease symptoms, worry about stroke medications, believe that doctors overuse or put too much trust in their medicines, and accept that stroke medications are harmful. This was consistent with a cross-sectional survey of chronic disease patients (asthma, hypertension, diabetes, hyperlipidemia, osteoporosis, depression) which found that in the mediation analysis, the effect of medication beliefs (perceived need, concerns, and affordability) on intentional non-adherence is mediated through unintentional non-adherence.49
Moreover, our findings were also supported by a mediating role study of type 2 diabetes patients that found that depressive symptoms affected diabetes medication adherence through perceived side effect barriers, perceived general barriers, and self-efficacy.50 Furthermore, research on asthma patients revealed that medication beliefs mediated the association between minority status and asthma medication adherence.51 Therefore, in our study, the promotion of the perception of disease and belief in medicine is vigorous in preventing non-adherence.
We acknowledge that in our research, patients with hemorrhagic stroke were not admitted into the ward in which our study was conducted due to the associated surgical procedures. Hence, our sample may under-represent those patients. Furthermore, as an observational study, we were not able to evaluate the causal relationship between variables, and our results may be confounded by unmeasured factors such as comorbidity, medication history and socioeconomic factors which may cause estimation bias. Therefore, to reduce this bias due to unobservable information, using an instrumental variable is needed in further studies.52
However, this was a specific psychological study conducted in China. We chose a large teaching hospital and collected data continues until the target quantities were reached. Furthermore, we believe that our study makes a significant contribution to the literature because, although the prevalence of ischemic stroke is on the rise and medication adherence is a strong means of preventing future strokes, studies on medication adherence in ischemic stroke patients are few in China. Further studies using longitudinal design with a better, randomized sample from different provinces of China are recommended to develop the generalizability of these findings and analyze medication adherence over time. Finally, our results justify developing interventions to improve medication adherence among stroke patients.
Conclusion
This research expands recognized literature on the perception of illness, medication beliefs, and medication adherence in ischemic stroke patients. Therefore, our findings have clear implications that healthcare providers should modify expectations and perceptions that stand in the way of effective stroke self-management. Additionally, we used the STROBE checklist in reports of this cross-sectional study (supplementary data 2).
Ethics Approval
The Second Affiliated Hospital of Harbin Medical University (approval number: KY2017-026) approved this study.
Patient Consent
Study information was given to patients, and verbal informed consent was acceptable and approved by the Second Affiliated Hospital of Harbin Medical University.
Acknowledgment
This study could not have been completed without the cooperation of healthcare providers in the Second Affiliated Hospital of Harbin Medical University.
Author Contributions
Suebsarn Ruksakulpiwat and Yuying Fan designed and conceived the whole study. Zhaojun Liu and Shihong Yue performed the survey. Suebsarn Ruksakulpiwat and Zhaojun Liu equally contributed to this work. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Johnson CO, Nguyen M, Roth GA, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):439–458. doi:10.1016/S1474-4422(19)30034-1
2. Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009;8(4):345–354. doi:10.1016/S1474-4422(09)70023-7
3. Chen Z. The mortality and death cause of national sample areas. Third National Surv Cause Death. 2008;1:14–15.
4. Liu L, Wang D, Wong KL, Wang Y. Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke. 2011;42(12):3651–3654. doi:10.1161/STROKEAHA.111.635755
5. Sun H, Zou X, Liu L. Epidemiological factors of stroke: a survey of the current status in China. J Stroke. 2013;15(2):109. doi:10.5853/jos.2013.15.2.109
6. Feng W, Hendry RM, Adams RJ. Risk of recurrent stroke, myocardial infarction, or death in hospitalized stroke patients. Neurology. 2010;74(7):588–593. doi:10.1212/WNL.0b013e3181cff776
7. Coull A, Lovett J, Rothwell P. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ. 2004;328(7435):326. doi:10.1136/bmj.37991.635266.44
8. Glader E-L, Sjölander M, Eriksson M, Lundberg M. Persistent use of secondary preventive drugs declines rapidly during the first 2 years after stroke. Stroke. 2010;41(2):397–401. doi:10.1161/STROKEAHA.109.566950
9. Bushnell C, Olson D, Zhao X, et al. Secondary preventive medication persistence and adherence 1 year after stroke. Neurology. 2011;77(12):1182–1190. doi:10.1212/WNL.0b013e31822f0423
10. Kucukarslan SN. A review of published studies of patients’ illness perceptions and medication adherence: lessons learned and future directions. Res Social Adm Pharm. 2012;8(5):371–382. doi:10.1016/j.sapharm.2011.09.002
11. Leventhal H, Diefenbach M, Leventhal EA. Illness cognition: using common sense to understand treatment adherence and affect cognition interactions. Cognit Ther Res. 1992;16(2):143–163. doi:10.1007/BF01173486
12. Furze G. Cardiac misconceptions: a problem in need of treatment. Pract Cardiovasc Risk Manag. 2007;5:13–15.
13. Chen S-L, Tsai J-C, Chou K-R. Illness perceptions and adherence to therapeutic regimens among patients with hypertension: a structural modeling approach. Int J Nurs Stud. 2011;48(2):235–245. doi:10.1016/j.ijnurstu.2010.07.005
14. Tucker JD, Cheng Y, Wong B, et al. Patient–physician mistrust and violence against physicians in Guangdong Province, China: a qualitative study. BMJ Open. 2015;5(10):e008221. doi:10.1136/bmjopen-2015-008221
15. Wei L, Champman S, Li X, et al. Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: a cross-sectional study in China. BMJ Open. 2017;7(10):e017293. doi:10.1136/bmjopen-2017-017293
16. Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PLoS One. 2013;8(12):e80633. doi:10.1371/journal.pone.0080633
17. Sun T-K, Chiu S-C, Yeh S-H, Chang K-C. Assessing reliability and validity of the Chinese version of the stroke scale: scale development. Int J Nurs Stud. 2006;43(4):457–463. doi:10.1016/j.ijnurstu.2005.07.004
18. Ng TS. Brief illness perception questionnaire (Brief IPQ). J Physiother. 2012;58(3):202. doi:10.1016/S1836-9553(12)70116-9
19. Miyazaki M, Nakashima A, Nakamura Y, et al. Association between medication adherence and illness perceptions in atrial fibrillation patients treated with direct oral anticoagulants: an observational cross-sectional pilot study. PLoS One. 2018;13(9):e0204814. doi:10.1371/journal.pone.0204814
20. Sjölander M, Eriksson M, Glader E-L. The association between patients’ beliefs about medicines and adherence to drug treatment after stroke: a cross-sectional questionnaire survey. BMJ Open. 2013;3(9):e003551. doi:10.1136/bmjopen-2013-003551
21. Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–637. doi:10.1016/j.jpsychores.2005.10.020
22. Lin Y-P, Chiu K-M, Wang T-J. Reliability and validity of the Chinese version of the brief illness perception questionnaire for patients with coronary heart disease. J Orient Inst Technol. 2011;2(31):145–155.
23. Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. doi:10.1016/S0022-3999(99)00057-4
24. Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. doi:10.1080/08870449908407311
25. Lyu Y, Li Z, Han My MX, Cheng G. An Fr. The reliability and validity of the Chinese version of beliefs about medical questionnaire among elderly patients with depressive disorder. Chin J Nurs. 2014;4:002.
26. Mahler C, Hermann K, Horne R, et al. Assessing reported adherence to pharmacological treatment recommendations. Translation and evaluation of the Medication Adherence Report Scale (MARS) in Germany. J Eval Clin Pract. 2010;16(3):574–579. doi:10.1111/j.1365-2753.2009.01169.x
27. Horne R. Measuring adherence: the case for self-report. Int J Behav Med. 2004;11:75.
28. Tian Q, Yu L. Reliability and validity of the Chinese version of medication adherence report scale for asthma. Chin J Nurs. 2014;49(5):621–624.
29. Peat J, Barton B. Medical Statistics: a Guide to Data Analysis and Critical Appraisal. John Wiley & Sons; 2008.
30. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: a Regression-Based Approach. Guilford Publications; 2017.
31. Guedes DT, Vafaei A, Alvarado BE, et al. Experiences of violence across life course and its effects on mobility among participants in the international mobility in aging study. BMJ Open. 2016;6(10):e012339. doi:10.1136/bmjopen-2016-012339
32. Preacher KJ, Hayes AF. SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi:10.3758/BF03206553
33. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi:10.3758/BRM.40.3.879
34. Brott T, Adams Jr HP, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–870. doi:10.1161/01.STR.20.7.864
35. Simpson SH, Eurich DT, Majumdar SR, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ. 2006;333(7557):15. doi:10.1136/bmj.38875.675486.55
36. Phatak HM, Thomas III J. Relationships between beliefs about medications and nonadherence to prescribed chronic medications. Ann Pharmacother. 2006;40(10):1737–1742. doi:10.1345/aph.1H153
37. Chambers JA, O’Carroll RE, Hamilton B, et al. Adherence to medication in stroke survivors: a qualitative comparison of low and high adherers. Br J Health Psychol. 2011;16(3):592–609. doi:10.1348/2044-8287.002000
38. Sangsongrit N, Pinyopasakul W, Ayuthya SKN, Sriprasong S, Nilanont Y. Predictors of medication adherence in ischemic stroke patients. Nurs J (Manila). 2014;41(2):61–71.
39. O’carroll R, Whittaker J, Hamilton B, Johnston M, Sudlow C, Dennis M. Predictors of adherence to secondary preventive medication in stroke patients. Ann Behav Med. 2010;41(3):383–390. doi:10.1007/s12160-010-9257-6
40. Kronish IM, Edmondson D, Goldfinger JZ, Fei K, Horowitz CR. Posttraumatic stress disorder and adherence to medications in survivors of strokes and transient ischemic attacks. Stroke. 2012;43(8):2192–2197. doi:10.1161/STROKEAHA.112.655209
41. Krauskopf K, Federman AD, Kale MS, et al. Chronic obstructive pulmonary disease illness and medication beliefs are associated with medication adherence. COPD. 2015;12(2):151–164. doi:10.3109/15412555.2014.922067
42. Sofianou A, Martynenko M, Wolf MS, et al. Asthma beliefs are associated with medication adherence in older asthmatics. J Gen Intern Med. 2013;28(1):67–73. doi:10.1007/s11606-012-2160-z
43. Leaungsomnapa Y, Promproh S, Leaungsomnapa S, Sourthao Y. Influence of beliefs about medication on high group of medication adherence in hypertensive patients. J Prapokklao Hosp Clin Med Educ Center. 2013;30(2):146–157.
44. Chan M, Mok E, Wong Y, et al. Attitudes of Hong Kong Chinese to traditional Chinese medicine and Western medicine: survey and cluster analysis. Complement Ther Med. 2003;11(2):103–109. doi:10.1016/S0965-2299(03)00044-X
45. Wei J-C-C, Su Y-C, Chang H-C, Jan M-S, Wong R-H, Chou C-T. Patient attitudes toward western medicine and the future of Chinese medicine for spondyloarthritis. Curr Rheumatol Rev. 2008;4(2):120–123. doi:10.2174/157339708784310275
46. Kronish IM, Diefenbach MA, Edmondson DE, Phillips LA, Fei K, Horowitz CR. Key barriers to medication adherence in survivors of strokes and transient ischemic attacks. J Gen Intern Med. 2013;28(5):675–682.
47. Mahler C, Hermann K, Horne R, Jank S, Haefeli WE, Szecsenyi J. Patients’ beliefs about medicines in a primary care setting in Germany. J Eval Clin Pract. 2012;18(2):409–413. doi:10.1111/j.1365-2753.2010.01589.x
48. Emilsson M, Gustafsson PA, Öhnström G, Marteinsdottir I. Beliefs regarding medication and side effects influence treatment adherence in adolescents with attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry. 2017;26(5):559–571. doi:10.1007/s00787-016-0919-1
49. Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC Health Serv Res. 2012;12(1):98. doi:10.1186/1472-6963-12-98
50. Chao J, Nau DP, Aikens JE, et al. The mediating role of health beliefs in the relationship between depressive symptoms and medication adherence in persons with diabetes. Res Social Adm Pharm. 2005;1(4):508–525. doi:10.1016/j.sapharm.2005.09.002
51. Le TT, Bilderback A, Bender B, et al. Do asthma medication beliefs mediate the relationship between minority status and adherence to therapy? J Asthma. 2008;45(1):33–37. doi:10.1080/02770900701815552
52. Jiang Y, Ni W. Estimating the impact of adherence to and persistence with atypical antipsychotic therapy on health care costs and risk of hospitalization. Pharmacother: J Hum Pharmacol Drug Ther. 2015;35(9):813–822. doi:10.1002/phar.2015.35.issue-9
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

