Back to Journals » Clinical Interventions in Aging » Volume 16
The Added Value of Combined Timed Up and Go Test, Walking Speed, and Grip Strength on Predicting Recurrent Falls in Chinese Community-dwelling Elderly
Authors Wang L, Song P, Cheng C, Han P, Fu L, Chen X, Yu H, Yu X, Hou L, Zhang Y, Guo Q
Received 7 July 2021
Accepted for publication 11 September 2021
Published 5 October 2021 Volume 2021:16 Pages 1801—1812
DOI https://doi.org/10.2147/CIA.S325930
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Lu Wang,1 Peiyu Song,1,* Cheng Cheng,1,2,* Peipei Han,3 Liyuan Fu,1 Xiaoyu Chen,3 Hairui Yu,1 Xing Yu,1 Lin Hou,1 Yuanyuan Zhang,1 Qi Guo1,3
1Department of Rehabilitation, School of Medical Technology, Tianjin Medical University, Tianjin, People’s Republic of China; 2Department of Rehabilitation, Tianjin Huanhu Hospital, Tianjin, People’s Republic of China; 3College of Rehabilitation Sciences, Shanghai University of Medicine and Health Sciences, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qi Guo
College of Rehabilitation Sciences, Shanghai University of Medicine and Health Sciences, Shanghai, China, 279 Zhouzhu Highway, Pudong New Area, Shanghai, 201318, People’s Republic of China
Tel +86-21-6588-3309
Fax +86-21-6588-3309
Email [email protected]
Purpose: To determine whether combined performance-based models could exert better predictive values toward discriminating community-dwelling elderly with high risk of any-falls or recurrent-falls.
Participants and Methods: This prospective cohort study included a total of 875 elderly participants (mean age: 67.10± 5.94 years) with 513 females and 362 males, recruited from Hangu suburb area of Tianjin, China. All participants completed comprehensive assessments.
Methods: We documented information about sociodemographic information, behavioral characteristics and medical conditions. Three functional tests—timed up and go test (TUGT), walking speed (WS), and grip strength (GS) were used to create combined models. New onsets of any-falls and recurrent-falls were ascertained at one-year follow-up appointment.
Results: In total 200 individuals experienced falls over a one-year period, in which 66 individuals belonged to the recurrent-falls group (33%). According to the receiver operating characteristic curve (ROC), the cutoff points of TUGT, WS, and GS toward recurrent-falls were 10.31 s, 0.9467 m/s and 0.3742 kg/kg respectively. We evaluated good performance as “+” while poor performance as “–”. After multivariate adjustment, we found “TUGT > 10.31 s” showed a strong correlation with both any-falls (adjusted odds ratio (OR)=2.025; 95% confidence interval (CI)=1.425– 2.877) and recurrent-falls (adjusted OR=2.150; 95%CI=1.169– 3.954). Among combined functional models, “TUGT > 10.31 s, GS < 0.3742 kg/kg, WS > 0.9467 m/s” showed strongest correlation with both any-falls (adjusted OR=5.499; 95%CI=2.982– 10.140) and recurrent-falls (adjusted OR=8.260; 95%CI=3.880– 17.585). And this combined functional model significantly increased discriminating abilities on screening recurrent-fallers than a single test (C-statistics=0.815, 95%CI=0.782– 0.884, P< 0.001), while not better than a single test in predicting any-fallers (P=0.083).
Conclusion: Elderly people with poor TUGT performance, weaker GS but quicker WS need to be given high priority toward fall prevention strategies for higher risks and frequencies. Meanwhile, the combined “TUGT–, GS–, WS+” model presents increased discriminating ability and could be used as a conventional tool to discriminate recurrent-fallers in clinical practice.
Keywords: recurrent-falls, elderly, physical functional performance, increased predictive value
Plain Language Summary
Since falls, especially recurrent-falls, pose a threat to the health of elderly people,investigations of conventional tools to screen recurrent-fallers are necessary. Our results indicated that the elderly with a poor TUGT performance, a weaker GS but a quicker WS were at highest risk of experiencing recurrent-falls, and this combined model showed significantly increased discriminating ability than any single test (P<0.001), with C-statistics at 0.815.
Introduction
Worldwide, one-third of people aged ≥65 years experience falls annually.1 Falls, especially recurrent-falls, have become the primary cause of unintentional injury death among the elderly,1 leading to injuries, loss of independence, and death in a third of those patients.2 Developing practical fall risk assessment tools is essential, especially for recurrent-falls, which may produce more severe impacts, like higher mortality and injuries.3
Muscle weakness, balance disturbance, and gait limitation are consistently identified as major fall risk factors4 although many factors, like cognitive problems and fear of falling, are also confirmed to be correlated with falls. This may suggest physical performances primarily worth more attention in a fall prevention program. Many single performance tests are proved to be good predictors of falls, however, literature about the diagnostic power of combined performance tests is still limited.4 Recent studies found combined functional tests had an additional predictive value in some adverse aspects. For example, walking speed (WS) and balance together was more useful in predicting potential stroke patients.5 Combined grip strength (GS), WS, and one-leg standing balance is better in predicting all-cause mortality than single test.6 Meanwhile, toward the effects of combined models on discriminating potential fallers, those models mostly included factors overriding multiple aspects to increase the reliability of assessment, like medical history, psychological condition, surrounding environment and functional tests,7–9 thus lacking of an easy and convenient fall-screening tool based on functional tests only, making our study more valuable.
In this study, we chose TUGT, WS, and GS, which were commonly used within the elderly population and always used as appropriate indicators of balance, mobility, and muscle strength,10–12 to clarify whether combined functional tests could exert a better predictive ability toward falls.
Previous studies have demonstrated these three tests could be used as screening tools for fall risks in elderly populations.13–16 Although these three tests targeted different aspects, correlations among them existed and could not be neglected. TUGT also included a stage of straight-ahead gait while GS was the key support during TUGT and WS test. Furthermore, our previous cross-sectional study found combined functional tests was more strongly correlated with previous falls.17 However, the predictive value and diagnostic accuracy of combined tests for identifying future falls, especially recurrent-falls, remains unknown.
Therefore, this study aim to discover whether combined functional tests could yield better predictive value in assessing any-falls or recurrent-falls. We focused on the community-dwelling elderly because they have relatively less mobility and more than 70% of elderly individuals living in suburban areas have limited access to medical treatment and a generally low health level.18
Materials and Methods
Subjects
Our study population consisted of residents of the suburb area who were ≥60 years and had been enrolled in the National Free Physical Examination Program. All subjects were invited to complete a comprehensive geriatric assessment in March 2016–2018 and attended re-assessment after one year. We set all the examined equipment and face-to-face interviewing in the local community hospital. The baseline physical performances were used to create predictive models. Exclusion criteria were as follows: (1) suffering from disturbing functional impairment, like visual disorders without adequate correction, cognitive problems, injury-induced loss of mobility and cause-specific muscle weakness interfering with daily activities; (2) using medications disturbing physical abilities or falls. (psychotropic drugs, cardiovascular drugs, hypoglycemic agents, nonsteroidal anti-inflammatory drugs, analgesics, dopaminergic drugs, Parkinson’s disease drugs or more than four kinds of complex drugs, which were evaluated by their medical history and doctors’ diagnosis); (3) refusing to complete assessments after one year. In total 1172 elderly took part in our study, according to the excluded criteria, 204 were excluded. Thus our primary included population contained 968 individuals. During the follow-up period, a further 93 were lost (79 cannot be connected, six died, eight bedridden). In total 875 people were in the final analysis. Detailed selecting process is shown in Figure 1. All participants were fully informed of the nature of research and signed an informed consent to participate. This prospective research was approved by the Ethics Committee of Tianjin Medical University and conducted in accordance with the Declaration of Helsinki, while the methodological sessions were carried out in accordance with the approved guidelines and regulations.
 |
Figure 1 The flowchart of selecting included participants. |
Covariates
Demographic, behavior performances and physical illnesses were obtained via face-to-face interview,19 lasting for nearly 40 min per individual. Demographic variables, comprising age, gender, living status, occupation, medicine use, history of falls and educational level, were assessed. Illness history was obtained from participants’ responses (yes or no) on hypertension, hyperlipidemia, stroke, coronary heart disease, peptic ulcer, gout, cancer, hepatic disease, biliary tract disease, thyroid disease, osteoarthritis, anemia, and kidney disease and corresponding medicine use and physician diagnosis. Living habits on smoking and drinking information (“currently”, “former” and “never”) were also acquired from the questionnaire. Weight and height were measured using a standard protocol.19 Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Physical activity level was measured by the average number of hours per day spent on leisure, household, and occupational physical activities over previous seven-day period, using the short form of the International Physical Activity Questionnaire (IPAQ).7 Responses were converted to metabolic equivalent task minutes per week (MET-min/week) and summed to create total MET scores.20 The Geriatric Depression Scale (GDS-30) was used to evaluate depression, with a score ≥11 were considered to be depressed.
GS (kg) was calculated with a handheld dynamometer (GRIP-D; Takei Ltd, Niigata, Japan). Participants were allowed to exert maximum efforts twice using dominant hand, and average GS was recorded.20 GS was adjusted with body weight to adjust grip strength to ensure muscle strength evaluated was independent of body size, since grip strength was correlated with muscle strength of lower limbs21 and body size17 while leg strength/body weight was predictive of functional ability in older adults.22 This standardized method had been recommended to normalize physical function testing results.22–24 TUGT assessed the seconds of standing up from a chair, walking three meters at usual pace past a line on the floor, turning around, walking back to the chair, and sitting down again with the back against the chair.7 WS was performed over four meters at the participants’ usual pace, using photocells to calculate time between activation of the first and second photocells and the average time of two trials were used in our analysis. Participants were allowed to use a gait-assistance device.20 Physical performance tests were monitored by corresponding professional physical therapists, providing sufficient practice for each participant.
Falls
A fall was defined as any event that results in a bodily change that forces an individual to inadvertently land on the ground or a lower level; the fall cannot be caused by a violent blow, loss of consciousness, sudden onset paralysis, or epileptic seizure.16 We collected data on falls through a telephone follow-up monthly and asked participants to complete a recall questionnaire on falls at the scene after the one-year follow-up period. The date, site and circumstances of falls were also recorded. Participants were divided into no-fall, any-falls and recurrent-falls group with experiencing new onset of 0, ≥1 and ≥2 falls during the follow-up period, respectively.
Statistical Analysis
Differences between variables were examined by one-way ANOVAs (continuous variables) or by chi-squared test (categorical variables). Continuous variables were expressed as mean ±SD while categorical variables used an absolute number and percentage of the total. Multigroup comparisons were carried out by one-way ANOVAs with post hoc contrasts by Student–Newman–Keuls test. Specificity measures the proportion of negatives that are correctly identified while sensitivity measures the proportion of positives that are correctly identified. The receiver operating characteristic curve (ROC), which was a graph of sensitivity plotted against (1–specificity) overall possible diagnostic cut points, was used to determine cutoff points of three tests toward any-falls and recurrent-falls, respectively, mainly obtained from the maximal Youden’s index, calculated as (sensitivity+specificity –1) and the greatest combination of sensitivity and specificity. Binary logistic regression analyses were used to assess the associations between models and any-falls or recurrent-falls. The crude model did not adjust for any confounders, while in model 1, only age and gender were adjusted. In model 2, models toward any-falls were additionally adjusted for widowed, cohabit with spouse, walking aid, fall history, diabetes, and depression, whereas models toward recurrent-falls were additionally adjusted for widowed, living alone, cohabiting with spouse, walking aid, fall history, diabetes, peptic ulcer, biliary tract disease, osteoarthritis, and depression. We further determined all significant functional models toward any-falls and recurrent-falls, respectively, using C-statistics to determine whether combined models improved discrimination ability. Significance was set at two-tailed P<0.05. All statistical analysis were performed with SPSS V18.0 software package (SPSS Inc., Chicago, IL, USA).
Results
We completed re-assessments on 875 elderly after the follow-up period, mainly concentrating on the new onset of falls. Two hundred people fell; 134 subjects experienced single-fall while 66 people experienced recurrent falls.
Characteristics of the Study Population at Baseline
The baseline characteristics of population are shown in Table 1. In total 875 elderly people (513 females and 362 males) aged ≥60 were included. The mean age was 67.10±5.94 years old. The percentages of any-falls for men and women were 19.1% and 25.5%, respectively, while the proportions of recurrent-falls for men and women were 6.1% and 8.6%, respectively, indicating that the female gender may be more likely to associated with higher risk and number of falls. More women experienced falls, accounting for 65.5% in any-fallers and 66.7% in recurrent-fallers. Recurrent-fallers were significantly older than those without falls or with a single fall. Any-fallers showed significant difference in age, gender, cohabiting with others, history of falls, walking aid, depression, and diabetes with no-fallers. Moreover, recurrent-fallers additionally presented significant difference in living alone, hepatic disease, peptic ulcer, osteoarthritis, biliary tract disease with other groups. Regarding of physical performances, any-fallers spent more time on TUGT, showed weaker GS and slower WS than no-fallers, and repeated fallers showed similar trends with any-fallers.
 |
Table 1 Baseline Characteristics of Study Participants (No-fall Group, Any-falls Group and Recurrent-falls Group) During the Follow-up Period |
Evaluations of Functional Tests Based on ROC Curve
Table 2 showed that the cutoff points of TUGT, GS and WS toward both any-falls and recurrent-falls were 10.31 s, 0.3742 kg/kg and 0.9467 m/s, respectively. Meanwhile, the ROCs of TUGT, GS, and WS toward any-falls were 0.616, 0.567, and 0.570, respectively, while recurrent-falls were 0.685, 0.576 and 0.605, respectively. We evaluated good performances as “+” and bad performances as “–” based on the cutoffs.
 |
Table 2 Cutoff Points of TUGT, GS, and WS Toward Any-falls and Recurrent-falls According to the Receiver Operating Characteristic Curve (ROC) |
(“TUGT+” <10.31 s, “TUGT–” >10.31 s; “GS+” >0.3742 kg/kg, “GS–” <0.3742 kg/kg; “WS+” >0.9467 m/s, “WS–” <0.9467 m/s.)
Increased Value of Combined Functional Models Toward New Onset of Any-falls and Recurrent-falls Over Follow-up Period
The correlations between all functional models with risks of any-falls and recurrent-falls were presented in Supplementary Table 1 and Supplementary Table 2 respectively. All significant performance-based models toward any-falls and recurrent-falls were listed in Tables 3 and 4 respectively. Toward any-falls, model 1 was adjusted for age and gender while model 2 was additionally adjusted for IPAQ, cohabiting with spouse, walking aid, fall history, diabetes and depression. It was clear that “GS–” (adjusted odds ratio, OR=1.498; 95% confidence interval, CI=1.032–2.173), “TUGT–” (adjusted OR=2.025; 95%CI=1.425–2.877), “TUGT–, GS–” (adjusted OR=2.091; 95%CI=1.440–3.036), “TUGT–, WS+” (adjusted OR=2.943; 95%CI=1.885–4.592), “TUGT–, GS–, WS+” (adjusted OR=5.499; 95%CI=2.982–10.140) were positively associated with any-falls. Toward recurrent-falls, model 1 was adjusted for age and gender while model 2 was additionally adjusted for IPAQ, cohabiting with spouse, living alone, walking aid, fall history, diabetes, peptic ulcer, biliary tract disease, osteoarthritis, and depression. “TUGT–” alone (adjusted OR=2.150; 95%CI=1.169–3.954), “TUGT–, GS–” (adjusted OR=2.536; 95%CI=1.351–4.759), “TUGT–, WS+” (adjusted OR=3.903; 95%CI=2.093–7.279) and “TUGT–, GS–, WS+” (adjusted OR=8.260; 95%CI=3.880–17.585) were observed to be tightly correlated with recurrent-falls.
 |
Table 3 Odds Ratio (OR) and 95% Confidence Interval of Performance-based Models for New Onset of Any-falls |
 |
Table 4 Odds Ratio (OR) and 95% Confidence Interval of Performance-based Models for New Onset of Recurrent-falls |
In addition, Table 5 showed C-statistics and 95%CI of all significant models towards any-fallers and recurrent-fallers, which were presented in Figure 2. Although “TUGT, GS–, WS+” showed an increasing tendency of discriminating any-fallers, it did not exert a more significant increase than a single test (P=0.083). While toward screening recurrent-fallers, “TUGT–, GS–, WS+” presented significantly increased discriminating ability (with C-statistics at 0.815), significantly better than a single test or other combined models (P<0.001).
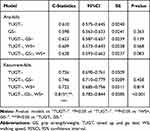 |
Table 5 Added Value of Combined Performance-based Models Than a Single Test |
Discussion
In this study, we compared the predictive values of TUGT, WS, and GS alone and combined models for screening any-fallers and recurrent-fallers in a suburb-dwelling population ≥60 years in China. And “TUGT–, GS–, WS+” showed increased prognostic power toward discriminating recurrent-fallers than a single test, with the AUC increasing from 0.726 to 0.815.
Previous studies suggested that gender and age should be controlled to provide better information about predictive value,7 mainly because female gender was associated with a higher prevalence of falls25 by the faster decline of bone mass,26 and skeletal muscle mass27 than men as well as age-related reduction in muscle mass and muscle strength and deterioration of overall physical motor skills and abilities.28 Meanwhile, other adjusted factors in our model, including IPAQ, cohabiting with others, living alone, walking aid, fall history, depression, osteoarthritis, and diabetes, have also been noted in previous studies.3,16,17,29,30
The Predictive Ability of TUGT, GS and WS Toward Two Types of Falls
TUGT has been widely recommended for assessing gait and balance31 to screen risks of falls in the elderly.15,31 Our results showed that TUGT had the best ROC over three tests and was significantly associated with any-falls and recurrent-falls, which may be because TUGT not only focuses on one function, but also contains multiple components of balance and mobility related with executive function, thus directly correlating with falls.32 In addition, we observed “TUGT–” had a moderate predictive ability in screening any-fallers (AUC at 0.610) but a greater efficacy in screening recurrent-fallers (AUC at 0.726), which may be because any-falls over a 12-month period were mostly considered as an accidental event related to environmental factors while recurrent-falls mostly reflected motor disorders,28 making “TUGT–” toward detecting recurrent-fallers more reliable. This was consistent with our previous finding that TUGT showed strong ability in discriminating recurrent-fallers.16
GS was a representative measure of upper muscle strength and correlated with trunk and lower limb strength,28 thus widely used as a symbol of total muscle strength. Our results showed “GS–” was correlated with any-falls, which may be caused by impaired mobility and frailty33 and loss of agility.34 Decreased muscle strength may subsequently lead to fear of falling and difficulties in completing activities, further contributing to activity limitations and more falls.35 However, our results found “GS–” was weakly associated with recurrent-falls. Such an unexpected result may be explained by a preceding finding that the elderly with both weak and strong muscle strength were at high risk of falls, people with stronger strength commonly fell when planted or raised foot while those with weaker strength typically fell after their foot left the ground.36 Meanwhile, previous results indicated effects of muscle strength exercises were limited and poorly translated into improvement in balance, functional tasks, and falling rate.22
WS was an established indicator of overall gait performance6 and was correlated with falling risks.37,38 Previous studies found slower WS lead to decreased falling risk.37,38 An average 0.1 m/s increase in WS produced 15% and 5% increased risks of falls in men and women, respectively.38 However, our results showed that WS was independent of two falls. Such differences may be caused by the average age of our group was younger than that group (67.10 years vs 69.7 years), meanwhile, the average WS of our group, which was relatively lower than that group (1.30±0.36 m/s vs 1.00±0.21 m/s). Faster WS may lead to an increased occurrence of leg lowering and a longer period of recovery toward a steady-state walking pattern, therefore limitations in the magnitude and rate of muscle recruitment in that group may be greater.39 And WS likely had a nonlinear relationship with falls,40 indicating that elderly with faster and slower WS were both at higher risk of falling.
The Predictive Ability of Combined Performance Models Toward Two Types of Falls
It should be noted firstly that most significant models toward two types of falls include “TUGT–”, which remained the dominant role of TUGT in the combined group. This may be because TUGT was a complex activity process assessing dynamic balance during gait and transfer tasks, mobility, and lower body strength.41 And dynamic balance exercises, targeting on improving TUGT, were key methods recommended for fall prevention since most falls occurred during complex task-walking which required good mobility and prefect turning or transferring abilities.21 Our finding that combining “WS+” or “GS–” with “TUGT–” did not increase discriminating abilities, which further indicated the important role of TUGT in combined models.
We observed GS only played a critical role in combined models toward recurrent-falls, with GS alone had no correlation while “TUGT–, GS–” showed a strong correlation. This may be explained by muscle strength, which was an important predictor during dynamic postural control for not providing enough stable support.36 And muscle strength always reflected the extent of fear of falling,21 which related to reduced physical activities, narrowed scope of movement, and increased falling risk and number.28
Our data showed WS should be combined with other performance tests to screen fallers. Using the “TUGT–, WS+” model, we found no-fallers had slower WS than any-fallers (0.867±0.153 m/s VS 0.892±0.219 m/s), which may because TUGT signified mobility performance and WS was part of TUGT, therefore the role of WS would vary with alternations of mobility. For instance, individuals with good mobility who walked more quickly34 would be exposed to more chances of falls than those walking slowly and carefully. Pavol et al42 also confirmed this view that individuals with a faster walking velocity were more likely to experience higher risk of during-step or elevating-response falls. This may be caused by different gait characteristics of no-fall, one-time fall, and repeated-fall groups, including gait speed, step length and gait cycle, thus using single WS to predict fall risks may not comprehensive enough.28 Therefore, we suggested WS should be incorporated with other mobility tests on predicting falls.
Obviously, combined the “TUGT–, GS–, WS+” model exhibited the biggest ORs over all the models both with any-falls an recurrent-falls. However, the combined model showed a significantly increased discriminating value in screening recurrent-fallers, rather than any-fallers. This difference may be caused by multiple reasons, which further added to the higher reliability of the combined model towards recurrent-fallers. A previous study pointed out that although TUGT could reflect various physical abilities, it may also have suffered from the same limitation that cannot separate the effect of subcomponents.21 For the elderly who showed “WS+”, they were more likely to experience higher risk or number of falls if they had poor sitting-to-stand transitions, turning and transferring or sitting down abilities.21 Meanwhile, weaker muscle strength not only indicated not enough stable support during movement,36 but also partly reflected impaired functions of musculoskeletal system.17 As functional tests, TUGT and WS could also be affected by internal factors related to more occurrences of falls, such as age, body shape, vestibular sense, proprioception and vision, which may have promoted increased numbers of falls through failing to navigate effectively because of imprecise vision,17 misjudgment of distances and misinterpretation of spatial information by impoverished visual input,43 postural instability and unsteady turns with vestibular hypofunction.44 Therefore, the joint effects of those internal factors on predicting recurrent-falls were addressed by our combined functional models.
Our combined screening tool was found to be reliable and a high-quality predictor of recurrent-fallers in this sample. Any health-care provider could easily perform this fall-risk assessment. The discriminating model can be rapidly assessed by carrying our three simple tests, thus it may serve as an initial step in community dwellings of the elderly to predict risks of recurrent-falls while avoiding unnecessary evaluations and extra costs. Admittedly, if this risk model is applied to another population, its effectiveness and feasibility should first be revalidated.
Strengths and Limitations
Our study includes some significant strengths. To our knowledge, this study is one of the first studies using TUGT, GS, and WS to identify the added value of combined performance-based tests in discriminating recurrent-fallers. In addition, the study is also the first one to examine a uniquely defined group of suburban elderly people living in a discrete geographic area, which may differ from individuals in other geographical areas.
Our study also includes some limitations. Firstly, this model has not yet been validated in other populations and the current sample size may not large enough. To validate the risk profile, its predictive ability has to be examined prospectively. Secondly, the follow-up period is relatively short, thus changes in overall health status may be limited. Thirdly, due to inconsistent population characteristic of different regions, the cutoff points of TUGT, GS, and WS may not applicable to all Chinese elderly populations. Therefore, it is necessary to further carry out such projects nationwide to verify whether there are uniform cutoff values of these three physical tests toward recurrent-falls.
Conclusion
In summary, we found combined “TUGT–, GS–, WS+” was more predictive than any single test in discriminating recurrent-fallers in Chinese community-dwelling elderly. In clinical practices, elderly people with poor balance and grip strength but good walking speed need more attention and be protected with fall prevention interventions. Meanwhile, “TUGT–, GS–, WS+” could be used as an conventional tool to discriminating potential recurrent-fallers exceeding AUC at 0.815 in clinical practices.
Acknowledgments
The authors thank Guiyan Shao from the public health center and Xiaofeng Ren from welfare house for providing place and organization. We also thank for the cooperation from Hairui Yu, Peiyu Song, Yuanyuan Zhang, Xing Yu and Lin Hou at Hangu community.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation of China (grant number 81372118), Tianjin Municipal Science and Technology Commission (grant number 16ZXMJSY00070) and Health and Family Planning Commission of Binhai New Area (2017BWKZ005).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Essien SK, Feng CX, Sun WJ, Farag M, Li LH, Gao YQ. Sleep duration and sleep disturbances in association with falls among the middle-aged and older adults in China: a population-based nationwide study. BMC Geriatr. 2018;18(1):1–4.
2. Zhong Q, Ali N, Gao Y, et al. Gait kinematic and kinetic characteristics of older adults with mild cognitive impairment and subjective cognitive decline: a cross-sectional study. Front Aging Neurosci. 2021;13:664558. doi:10.3389/fnagi.2021.664558
3. Wu TY, Chie WC, Yang RS, Kuo KL, Wong WK, Liaw CK. Risk factors for single and recurrent falls: a prospective study of falls in community dwelling seniors without cognitive impairment. Prev Med. 2013;57(5):511–517. doi:10.1016/j.ypmed.2013.07.012
4. Hirase T, Inokuchi S, Matsusaka N, Nakahara K, Okita M. A modified fall risk assessment tool that is specific to physical function predicts falls in community-dwelling elderly people. J Geriatr Phys Ther. 2014;37(4):159–165. doi:10.1519/JPT.0b013e3182abe7cb
5. Rosa MC, Marques A, Demain S, Metcalf CD. Fast gait speed and self-perceived balance as valid predictors and discriminators of independent community walking at 6 months post-stroke - a preliminary study. Disabil Rehabil. 2015;37(2):129–134. doi:10.3109/09638288.2014.911969
6. Nofuji Y, Shinkai S, Taniguchi Y, et al. Associations of walking speed, grip strength, and standing balance with total and cause-specific mortality in a general population of Japanese elders. J Am Med Dir Assoc. 2016;17(2):
7. Kang L, Chen XY, Han PP, et al. A screening tool using five risk factors was developed for fall-risk prediction in Chinese community-dwelling elderly individuals. Rejuvenation Res. 2018;21(5):416–422. doi:10.1089/rej.2017.2005
8. Novin RS, Taylor E, Hermans T, Merryweather A. Development of a novel computational model for evaluating fall risk in patient room design. HERD. 2021;14(2):350–367. doi:10.1177/1937586720959766
9. Severo IM, Kuchenbecker R, Vieira DFVB, et al. A predictive model for fall risk in hospitalized adults: a case-control study. J Adv Nurs. 2019;75(3):563–572. doi:10.1111/jan.13882
10. Hansson EE, Valkonen E, Moller UO, Lin YC, Magnusson M, Fransson PA. Gait flexibility among older persons significantly more impaired in fallers than non-fallers-A longitudinal study. Int J Environ Res Public Health. 2021;18(13):7074.
11. Groessl EJ, Kaplan RM, Rejeski WJ, et al. Physical activity and performance impact long-term quality of life in older adults at risk for major mobility disability. Am J Prev Med. 2019;56(1):141–146. doi:10.1016/j.amepre.2018.09.006
12. Yang S, Chen C, Du SY, et al. Assessment of isokinetic trunk muscle strength and its association with health-related quality of life in patients with degenerative spinal deformity. BMC Musculoskel Dis. 2020;21(1):1–9. doi:10.1186/s12891-020-03844-8.
13. Sasaki E, Sasaki S, Chiba D, et al. Age-related reduction of trunk muscle torque and prevalence of trunk sarcopenia in community-dwelling elderly: validity of a portable trunk muscle torque measurement instrument and its application to a large sample cohort study. PLoS One. 2018;13(2):e0192687. doi:10.1371/journal.pone.0192687
14. Davis JC, Best JR, Khan KM, et al. Slow processing speed predicts falls in older adults with a falls history: 1-year prospective cohort study. J Am Geriatr Soc. 2017;65(5):916–923. doi:10.1111/jgs.14830
15. Larsson BAM, Johansson L, Johansson H, et al. The timed up and go test predicts fracture risk in older women independently of clinical risk factors and bone mineral density. Osteoporosis Int. 2021;32(1):75–84. doi:10.1007/s00198-020-05681-w
16. Kang L, Han P, Wang J, et al. Timed up and go test can predict recurrent falls: a longitudinal study of the community-dwelling elderly in China. Clin Interv Aging. 2017;12:2009–2016. doi:10.2147/CIA.S138287
17. Wang XY, Ma YX, Wang JZ, et al. Mobility and muscle strength together are more strongly correlated with falls in suburb-dwelling older Chinese. Sci Rep. 2016;6(1):1–7.
18. Jiang H, Liu L, Liu T, Zhu S, Hou L. Current status on the ability of the elderly in rural China: implications for future nursing and policy. Cardiovasc Diagn Ther. 2020;10(5):1216–1225. doi:10.21037/cdt-20-555
19. Zhang W, Shen SX, Wang W, et al. Poor lower extremity function was associated with pre-diabetes and diabetes in older Chinese people. PLoS One. 2014;9(12):e115883. doi:10.1371/journal.pone.0115883
20. Yu X, Hou L, Guo J, et al. Combined effect of osteoporosis and poor dynamic balance on the incidence of sarcopenia in elderly Chinese community suburban-dwelling individuals. J Nutr Health Aging. 2020;24(1):71–77. doi:10.1007/s12603-019-1295-6
21. Ho HH, Fang IY, Yu YC, et al. Is functional fitness performance a useful predictor of risk of falls among community-dwelling older adults? Arch Public Health. 2021;79(1):1–9. doi:10.1186/s13690-021-00608-1.
22. Song PY, Han PP, Zhao YJ, et al. Muscle mass rather than muscle strength or physical performance is associated with metabolic syndrome in community-dwelling older Chinese adults. BMC Geriatr. 2021;21(1):1–9. doi:10.1186/s12877-021-02143-8.
23. Suwa M, Imoto T, Kida A, Iwase M, Yokochi T. Age-related reduction and independent predictors of toe flexor strength in middle-aged men. J Foot Ankle Res. 2017;10(1):15. doi:10.1186/s13047-017-0196-3
24. Li FE, Zhang FL, Zhang P, et al. Sex-based differences in and risk factors for metabolic syndrome in adults aged 40 years and above in Northeast China: results from the cross-sectional China national stroke screening survey. BMJ Open. 2021;11(3):e038671.
25. Cella A, De Luca A, Squeri V, et al. Development and validation of a robotic multifactorial fall-risk predictive model: a one-year prospective study in community-dwelling older adults. PLoS One. 2020;15(6):e0234904. doi:10.1371/journal.pone.0234904
26. Sharif SI, Al-Harbi AB, Al-Shihabi AM, Al-Daour DS, Sharif RS. Falls in the elderly: assessment of prevalence and risk factors. Pharm Pract (Granada). 2018;16(3):1206. doi:10.18549/PharmPract.2018.03.1206
27. Chatzipetrou V, Begin MJ, Hars M, Trombetti A. Sarcopenia in chronic kidney disease: a scoping review of prevalence, risk factors, association with outcomes, and treatment. Calcif Tissue Int. 2021:1–31. doi:10.1007/s00223-021-00898-1
28. Jeon M, Gu MO, Yim J. Comparison of walking, muscle strength, balance, and fear of falling between repeated fall group, one-time fall group, and nonfall group of the elderly receiving home care service. Asian Nurs Res. 2017;11(4):290–296.
29. Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the timed up and go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta- analysis. BMC Geriatr. 2014;14(1):14. doi:10.1186/1471-2318-14-14
30. Zhou H, Peng K, Tiedemann A, Peng J, Sherrington C. Risk factors for falls among older community dwellers in Shenzhen, China. Inj Prev. 2018;25(1):31–35.
31. Bristow SM, Bolland MJ, Gamble GD, Leung W, Reid IR. Dietary calcium intake and change in bone mineral density in older adults: a systematic review of longitudinal cohort studies. Eur J Clin Nutr. 2021:1 doi:10.1038/s41430-021-00957-8
32. Pinto EB, Nascimento C, Monteiro M, et al. Proposal for a new predictive scale for recurrent risk of fall in a cohort of community-dwelling patients with stroke. J Stroke Cerebrovasc Dis. 2016;25(11):2619–2626. doi:10.1016/j.jstrokecerebrovasdis.2016.06.045
33. Caetano MJD, Lord SR, Allen NE, et al. Executive functioning, muscle power and reactive balance are major contributors to gait adaptability in people with Parkinson’s disease. Front Aging Neurosci. 2019;11:154. doi:10.3389/fnagi.2019.00154
34. Prato SCF, Andrade SM, Cabrera MAS, et al. Frequency and factors associated with falls in adults aged 55 years or more. Rev Saude Publica. 2017;51:37. doi:10.1590/s1518-8787.2017051005409
35. Sex LE. Differences in fear of falling among older adults with low grip strength. Iran J Public Health. 2016;45(5):569–577.
36. Paillard T. Relationship between muscle function, muscle typology and postural performance according to different postural conditions in young and older adults. Front Physiol. 2017;8:585. doi:10.3389/fphys.2017.00585
37. Laddu DR, Parimi N, Stone KL, et al. Physical activity trajectories and associated changes in physical performance in older men: the MrOS study. J Gerontol a Biol Sci Med Sci. 2020;75(10):1967–1973. doi:10.1093/gerona/glaa073
38. Kato S, Murakami H, Demura S, et al. Abdominal trunk muscle weakness and its association with chronic low back pain and risk of falling in older women. BMC Musculoskelet Disord. 2019;20(1):273. doi:10.1186/s12891-019-2655-4
39. Xu JC, Silvano AP, Keller A, et al. Identifying and characterizing types of balance recovery strategies among females and males to prevent injuries in free-standing public transport passengers. Front Bioeng Biotechnol. 2021;9:670498. doi:10.3389/fbioe.2021.670498
40. Gade GV, Jorgensen MG, Ryg J, Masud T, Jakobsen LH, Andersen S. Development of a multivariable prognostic PREdiction model for 1-year risk of FALLing in a cohort of community-dwelling older adults aged 75 years and above (PREFALL). BMC Geriatr. 2021;21(1):402. doi:10.1186/s12877-021-02346-z
41. Martins AC, Moreira J, Silva C, et al. Multifactorial screening tool for determining fall risk in community-dwelling adults aged 50 years or over (FallSensing): protocol for a prospective study. JMIR Res Protoc. 2018;7(8):e10304. doi:10.2196/10304
42. Pavol MJ, Owings TM, Foley KT, et al. Influence of lower extremity strength of healthy older adults on the outcome of an induced trip. J Am Geriatr Soc. 2002;50(2):256–262.
43. Zhang SL, Liu D, Yu DZ, et al. Multisensory exercise improves balance in people with balance disorders: a systematic review. Curr Med Sci. 2021;41(4):635–648. doi:10.1007/s11596-021-2417-z
44. Noohi F, Kinnaird C, De Dios Y, et al. Deactivation of somatosensory and visual cortices during vestibular stimulation is associated with older age and poorer balance. PLoS One. 2019;14(9):e0221954. doi:10.1371/journal.pone.0221954
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

