Back to Journals » Journal of Pain Research » Volume 15
Testing Topical Products Specifically to Reduce Inflammatory Pain from Gout: Transdermal NSAID Delivery and Monosodium Urate Solubility
Received 22 March 2022
Accepted for publication 21 June 2022
Published 29 June 2022 Volume 2022:15 Pages 1825—1835
DOI https://doi.org/10.2147/JPR.S367536
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert B. Raffa
Video abstract presented by Mark Hooper.
Views: 873
Mark W Hooper,1 Liang He2
1MedCryst Therapeutics Ltd, Centre for Innovation & Enterprise, Oxford University Begbroke Science Park, Oxford, OX5 1PF, UK; 2PharmHe, Chertsey, UK
Correspondence: Mark W Hooper, MedCryst Therapeutics Ltd, Centre for Innovation & Enterprise, Oxford University Begbroke Science Park, Oxford, OX5 1PF, UK, Tel +44 7468 902851, Email [email protected]
Purpose: Gout is caused by crystals of monosodium urate (MSU) in the joints. Topical nonsteroidal anti-inflammatory drug products (NSAIDs) are often the first-choice immediate treatment. This study examined the effect of commercially available and newly developed transdermal NSAID products on the solubility of MSU in a physiologically relevant system, alongside the efficacy of transdermal NSAID delivery.
Materials and Methods: Drug permeability of 7 commercially available topical NSAID products, alongside 3 newly developed “Gout Buster” products, was evaluated in vitro using pig’s ear skin in Franz diffusion cells. The standard Franz cell experimental protocol was adapted to include assessment of MSU solubility in phosphate buffered saline for each product. Some materials were also tested via direct solubility studies.
Results: The amount of drug delivered transdermally varied significantly between different formulations, with the best ibuprofen delivery being ∼ 5 times higher than the lowest, and best diclofenac delivery being ∼ 3.5 times higher than the lowest. Changes in formulations and the drug concentration in the product both affected the amount of drug delivered. Overall ibuprofen permeation was higher than diclofenac. The commercially available products showed little or no effect on the MSU solubility (99– 103% vs control). The Gout Buster products showed significant improvement in the MSU solubility after permeation through skin (120– 126%). Increased sodium levels reduced the solubility of MSU in direct solubility studies.
Conclusion: In these trials, the Gout Buster products showed significantly improved permeation of both ibuprofen and diclofenac over the commercial products at similar drug concentrations, and showed significant improvement for MSU solubility. Increased sodium levels reduced the solubility of MSU and could cause more crystallisation in vivo. Therefore, topical NSAID products with the Gout Buster formulation may have the best likelihood of both reducing inflammation and helping re-dissolve the MSU crystals that cause gout.
Keywords: Franz-cell experiments, nonsteroidal anti-inflammatory drug, in vitro study, Gout Buster
Introduction
NSAIDs are an effective treatment for acute and chronic pain for arthritis.1 Gout is a form of arthritis, caused by high levels of urate in blood (hyperuricemia), leading to formation of monosodium urate (MSU) crystals in joints. This causes a very painful inflammatory response. MSU crystals were shown to cause gout in 1960s2 and there was a seminal study on factors affecting solubility of MSU in relevant media in 1974 (Kippen).3 The main factors affecting MSU solubility were shown to be pH and sodium levels. Long-term treatments for gout generally target lowering urate levels in the blood, reducing the likelihood of MSU crystals forming.
Short-term treatments mostly focus on reducing inflammation.1 Topical NSAIDs are a mainstay of this treatment. Topical delivery avoids issues associated with oral or intravenous NSAID delivery (serious side-effects, inconvenient injections).4 There have been some studies investigating the combination of treatments for both urate lowering and anti-inflammatory with transdermal delivery. Tiwari et al investigated nano-particles of both uricase (lowering urate levels) and aceclofenac (an NSAID) together with good efficacy.5 Bou-Salah et al carried out in-vitro and in-silico investigation into the urate lowering potential of several NSAIDs.6
Permeability of the drug is an important factor in topical NSAID delivery. The drugs need to get through the layers of skin (stratum corneum, epidermis and dermis) to reach the inflamed area, typically around a joint for gout. Various factors affect the rate of permeation and amount of drug delivered. These include concentration of drug, the drug properties, specific salt used and the formulation.7,8 However, most topical NSAID drug delivery results in lower systemic levels of drug when compared to recommended oral doses.9,10 Therefore, higher permeation is generally desired to maximise the anti-inflammatory effect of topically applied NSAIDs.
It is not clear from available information supplied with commercial products which formulation or strength of topical product actually delivers the highest levels of drug to the affected areas. There have also been few or no studies on whether the commercial topical products have any direct effect on the in-situ solubility of the MSU crystals.
There is no definitive simple lab test to rate the absolute permeability of a NSAID from a topical formulation, but Franz cell experiments give good comparative data.7 Human skin is the best membrane to use to imitate in vivo, but not it is always available. Pig’s ear skin has been shown to be a good equivalent to human skin.11 For gout, we are looking at release of drugs into joints, so full thickness skin can be used to better imitate the challenges of delivering into the synovial capsule. This leads to longer experiments in the Franz cell apparatus, up to 72 hours. This shows good comparative data, even if it is a less direct imitation real-life application of the gels on to a joint. It is difficult to get fully repeatable data from Franz-cell experiments, as investigated in various validation studies such as Ng et al.12 However, if the investigation parameters are kept consistent, then useful results can be generated to compare different products and formulation, even if the absolute values obtained will not be identical to those with live human skin.
The second part of this study is to examine the effect of topical formulations on the specific cause of gout, which is the MSU crystals. pH and sodium levels were shown to be the main factors controlling MSU solubility, so controlling the pH and level of sodium to physiological levels results in a medium that is a good lab-based imitation of synovial fluids/blood, eg, using phosphate buffered saline. It would be too inaccurate to isolate the MSU solids and measure “re-dissolving” directly, as the changes in weight would be small and the samples would retain significant water. However, the saturated MSU solubility in the medium can be measured. If higher MSU solubility is observed, then more crystals will dissolve and can be removed via the body’s normal equilibration process. The kinetics of MSU dissolution in vivo is often very slow,13 so the crystals need help to re-dissolve.
Reducing MSU saturated solubility will have the opposite effect, making it more likely that MSU will precipitate and cause further gout attacks. The effect of the products on MSU solubility should ideally be tested after permeation through skin (ie, in a Franz cell experiment), as some components will not diffuse through the skin (eg, carbomer) and therefore will have no effect on MSU solubility in vivo. However, some indication of effect on MSU solubility can be found using direct addition of a component or formulation into a media (such as PBS) saturated with excess MSU.
Therefore, Franz-cell experiments using pig’s ear membranes and phosphate buffered saline, with excess mono-sodium urate (MSU) should result in a good comparative lab-based model to assess both the relative permeability of the NSAID drugs from commercially available topical formulations, and also assess any potential effect on the in-situ MSU solubility. NSAID delivery and MSU solubilities are both important factors in treating the inflammation resulting from gout, and in resolving the unwanted MSU crystals.
Materials and Methods
Materials
Seven commercial products and three new “Gout Buster” products were used for this study, alongside a control of just phosphate buffered saline (PBS). The components of the formulations are shown below.
- Boots ibuprofen gel 5% (“BO ibuprofen gel 5%”, The Boots Company PLC, Nottingham, UK): ibuprofen, carbomer, diisopropanolamine, propylene glycol, ethanol and water
- Radian B ibuprofen gel 5% (“RB ibuprofen gel 5%”, Thornton & Ross Ltd, Huddersfield, UK): ibuprofen, hydroxyethyl cellulose, sodium hydroxide, benzyl alcohol, isopropyl alcohol, water
- Ibuleve ibuprofen gel 5% (“IB ibuprofen gel 5%”, Diomed Developments Ltd, Hitchin, UK): ibuprofen, carbomer, diethylamine, IMS, water, propylene glycol
- Ibuleve ibuprofen gel 10% (“IB ibuprofen gel 10%”, Diomed Developments Ltd, Hitchin, UK): ibuprofen, carbomer, diethylamine, IMS, water
- Nurofen ibuprofen gel 10% (“NU ibuprofen gel 10%”, Reckitt Benckiser Healthcare, Slough, UK): ibuprofen, hydroxyethyl cellulose, sodium hydroxide, benzyl alcohol, isopropyl alcohol, water
- Voltarol diclofenac Emugel 1.16% (“VO diclofenac gel 1%”, GlaxoSmithKline, Brentford, UK): diclofenac diethylammonium, carbomer, macrogol cetostearyl ether, cocoyl caprylocaprate, isopropyl alcohol, liquid paraffin, perfume, propylene glycol, water
- Voltarol diclofenac Emugel 2.32% (“VO diclofenac gel 2%”, GlaxoSmithKline, Brentford, UK): diclofenac diethylammonium, carbomer, butylhydroxytoluene, diethylamine, macrogol cetostearyl ether, cocoyl caprylocaprate, isopropyl alcohol, liquid paraffin, perfume, oleyl alcohol, propylene glycol, water
- Gout Buster ibuprofen gel 5% (“GB ibuprofen gel 5%”, MedCryst Therapeutics, Oxford, UK): ibuprofen, menthol, trolamine (triethanolamine), benzyl alcohol, oleic acid, isopropyl alcohol, propylene glycol, PEG-200, carbomer, transcutol (diethylene glycol monoethyl ether), water
- Gout Buster diclofenac gel 1% (“GB diclofenac gel 1%”, MedCryst Therapeutics, Oxford, UK): diclofenac, menthol, trolamine (triethanolamine), benzyl alcohol, oleic acid, isopropyl alcohol, propylene glycol, PEG-200, carbomer, transcutol (diethylene glycol monoethyl ether), water
- Gout Buster no drug gel (“GB no drug gel”, MedCryst Therapeutics, Oxford, UK): menthol, trolamine (triethanolamine), benzyl alcohol, oleic acid, isopropyl alcohol, propylene glycol, PEG-200, carbomer, transcutol (diethylene glycol monoethyl ether), water
Note: The ibuprofen products are labelled directly with the amount of ibuprofen they contain, independent of the salt that is formed (in-situ). Ibuprofen (as free acid) has very low solubility in water-based gels, so is almost always present as a salt (to improve solubility), but the convention is to list the salt components separately for ibuprofen products.
However, for diclofenac products, the percentage drug content is somewhat confusingly added to be equivalent to the original sodium salt used in early products. So an original “Voltarol 1%” product contained 1% sodium diclofenac, ie, 0.93% diclofenac. The 1.16% Voltarol product above refers to the amount of diclofenac diethylammonium salt added, which is equivalent to 1% sodium diclofenac and 0.93% diclofenac. The 2.32% Voltarol product again refers to the amount of diclofenac diethylammonium added, ie, twice the concentration of the 1.16% product, equivalent to 1.86% diclofenac. The Gout Buster “1%” gel contains 0.93% diclofenac, forming a salt in-situ with trolamine. So all the “1%” products contain the same amount of drug (diclofenac) in spite of the confusing labelling. So for simplicity, the products containing 0.93% diclofenac will be labelled as “1%” in this paper, and the product containing 1.86% diclofenac will be labelled “2%”.
Methods
In vitro Skin Permeation with Franz Cells and Added MSU Solubility Assessment
Pig’s ears (pink) were sourced from a local abattoir as a waste product from the food industry and processed within 1 day of sourcing. As no human product or animal testing was used, the experiments did not raise ethical compliance issues. Full thickness pig’s ear skin was removed from the cartilage and frozen at −20°C until use. The skin was thawed, any excess fat was removed from under the skin and it was cut to ~2cm diameter circles for use directly in the Franz cell experiments. Each formulation was tested in minimum in duplicate, and a control was always used. (Ideally more repeats would have been run, but there was a limit to the number of experiments we could run. The minimum duplicate repeat allowed for any excessive variability to be observed and excluded, such as the possibility of a tear in the pig’s skin.) Skin samples were clamped between the donor and receiver cells and placed with the outside skin up, ie, in contact with the donor sample.
Static Franz cells were used with an exposed skin diameter of 0.7cm (1.05cm2 surface area, supplied by Soham Scientific, Soham, UK). The cells had a receiver volume of 10mL and stir bars were added to the cells. 10mg of monosodium urate (MSU) mono-hydrate (Sigma-Aldrich) was added to each cell (ie, 1mg/mL - this is a large excess of MSU as the control solubility for MSU in PBS at 25°C in 0.04mg/mL. This will allow any increase or decrease in the equilibrium MSU solubility to be achieved in the receiver cell). Phosphate buffered saline (PBS) was used as the receiving media (pH 7.4, phosphate buffer strength 0.01N, sodium concentration adjusted to 0.14mol/L with sodium chloride). All experiments were carried out at room temperature (20–25°C). Samples of the receiver media were removed after 72 hours, and filtered through a 0.2 micron syringe filter before being analysed by HPLC for urate and drug content (either ibuprofen or diclofenac as relevant).
1mL of each product/formulation was placed in the donor cell – this always gave full coverage of the skin, and provided sink conditions for the formulations. 1mL PBS was applied as a control for all experiments, and this cell was used as the “100%” level for MSU solubility in PBS.
HPLC Analyses of Sample from Receptor Media
Linearity for both drugs and MSU was established over the ranges analysed and specificity for each component was established when a single HPLC method was used (eg, to analyse both diclofenac and MSU content). Ibuprofen and MSU were analysed separately for each relevant sample using separate HPLC methods. Where needed, the excipients in each formulation/product were also tested for specificity to confirm that they did not interfere with the determination of concentrations of the drugs and MSU.
HPLC Methods
MSU content: Mobile phase: pH 5 acetate buffer 0.035M. HPLC column: Supelco OSIL LC5, 15cm x 4.6mm, 5µm. Flow rate: 1mL/min. Detector: UV set @ 292nm. Inj = 10µL. Urate peak at ~ 2.45mins. Run time 5mins.
MSU and diclofenac content: Mobile phase A (MPA): pH 5 acetate buffer 0.035M. Mobile phase B (MPB): acetonitrile. T=0: 100% MPA; T=6mins to T=6.5mins gradient to 60% MPA: 40% MPB; T=14mins to T=14.5mins gradient to 100% MPA. Run time 18mins. HPLC column: Supelco OSIL LC5, 15cm x 4.6mm, 5µm. Flow rate: 1mL/min. Inj = 10µL. Detector: UV set @ 292nm. Urate peak at ~ 2.45mins, diclofenac peak at ~11.3mins.
Ibuprofen content: Mobile phase A (MPA): pH 3 buffer (from 1mL NEt3 + 0.5mL conc. phosphoric acid in 1 litre DI water). Mobile phase B (MPB): acetonitrile. Run with 50% MPA and 50% MPB. Run time 8 mins. HPLC column: Supelco OSIL LC5, 15cm x 4.6mm, 5µm. Flow rate: 1mL/min. Inj = 10µL. Detector: UV set @ 220nm. Ibuprofen peak at ~ 4.9mins.
Vial-Based Solubility Assessments
A magnetic stirrer bar was added to a 7mL glass vial, followed by 5mg of MSU. 5mL of PBS was added followed by 1% (0.05mL or 0.05g) of the material to be tested. The vial was stirred at room temperature overnight. A sample was removed, filtered through a syringe filter and analysed by HPLC for MSU content. Results given are always the average of two vials.
Confirmation of Similar Trends at Room Temperature vs 37°C
Some vial-based solubility assessments were run following the same method as described above, but stirring at 37°C in a water bath overnight instead of room temperature.
Results
Drug Permeation
Overall, the permeation of ibuprofen through the skin was around 10 to 15 times higher than diclofenac (Figures 1 and 2). Amounts of ibuprofen delivered ranged from 549µg to 2963µg and amounts of diclofenac delivered ranged from 64µg to 220µg, through full thickness pig’s ear skin after 72 hours at room temperature.
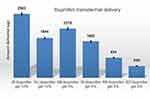 |
Figure 1 Permeation of ibuprofen through pig’s skin. |
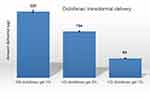 |
Figure 2 Permeation of diclofenac through pig’s skin. |
Ibuprofen Permeation
For the 5% ibuprofen containing gels, the amount delivered through the skin ranged from 2278µg (GB ibuprofen gel 5%) to 549µg (BO ibuprofen gel 5%) (Figure 1). The 10% ibuprofen containing gels generally delivered more ibuprofen through the skin, delivering 2963µg (IB ibuprofen gel 10%) and 1844µg (NU ibuprofen gel 10%).
The two IB gels have similar formulations (except that IB ibuprofen gel 10% omits propylene glycol), and the NU ibuprofen gel 10% has a similar formulation to the RB ibuprofen gel 5% (identical ingredients). IB ibuprofen gel 10% delivered ~60% more ibuprofen through the skin than NU ibuprofen gel 10%. IB ibuprofen gel 5% delivered ~80% more ibuprofen through the skin than RB ibuprofen gel 5%.
IB ibuprofen gel 10% delivered ~75% more ibuprofen through the skin than the IB ibuprofen gel 5%. NU ibuprofen gel 10% delivered ~100% more ibuprofen through the skin than RB ibuprofen gel 5%.
GB ibuprofen gel 5% delivered an amount of ibuprofen through the skin (2278µg) that was intermediate between the two 10% gels (2963µg and 1844µg).
Diclofenac Permeation Results
The amount of diclofenac delivered through the skin ranged from 220µg (GB diclofenac gel 1%) to 64µg (VO diclofenac gel 1%) (Figure 2). The VO diclofenac gel 2% delivered ~140% more diclofenac through the skin than the VO diclofenac gel 1%. The VO products have similar formulations, with the VO diclofenac gel 2% having one extra ingredient (oleyl alcohol).
GB diclofenac gel 1% delivers ~240% more diclofenac through the skin than VO diclofenac gel 1%, and ~40% more than the VO diclofenac gel 2%.
Monosodium Urate (MSU) Solubility Results
Franz-Cell Solubility Experiments
The saturated solubility of MSU was measured in the PBS media in the receptor cells of Franz cells. Pig’s skin was used as the membrane between the donor and receptor cells. The 10 products and control (PBS) were added to the donor cells ensuring complete coverage of the exposed membrane. Samples were taken after 72 hours. Results are given as percentages with respect to the control for each experiment and are shown in Figure 3.
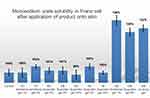 |
Figure 3 Solubility of monosodium urate (MSU) in phosphate buffered saline (PBS) in the receptor cell of a Franz cell after application of the product onto the pig’s skin membrane. |
The seven commercial products all showed MSU solubilities in a similar range to the control, between 99% and 103%. VO diclofenac gel 2% and IB ibuprofen gel 5% gave the highest solubilities (103%) and NU ibuprofen gel 10% gave the lowest solubility (99%).
The three “GB” products all gave significant increase in the solubility of MSU, ranging from 120% (GB ibuprofen gel 5%) to 126% (GB diclofenac gel 1%). The “GB no drug gel” product showed an increase in solubility to 122%.
Vial-Based Solubility Experiments
The saturated solubility of MSU in PBS (5mL) was determined in vials with the direct addition of some extra materials (Table 1). All percentage values are relative to the control PBS solubility at that temperature.
 |
Table 1 Saturated Solubility of Monosodium Urate (MSU) in PBS in Vials After 24 Hours |
Addition of 50mg (1% w/w) of sodium carbonate at 25°C gave an increase in solubility to 276% and also increased the pH to 11.3 (overriding the buffering capability). When the pH was re-adjusted back to the physiological range (around pH 7.4) the solubility dropped to 83%. Addition of 50mg (1% w/w) of sodium bicarbonate at 25°C gave a solubility of 66% and the pH was increased to 8.3. When the pH was re-adjusted back to the physiological range (around pH 7.4) at 25°C the solubility dropped to 65%. Addition of 50mg (1% w/w) of sodium bicarbonate at 37°C gave a solubility of 52% and the pH was increased to 8.3.
Addition of 50µL of “GB no drug gel” at 25°C increased the solubility to 123%. Carrying out the same experiment at 37°C gave a solubility of 171% (relative to the control at 37°C). Addition of 50µL of GB diclofenac gel 1% at 25°C increased the solubility to 123%. Carrying out the same experiment at 37°C gave a solubility of 160% (relative to the control at 37°C).
Discussion
Ibuprofen versus Diclofenac Permeation
The ibuprofen products delivered significantly more drug through the skin than the diclofenac products. This is partly due to the higher concentrations of ibuprofen present (5% and 10% ibuprofen vs 1% and 2% diclofenac). The levels of drug in these products are probably limited mostly by the solubility of the salts – ibuprofen salts are considerably more soluble than diclofenac salts. However, the 5-fold increase in drug concentration probably does not account for all of the extra permeability of ibuprofen (ibuprofen levels were around 10–15 times higher than diclofenac). Other factors such as lower molecular weight and higher hydrophilicity of ibuprofen also probably contribute to the higher permeability.
The observed faster permeability of ibuprofen agrees with previously observed results.7,8 In a recent paper by Pradal,7 it is suggested that the higher potency of diclofenac would result in a significantly higher values of “modified index of anti-inflammatory activity” for the diclofenac products in-spite of the lower permeation rates versus ibuprofen (around 10 fold increase for diclofenac). However, another recent paper by Wade et al14 compared 1% diclofenac gel with 5% ibuprofen gel and 5% ibuprofen/3% menthol gel in a clinical trial. In this trial there is only a small improvement in delivered pain relief for the diclofenac product over the ibuprofen gel. As the predicted significant improvement for diclofenac was not observed in the clinical trial, it raises the question of whether any of the products are delivering enough drug to allow the difference to be observed.
Ibuprofen Permeation
The six different ibuprofen products showed significantly different permeability of ibuprofen, with the highest amount delivered being 5.5 times higher than the lowest. The concentration of ibuprofen within the gels played a significant role in the permeability. The two IB products had similar formulations, and IB ibuprofen gel 10% gave 75% higher permeation than IB ibuprofen gel 5%. NU ibuprofen gel 10% has a similar formulation to RB ibuprofen gel 5% and NU ibuprofen gel 10% showed a 100% increase in permeation versus RB ibuprofen gel 5%. Thus, doubling the concentration of ibuprofen does almost double the amount delivered for similar formulations.
There was a significant difference in ibuprofen delivery through the skin for products with the same concentration of drug. For the 5% products, the highest permeating product (GB ibuprofen gel 5%) delivered ~4 times more ibuprofen than the lowest permeating product (BO ibuprofen gel 5%). A similar effect was observed in the 10% products, with the IB ibuprofen gel 10% delivering ~60% more ibuprofen than the NU ibuprofen gel 10%. A similar difference was observed in the Pradal study,7 where the 10% ibuprofen gel with similar formulation to IB ibuprofen gel 10% delivered 64% more ibuprofen through the human skin than the 10% formulation similar to NU ibuprofen gel 10%. As the drug and concentrations are identical in the above examples, this difference must be attributed to the formulation used. This includes the salt form and the excipients in the gel. It is likely that the improved permeation is a combination of various factors. For example, the more “hard” polar sodium salt in RB ibuprofen gel 5% shows intermediate permeability between the “softer” less-polar diisopropanolamine salt (in BO ibuprofen gel 5%) and the diethylamine and trolamine salts in IB ibuprofen gel 5% and GB ibuprofen gel 5%. So it is difficult to generalise about which type of salt will be best. Each formulation contains potential penetration enhancers such as ethanol, propylene glycol, benzyl alcohol, oleic acid, transcutol, etc. The exact quantities of each ingredient are not known, and each component is not varied independently, so the best conclusion is to state that the formulation can have a significant effect on permeation and it is likely that the various factors work together to influence the outcome. The best 5% formulation is comparable with the 10% products, so formulation can exert a significant influence on permeation.
Diclofenac Permeation
Three different diclofenac products were tested. VO diclofenac gel 2% showed better permeation than VO diclofenac gel 1%, but the increase was only 40% even with added oleyl alcohol as a penetration enhancer. This suggests that drug concentration alone is not the only limiting factor of amount of drug delivered transdermally for the VO formulations. GB diclofenac gel 1% showed better permeation than both 1% and 2% VO products. This is presumably due to the nature and balance of the formulation ingredients and different salt form used (trolamine rather than diethylamine). The formulation can have a strong influence on permeation for topical diclofenac products.
Increased NSAID Permeation is Desirable for Topical Products
It is often the case that the amount of drug delivered via topical products into the body is significantly lower than via oral administration. This can be illustrated with regard to ibuprofen. Oral ibuprofen is recommended at 400mg per dose (adult) and 1200mg per day, and it has ~97–100% bioavailability,9,10 so around 390–400mg ibuprofen is delivered to the body per dose. Normal recommended application (dose) of topical ibuprofen products is 2–10cm ribbon of gel which equates in total 50–125mg of ibuprofen, but bioavailability is around 22% maximum,13 ie, ~11–30mg delivered per dose. Transdermal ibuprofen delivery is still very low overall versus oral delivery. There are significant advantages in topical delivery in avoiding unwanted side effects in the stomach/intestines, and potentially delivering the drug in a targeted manner. However, as the pain and inflammation associated with arthritis such as gout is generated relatively deep beyond the skin, we should be maximising the penetration/permeability of the NSAIDs to deliver a significant amount to the joints and other affected areas.15–17
Effect on Monosodium Urate Solubility in Franz Cells
The immediate cause of gout is precipitation of crystals of monosodium urate (MSU) within joints. These crystals are often in the synovial fluid and surrounding tissues. A study by Kippen in 1974 showed that phosphate buffered saline (PBS) is a good laboratory substitute for testing the solubility of MSU.3 In our study, we have examined the effect of various topical products on the saturated solubility of MSU “under the skin” after the products had been applied transdermally to pig’s skin on Franz cell apparatus. This is an in vitro model to imitate the effect of applying the products onto the skin of an affected joint.
All the commercially available products showed just a small effect on the saturated MSU solubility, with values ranging from 99% to 103% of the control saturated solubility. This suggests that the components of the commercial products that permeate through the skin have little effect on the solubility of MSU.
The three GB products all had a consistent and significant effect, with the saturated solubility increasing to 120–126%. The formulations are very similar, with the difference being either no drug, or added ibuprofen or diclofenac. As the diclofenac product showed the highest improvement in solubility, diclofenac may have a small positive effect on the MSU solubility. However, most of the solubility increase is due to the formulation of the GB products, with the drug-free product still giving a significant increase in solubility (to 122%). Presumably, some of the components of the formulation can act as “co-solvents” for MSU in PBS after permeating through the skin. This exerts a physical effect of helping the solid crystals dissolve. In terms of helping gout, this would not directly resolve the inflammation, but could support the body’s normal function in removing the excess urate from the synovial cavity and surrounding areas.
Vial-Based Solubility of Monosodium Urate (MSU)
The sodium salts of diclofenac and ibuprofen have been commonly used in topical products. However, in the early paper by Kippen,3 it was shown that increased NaCl concentration will lower the solubility of MSU. This can be attributed to the “common ion effect” where increasing the concentration of the shared ion (sodium) will affect the solubility of the second salt. This was further investigated by adding sodium bicarbonate to a saturated suspension of MSU in PBS. When the pH was kept at around pH 7, the solubility of MSU was reduced to 65% of the control. When the pH is allowed to shift to pH 8.3, the solubility is reduced to 66%. Kippen also describes the effect of pH on solubility.3 Small changes in pH (eg, to around pH 8) can actually decrease the MSU solubility, whereas increasing the pH above pH 10 will significantly increase MSU solubility, as was observed with addition of excess sodium carbonate shifting the pH to 11.3.
These results suggest that any increase in sodium concentration at physiological pH (around pH 7) will reduce MSU solubility, which could lead to more crystals being formed in vivo.
The Kippen study also shows that factors that affect MSU solubility at 26°C have similar solubility trends at 37°C (such as pH, sodium ion concentration and addition of albumin).3 This is the basis of suggesting that improvements in solubility (and permeability) observed in this study at room temperature (20–25°C) will correlate with similar improvements at 37°C (ie, in vivo). This was confirmed in the vial solubility experiments, where improvements in MSU solubilities observed for GB no drug gel and GB diclofenac gel 1% at 25°C were also shown at 37°C – the improvements in MSU solubility were actually greater at 37°C. The reduction in MSU solubility due to adding extra sodium (bicarbonate) was also observed at 37°C (similar to at 25°C).
Comments on the Experimental Protocols Used
This study was aiming to investigate the overall differences in efficacy of the products for treating gout, which occurs mostly in joints. This means that the effects would have to be transdermal, not just within the skin. Full thickness pig’s skin was therefore used to best imitate the permeation towards the joint/synovial cavity. This leads to significant variability in the skin samples used, and variability in the repeated results. In general, variability of up to ± 5% was observed in the Franz cell experiments. However, this also imitates the variability in human skin, and the differences observed for MSU solubility were greater than 20% and more than 40% difference for drug permeation. So whilst the absolute rates of diffusion and changes in solubility values may not be fully accurate, the trends and differences are greater than the inherent variability in the experiments and there are sufficient data to show comparative efficacy between the products tested. The experiments are just lab-based models, but it is a fair suggestion that a product that performs better in these tests has a good chance to perform better in vivo.
Note: the MSU crystals used were tested by X-ray powder diffraction to confirm that they were the same polymorphic form as those isolated from ex vivo synovial fluid samples (monosodium urate monohydrate).18
Conclusions
Topical NSAIDs such as ibuprofen and diclofenac do not address the cause of gout, but aim to reduce the pain and inflammation that are common symptoms.1 These symptoms can be significantly debilitating and very painful,19 so it is important to have the most effective delivery of the NSAID drugs to the affected regions. This suggests that the highest permeation available would be best, as the current levels of delivery are significantly lower than the standard accepted oral doses.9,10,15 Better penetration of the NSAID drugs will lead to faster pain and inflammation relief, and better patient outcomes. This can be achieved with well-optimised formulations, such as Gout Buster Ibuprofen/Diclofenac gels.
The Gout Buster gels have shown good potential to improve the solubility of the MSU crystals that are the immediate trigger for gout. Improved MSU solubility would support the normal functioning of the body to remove the unwanted crystals by assisting the physical dissolution of crystals. The body should then function more effectively in flushing out the excess urate in the synovial fluids and blood via its normal processes.20 Helping MSU crystals to re-dissolve, however, is not a treatment for the underlying cause of gout – the hyperuricemia.
Topical formulations containing sodium should be avoided as this may increase sodium concentration in the affected areas which has been shown to decrease MSU solubility (in this study and in previous publications)3 and could make gout attacks more frequent.
Acknowledgments
The author gratefully acknowledges Gattefosse (Saint-Priest, France) for supplying samples of excipients used in this research including Transcutol P.
Disclosure
Mark W Hooper is Founder and CEO of MedCryst Therapeutics and has developed the Gout Buster products under patent WO2019116045A1 (Dissolution of monosodium urate to treat gout). Liang He is affiliated to PharmHe. The authors report no other conflicts of interest in this work.
References
1. Dalbeth N, Choi HK, Joosten LAB, et al. Gout primer. Nat Rev. 2019;5:69. doi:10.1038/s41572-019-0115-y
2. Seegmiller JE. The acute attack of gouty arthritis. Arthr Rheum. 1965;8:714–725. doi:10.1002/art.1780080431
3. Kippen I, Klinenberg JR, Weinberger A, Wilcox WR. Factors affecting urate solubility in vitro. Ann Rheum Dis. 1974;33:313. doi:10.1136/ard.33.4.313
4. Heyneman CA, Lawless-Liday C, Wall GC. Oral versus topical NSAIDs in rheumatic diseases. Drugs. 2000;60(3):555–574. doi:10.2165/00003495-200060030-00004
5. Tiwari S, Dwivedi H, Kymonil K, Saraf S. Urate crystal degradation for treatment of gout: a nanoparticulate combination therapy approach. Drug Deliv Transl Res. 2015;5(3):219–230. doi:10.1007/s13346-015-0219-1
6. Bou-Salah L, Benarous K, Linani A, et al. Anti-inflammatory drugs as new inhibitors to xanthine oxidase: in vitro and in silico approach. Mol Cell Probes. 2021;58:101733. doi:10.1016/j.mcp.2021.101733
7. Pradal J. Comparison of skin permeation and putative anti-inflammatory activity of commercially available topical products containing ibuprofen and diclofenac. J Pain Res. 2020;Volume 13:2805–2814. doi:10.2147/JPR.S262390
8. Pennick G, Robinson-Miller A, Cush I. Topical NSAIDs for acute local pain relief: in vitro characterization of drug delivery profiles into and through human skin. Drug Dev Industr Pharma. 2021;47(6):908–918. doi:10.1080/03639045.2021.1935996
9. Hattrem MN, Dille MJ, Seternes T, Ege T, Draget KI. The relative bioavailability of ibuprofen after administration with a novel soft chewable drug formulation. Clin Pharmacol Drug Dev. 2018;7(2):168–176. doi:10.1002/cpdd.357
10. Atkinson HC, Stanescu I, Frampton C, Salem II, Beasley CPH, Robson R. Pharmacokinetics and bioavailability of a fixed-dose combination of ibuprofen and paracetamol after intravenous and oral administration. Clin Drug Investig. 2015;35:625–632. doi:10.1007/s40261-015-0320-8
11. Flatena GE, Palacb Z, Engeslanda A, Filipovic-Grcic J, Vanic Z, Škalko-Basnet N. In vitro skin models as a tool in optimization of drug formulation. Eur J Pharma Sci. 2015;75:10–24. doi:10.1016/j.ejps.2015.02.018
12. Ng SF, Rouse JJ, Sanderson FD, Meidan V, Eccleston GM. Validation of a static Franz diffusion cell system for in vitro permeation studies. AAPS PharmSciTech. 2010;11(3):1432–1441. doi:10.1208/s12249-010-9522-9
13. Pascual E, Sivera F. Time required for disappearance of urate crystals from synovial fluid after successful hypouricaemic treatment relates to the duration of gout. Ann Rheum Dis. 2007;66:1056–1058. doi:10.1136/ard.2006.060368
14. Wade AG, Crawford GM, Young D, Corson S, Brown C. Comparison of diclofenac gel, ibuprofen gel, and ibuprofen gel with levomenthol for the topical treatment of pain associated with musculoskeletal injuries. J Int Med Res. 2019;47(9):4454–4468. doi:10.1177/0300060519859146
15. Kleinbloesem CH, Ouwerkerk M, Spitznagel W, Wilkinson FE, Kaiser RR. Pharmacokinetics and bioavailability of percutaneous ibuprofen. Arzneimittelforschung. 1995;45(10):1117–1121.
16. Lee CM, Maibach HI. Deep percutaneous penetration into muscles and joints. J Pharm Sci. 2006;95(7):1405. doi:10.1002/jps.20666
17. Alexander A, Dwivedi S, Ajazuddin GTK, Saraf S, Saraf S, Tripathi DK. Approaches for breaking the barriers of drug permeation through transdermal drug delivery. J Control Release. 2012;164:26–40. doi:10.1016/j.jconrel.2012.09.017
18. Howell RR, Eanes ED, Seegmiller JE. X‐ray diffraction studies of the tophaceous deposits in gout. Arthritis Rheum. 1963;6(2):97–103. doi:10.1002/art.1780060202
19. Gout: Causes, symptoms, treatments. Versus Arthritis. Website information. 2022 Available from: www.versusarthritis.org/about-arthritis/conditions/gout.
20. Simkin PA. Synovial perfusion and synovial fluid solutes. Ann Rheum Dis. 1995;54:424–428. doi:10.1136/ard.54.5.424
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
