Back to Journals » Psychology Research and Behavior Management » Volume 10
Testing domains of the healing experiences in all life stressors questionnaire in a cohort of HIV-infected and HIV-uninfected Chicago women
Authors Mistretta EG, Sloan D, BrintzenhofeSzoc K, Weber KM, Berger A
Received 13 December 2016
Accepted for publication 12 April 2017
Published 4 July 2017 Volume 2017:10 Pages 201—208
DOI https://doi.org/10.2147/PRBM.S129566
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Igor Elman
Erin G Mistretta,1,2 Danetta Sloan,1 Karlynn BrintzenhofeSzoc,3 Kathleen M Weber,4 Ann Berger1
1Pain and Palliative Care Service, National Institutes of Health, Bethesda, MD, 2Department of Psychology, Catholic University of America, Washington, DC, 3School of Social Work, College of Allied Health Sciences, University of Cincinnati, Cincinnati, OH, 4HIV Research, Hektoen Institute of Medicine/Cook County Health and Hospitals System, Chicago, IL, USA
Purpose: Patients may deal with issues of spiritual and religious meaning when coping with life-threatening or chronic illness. Researchers at the National Institutes of Health have developed the healing experiences in all life stressors (HEALS) questionnaire, an assessment to determine psychosocial spiritual adjustment to healing. Many measures assess religious and spiritual behavior, but there exists a need to capture the meaning of these factors in the process of healing. The instrument consists of spirituality, religion, interpersonal, and intrapersonal domains. This study explores the preliminary partial validation of the spirituality and religion domains of the HEALS against the Ironson–Woods Spirituality and Religiousness Index (IWSR).
Methods: The abbreviated HEALS, IWSR, and a measure of depression were completed by 205 human immunodeficiency virus (HIV)-infected and HIV-uninfected women from Chicago as part of the Women’s Interagency HIV Study. Total scores on the HEALS and IWSR were correlated using Pearson correlations to examine convergent validity. Total depression scores were analyzed with Pearson correlations to investigate criterion validity.
Results: Responses between the abbreviated HEALS and IWSR were highly correlated (r=0.74). Similar to other measures of its kind, scores on the HEALS were associated with depressive symptoms. Women with clinically significant depressive symptoms scored significantly lower on the HEALS than women without. No significant differences were found for race, age, education, or HIV status.
Conclusion: This study is an important step in the future validation of the HEALS. Results suggest that the spirituality and religion domains of the HEALS have good construct validity with the IWSR. After further validation, this measure may provide clinicians and researchers with a unique way to assess psychosocial spiritual healing.
Keywords: HIV, spirituality, healing, construct validity, life-threatening illness
Introduction
Spirituality is defined as attributing meaning and purpose to one’s life. This could derive from belief in a higher power or inter/intrapersonal connection.1 Religion refers to the extent that people observe the beliefs and rituals of a particular religion, which can be considered under the larger construct of spirituality.2 Individuals dealing with life-threatening and chronic illness often question spiritual and existential meaning.3 Regardless of patients’ desire to discuss spirituality with their physicians,4 it is not a common practice. An emphasis on how spirituality influences healing and how to measure these concepts is a necessary step toward patient-centered care.
Holistic healing encompasses the balancing of psychological, social, and spiritual dimensions. This broad definition means that even when the physical body is suffering, there is still potential for healing.5 Allopathic medicine tends to confine healing to the physical, but patients with life-threatening and chronic illness often desire emotional and spiritual healing as well.6
The importance of spirituality and religion in the context of healing the physical, emotional, and social realms is well documented. Spirituality and religiosity are associated with better physical and emotional health in studies of cancer patients.7,8 In chronic illnesses such as human immunodeficiency virus (HIV), spiritual adjustment has been shown to improve health-related quality of life,9,10 immune status,11 risk behavior,12 and sleep quality.13 The increase in research examining the benefits of spirituality on disease progression and well-being has led to the development of several instruments to capture the aspects of spirituality and religiousness. These include the Ironson–Woods Spirituality and Religiousness Index (IWSR),14 the Brief Multidimensional Measure of Religiousness/Spirituality,15 the Functional Assessment of Chronic Illness Therapy – Spirituality Scale,16 the Duke Religion Index,17 and the Brief Religious Coping Activity Scale.18
The goal of these self-report measures is to assist health care workers in identifying the significance of religion and spirituality in a person’s life. In the health field, the concepts of religion and spirituality have been examined through questions of religious behavior such as how often people attend religious activities or the frequency of personal spiritual practices.19 The usefulness of answers to such questions in the context of healing is debatable because the act of attending religious services often requires a certain state of physical health to begin with and because social support associated with religious activity can be a confounding factor when examining the effect of religious involvement on health.20 Some instruments focus on religious motivation/orientation such as Allport’s distinction between extrinsic and intrinsic orientations,21 which can help to identify the aspects of religiousness. These methods, however, have been criticized for being culturally constrained and not relevant to the larger construct of spirituality.19,22 In this regard, religiousness and spirituality are often conceptualized as unique albeit overlapping constructs.22 To determine how spirituality facilitates healing in the lives of people with chronic and life-threatening illness, questions that probe for such things as the meaning and purpose in one’s life are needed.
Instruments assessing spirituality and general health tend to neglect the meaning of spirituality in the context of healing from a life-threatening and chronic illness. Although many studies have used spirituality instruments in palliative care settings, a systematic review of such measures found that over half (n=30) of measures reported in research studies had not been validated in a palliative and/or chronic illness population.23 This is an important consideration as palliative and chronically ill patients have unique spiritual needs such as finding purpose through religion, relationships, occupation, and self.6,24 In addition, there is a paucity of measures considered to be culturally inclusive.23
Lewis25 conducted a systematic review of spirituality instruments and found that those used in the health field were not culturally appropriate for the African American population either because African Americans were not adequately represented in studies of instrument development and testing or they did not include constructs of African American spirituality such as faith in a higher power; personal relationships with a higher power, self, and others; and providing a transforming experience. A qualitative study examining the constructs of spirituality, specifically in African American women with HIV, defined spirituality in terms of a process/journey or connection; spiritual expressions such as church attendance, prayer, and being thankful; and spiritual benefits such as being healed or finding inner strength.1 Achieving a balance between cultural representativeness and generalizability can be challenging, but literature that reveals distinct differences in patient definitions of spirituality suggests that this endeavor should be pursued.19,23,26–29
Rationale for the current study
In an effort to identify the factors that promote healing and facilitate meaningful conversation between patient and physician, the National Institutes of Health (NIH) Pain and Palliative Care Service developed an instrument of psychosocial spiritual healing: the healing experience in all life stressors (HEALS) questionnaire. The items in the questionnaire were derived from qualitative interviews asking patients about their experience of healing and the meaning of spirituality in their lives, and through palliative care providers’ observations of those with chronic and/or life-threatening illness.30
As the second in a series of three papers, this study seeks to test the spirituality and religion domain items of the HEALS (abbreviated HEALS) against the IWSR14 in a convenience sample of HIV-infected and demographically similar uninfected women participating in the Chicago site of the NIH funded Women’s Interagency HIV Study (WIHS). The WIHS is an ongoing longitudinal cohort study of the natural and treated history of HIV in women initiated in 1994.31,32 Correlations between the HEALS and the Center for Epidemiological Studies-Depression Scale (CES-D)33 were also of interest due to similar associations between the measures of depression and other validated measures of spirituality and religion in comparable populations.14,16,20,34 Of tertiary interest, the associations between scores on the HEALS and demographic variables of HIV-infected and HIV-uninfected women were assessed to see how the HEALS performed in a population who may have a chronic illness and those who may not. Although the HEALS is still undergoing testing for validity, we feel that this data provide useful information about the development of a new tool assessing psychosocial spiritual adjustment to healing in those with life-threatening and chronic illness.
Methods
Participants
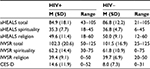
Participants were 205 (142 HIV infected and 63 uninfected) women enrolled in the Chicago WIHS who had a study visit for other purposes at the Cook County Health and Hospital Systems/Hektoen Institute of Medicine site between July and November of 2015. Women were predominantly African American (78%), with a mean age of 48.9 years (range 31–73 years). About 30% of the women had not completed high school, 30% had completed high school, and around 30% had attended some years of college. Religion was not a question asked for the WIHS study. As this study was using secondary data, religion, although potentially an important variable, could not be included in the analysis. This study was reviewed and approved by Johns Hopkins Bloomberg School of Public Health through the WIHS parent study. It was also approved by Cook County Health and Hospital Systems, and the Office of Human Subjects Research Protection at the National Institutes of Health Clinical Center. Demographics are shown in Table 1.
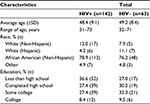  | Table 1 Demographics by HIV status Abbreviation: HIV, human immunodeficiency virus. |
Procedure
Women were invited and verbally consented to complete the abbreviated HEALS questionnaire and the IWSR index during their wait time for other WIHS study visits. Questionnaires were interview administered to women with low reading/literacy levels. Sociodemographic, CES-D, and other data were collected and extracted from the WIHS study visit closest to the spirituality assessments.
Measures
HEALS (formally known as the NIH spirituality and coping assessment)
The full HEALS is a 54-item self-report measure assessing psychosocial spiritual healing in people with chronic or life-threatening illness, and uses 5-point Likert scales ranging from 1 (strongly disagree) to 5 (strongly agree). In this study, we used the abbreviated HEALS, a 21-item self-report measure with the same response set. Participants are asked to consider the past 30 days when answering questions. Domain items included in this study are listed in Table 2.
  | Table 2 Items on the spirituality and religion domains of the abbreviated HEALS Abbreviation: HEALS, healing experiences in all life stressors. |
The most recent preliminary factor analysis of the full HEALS categorized four domains: spirituality, religion, interpersonal, and intrapersonal factors.30 In this study, the entire religion domain and select items of the spirituality domain were included in the abbreviated scale. In the spirituality domain, items were selected to be included based on those representing intrinsic aspects of spirituality.22 Items that probe about spiritual fulfillment through connections between nature, arts, relationships, and self were kept, whereas those asking for how such connections sustain one’s other needs such as feeling less stressed or being more positive were excluded. Scores ranged from 21 to 105 with higher scores indicating greater psychosocial spiritual adjustment to healing.
Spirituality for this study is conceptually defined as an individual’s sense of meaning through outward interactions (e.g., “Connecting with the peace in nature gives my life meaning”; “I have a heightened sense of gratitude”). The full spirituality domain consists of 16 items, 9 of which were included in the abbreviated spirituality scale used with this study sample. On the basis of the preliminary factor analysis with all questions, the spirituality factor demonstrated good reliability with a Cronbach’s a=0.87.35
Religion for this study is conceptually defined as an individual’s connection with a religious community and belief in a higher power (e.g., “My situation strengthened my connection to a higher power”; “My participation in a religious community is an important aspect of my life”). This domain consists of 12 items, all of which were included in the questionnaire administered to the WIHS sample. On the basis of the preliminary factor analysis using orthogonal varimax rotation with all questions, this factor showed excellent reliability with a Cronbach’s a=0.97. This high α suggests that there may be too many items. This will be addressed in the next study when confirmatory analysis will be conducted.35
Ironson–woods spirituality and religiousness index
The IWSR index14 is a 25-item questionnaire adapted from the 89-item long form.36 The scale measures what people mean when they say they are religious or spiritual and also assesses public and private religious behavior using a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The instrument has a four-factor structure of religion and spirituality: sense of peace, faith in god, religious behavior, and compassionate view of others. The domains sense of peace and compassionate view of others address aspects of spirituality, whereas the domains faith in god and religious behavior address aspects of religion. Scores range from 25 to 125 with higher scores indicating that someone is more spiritual/religious. The measure is reported to have good convergent and discriminant validity as well as excellent reliability with the Cronbach’s a=0.96.14
Center for epidemiological studies-depression scale
The CES-D33 is a 20-item scale measuring depressive symptoms within the past week with participants reporting whether symptoms occur rarely, some of the time, occasionally, or most of the time. Scores range from 0 to 60, with higher scores indicative of greater depressive symptoms. A score of 16 or higher indicates clinically significant depressive symptoms. The measure has good reliability with Cronbach’s a=0.88, and good test–retest reliability being r=0.87.37 The measure is reported to have good convergent and discriminant validity.37,38
Analysis
Analysis of variances (ANOVAs) and Pearson product-moment correlations were performed to evaluate if the HIV-infected and HIV-uninfected women were similar or different on the demographic characteristics. To assess the religion and spirituality domain items of the HEALS against the IWSR, Pearson product-moment correlations were utilized. Both the total HEALS and the total IWSR and the spirituality and religion domain items of both the HEALS and the IWSR were included. Regressions, one-way ANOVAs, and independent samples t-tests were performed to assess associations between scores on the HEALS and sociodemographic and clinical variables of the sample including race, education, age, HIV status, and CES-D data.
Results
Sample characterization
Descriptive statistics are listed in Table 1. Race, education, and age were similar across HIV status groups. As the primary aim of this analysis is the preliminary validation of the HEALS religion and spirituality domain items rather than HIV status differences, and scores were similar across HIV status groups, HIV-infected and HIV-uninfected women were included together in the analyses. For thoroughness, however, data from HIV-infected and HIV-uninfected women were also analyzed separately.
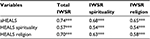
Table 3 presents the mean scores, SDs, and the ranges for the abbreviated HEALS (aHEALS) and its two domains, the IWSR and its two domains, and the CES-D. There are no significant differences between the aHEALS total and IWSR total or between the two aHEALS domains and the IWSR domains. The depression scores measured by the CES-D were statistically different (t(177.6)=−4.78, p<0.001). The participants who were HIV positive had higher mean depression scores than did the HIV-negative participants. Looking at the CES-D cut-off scores, 38% of those who were HIV positive had clinically significant depressive symptom scores, whereas 14.8% of those who were HIV negative had clinically significant depressive symptom scores.
Convergent validity between HEALS and IWSR
Pearson product-moment correlations were computed between the total HEALS and the total IWSR (r=0.74) and between the spirituality (r=0.54) and religion (r=0.58) domain items of both the HEALS and the IWSR. Results provide additional support with these moderate-to-high correlations of the validity of the HEALS (Table 4).
Associations between HEALS and CES-D
Associations between scores on the HEALS and scores on the CES-D were analyzed due to the fact that the IWSR and other measures of religion and spirituality have shown to be correlated with measures of depression as well as perceived stress, anxiety, and hopelessness.14 A significant but weak negative correlation was found (r=0.14; p=0.044). This suggests that those with a higher CES-D score are more likely to report lower scores on the aHEALS. The CES-D explains 2% of the variance in the aHEALS total score.
Associations between HEALS and demographic variables
No associations were found between the demographic variables, HIV status, and the combined total score of the spirituality and religion domain items of the aHEALS or the IWSR.
Literature indicates that African American women value spirituality as a factor in healing more than women of other races.2 Research also finds that some people diagnosed with HIV equate religion with spirituality, while others say they are distinct factors.39 To elucidate these differences between religion and spirituality, we analyzed the two domains separately to see whether there were differences in scores between women of different races. Only participants who self-reported race as African American, White, and Hispanic were included due to the small number of the other four races. A one-way ANOVA comparing scores on the religion domain items of the HEALS between women of different races (Table 1) revealed that their means were significantly different, F(2, 190)=3.18, p=0.001. Post hoc Scheffe test revealed only a marginally significant difference between African American (M=51.22) and White women (M=42.81, p=0.001). There were no significant differences between races on the spirituality domain of the aHEALS. There was a statistically significant difference between races on the spirituality domain of the IWSR, F(2, 192)=3.16, p=0.045, although the post hoc Scheffe was only trending toward significance (p=0.065). The mean spirituality score for African American women was 63.58, whereas for White women it was 56.41. There were no significant differences by race on the religion domain of the IWSR.
Discussion
This research contributes to the field of palliative care by providing information on the preliminary validation of a novel tool to measure psychosocial spiritual aspects of healing in those with life-threatening or chronic illness. First, the religion and spirituality domain items of the abbreviated HEALS were significantly correlated with scores on the IWSR, a validated measure of religiousness and spirituality. Second, the demographic and clinical variables of race, education, age, and HIV status were not related to the scores on the HEALS. However, women with clinically significant depressive symptoms scored significantly lower on the HEALS than women without clinically significant depressive symptoms.
The significant correlation between the spirituality and religion domain items of the HEALS and the IWSR suggests that these factors are measuring what they are intended to measure. This is an essential criterion in the construct validity of a new instrument. Although the correlation of 0.74 is adequate, it is likely not good or excellent due to unique distinctions between the HEALS and the IWSR such as the lack of questions related to religious behaviors in the HEALS and a greater emphasis on how people attribute meaning and purpose of life in the midst of dealing with life-threatening or chronic illness. These measures can provide clinicians with a more holistic understanding of patients’ psychosocial functioning and capacity for spiritual healing.
The HEALS was significantly associated with scores on the CES-D, showing that lower HEALS scores were significantly related to higher scores on the depression measure, CES-D. This finding complements not only literature from other studies examining women diagnosed with HIV9,40 but also with other validated measures of religion and spirituality.14 This corroboration is promising for the subsequent validation of the HEALS.
The spirituality and religion domains of the HEALS were not significantly related to any demographic or clinical variables explored in this analysis. The finding that HIV status was not related to scores on the HEALS or the IWSR was not entirely unexpected. HIV-infected women may fare better than HIV-uninfected women with similarly low socioeconomic status and HIV risk behaviors who continue to struggle with access to quality healthcare including mental health services and housing support. So while HIV-uninfected women may not be prompted to address life meaning in the same way that HIV-infected women do as a result of their chronic disease, HIV-uninfected women living in poverty continue to endure other life struggles that may stimulate greater religiousness and spirituality as a coping strategy. Once diagnosed, women living with HIV receive access to psychosocial, mental health, and medical resources that were not available prior to their diagnosis. Therefore, because the women living with HIV have access to these resources, it could have provided them with better ways to cope compared with the HIV-uninfected women living in poverty. At present, no studies have identified differences in spiritual adjustment to healing between HIV-infected and HIV-uninfected women. This finding may also be due to the large African American sample. As the literature reports, about 88% of African Americans report religious affiliation with a formal community, whereas 72% indicate that religion holds a significant role in their lives despite not being affiliated with any formal religion.41 Racial characteristics across HIV status groups were similar, so it is possible that even WIHS women who were not diagnosed with a chronic disease such as HIV still held strong spiritual/religious beliefs due to the majority of the sample being African American. The finding that age and education were not related to scores on the HEALS or the IWSR is consistent with other literature assessing variables of religion and spirituality.10,42,43
When viewed separately, the religion domain revealed higher scores among African American women than White women. This is worth exploring in a larger sample to determine whether African American women may incorporate religiousness in their healing more than White women. This complements research which indicates that African American women with HIV value religion in the context of healing.1,9–12 However, this difference was not significant for the IWSR. One reason for this may be the differences in scale items. Looking at both instruments, the HEALS considers additional dimensions of religion and spirituality including the meaning of religion and spirituality in one’s life. The IWSR religion domain asks questions related to religious behaviors and faith. Although these factors have been shown to be predictive of health outcomes in HIV-infected women, there is less emphasis in the IWSR on explaining what the underlying meaning is in engaging in these practices. Without an understanding of the meaning of religion and faith, it can be difficult to account for the significance of these practices in the context of healing in general and healing across specific domains. The HEALS was developed to fill this gap and to more thoroughly address the overall meaning of spirituality in the context of healing from a chronic illness. These themes are supported in qualitative literature and could be captured with a quantitative measure such as the abbreviated HEALS that is easy to collect and score.
Limitations
These findings should be viewed in the light of several limitations including that the HEALS is not yet validated. Although preliminary factor analysis30 and cognitive interviewing has been performed, the questions and domains will not be finalized until results from the cognitive interviewing have been analyzed. At that point, the larger validation process with confirmatory factor analysis will be conducted. After confirmatory factor analysis, future research should examine these domains of the HEALS in comparison to a different spirituality instrument with a primary focus on meaning in health-related outcomes.16 Despite this limitation, the results of this study are promising for the future of this measure of psychosocial spiritual healing.
Second, the results of this preliminary partial validation cannot be generalized to people with other chronic and life-threatening illness, or perhaps to other women living with HIV. Since women in this sample have been with the WIHS cohort study for a median of 13.6 years, there could be cohort effects. Further research will need to examine the feasibility of the HEALS in a variety of populations diverse in both demographic characteristics and disease diagnosis. Similarly, the convenience sampling limits the extent to which these findings can be generalized to other HIV populations who may be less engaged in research and care. Finally, as this was a secondary data analysis, we could only include variables that had been collected in the original data collection process.
Conclusion
This study is an important step in preliminary validation of the HEALS. As questions become finalized, the HEALS will hopefully be able to detect the degree to which religious, spiritual, interpersonal, and intrapersonal factors contribute to patient healing. This study also helps to fill an important gap in our knowledge about the meaning of religion in women with HIV living in Chicago and its metropolitan area. Extant literature examining spirituality and religiousness among HIV-infected women tends to focus on the Southeastern region of the USA,1,10,12,13,39 with other regions being less closely examined.29,41 With the validation of this tool, clinicians and researchers will have a unique way to assess for psychosocial spiritual factors in healing people with life-threatening and chronic illness.
Acknowledgments
Data in this manuscript were collected by the Women’s Interagency HIV Study (WIHS). The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). WIHS (Principal Investigators): Chicago WIHS U01-AI-034993 (Mardge Cohen and Audrey French). The WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID), with additional co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA), and the National Institute on Mental Health (NIMH).
Disclosure
The authors report no conflict of interest in this work.
References
Dalmida SG, Holstad MM, Dilorio C, Laderman G. The meaning and use of spirituality among African American women living with HIV/AIDS. West J Nurs Res. 2012;34(6):736–765. | ||
Mattis JS, Jagers RJ. A relational framework for the study of religiosity and spirituality in the lives of African Americans. J Community Psychol. 2001;29(5):519–539. | ||
Edwards A, Pang N, Shiu V, Chan C. The understanding of spirituality and the potential role of spiritual care in the end-of-life and palliative care: a meta-study of qualitative research. Palliat Med. 2010;24(8)753–770. | ||
Ehman JW, Ott BB, Short TH, Ciampa RC, Hansen-Flaschen J. Do patients want their physicians to inquire about their spiritual or religious beliefs if they become ill? Arch Intern Med. 1999;159(15):1803–1806. | ||
Sulmasy DP. A biopsychosocial-spiritual model for the care of patients at the end of life. Gerontologist. 2002;42(3):24–33. | ||
Puchalski CM. Spirituality and the care of patients at the end-of-life: an essential component of care. Omega (Westport). 2007;56(1):33–46. | ||
Jim HS, Pustejovsky JE, Park CL, et al. Religion, spirituality, and physical health in cancer patients: a meta-analysis. Cancer. 2015;121(21):3760–3768. | ||
Mako C, Galek K, Poppito SR. Spiritual pain among patients with advanced cancer in palliative care. J Palliat Med. 2006;9(5):1106–1113. | ||
Dalmida SG. Spirituality, mental health, physical health, and health-related quality of life among women with HIV/AIDS: integrating spirituality into mental health care. Issues Ment Health Nurs. 2006;27(2):185–198. | ||
Dalmida SG, Holstad MM, Dilorio C, Laderman G. Spiritual well-being and health-related quality of life among African-American women with HIV/AIDS. Appl Res Qual Life. 2011;6(2):139–157. | ||
Dalmida SG, Holstad MM, Dilorio C, Laderman G. Spiritual well-being, depressive symptoms, and immune status among women living with HIV/AIDS. Women Health. 2009;49(2–3):119–143. | ||
Ludema C, Doherty IA, White BL, Simpson CA, Villar-Loubet O. Religiosity, spirituality, and HIV risk behaviors among African American women from four rural counties in southeastern U.S. J Health Care Poor Underserved. 2015;26(1):168–181. | ||
Phillips KD, Mock KS, Bopp CM, Dudgeon WA, Hand GA. Spiritual well-being, sleep disturbance, and mental and physical health status in HIV-infected individuals. Issues Ment Health Nurs. 2006;27(2):125–139. | ||
Ironson G, Solomon GF, Balbin EG, et al. The Ironson-woods spirituality/religiousness index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Ann Behav Med. 2002;24(1):34–48. | ||
Fetzer Institute & National Institute on Aging Working Group. Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research. Fetzer Institute, Kalamazoo, MI; 1999. | ||
Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy – spiritual well-being scale (FACIT-Sp). Ann Behav Med. 2002;24(1):49–58. | ||
Koenig H, Parkerson GR Jr, Meador KG. Religion index for psychiatric research. Am J Psychiatry. 1997;154(6):885–886. | ||
Pargament KI, Feuille M, Burdzy D. The brief RCOPE: current psychometric status of a short measure of religious coping. Religions. 2011;2(1):51–76. | ||
Hall DE, Meador KG, Koenig HG. Measuring religiousness in health research: review and critique. J Relig Health. 2008;47(2):134–163. | ||
Underwood LG, Teresi JA. The daily spiritual experience scale: development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Ann Behav Med. 2002;24(1):22–33. | ||
Allport GW, Ross JM. Personal religious orientation and prejudice. J Pers Soc Psychol. 1967;5(4):432–443. | ||
Hodge DR. The intrinsic spirituality scale. J Soc Serv Res. 2003;30(1):41–61. | ||
Selman L, Harding R, Gysels M, Speck P, Higginson IJ. The measurement of spirituality in palliative care and the content of tools validated cross-culturally: a systematic review. J Pain Symptom Manage. 2011;41(4):728–753. | ||
Young WC, Nadarajah SR, Skeath PR, Berger AM. Spirituality in the context of life-threatening illness and life-transforming change. Palliat Support Care. 2014;13(3):653–660. | ||
Lewis LM. Spiritual assessment of in African-Americans: a review of measures of spirituality used in health research. J Relig Health. 2008;47(4):458–475. | ||
Coats H, Crist JD, Berger A, Sternberg E, Rosenfeld AG. African American elders’ serious illness experiences: narratives of “God did,” “God will,” and “life is better”. Qual Health Res. 2015;1–15. | ||
Johnstone B, McCormack G, Yoon DP, Smith ML. Convergent/divergent validity of the brief multidimensional measure of religiousness/spirituality: empirical support for emotional connectedness as a “spiritual” construct. J Relig Health. 2012;51(2):529–541. | ||
Muturi N, An S. HIV/AIDS stigma and religiosity among African American women. J Health Commun. 2010;15(4):388–401. | ||
Simoni J, Martone MG, Kerwin JF. Spirituality and psychological adaptation among women with HIV/AIDS: implications for counseling. J Couns Psychol. 2002;49(2):139–147. | ||
Sloan D, BrintzenhofeSzoc K, Kichline T, et al. An assessment of meaning in life threatening illness: development of the HEALS – healing experience in all life stressors. Patient Relat Outcome Meas. 2017;8:15–21. | ||
Bacon MC, von Wyl V, Alden C, et al. The women’s interagency HIV study: an observational cohort brings clinical sciences to the bench. Clin Vaccine Immunol. 2005;12(9):1013–1019. | ||
Barkan SE, Melnick SL, Preston-Martin S, et al. The women’s interagency HIV study. Epidemiology. 1998;9(2):117–125. | ||
Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):382–401. | ||
Ellison CW. Spiritual well-being: conceptualization and measurement. J Psychol Theol. 1983;11:330–340. | ||
Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. | ||
Ironson G, Woods T. IWORSHIP: An Unpublished Assessment Instrument of Religious and Spiritual Dimensions. Coral Gables, FL: University of Miami; 1998. | ||
Miller WC, Anton HA, Townson AF. Measurement properties of the CES-D scale among individuals with spinal cord injury. Spinal Cord. 2008;46(4):287–292. | ||
Kuptniratsaikul V, Chulakadabba S, Ratanavijitrasil S. An instrument for assessment of depression among spinal cord injury patients: comparison between the CES-D and the TDI. J Med Assoc Thai. 2002;85(9):978–982. | ||
Belcher AE, Dettmore D, Holzemer SP. Spirituality and sense of well-being in persons with AIDS. Holist Nurs Pract. 1989;3(4):16–25. | ||
Braxton ND, Lang DL, Sales JM, Wingood GM, DiClemente RJ. The role of spirituality in sustaining the psychological well-being of HIV-positive Black women. Women Health. 2007;46(2–3):113–129. | ||
Pew Research Center. A Religious Portrait of African-Americans. Washington, DC: Pew Research Center; 2009. Web 16 July 2016. Available from: http://www.pewforum.org/2009/01/30/a- religious-portrait-of-african-americans/. Accessed July 11th, 2016. | ||
Cotton S, Puchalski CM, Sherman SM, et al. Spirituality and religion in patients with HIV/AIDS. J Gen Intern Med. 2006;21(S5):S5–S13. | ||
Park CL, Lim H, Newlon M, Suresh DP, Bliss DE. Dimensions of religiousness and spirituality as predictors of well-being in advanced chronic heart failure patients. J Relig Health. 2014;53(2):579–590. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.