Back to Journals » Clinical Epidemiology » Volume 12
Temporal Trends of the Incidence of Ischemic Heart Disease in Iran Over 15 Years: A Comprehensive Report from a Multi-Centric Hospital-Based Registry
Authors Nouri F , Feizi A, Taheri M , Mohammadifard N , Khodarahmi S , Sadeghi M , Sarrafzadegan N
Received 25 April 2020
Accepted for publication 19 July 2020
Published 6 August 2020 Volume 2020:12 Pages 847—856
DOI https://doi.org/10.2147/CLEP.S259953
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Eyal Cohen
Fatemeh Nouri,1,2 Awat Feizi,2 Marzieh Taheri,3 Noushin Mohammadifard,4 Somayeh Khodarahmi,5 Masoumeh Sadeghi,6 Nizal Sarrafzadegan7
1Pediatric Cardiovascular Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran; 2Department of Biostatistics and Epidemiology, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran; 3Interventional Cardiology Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran; 4Hypertension Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran; 5Heart Failure Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran; 6Cardiac Rehabilitation Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran; 7Isfahan Cardiovascular Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran
Correspondence: Nizal Sarrafzadegan
Isfahan Cardiovascular Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan 8158388994, Iran
Tel +983136115310
Fax +983136115303
Email [email protected]
Background: We sought to explore the temporal trend of ischemic heart disease (IHD) incidence rate (IR) in a large city of Iran.
Methods: The study population comprised hospitalized patients who were living in Isfahan, Iran, with first or recurrent IHD during the period of 2001 to 2016. To identify patients, clinical diagnostic codes were applied according to the International Classification of Diseases 10 (ICD-10: I20.0, I21–I25) and the “World Health Organization Monitoring Trends and Determinants in Cardiovascular Disease” diagnostic categories (WHO-MONICA). Using a direct method, we calculated age-, sex-, and place-of-residence-adjusted incidence rates based on multiple reference populations. To examine the long-term trend for the IR, a bootstrap robust zero-truncated negative binomial regression model was used.
Results: A total of 102,254 hospitalized patients, with a mean (SD) age of 61.85 (12.79), were registered between 2001 and 2016. After an initial reduction from 2006 to 2010, crude and adjusted IRs of IHD increased between 2010 and 2016. We further observed a significant increasing long-term temporal trend in the IR with an average annual change of 1.42% to 3.36% over the study period.
Conclusion: Our findings showed a decreasing trend in the IR of IHD between 2006 and 2010, possibly attributed to the comprehensive community-based interventions named “Isfahan Healthy Heart Program” performed from 2001 to 2007, followed by an increase in the adjusted IR of IHD between 2010 and 2016 in Isfahan; this indicates the importance of continuing the preventive measures to preclude the risk factors of cardiovascular diseases in our population.
Keywords: ischemic heart disease, incidence rate, temporal trend, registry
Introduction
Based on the Global Burden of Disease study (GBD), cardiovascular diseases (CVDs) have been the leading cause of death since 1980.1 In previous studies, a reduced CVDs mortality rate was observed in high-income countries; however, high rates of CVDs mortality have been reported in low- and middle-income countries (LMIC), particularly in the Eastern Mediterranean Region (EMR).2 In the EMR, the total number of deaths from CVDs was 1,373,329 in 2015, which accounted for over one-third of all deaths. Moreover, age-standardized mortality rate of CVDs in EMR was higher than the global average.1 Iran is among the countries in the EMR with the highest burden of CVD.2 Previous studies have shown that among all CVDs, ischemic heart disease (IHD) is the leading cause of mortality and disability-adjusted life years (DALY) in Iran and around the world.2,4 Mortality remains the most important contributor to the burden of IHD in Iran. Moreover, population growth and aging can lead to more incidences, which ultimately increases the burden of IHD in Iran.5
The GBD study on IHD epidemiology estimates has highlighted the paucity of data concerning IHD in many LMIC and EMR countries.1,6,7 More reliable information regarding the global burden of IHD and epidemiologic measures, including incidence, prevalence, case fatality, and mortality has to improve the surveillance programs in all regions of world.6 The reports of health system challenges in managing CVD in certain EMR countries re-emphasize the need for high quality data.1,7 The GBD results are a combination of real and estimated data; moreover, the low level of data completeness in regard to certain locations implies that the estimates for these places rely more on the modelling process. The improvement in estimation methods represented in each iteration of GBD does not mitigate the pressing need for investments in data gathering and surveillance at country level.8
To the best of our knowledge, there are very few data on the incidence of IHD in Iran, and if there are, it is usually based on cohort studies with short follow-ups or small sample sizes. The present study aimed to examine the 15-year temporal trends in crude and age-, sex-, and place-of-residence-adjusted incidence rate (IR) of IHD in a large city of Iran. The adjustments were done using multiple populations as reference and different diagnostic methods which helped identify the heterogeneity and variability.
Materials and Methods
Design and Patients
This study consists of IHD and stroke registries initiated by the “Isfahan Healthy Heart Program” (IHHP) in 2001 and continued until 2016. Here, we reported the IHD registry methods and results as we published the stroke registry before.9,10 IHHP is a comprehensive integrated community-based program that consists of multiple simultaneous interventions at community levels and in high risk groups.11,12 The registry was performed using the methodology of the “World Health Organization Monitoring Trends and Determinants in Cardiovascular Disease” diagnostic categories (WHO-MONICA).13,14 In this study, we reported the incidence rate and case-fatalities of IHD in Isfahan, Iran; this was done through gleaning information from the disease registration covering all hospitalized IHD patients from April 2001 to March 2016. Isfahan is an industrial city located in central Iran and the second most populous metropolitan area in Iran after Tehran. Most large cities in Iran are similar regarding socioeconomic status, population density, age distribution, men to women ratio, demographic picture, and health profile.15,16 The population of Isfahan district was 1,253,338 (51.6% men and 90.6% urban residents) in 2001. In 2016, the population of Isfahan grew up to 1,791,621. Because Isfahan city is the center of Isfahan province, patients from other cities of the province are also referred to its hospitals. In this registry, we collected private, governmental, social security insurance, university-affiliated, and military hospital records. This study was approved by the Research Council of Isfahan Cardiovascular Research Institute (ICRI).17 Ethics approval was obtained from the Ethics Committee of Isfahan Cardiovascular Research Center. Patients’ privacy was protected at all times. In order to maintain a full confidentiality of the patients’ information, a registration code, (as inspired by Huffman coding)18 formed by a de-identifiable combination of patient information, such as the first and last name and date of birth, was assigned to be used for research purposes.
In 2015, we started a new CVD registry named the “Persian Registry of Cardiovascular Disease” (PROVE) that covered many CVD types and used methodologies other than MONICA. PROVE was initiated in Isfahan with some elements of national scale-up while both stroke and IHD continued to be registered as before. IHD has been expanded in PROVE to register all acute coronary syndromes (ACSs).19
Data Collection
Patients’ IHD records and basic information were evaluated by our trained nurses. Medical records of patients, who were hospitalized in Isfahan hospitals, were assessed for IHD signs and symptoms. All cases of possible heart attack were identified retrospectively based on death certificates and hospital discharge reports. The studied variables included sex, birthdate, date of chest pain onset and its management, admission date, hospital name, risk factors, IHD history, diagnostic categories associated with clinical diagnosis (CD) based on the International Classification of Diseases 10 (ICD-10) (CD-ICD-10), and WHO-MONICA. All patients were followed up for a period of 28 days to define their case fatality and survival. Details of death, death certificate diagnoses, and findings at autopsy were recorded on fatal events.17
In CD-ICD-10 method, subgroups of IHD included myocardial infarction (MI) (I21 and I22), unstable angina (I20.0), stable angina (I20.1–I20.9), and other IHD such as chronic IHD (I25), other acute IHD (I24), and complications following acute MI (I23).20 IHD patients were identified based on primary diagnoses or underlying causes of death and the secondary diagnoses at discharge from hospital or contributory causes of death from death certificate. In WHO-MONICA method, events are classified as first-ever or recurrent and fatal or non-fatal. Diagnostic criteria are based on previous history of IHD, symptoms at onset, maximum levels of serum enzymes, relevant electrocardiograms (coded according to the Minnesota codes), clinical findings, investigations undertaken within 28 days of onset, and postmortem findings. Fatal cases were defined as death occurring within 28 days of the onset of an event. Signs of angina within 28 days were not regarded as a new event. Non-fatal events were classified as “definite” (NFl), “possible” (NF2), “ischemic cardiac arrest” (NF3), or “no myocardial infarction” (NF4). In addition, fatal events were classified as “definite” (F1), “possible” (F2), “unclassifiable” (F9) (called “insufficient data”), or “no myocardial infarction or coronary death” (F4). Details pertaining to the categories of the WHO-MONICA diagnostics were previously reported.13,14 In this study, the two following diagnostic methods were used to identify hospitalized IHD patients: CD-ICD-10 method (I20.0 and I21-I25) and third definition (NFl+NF2+Fl+F2+F9) from the WHO-MONICA method.
Statistical Analysis
We calculated age, sex, and place of residence whether urban- or rural-area adjusted IRs of IHD per 10,000 from April 2001 to March 2016. The annual numbers of the Isfahan population for the study years based on different age groups, place of residence, and sex were used as the denominators for all IR calculations. To adjust the age, sex, and place of residence differences in the studied years, the direct method was applied using the following five different populations as reference; 2006 and 2011 Iranian population census, 2006 and 2011 Isfahan province population census, and the sum of Isfahan district population from April 2001 to March 2016. To examine the trend of IHD incidence across time, bootstrap robust zero-truncated negative binomial regression models were used for analysis; the year was considered as an independent variable while crude and age-, sex-, and place-of-residence-adjusted IRs were dependent variables. The negative binomial regression model addresses the over dispersion issue and requires fewer assumptions concerning the patterns of variance compared to Poisson regression. By adjusting the IRs, we obtained the data for dependent variables in a regression model which truncated at zero. In other words, we used zero-truncated negative binomial regression because dependent variables do not include the zero value. All hospitalized patients with first and recurrent IHD events were further considered, hence an intra-group correlation was expected. A common approach to examining the intra-group correlation is robust standard error of regression coefficients using different methods. In this study, we used robust bootstrap to address the misspecification caused by intra-group correlation. This regression model allows for the estimation of trends across individual calendar years to obtain average annual percentage changes. On the basis of the corresponding estimated regression coefficient and standard error, a yearly change in IHD can be derived along with 95% confidence interval (CI). The exponent of the estimated regression coefficient is the relative risk (RR) per each calendar year. The regression coefficient of year multiplied by 100 gives the average annual change of incidence in percentages. Data were analyzed by R Statistical Software version 3.5.3 (R Core Team, 2019).
Results
In total, we registered 102,254 hospitalized patients of first and recurrent IHD incident events in Isfahan, Iran, over the period of April 2001 to March 2016. Approximately 97% were hospitalized with IHD as the primary diagnosis. Among the 102,254 admissions with IHD assessed by CD-ICD-10 method, 48,465 IHD cases were identified via the WHO-MONICA method. Patients’ demographic data based on diagnosis methods are summarized in Table 1. About 54% of the hospitalized IHD patients were men, more than 50% aged 55–75 years, around 1.5% were younger than 35 years old, and approximately 95% were from urban areas. The mean (SD) age was 61.85 (12.79) years. Table 1 provides more details as to the basic characteristics of study participants.
 |
Table 1 Characteristics of the Ischemic Heart Disease Patients Based on Diagnostic Methods |
Tables 2 and 3 depict the age, sex, and place of residence-specific IRs (per 10,000) of IHD based on CD-ICD-10 and WHO-MONICA methods, respectively, over the three observation periods: April 2001–March 2006, April 2006–March 2011, and April 2011–March 2016. The IR of IHD based on WHO-MONICA for urban women increased with the rise in age. Among all periods in both areas, IR of IHD (based on both studied diagnosis methods) for men aged 30–60 years were higher than that of women with the same age range. For both genders in all age categories, the IR of IHD for urban area was higher than that of rural areas in the first time period. Based on both studied diagnosis methods, the increase in the IR of IHD was considerably higher in patients older than 65 years compared to those aged 40–65 years old, in women compared to men, and in urban areas compared to rural areas.
 |
Table 2 Incidence Rate (per 10,000) of Ischemic Heart Disease Based on CD-ICD-10 in Isfahan, Iran, Between April 2001andMarch 2016 |
 |
Table 3 Incidence Rate (per 10,000) of Ischemic Heart Disease Based on WHO-MONICA Diagnostic Categories in Isfahan, Iran, During April 2001–March 2016 |
Figure 1 and Supplementary Appendix 1 show the crude and age-, place-of-residence, and sex-adjusted trend of IR (per 10,000) of IHD based on CD-ICD-10 method across 15 years: from April 2001 to March 2016. IRs of IHD were adjusted by the five mentioned populations as reference. Furthermore, Figure 2 and Supplementary Appendix 2 graphically depict the crude and adjusted trends of estimated IR based on different standard populations in terms of IHD diagnosed by WHO-MONICA criteria over the study periods. The lowest and highest adjusted IRs of IHD based on both studied diagnosis methods were respectively related to adjustment based on 2006 Iranian population census and 2011 Isfahan province population census as reference across the time periods. Therefore, according to different reference populations, adjusted IRs of IHD based on CD-ICD-10 ranged from 27 to 37 (per 10,000) in April 2001 to March 2002 and from 39 to 51 in April 2015 to March 2016. Similarly, adjusted IR based on WHO-MONICA ranged from 11 to 16 and 19 to 25 in the same time periods. According to Figures 1 and 2, after the initial decrease from 2006 to 2010, crude and age-, sex-, and place-of-residence-adjusted IR of IHD increased over the study period based on all reference populations.
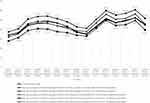 |
Figure 1 Crude and adjusted incidence rate (per 10,000) of ischemic heart disease based on CD-ICD-10 in Isfahan, Iran, during April 2001–March 2016. |
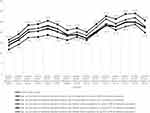 |
Figure 2 Crude and adjusted incidence rate (per 10,000) of ischemic heart disease based on WHO-MONICA in Isfahan, Iran, during April 2001–March 2016. |
As seen in Table 4, the average annual increase in IHD incidence based on CD-ICD-10 in Isfahan ranged from 1.42% (95% CI= 0.16–2.68) to 2.42% (95% CI= 0.89–3.95) per year. A significant increasing trend was detected for all estimated IRs based on different reference populations. In addition, a significant increasing trend was also observed for the IR of IHD based on WHO-MONICA during the 15-year study period, for all reference populations in Isfahan. The average annual increase in the incidence of IHD ranged between 1.93% (95% CI= 0.59–3.26) and 3.36% (95% CI= 1.96–4.76) per year.
 |
Table 4 Annual Percent Change in the Incidence of Ischemic Heart Disease in Isfahan, Iran, During April 2001–March 2016 |
Discussion
In this study, we elucidated the temporal trends in age-, sex-, and place-of-residence-adjusted IR of IHD in Isfahan, Iran. We used five populations as reference or standard for adjustment and two diagnostic methods, namely WHO-MONICA and CD-ICD-10 between April 2001 and March 2016.
A significant increasing long-term temporal trend was detected in the crude and age-, sex-, and place-of-residence-adjusted IR of IHD based on all reference populations and diagnostic methods in an Iranian population across a 15-year period with an average annual change of 1.42–3.36%.
Previous reports from some western countries showed that the adjusted incidence trend of IHD or MI decreased over the same time period.20,22 A binational study of more than 7 million IHD hospitalizations in England and Australia highlighted that the age-adjusted hospitalization rates for total IHD declined in Australia from 1996 to 2013 (with an average annual percent change of −3.0); meanwhile, IHD rates increased in England from 1996 to 2003 (with an average annual percentage change of 0.8), followed by a significant decrease from 2004 to 2013 (with average annual percentage change of −2.4).20 On the contrary, in Asian countries, increasing trends in the adjusted incidence of IHD or MI have been reported over the same time period.23,25 In Korea, using the Korean National Health Insurance Database, the crude incidence of AMI increased by 2.1 times from 43.5 cases per 100,000 persons in 1997 to 91.8 cases per 100,000 persons in 2007. Crude and age-adjusted IR in Korea increased from 1997 to 2002, indicating a continuous increase after 2002. Age-adjusted IRs of AMI increased from 60.4 and 40.7 in 1997 to 92.2 and 63.7 in 2007 regarding males and females, respectively.25
Previous studies showed that the trends of age-standardized IHD mortality declined in high-income western regions from 1980 to 2010, but they increased in South Asia, Central Asia, East Asia, and Eastern Europe. In addition, the highest age-standardized IHD death rates were concentrated in a cluster of regions, including North Africa and Middle East called MENA region.26 Mortality rate depends on the number of new cases and the survival among the patients. Therefore, the change in mortality rate may be caused by 1) a change in the incidence of IHD due to the changes in known coronary risk factors in the population or 2) from the change survival rate as a result of the changes in the disease management and treatment.27,28 GBD study showed that traditional risk factors play a major role in the regional differences in IHD mortality rates around the world.26 A recent systematic review reported increased rates in all major risk factors, including diabetes, hypertension, hyperlipidemia, smoking, obesity, and sedentary lifestyle in the Middle East. Specifically, significant changes in dietary habits and the growing epidemic in the use of alternative tobacco products have been further reported.29 Findings of a longitudinal study showed that the prevalence of metabolic syndrome, as a cluster of interconnected risk factors and a major determinant of IHD incidence,30 had a significant increasing trend in the Iranian middle-aged population from 2001 to 2013.31 Therefore, the increasing trend in IHD incidence rate in our study in Iran may have also been affected by such conditions.
Moreover, our findings showed that the IRs of IHD based on CD-ICD-10 were higher than the data obtained according to WHO-MONICA criteria identifying IHD patients. Because the WHO-MONICA criteria are fairly quantitative and complicated, it is not surprising that only some of the cases diagnosed by clinicians as IHD qualify it.13 In the current study, according to the different reference populations, the adjusted IRs (per 10,000) of IHD based on CD-ICD-10 method varied from 27 to 37 and 39 to 51 in April 2001–March 2002 and April 2015–March 2016, respectively. According to the Iranian MI Registry in 2012, the crude and age-standardized IR of MI based on ICD-10 were 64.9 and 73.3 per 100,000, respectively, in the whole country, significantly ranging from 24.5 to 152.5 per 100,000 across the 31 provinces.32 In 2001, a large ongoing prospective cohort named the Isfahan Cohort Study (ICS) was initiated for the healthy population without CVDs at baseline; from 2001 to 2011, the age adjusted IRs of ACS including fatal and nonfatal MI, sudden cardiac death, and unstable angina events were reported to be 1168 and 887 per 100,000 person-years for men and women, respectively.33
Although a significant increasing long-term temporal trend was detected in the crude and age-, sex-, and place-of-residence-adjusted IR of IHD based on all reference populations and diagnostic methods, the trend of incidence rate showed fluctuation. According to Figures 1 and 2, after an initial reduction from 2006 to 2010, crude and adjusted IRs increased between 2010 and 2016. In this regard, similar results were observed in previous studies. Among hospitalized stroke patients in Isfahan from 2000 to 2014, the age-standardized incidence of stroke significantly raised by 6.65% per year, from 2009 to 2014.9 The changes in IR may be caused by the changes in known coronary risk factors in the population.27,28 The MONICA results based on 38 populations from 21 countries (three in Asia, three in Australasia, two in North America, and others in Europe) suggested the need to consider a time lag between risk factor changes occurring in the population and their effect on disease incidence.34 Therefore, the decline in IR could be related to many reasons, including improved knowledge of the population and healthier lifestyle, at least in part, by preventive care programs and interventional projects. In Isfahan, a community intervention trial, namely IHHP, was launched in 1999–2000 and implemented from 2001 to 2007. IHHP was a 6-year, action-oriented, comprehensive integrated community-based program for the prevention and control of CVDs via reducing its risk factors and improving relevant healthy behaviors. It targeted the whole population and high risk groups living in two intervention cities of Isfahan and Najaf Abad. It included a large number of interventions for increasing awareness among the adults, health professionals, cardiac patients, children, and adolescents of the importance of controlling CVD risk factors.11,35,36 Previous studies showed that implementing educational, environmental, and legislation strategies in the IHHP could improve lifestyle behaviors, physical and metabolic risk factors, and survival among patients.11,36,37 Based on evidence, sustainability of interventional programs need to examine two or more years after implementation.38 Previous studies showed that many IHHP interventions were sustainable and integrated in health system and the society after the completion of this program in 2007;11,39 however, after 2010, the impact of IHHP interventions seems to have been diluted. Based on a review study, it is difficult to generalize about the long-term impact of implementation efforts and the extent to which interventional programs and practices are sustained.38
Strengths and Limitations
The first strength of this study is its long-term follow-up that can be conducive to determining the trends of incidence rate over time. The second is the registry of IHD in all private, governmental, social security insurance, university-affiliated, and military hospitals in Isfahan city. The third strength is that we applied two diagnosis approaches and multiple reference populations which helped identify heterogeneity and variability. And, finally, a comprehensive statistical method was used.
One of the limitations is the non-generalizability to all hospitalized patients with IHD because we did not have access to patients who were managed at home, died before reaching the hospital, or failed to receive medical care due to their lack of access to information or economic reasons. The number of patients who were not included in the study might be small as most IHD events, particularly acute IHD, are considered as emergency in the healthcare system in Iran and all hospitals must admit such patients irrespective of their insurance status. In addition, patients with stable angina were not included in the study and, obviously, these results cannot be generalized to all patients with IHD. Moreover, although the current study tried to cover all hospitals, the samples were limited to a central area of Iran. Since the incidence rates are dependent on the prevalence of the risk factors, it is necessary to examine the temporal trend in adjusted incidence rate in other cities of Iran. The present analysis does not include trend of mortality rates, environmental, or other risk factor information that is often measured in a clinical setting. In addition, due to the lack of reference standards for reporting and possible challenges in the quality of data in primary care, data quality measurement in hospital records was limited. These limitations should be taken into account when interpreting the results of the study.
Conclusions
We reported increasing long-term trends in age-, sex-, and place-of-residence-adjusted IR of IHD in Isfahan, Iran. A cross-sectional decline was observed over the time periods after the implementation of the interventional program; however, it is still necessary to reinforce the implementation of community-based interventions regarding disease prevention and healthy lifestyle promotion. In addition, it is important to implement effective surveillance programs and better monitor the trends over time in regard to the incidence and prevalence of IHD and its risk factors.
Data Sharing Statement
To discuss our data sharing policy, please contact Nizal Sarrafzadegan at [email protected].
Acknowledgment
This study was supported by grant number 91116 from ICRC. We appreciate all registry staff that helped us in data gathering, especially Leila V. Dalili, Zahra Kiani, Zahra Ghorbani, Mahtab Sepahifar, and Farzaneh Nilforooshzade.
Disclosure
The authors declare they have no conflict of interest with respect to this research study and paper.
References
1. Tehrani-Banihashemi A, Moradi-Lakeh M, El Bcheraoui C, et al. Burden of cardiovascular diseases in the Eastern Mediterranean Region, 1990–2015: findings from the Global Burden of Disease 2015 study. Int J Public Health. 2018;63(Suppl. 1):137–149.
2. Sarrafzadegan N, Mohammadifard N. Cardiovascular disease in iran in the last 40 years: prevalence, mortality, morbidity, challenges and strategies for cardiovascular prevention. Arch Iran Med. 2019;22(4):204–210.
3. Sepanlou SG, Parsaeian M, Krohn KJ, et al. Disability-Adjusted Life-Years (DALYs) for 315 diseases and injuries and Healthy Life Expectancy (HALE) in Iran and its neighboring Countries, 1990–2015: findings from Global Burden of Disease Study 2015. Arch Iran Med. 2017;20(7):403–418.
4. Moradi-Lakeh M, Sepanlou SG, Karimi SM, et al. Trend of socio-demographic index and mortality estimates in Iran and its neighbors, 1990–2015: findings of the Global Burden of Diseases 2015 Study. Arch Iran Med. 2017;20(7):419–428.
5. Maracy MR, Isfahani MT, Kelishadi R, et al. Burden of ischemic heart diseases in Iran, 1990–2010: findings from the Global Burden of Disease study 2010. J Res Med Sci. 2015;20(11):1077–1083. doi:10.4103/1735-1995.172832
6. Moran AE, Oliver JT, Mirzaie M, et al. Assessing the global burden of ischemic heart disease: part 1: methods for a systematic review of the global epidemiology of ischemic heart disease in 1990 and 2010. Glob Heart. 2012;7(4):315–329. doi:10.1016/j.gheart.2012.10.004
7. Ramahi TM. Cardiovascular disease in the Asia Middle East region: global trends and local implications. Asia Pac J Public Health. 2010;22(3_suppl):83S–89S. doi:10.1177/1010539510373034
8. Roth GA, Abate D, Abate KH, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788.
9. Arsang-Jang S, Mansourian M, Mohammadifard N, et al. Temporal trend analysis of stroke and salt intake: a 15-year population-based study. Nutr Neurosci. 2019:1–11. doi:10.1080/1028415X.2019.1638665
10. Bahonar A, Khosravi A, Khorvash F, et al. Ten-year trend in stroke incidence and its subtypes in Isfahan, Iran during 2003–2013. Iran J Neurol. 2017;16(4):201–209.
11. Sarrafzadegan N, Laatikainen T, Mohammadifard N, Fadhel I, Yach D, Puska P. “Isfahan healthy heart program”: a practical model of implementation in a developing country. Prog Prev Med. 2018;3(3):e0014.
12. Sarraf-Zadegan N, Sadri G, Malek Afzali H, et al. Isfahan healthy heart programme: a comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58(4):309–320. doi:10.2143/AC.58.4.2005288
13. Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas A-M, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90(1):583–612. doi:10.1161/01.CIR.90.1.583
14. Luepker RV. WHO MONICA project: what have we learned and where to go from here? Public Health Rev. 2011;33(2):373. doi:10.1007/BF03391642
15. Statistical Center of Iran. Selected Findings of National Population and Housing Census, 2011. Tehran: Vice Presidency for Strategic Planning and Supervision, Statistical Centre of Iran. 2011.
16. Sarrafzadegan N, Hassannejad R, Marateb HR, et al. Correction: PARS risk charts: a 10-year study of risk assessment for cardiovascular diseases in Eastern Mediterranean Region. PLoS One. 2018;13(1):e0191379. doi:10.1371/journal.pone.0191379
17. Sarrafzadegan N, Oveisgharan S, Toghianifar N, Hosseini S, Rabiei K. Acute myocardial infarction in Isfahan, Iran: hospitalization and 28th day case-fatality rate. ARYA Atheroscler. 2009;5(3).
18. Huffman DA. A method for the construction of minimum-redundancy codes. Resonance. 2006;11(2):91–99. doi:10.1007/BF02837279
19. Givi M, Sarrafzadegan N, Garakyaraghi M, et al. Persian Registry Of cardioVascular diseasE (PROVE): design and methodology. ARYA Atheroscler. 2017;13(5):236–244.
20. Nedkoff L, Goldacre R, Greenland M, et al. Comparative trends in coronary heart disease subgroup hospitalisation rates in England and Australia. Heart. 2019;105(17):1343–1350. doi:10.1136/heartjnl-2018-314512
21. Rosamond WD, Chambless LE, Heiss G, et al. Twenty-two–year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125(15):1848–1857. doi:10.1161/CIRCULATIONAHA.111.047480
22. Robitaille C, Dai S, Waters C. Ischemic heart disease prevalence and incidence in Canada. Can J Cardiol. 2014;30(10):S75–S76. doi:10.1016/j.cjca.2014.07.062
23. Rumana N, Kita Y, Turin TC, et al. Trend of increase in the incidence of acute myocardial infarction in a Japanese population: Takashima AMI registry, 1990–2001. Am J Epidemiol. 2008;167(11):1358–1364. doi:10.1093/aje/kwn064
24. Lee CH, Cheng CL, Yang YHK, et al. Trends in the incidence and management of acute myocardial infarction from 1999 to 2008: get with the guidelines performance measures in Taiwan. J Am Heart Assoc. 2014;3(4):e001066. doi:10.1161/JAHA.114.001066
25. Hong JS, Kang HC, Lee SH, Kim J. Long-term trend in the incidence of acute myocardial infarction in Korea: 1997–2007. Korean Circ J. 2009;39(11):467–476. doi:10.4070/kcj.2009.39.11.467
26. Moran AE, Forouzanfar MH, Roth GA, et al. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the Global Burden of Disease 2010 study. Circulation. 2014;129(14):1483–1492. doi:10.1161/CIRCULATIONAHA.113.004042
27. Tunstall-Pedoe H, Kuulasmaa K, Mähönen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronar y-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA Project populations. Lancet. 1999;353(9164):1547–1557. doi:10.1016/S0140-6736(99)04021-0
28. Madsen M, Davidsen M, Rasmussen S, Abildstrom SZ, Osler M. The validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA registry. J Clin Epidemiol. 2003;56(2):124–130. doi:10.1016/S0895-4356(02)00591-7
29. Traina MI, Almahmeed W, Edris A, Tuzcu EM. Coronary heart disease in the Middle East and North Africa: current status and future goals. Curr Atheroscler Rep. 2017;19(5):24. doi:10.1007/s11883-017-0659-9
30. Talaei M, Sadeghi M, Marshall T, et al. Impact of metabolic syndrome on ischemic heart disease–A prospective cohort study in an Iranian adult population: Isfahan cohort study. Nutr Metab Cardiovasc Dis. 2012;22(5):434–441. doi:10.1016/j.numecd.2010.08.003
31. Hassannejad R, Kazemi I, Sadeghi M, et al. Longitudinal association of metabolic syndrome and dietary patterns: a 13-year prospective population-based cohort study. Nutr Metab Cardiovasc Dis. 2018;28(4):352–360. doi:10.1016/j.numecd.2017.10.025
32. Ahmadi A, Soori H, Mehrabi Y, Etemad K, Samavat T, Khaledifar A. Incidence of acute myocardial infarction in Islamic Republic of Iran: a study using national registry data in 2012. East Mediterr Health. 2015;21(1):5–12. doi:10.26719/2015.21.1.5
33. Sarrafzadegan N, Sadeghi M, Oveisgharan S, Iranipour R. Incidence of cardiovascular diseases in an Iranian population: the Isfahan Cohort Study. Arch Iran Med. 2013;16(3):138–144. doi:013163/AIM.004
34. Kuulasmaa K, Tunstall-Pedoe H, Dobson A, et al. Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA project populations. Lancet. 2000;355(9205):675–687. doi:10.1016/S0140-6736(99)11180-2
35. Nouri F, Feizi A, Mohammadifard N, Sarrafzadegan N. Methods of sampling and sample size determination of a comprehensive integrated community-based interventional trial: Isfahan Healthy Heart Program. ARYA Atheroscler. 2018;14(2):58–70. doi:10.22122/arya.v14i2.1488
36. Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ. 2009;87:39–50. doi:10.2471/BLT.07.049841
37. Sarrafzadegan N, Kelishadi R, Pourmoghaddas M, et al. Outcomes of a comprehensive healthy lifestyle program on cardiometabolic risk factors in a developing country: the Isfahan Healthy Heart Program. Arch Iran Med. 2013;16(1):4–11. doi:013161/AIM.004
38. Stirman SW, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci. 2012;7(1):17. doi:10.1186/1748-5908-7-17
39. Sarrafzadegan N, Rabiei K, Wong F, et al. The sustainability of interventions of a community-based trial on children and adolescents’ healthy lifestyle. ARYA Atheroscler. 2014;10(2):107–117.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
