Back to Journals » Clinical Epidemiology » Volume 14
Temporal Trends and Projections of Bladder Cancer Burden in China from 1990 to 2030: Findings from the Global Burden of Disease Study
Authors Xiang Z , Ye Z, Ma J, Lin Y, Zhou Y
Received 23 August 2022
Accepted for publication 23 October 2022
Published 6 November 2022 Volume 2022:14 Pages 1305—1315
DOI https://doi.org/10.2147/CLEP.S387289
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Lars Pedersen
Zhisheng Xiang,1 Zijie Ye,2 Jingyu Ma,1 Yongtian Lin,1 Yan Zhou1
1Department of Epidemiology, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou, People’s Republic of China; 2Department of Gastroenterology, The First Hospital of Fuzhou City Affiliated Fujian Medical University, Fuzhou, People’s Republic of China
Correspondence: Yan Zhou, Department of Epidemiology, Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, No. 420 Fuma Road, Fuzhou, 350014, People’s Republic of China, Email [email protected]
Purpose: Identifying disease burden and risk factors of bladder cancer and projecting its epidemiological trend in China, which can provide reference data to formulate measures for its management and prevention.
Methods: We analyzed the incidence, mortality, and disability-adjusted life-years (DALYs) data of bladder cancer in China from 1990 to 2019 and predicted to 2030 based on the Global Burden of Disease Study 2019. We also estimated the proportion of risk factors contributing to bladder cancer DALYs. The average annual percentage change (AAPC) in both sexes was calculated to quantify the temporal trends.
Results: In China, the age-standardized incidence rate of bladder cancer increased from 3.3/100,000 in 1990 to 5.16/100,000 in 2019 (AAPC of 1.47), while the age-standardized mortality rate and age-standardized DALYs rate declined slightly (AAPC of − 0.58 and − 0.65, respectively). The burden of bladder cancer increased with age, which reached a peak over 85 years old. The main risk factor for bladder cancer was smoking, and the contribution of high fasting plasma glucose increased from 1990 to 2019, with an AAPC of 0.85 in males and 0.61 in females. We predicted total incident cases, deaths and DALYs will increase to 150,372 and 53,520 and 1043,688 in 2030, respectively. The disease burden of bladder cancer in males will consistently higher than that in females from 2020 to 2030.
Conclusion: Although mortality and DALYs rates showed downward trends, the disease burden remained heavy in China at present. More effective and long-term health policies are needed to develop for early prevention and treatment of bladder cancer.
Keywords: bladder cancer, disease burden, trend, risk factors, China
Background
Bladder cancer is the most common urinary malignant tumor, with a variety of typical clinical symptoms, and has a significant impact on the quality of life of patients.1,2 This cancer originates from bladder mucosa, and its main pathological types include urothelial cell carcinoma, squamous cell carcinoma and adenocarcinoma. Among these pathological types, the most prevalent is urothelial cell carcinoma, accounting for more than 90% of bladder cancer.3 According to the 2020 global cancer statistics,4 bladder cancer was 1 of top 10 cancer worldwide, and its new cases and deaths were approximately 573,000 and 213,000, respectively. The latest trend of global showed that, the cases of bladder cancer in 2019 were 123.34% higher than that in 1990, while the age-standardized mortality rate decreased by 15.7%.5,6 The trend of the burden of cancer is influenced by several factors. It is possible to reduce the burden of cancer by changing the exposure risk of potential factors. Therefore, knowing the relationship between inherited or environmental factors and the occurrence of bladder cancer will play an important role in the prevention and treatment of this cancer. It is public knowledge that the major risk factors for bladder cancer include age, smoking and occupational exposure to aromatic amines.7–9 The exposure of some risk factors can be avoided by taking relevant measures. Currently, the etiology of bladder cancer remains unclear, so determining the contribution of various risk factors will be helpful to screen and prevent bladder cancer.
The highly heterogeneous is found in bladder cancer, and its incidence and mortality vary greatly around the world.10 The countries with the highest incidence and mortality were Morocco and Lebanon, respectively, while countries such as Nigeria and Guatemala had a lower burden of bladder cancer.6 In China, the incidence of cancer continues to increase, exceeding the world average.11 With the population aging and urbanization in China, cancer has become a major public health problem.12 Although two studies had described the burden of bladder cancer in some regions of China, these studies had some limits due to the sample sizes or data sources.13,14 Meanwhile, no research has been done to predict the trend of bladder cancer in China for the next 10 years. The latest Global Burden of Diseases (GBD) study provides data on the incidence, mortality, and disability-adjusted life-years (DALYs) of bladder cancer from 1990 to 2019, which gives us the opportunity to know the burden of bladder cancer in China nearly 30 years. Therefore, in this study, we will comprehensively evaluate the burden of bladder cancer in China and its trend related to risk factors by using the latest data of GBD 2019. We also will predict the future trend of burden of bladder cancer in China. We can know more epidemiology characteristics of bladder cancer from the study, and the results can be regarded as a scientific evidence for the formulation and application of cancer prevention strategies in China.
Methods
Data Sources
Data on the incidence, mortality, and DALYs of bladder cancer in China by gender and age from 1990 to 2019 were extracted from the GBD 2019 database, which provided more than 350 diseases data in 195 countries from 1990 to 2019. The inclusion criteria of the study was that the location was “China”, the cause was “bladder cancer” and the measures were “incidence”, “mortality” and “DALYs”. Since there were few cases below 15 years old, we combined patients whose age was below 15 years into one group. Then, we analyzed 16 age-specific rates by every 5 years in both sexes. We also downloaded the data of risk factors of bladder cancer in order to identify the proportion of DALYs attributable to these factors. More detailed methodology for GDB 2019 has been described previously.15 These data can be freely downloaded from the Institute for Health Metrics and Evaluation (http://ghdx.healthdata.org/gbd-results-tool). In addition, for the projection of bladder cancer burden, the future Chinese population between 2020 and 2030 was obtained from the United Nations World Population Prospects 2019 Revision by gender and age (https://population.un.org/wpp/Download/Standard/Population/). The Ethics Committee of Fujian Cancer Hospital determined that ethics approval and informed consent were not required for this research, because the GBD 2019 was a publicly available database, and all data were anonymous. The research was conducted in accordance with the Declaration of Helsinki, and the research data were kept confidential.
Statistical Analyses
Using the estimated value to describe the burden of bladder cancer by age, sex and year. To avoid the effect of the age composition of the populations, we chose the world population age distribution from the GBD 2019 study to standardize incidence, mortality and DALYs per 100,000 person-years for bladder cancer. We calculated the average annual percentage change (AAPC) to describe the overall temporal trend of count, crude rates and age-standardized rates (ASRs) for bladder cancer based on the following regression model. In the model, In(R) = α + β·T + ɛ, where R is count or rate, T is calendar year, α is the constant term, β is the regression coefficient, and ε is the random error term. The AAPC with its 95% confidence interval (CI) were derived from the formula of 100·(exp (β) − 1).16 If the AAPC and the lower boundary of 95% CI are both higher than 0, the index is considered to have an upward trend. If both the AAPC and the upper limit of 95% CI are less than 0, the estimated value is considered to have a downward trend. Otherwise, indicators are considered stable for a long time. The Joinpoint Regression Program (version 4.9.1.0) was applied to analyze temporal trend and AAPC of bladder cancer in China.
In order to predict the burden of bladder cancer by 2030, we first calculated age-specific rates for 18 five-year age groups (0–4 to >85 years) from 1990 to 2019 by gender. Then, the joinpoint regression model was used to find the year of significant changes in the trends of rate by the age group. For age groups without a statistically significant log-linear trend, we used the average value of 30 years as a value to forecast the future trend. For age groups showing a statistically significant trend with monotonicity, the predictive value will be calculated through the model. If the trend changed with multiple segments, we selected the model parameter of the last segment for prediction. Moreover, we multiplied the predicted age-specific rates and population prospects in each age group to obtain the number of cases. At last, we calculated ASRs by dividing the total cases and total populations for all ages. The main statistical analyses were implemented using R program (version 3.6.2).
Results
The Burden of Bladder Cancer in China at Present
In China, there were approximately 100,020 newly diagnosed bladder cancer patients in 2019. Among cases, there were 82,680 males and 17,339 females. The age-standardized incidence rate (ASIR) of bladder cancer in the total population was 5.16/100,000. Compared to females, males had a higher ASIR of bladder cancer (9.38/100,000 and 1.72/100,000). The number of deaths of bladder cancer in China was 40,094 with an age-standardized mortality rate (ASMR) of 2.23/100,000. The ASMR of bladder cancer for males was higher than that in females (4.29/100,000 and 0.88/100,000). Meanwhile, bladder cancer caused 816,119 DALYs in China and the age-standardized DALYs rate (ASDR) was 41.87/100,000. The ASDR of bladder cancer in males was about 4.5 times higher than that of females (Table 1).
 |
Table 1 The Number, Crude Rate, Age-Standardized Rate, and Changing Trend of Bladder Cancer Burden in China from 1990 to 2019 |
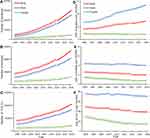
Figure 1 shows the incidence, mortality, and DALYs number and rate of bladder cancer in China by gender and age in 2019. The cases and DALYs for the males and females both reached a peak at 70–74 years old. However, there were differences between males and females for the age group with the highest number of deaths. The peak of death for males and females was 80–84 age group and over 85 years old, respectively. The number of incidence, deaths and DALYs in males were higher than those in females in every age group. The incidence, mortality and DALYs rates of bladder cancer increased with age. The age-specific rates of incidence, mortality and DALYs for males and females both reached a peak in the age group of 85 years (incidence: 173.75/100,000 and 23.91/100,000; mortality: 144.73/100,000 and 23.54/100,000; DALYs: 1290.91/100,000 and 195.59/100,000). Moreover, it can be seen that the highest incidence, deaths and DALYs were concentrated in the elderly population (≥65 years old).
 |
Figure 1 Numbers and rates of incidence cases (A), death (B) and DALYs (C) of bladder cancer by age and sex in 2019 in China. Abbreviation: DALYs, disability-adjusted life-years. |
Temporal Trends of Incidence, Mortality and DALYs of Bladder Cancer from 1990 to 2019
The new cases of bladder cancer increased from 25,548 in 1990 to 100,020 in 2019, with an AAPC of 4.72 (95% CI: 4.54, 4.89) in the total population. The ASIR of males increased significantly during 1990–2019 (AAPC=1.87, 95% CI: 1.65, 2.10). While the ASIR of females decreased significantly during this period, and the AAPC was −0.24 (95% CI: −0.46, −0.02). The ASIR in males was always higher than that in females. The deaths of bladder cancer increased significantly from 17,293 in 1990 to 40,094 in 2019, with an AAPC of 2.87 (95% CI: 2.63, 3.10). While the trend of ASMR was decreased significantly for the males (AAPC=−0.07, 95% CI: −0.13, −0.01) and females (AAPC=−1.75, 95% CI: −2.21, −1.31). The ASMR of females changed more significantly than that of males. The long-term trend for DALYs was similar to that of death except for the ASDR of males. There was not significantly changed for the ASDR of males from 1990 to 2019, with an AAPC of −0.15 (95% CI: −0.34, 0.03) (Table 1).
The trend for incidence, mortality, and DALYs rate of bladder cancer in China by gender in three age groups was shown in Figure 2. Significant increased in incidence was found in all age groups of males, with the AAPC of 3.57 (95% CI: 3.01, 4.10) and 2.34 (95% CI: 2.09, 2.59) and 1.83 (95% CI: 1.67, 2.10), respectively. However, these incidence trends were not found in the females. For mortality, females showed an obvious decline in all age groups. The AAPC of 15–49-year-old group was −2.22 (95% CI: −1.35, −3.08), 50–69-year-old group was −2.47 (95% CI: −2.06, −2.88), and over 70-year-old group was −1.23 (95% CI: −0.79, −1.68), respectively. While there was not any statistical significance of AAPC for the males. The trend of DALYs rate was similar to mortality for males and females in every age group. The incidence, mortality, and DALYs rate of males were always higher than that in females in all age groups. Meanwhile, with increasing age, the difference of incidence, mortality, and DALYs rate between males and females increased.
Proportions of DALYs for Bladder Cancer Attributable to Risk Factors
From 1990 to 2019, a considerable proportion of the DALYs of bladder cancer was attributable to two risk factors, including smoking (43.82–48.33%) and high fasting plasma glucose (5.29–7.38%). For these two risk factors, smoking was the most significant contribution to the DALYs in 2019 (Figure 3). The proportion of DALYs for bladder cancer attributable to smoking increasing with age, and reached a peak at 65–69 years old in both sexes. Moreover, the proportions of DALYs attributable to smoking for the males were always higher than that for females in every age group. High fasting plasma glucose was the other risk factor contributed to DALYs of bladder cancer. There were differences for the highest proportion age group between males and females. The highest proportion of high fasting plasma glucose for males and females was over 80 years old (8.41%) and 75–79 age group (7.76%), respectively. Except for the 60–69 age group, other age groups for the proportion of DALYs attributable to high fasting plasma glucose in males were higher than that of females.
 |
Figure 3 Proportions of DALYs for bladder cancer attributable to risk factors by age and sex in 2019. Abbreviation: DALYs, disability-adjusted life-years. |
Furthermore, the trend for proportions of DALYs attributable to risk factors of bladder cancer during 1990–2019 is shown in Figure 4. The largest contribution was smoking, with a relatively stable trend in males (AAPC=−0.02, 95% CI: 0.01, −0.05) and declined trend in females (AAPC=−0.28, 95% CI: −0.22, −0.35). On the contrary, there were upward trends for contributions of high fasting plasma glucose in both sexes (males: AAPC=0.85, 95% CI: 0.48, 1.22, females: AAPC=0.61, 95% CI: 0.35, 0.86).
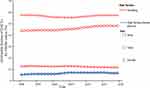 |
Figure 4 The trend of proportions of DALYs for bladder cancer attributable to risk factors by age and sex, from 1990 to 2019 in China. Abbreviation: DALYs, disability-adjusted life-years. |
Projection of Bladder Cancer Burden in China from 2020 to 2030
Based on GBD database of bladder cancer in China, we further predicted the numbers and age-standardized rate of incidence, mortality and DALYs between 2020 and 2030. In future years, the total number of bladder cancer in China both males and females will keep upward trend. By 2030, the overall incident cases, deaths and DALYs are predicted to increase to 150,372 and 53,520 and 1043,688, respectively. For males, incident cases will increase to 127,317 and ASIR will reach at 10.77/100,000 in 2030. While ASMR and ASDR of males are predicted to decline to 3.95/100,000 and 70.36/100,000, respectively. For females, the number of cases increases less than that of males, which will reach at 23,055 in 2030. In addition, due to population growth and aging, the ASIR, ASMR and ASDR of females all will show a slow decrease trend in the next decade, with 1.63/100,000, 0.75/100,000 and 14.90/100,000 in 2030, respectively. Both the numbers and age-standardized rate in males will consistently be higher than that in females from 2020 to 2030 (Figure 5).
Discussion
Bladder cancer is the 10th most common cancer in the world, which is one of the main malignant tumors threatening human health.17,18 This study used GBD 2019 data to analyze the current burden of bladder cancer in China and the trend from 1990 to 2019, and predicted the disease burden in 2030. In 2019, the ASIR and ASMR of bladder cancer in total population was 5.16/100,000 and 2.23/100,000, respectively. These results were higher than assessment data in 2015.19 The ASIR and ASMR were four to five times higher in males than in females. No matter the patients were males or females, the disease burden of bladder cancer increased with the age, and reached the peak in the age group over 85. Temporal trend analysis showed that the total cases and deaths of bladder cancer in 2019 is significantly higher than that in 1990. We further applied the joinpoint model to predict that the number of bladder cancer over the next decade. From 2020 to 2030, cases and deaths of bladder cancer will maintain upward trend, with the number of 150,372 and 53,520, respectively, in 2030. Above results all showed that bladder cancer is still a main disease burden in China. Therefore, effective preventive measures should be implemented to combat the prevalence of bladder cancer.
There were obvious disparities by gender in bladder cancer.20,21 Similar to the global epidemiological characteristics of bladder cancer, the burden of bladder cancer in China was significantly different between males and females. Currently, the main reason for this difference is smoking.22 There is a dose–response relationship between quantity or duration of smoking and the occurrence of bladder cancer.23 Smoking rate in males is higher than that in females, which causes higher the risk of bladder cancer. Females in areas with high smoking rates have a higher risk of bladder cancer than those in areas with low smoking rates. In addition, there are some phenomena, such as exposure to occupational risk factors of males, pregnancy or hormonal changes in females, which may cause the difference between the morbidity and mortality of males and females.24 Age is another major factor that causes the difference of bladder cancer burden in China. In this study, the incidence rate, mortality rate and DALYs rate of bladder cancer were at a low level before the age of 50, and these rates increased rapidly after the age of 50, reaching the highest in the age group over 85. This phenomenon was similar to the US.25 The possible reason for this situation was that the elderly were more often exposed to risk factors, and declined in physiological function and immunity in the meantime.26 Therefore, we should pay more attention to the physical fitness of elderly people, and enhance their awareness of cancer prevention at the same time. Especially for the elderly males, we can guide them to keep healthy living habits, which to reduce the risk of bladder cancer.
In recent years, the etiology of bladder cancer is still not clear. Therefore, the key to the prevention and treatment of bladder cancer is to find out the factors related to its occurrence and development. In this study, we used GBD database to analyze the relationship between smoking, high fasting plasma glucose and the burden of bladder cancer. Smoking was the most significant factor contribution to the DALYs of bladder cancer in 2019 in China, with 57.39% and 11.71% in males and females, respectively. The results were similar to study of worldwide, and East Asia is the region where DALYs is most attributed to smoking.4 One study had shown that the risk of bladder cancer among smokers was 2.5 times than that of non-smokers, and with the increasing in quantity or duration of smoking, the risk of bladder cancer also increased.27 Our country has formulated policies to control the smoking level of the population according to the standards of the World Health Organization.28 But the rate of smoking remained high with the growing population. From the current trend, it could be seen that the proportion of DALYs attributed to smoking remained stable. Therefore, it is the key to carry out some strict tobacco control measures in order to reduce the burden of bladder cancer. High fasting plasma glucose was the other factor contributed to DALYs of bladder cancer. From 1990 to 2019, the proportions of DALYs attributable to high fasting plasma glucose remained upward trend in both sexes. With the aging of the population, complications caused by high fasting plasma glucose will bring serious risks to health of the elderly.29 Therefore, we should strengthen the intervention of fasting plasma glucose, monitor the changes of it, and reduce the harm caused by hyperglycemia. Besides the above two factors, the burden of bladder cancer is affected by, for example, occupational exposure or history of bladder infection.30–32 Further study is warranted to find specific influencing factors.
For the burden of bladder cancer in China, we found that the temporal trend of ASIR of the total population was on the rise. On the contrary, the ASMR of the total population declined from 1990 to 2019. There may be three reasons to explain this phenomenon. Firstly, with the population expansion and urbanization, the incidence and mortality of bladder cancer in China are mild similar to developed countries, which change trends of ASIR and ASMR of common cancer are opposite.33 Secondly, in recent years, many areas have carried out early detection cancer programs. High-risk population of bladder cancer can be screened through screening programs or cohort studies. Patients can be found in the early stage of the disease and receive treatment before the illness worsens. Finally, advanced techniques are becoming more widely implied in bladder cancer clinical treatment.34,35 Personalized treatments also have already emerged in clinical practice. Multidisciplinary comprehensive therapy may be helpful to the prognosis of patients with bladder cancer. Whether or not other factors are associated with this characteristic warrant further investigations.
Our study has certain limitations. First, GBD database includes data from various sources. These data sources have different quality standard for registry-based data. There may be incompatibility among these data sources. Second, urothelial cell carcinoma is the most common pathological type of bladder cancer. We could not analyze the burden of this subtype at the present due to limited information in the GBD database. Lastly, the burden of bladder cancer attributable to other important risk factors, such as occupational exposure to aromatic amines or history of bladder infection, could not be investigated because the GBD database did not include the corresponding data. Although our study has above deficiencies, strengths of this study are it has large-scale and long-term cancer data. These data can well reflect the burden of bladder cancer in China.
Conclusions
In summary, we comprehensively analyze the burden of bladder cancer in China for 30 years through GBD database. Despite the decrease in ASMR and ASDR, the number of new cases and deaths increased and will further rise in the next decade years. The elderly are at high risk of this disease, with the highest incidence and mortality. Several established or potential risk factors can lead to an increase in the burden of bladder cancer. This important public health problem may be effectively solved through lifestyle intervention, early screening project, and updated treatment technology.
Abbreviations
GBD, Global Burden of Diseases; DALYs, disability-adjusted life-years; AAPC, average annual percentage change; ASRs, age-standardized rates; CI, confidence interval; ASIR, age-standardized incidence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate.
Acknowledgments
We would like to thank the works by the Global Burden of Disease Study 2019 collaborators.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Fujian Provincial Health Technology Project (Grant number: 2018-ZQN-17).
Disclosure
The authors declared no conflict of interests in this work.
References
1. Lenis AT, Lec PM, Chamie K, Mshs MD. Bladder cancer: a review. JAMA. 2020;324(19):1980–1991. doi:10.1001/jama.2020.17598
2. Saginala K, Barsouk A, Aluru JS, Rawla P, Padala SA, Barsouk A. Epidemiology of bladder cancer. Med Sci. 2020;8(1):15. doi:10.3390/medsci8010015
3. Lopez-Beltran A, Henriques V, Montironi R, Cimadamore A, Raspollini MR, Cheng L. Variants and new entities of bladder cancer. Histopathology. 2019;74(1):77–96. doi:10.1111/his.13752
4. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
5. Zi H, He SH, Leng XY, et al. Global, regional, and national burden of kidney, bladder, and prostate cancers and their attributable risk factors, 1990–2019. Mil Med Res. 2021;8(1):60. doi:10.1186/s40779-021-00354-z
6. Safiri S, Kolahi A-A, Naghavi M. Global, regional and national burden of bladder cancer and its attributable risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease study 2019. BMJ Glob Health. 2010;105(3):300–308. doi:10.1111/j.1464-410X.2009.09076.x
7. Shariat SF, Sfakianos JP, Droller MJ, Karakiewicz PI, Meryn S, Bochner BH. The effect of age and gender on bladder cancer: a critical review of the effect of age and gender on bladder cancer: a critical review of the literature. BJU Int. 2010;105(3):300–308. doi:10.1111/j.1464-410X.2009.09076.x
8. Ghadimi T, Gheitasi B, Nili S, Karimi M, Ghaderi E. Occupation, smoking, opium, and bladder cancer: a case-control study. South Asian J Cancer. 2015;4(3):111–114. doi:10.4103/2278-330X.173174
9. Cogliano VJ, Baan R, Straif K, et al. Preventable exposures associated with human cancers. J Natl Cancer Inst. 2011;103(24):1827–1839. doi:10.1093/jnci/djr483
10. Richters A, Aben K, Kiemeney L. The global burden of urinary bladder cancer: an update. World J Urol. 2020;38(8):1895–1904. doi:10.1007/s00345-019-02984-4
11. Kocarnik JM, Compton K, Dean FE, et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the global burden of disease study 2019. JAMA Oncol. 2022;8(3):420–444. doi:10.1001/jamaoncol.2021.6987
12. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi:10.3322/caac.21338
13. Liu X, Jiang J, Yu C, et al. Secular trends in incidence and mortality of bladder cancer in China, 1990–2017: a joinpoint and age-period-cohort analysis. Cancer Epidemiol. 2019;61:95–103. doi:10.1016/j.canep.2019.05.011
14. Xu H, Li K, Liang Y, Dong H, Chen Y. Analysis on incidence of bladder cancer in Guangzhou City and its trend from 2004 to 2016. Chin Cancer. 2019;28(12):913–917. doi:10.11735/j.issn.1004-0242.2019.12.A006
15. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/s0140-6736(20)30925-9
16. Yang X, Fang Y, Chen H, et al. Global, regional and national burden of anxiety disorders from 1990 to 2019: results from the global burden of disease study 2019. Epidemiol Psychiatr Sci. 2021;30:e36. doi:10.1017/S2045796021000275
17. Antoni S, Ferlay J, Soerjomataram I, Znaor A, Jemal A, Bray F. Bladder cancer incidence and mortality: a global overview and bladder cancer incidence and mortality: a global overview and recent trends. Eur Urol. 2017;71(1):96–108. doi:10.1016/j.eururo.2016.06.010
18. Wong M, Fung F, Leung C, Cheung W, Goggins W, Ng C. The global epidemiology of bladder cancer: a joinpoint regression analysis of its incidence and mortality trends and the global epidemiology of bladder cancer: a joinpoint regression analysis of its incidence and mortality trends and projection. Sci Rep. 2018;8(1):1129–1140. doi:10.1038/s41598-018-19199-z
19. Li H, Zheng R, Du L, et al. Prevalence and trend of bladder cancer in China. Zhonghua Zhong Liu Za Zhi. 2021;43(3):293–298. doi:10.3760/cma.j.cn112152-20200421-00362
20. Fajkovic H, Halpern JA, Cha EK, et al. Impact of gender on bladder cancer incidence, staging, and prognosis. World J Urol. 2011;29(4):457–463. doi:10.1007/s00345-011-0709-9
21. Dobruch J, Daneshmand S, Fisch M, et al. Gender and bladder cancer: a collaborative review of etiology, biology, and outcomes. Eur Urol. 2016;69(2):300–310. doi:10.1016/j.eururo.2015.08.037
22. Samanic C, Kogevinas M, Dosemeci M, et al. Smoking and bladder cancer in Spain: effects of tobacco type, timing, environmental tobacco smoke, and gender. Cancer Epidemiol Biomarkers Prev. 2006;15(7):1348–1354. doi:10.1158/1055-9965
23. Zhao X, Wang Y, Liang C. Cigarette smoking and risk of bladder cancer: a dose-response meta-analysis. Int Urol Nephrol. 2022;54(6):1169–1185. doi:10.1007/s11255-022-03173-w
24. Ferrís J, Garcia J, Berbel O, Ortega JA. Constitutional and occupational risk factors associated with bladder cancer. Actas Urol Esp. 2013;37(8):513–522. doi:10.1016/j.acuro.2013.01.001
25. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. doi:10.3322/caac.21551
26. Neuzillet Y, Geiss R, Caillet P, Paillaud E, Mongiat-Artus P. Epidemiological, pathological and prognostic characteristics of bladder cancer in elderly patients. Prog Urol. 2019;29(14):840–848. doi:10.1016/j.purol.2019.08.268
27. Cumberbatch MG, Rota M, Catto JW, La Vecchia C. The role of tobacco smoke in bladder and kidney carcinogenesis: a comparison of exposures and meta-analysis of incidence and mortality risks. Eur Urol. 2016;70(3):458–466. doi:10.1016/j.eururo.2015.06.042
28. Guo H. Tobacco control in China and the road to healthy China 2030. Int J Tuberc Lung Dis. 2020;24(3):271–277. doi:10.5588/ijtld.19.0106
29. Li W, Song F, Wang X, et al. Prevalence of metabolic syndrome among middle-aged and elderly adults in China: current status and temporal trends. Ann Med. 2018;50(4):345–353. doi:10.1080/07853890.2018.1464202
30. Pedroso TMA, Benvindo-Souza M, de Araújo Nascimento F, Woch J, Dos Reis FG. Cancer and occupational exposure to pesticides: a bibliometric study of the past 10 years. Environ Sci Pollut Res Int. 2022;29(12):17464–17475. doi:10.1007/s11356-021-17031-2
31. Jiang X, Castelao JE, Groshen S, et al. Urinary tract infections and reduced risk of bladder cancer in Los Angeles. Br J Cancer. 2009;100(5):834–839. doi:10.1038/sj.bjc.6604889
32. Scarselli A, Scanno P, Marinaccio A, Iavicoli S. Bladder cancer and occupational exposure: estimating the workers potentially at risk in Italy. Ann Ist Super Sanita. 2011;47(2):200–206. doi:10.4415/ANN_11_02_12
33. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1223–1249. doi:10.1016/S0140-6736(20)30752-2
34. Hu X, Li G, Wu S. Advances in diagnosis and therapy for bladder cancer. Cancers. 2022;14(13):3181. doi:10.3390/cancers14133181
35. Koimtzis G, Alexandrou V, Chalklin CG, et al. The role of adjuvant single postoperative instillation of gemcitabine for non-muscle-invasive bladder cancer: a systematic review and meta-analysis. Diagnostics. 2022;12(5):1154. doi:10.3390/diagnostics12051154
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.