Back to Journals » Clinical Ophthalmology » Volume 14
Telemedicine Follow-Up for Intravitreal Bevacizumab Injection in the Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP) Cohort
Authors Ji MH , Callaway NF , Greven MA, Vail D , Moshfeghi DM
Received 18 February 2020
Accepted for publication 16 April 2020
Published 29 April 2020 Volume 2020:14 Pages 1161—1163
DOI https://doi.org/10.2147/OPTH.S250361
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Marco H Ji,1 Natalia F Callaway,1 Margaret A Greven,2 Daniel Vail,1 Darius M Moshfeghi1
1Byers Eye Institute, Horngren Family Vitreoretinal Center, Department of Ophthalmology, Stanford University School of Medicine, Palo Alto, California; 2Department of Ophthalmology, Wake Forest University School of Medicine, Winston-Salem, North Carolina
Correspondence: Darius M Moshfeghi Tel +1 (650) 723-6995
Email [email protected]
Abstract: Telemedicine has emerged as a potential solution to face the disproportion between infants that need to be screened for retinopathy of prematurity (ROP) and the lack of ophthalmologists. We evaluated its utility in the follow-up after off-label intravitreal injection of bevacizumab. None of the treated infants ended up with bad anatomic outcome. Telemedicine is an alternative safe method to monitor patients after treatment.
Keywords: pediatric retina, retina, pediatric ophthalmology
Introduction
The discrepancy between the increasing screening population and the decreasing retinopathy of prematurity (ROP) workforce has raised concerns with the feasibility of binocular indirect ophthalmoscopy for every infant and telemedicine has emerged as a potential alternative to ensure all infants receive ROP screening efficiently while utilizing limited resources. Telemedicine applied to ROP screening has demonstrated feasibility, efficacy, and non-inferiority in pilot studies,1 medical outreach,2,3 and randomized clinical trials.4 It has been evaluated by the American Academy of Ophthalmology and found to be an useful adjunct.5 The Joint Statement screening guidelines for ROP validated its utility in the 2013 edition and reaffirmed it in the 2018 update.6 Historically, telemedicine has been used to screen at-risk infants for treatment intervention. Since telemedicine have been reported to be a reliable tool to screen infants for ROP, it is also a very promising technology for follow-ups after treatment with laser or injection of anti-VEGFs. Recently, we have demonstrated that telemedicine can be used to follow patients post-laser therapy to evaluate for progression to retinal detachment.7 With the recent shift to anti-VEGF therapy for ROP treatment, we reviewed our experience with telemedicine monitoring of post-anti-VEGF treated patients. In contrast to laser, injection of anti-VEGFs changes the natural history of ROP and requires continued surveillance for a longer interval to detect promptly recurrences or reactivations of disease that may occur even years after injection,8,9 with the highest risk between postmenstrual age 45 to 55 weeks.6 Reactivations or recurrences of ROP, if untreated, may progress to tractional retinal detachment despite early regression of the disease. The growing worldwide use of off-label anti-VEGF medications in ROP is expected to increase the already heavy burden of ophthalmologists who provide ROP care.
Patients and Methods
The Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP) is a community outreach telemedicine screening program for ROP in six intensive care units in northern California. Among this cohort, we investigated the baseline characteristics and follow-up data for infants who received intravitreal injection of bevacizumab (IVB). The study was conducted in accordance with the Health Insurance Portability and Accountability Act (HIPAA) and the tenets of the Declaration of Helsinki. Institutional Board Review (IRB 8752) at Stanford University School Of Medicine, which granted a waiver of consent for retrospective data analysis of the efficacy and outcomes. At our institution, IVB has been offered as treatment option for Type 1 ROP or AP-ROP in the appropriate clinical context since 2013.
Results
Among a total of 959 screened for ROP from November 30, 2013, to December 1, 2018, 26 infants out of 28 who presented with treatment warranted ROP (TW-ROP) underwent treatment with IVB. Among them, 7 patients were followed in clinic following treatment and discharge from the neonatal intensive care unit (NICU), whereas the remaining 19 infants were monitored with telemedicine until discharge from their respective NICU for an average of 6.83 (range 2–14) exams. The first Retcam exams were performed at a mean of 6.63 (range 1–37) days after primary injection and the last ones averaged 6.06 (range 0.86–13.57) weeks after treatment (Figure 1). At the outpatient follow-up, none of the infants treated with IVB developed bad anatomic outcome, including retinal detachment, macular fold and retrolental mass.
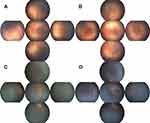 |
Figure 1 Color fundus photographs of Aggressive Posterior ROP at treatment (A) and at follow-up 1.5 months later (B); Type 1 ROP at treatment (C) and at follow-up 1.5 months later (D). |
Conclusion
The unpredictable course of the disease after anti-VEGFs urges strict and long-term follow-up in these infants. Telemedicine appears likely to be a safe method to monitor infants treated with anti-VEGF medications in the short term and has the potential to provide continued ROP care in resource limited settings.
Acknowledgments
This work was supported by the Heed Ophthalmic Foundation and Michels Fellowship Foundation awarded to Natalia F. Callaway, unrestricted grant from Research to Prevent Blindness, and NEI P30-EY026877.
Disclosure
DMM has the following disclosures: consultant for Akebia, Congruence, and Praxis UNS; Scientific Advisory Board: Allergan, Allegro, Clearside; Equity: dSentz, Grand Legend Technologies, Promisight, Versl, Visunex; Steering Committee/Data Monitoring Committee: Bayer, Genentech, Regeneron, Novartis, Iconic Therapeutics; Board of Director: 1800 Contacts, dSentz, Promisight, Versl, Linc, and Pr3vent. He also reports personal fees from Akebia, Bayer Pharma AG, Genentech, Novartis, Regeneron, and Shapiro Law Group, outside the submitted work; and runs the Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP) telemedicine network. NFC has the following disclosure: consultant for Genentec. The authors report no other conflicts of interest in this work.
References
1. Ells AL, Holmes JM, Astle WF, et al. Telemedicine approach to screening for severe retinopathy of prematurity. Ophthalmology. 2003;110(11):2113–2117. doi:10.1016/S0161-6420(03)00831-5
2. Wang SK, Callaway NF, Wallenstein MB, Henderson MT, Leng T, Moshfeghi DM. SUNDROP: six years of screening for retinopathy of prematurity with telemedicine. Can J Ophthalmol. 2015;50(2):101–106. doi:10.1016/j.jcjo.2014.11.005
3. Vinekar A, Gilbert C, Dogra M, et al. The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian J Ophthalmol. 2014;62(1):41–49. doi:10.4103/0301-4738.126178
4. Quinn GE, Ying G, Daniel E, et al. Validity of a telemedicine system for the evaluation of acute-phase retinopathy of prematurity. JAMA Ophthalmol. 2014;132(10):1178. doi:10.1001/jamaophthalmol.2014.1604
5. Fierson WM, Capone A. Telemedicine for evaluation of retinopathy of prematurity. Pediatrics. 2015;135(1):e238–e254. doi:10.1542/peds.2014-0978
6. Fierson WM. American academy of pediatrics section on ophthalmology, American academy of ophthalmology, American association for pediatric ophthalmology and strabismus, American association of certified orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2018;142(6):e20183061. doi:10.1542/peds.2018-3061
7. Greven MA, Moshfeghi DM. Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP): telemedicine-based examination after laser photocoagulation for treatment-warranted retinopathy of prematurity. Eye. 2019;10–12. doi:10.1038/s41433-019-0392-4
8. Ji MH, Moshfeghi DM, Callaway NF, et al. Retinopathy of prematurity reactivated 28 months after injection of ranibizumab. Ophthalmol Retin. 2019;3(10):913–915. doi:10.1016/j.oret.2019.06.017
9. Hajrasouliha AR, Garcia-Gonzales JM, Shapiro MJ, Yoon H, Blair MP. Reactivation of retinopathy of prematurity three years after treatment with bevacizumab. Ophthalmic Surg Lasers Imaging Retina. 2017;48(3):255–259. doi:10.3928/23258160-20170301-10
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
