Back to Journals » Advances in Medical Education and Practice » Volume 10
Targeted Enrollment of Medical Students for Rural China: Prospects and Challenges
Authors Hou J, Liang Y, Tong L, Kolars JC , Wang M
Received 13 August 2019
Accepted for publication 14 November 2019
Published 4 December 2019 Volume 2019:10 Pages 1021—1030
DOI https://doi.org/10.2147/AMEP.S227028
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Jianlin Hou,1 Yi Liang,2 Lang Tong,3 Joseph C Kolars,4 Minghao Wang5
1Institute of Medical Education & National Center for Health Professions Education Development, Peking University, Beijing 100083, People’s Republic of China; 2National Center for Poverty Alleviation Publicity and Education, State Council Leading Group Office of Poverty Alleviation and Development, Beijing 100101, People’s Republic of China; 3International Poverty Reduction Center in China, Beijing 100028, People’s Republic of China; 4University of Michigan Medical School, Ann Arbor, MI, USA; 5Institute of Agricultural Economics and Development, Chinese Academy of Agricultural Sciences, Beijing 100081, People’s Republic of China
Correspondence: Minghao Wang
Institute of Agricultural Economics and Development, Chinese Academy of Agricultural Sciences, Beijing 100081, People’s Republic of China
Tel +86 10 8210 9553
Fax +86 10 8210 9801
Email [email protected]
Purpose: Most countries are faced with the challenge of inadequate human resources for health in rural and remote areas. In China, approximately 41% of the total population reside in rural areas where there is a severe shortage of qualified practicing physicians. The Chinese government adopted a plan to strengthen the primary healthcare workforce by increasing enrollment of students from rural areas and providing free medical education. The purpose of this study is to examine the design and implementation of this plan in China, including its construct, outcomes, and challenges.
Methods: Three databases and Baidu were searched to find literature relating to targeted enrollment of medical students for rural China. Official government documents were also reviewed.
Results: Targeted enrollment of medical students from rural areas was implemented in 2010 throughout China. For example, under financial support from the Ministry of Finance, over 5000 5-year medical students per year were admitted from central and western China. Most graduates went to rural primary care settings to provide health services in accordance with their signed commitments to provide service as intended by the government. These medical school initiatives are faced with a number of challenges, including unfilled enrollment vacancies, low motivation to study among these students along with a reluctance to serve a rural population, and unguaranteed job opportunities.
Conclusion: Targeted enrollment of medical students and free medical education in exchange for obligatory services contribute to improve the allocation of physicians in rural China. However, there are opportunities to improve the design and implementation of these programs. This review of the approach taken in China may be informative to other countries in their efforts to address the shortage of health professionals in rural and remote areas.
Keywords: targeted enrollment, rural oriented medical students, medical education, rural areas, human resources for health, China
Introduction
The shortage of physicians in rural areas is a serious global problem, resulting in limited access to health care by rural residents. In India, the number of physicians per 1000 population is reported at 0.69 for rural communities, compared with 1.33 for urban areas.1 A considerably lower physician–population ratio was also observed in rural Germany.2 In the United States and Canada, only 11% or less of physicians practice in rural areas where 20% of the population resides.3,4 It is important to increase the pool of future physicians who are more likely to practice in rural areas.2
A substantial component of the Chinese population resides in rural areas distributed over approximately 32,000 townships. Although urbanization is decreasing the population in rural areas, 577 million people resided in the rural areas of China as of 2017. With economic reform and rapid globalization, China’s economy has grown substantially for the past 40 years. When compared with urban populations, rural residents have received fewer benefits of this modernization and lag behind in health status in part because of reduced access to health resources. For example, the neonatal mortality rate and infant mortality rate in rural areas were, respectively, 5.7 and 9.0 per 1000 live births in 2016, which is twice the rate observed in urban areas. The number of health professionals in urban areas per 1000 population was nearly three times of that of rural areas in 2017. Furthermore, only 21.8% of health professionals and 23.1% of physicians worked in rural areas although rural citizens accounted for 41.5% of the China’s total population.5
Maldistribution of China’s health professionals favoring urban over rural areas has resulted in serious disparity issues. While there is a severe shortage of practicing physicians in rural areas, the opportunities for physician employment in urban areas are limited resulting in the diversion of graduates into non-medical fields or unemployment in these densely populated cities. The density of physicians was 3.9/1000 population in urban areas, yet only 1.6/1000 in rural areas.5
In China, the duration of medical education programs ranges from 3 to 8 years, leading to a secondary school (i.e. Zhong Zhuan), junior college (i.e. Da Zhuan), undergraduate, master, or doctorate degree. On average, physicians in rural areas have spent less time in education programs resulting in weaker performance competencies and outdated professional knowledge.6,7 Over 50% of the physicians practicing at rural township health centers have not been educated beyond secondary schools which is problematic as township health centers are considered a major component of the three-tier rural health services system which includes country hospitals and village health stations.8 Some township health centers, especially those in the central and western regions, have no licensed physicians. To make matters worse, there has been a decreasing trend in the number of practicing rural doctors, causing concerns about workforce retention.9 The unwillingness to pursue careers in rural health care delivery systems are similar to reasons observed in other countries, including low social recognition, unclear pathways for career development, and the lack of effective incentive and reinforcement mechanisms, which make it difficult for rural health entities to attract and retain qualified healthcare practitioners.10–12 Also, the tuition fees of those choosing to become doctors are higher than many other professions, which dissuades students, especially those in rural areas, to study Medicine.
To address the rural health workforce storage, the Chinese government adopted the “Plan for Developing Primary Health Care Workforce with a Focus on General Practitioners” jointly issued by the National Development and Reform Commission and five other ministries in March 2010. This plan emphasized strengthening the primary healthcare workforce through increasing enrollment of students from rural areas and providing free medical education for these students who commit to serving the rural population for at least 6 years after graduation (hereafter referred to as rural-oriented students).13
Under financial supports from the Ministry of Finance, this plan resulted in over 5000 medical students per year admitted from rural areas in 23 provinces across central and western China. As one of the biggest initiatives in the world to increase rural doctors, it has the potential of substantively improving the allocation of physicians in rural China and generating informative implications for other developing countries in their efforts to address the shortage of health professionals in rural and remote areas. Although this plan was implemented in 2010, few publications in international peer-reviewed journals provide an overall description of the plan’s design and implementation. To address this knowledge gap, we examine the design and implementation of this plan in China, including its construct, outcomes, and challenges. Finally, we provide a discussion of policy suggestions to further improve the plan with potential implications for other developing countries.
Methods
A database search using China National Knowledge Infrastructure (CNKI), Wanfang Data, and PubMed MEDLINE was performed using the search terms “targeted enrollment”, “rural-oriented medical students” for students from rural areas, and “tuition-waived medical student” combined with the terms “medical education” and “China”. Included articles were published in Chinese or English since 2010 when the policy was first issued. Baidu, a search engine based in China, was used to find works of literature relating to the plan. Official documents on the targeted enrollment of rural-oriented medical students issued by China’s government sectors were also reviewed.
Results
The free medical education for rural-oriented students was initiated and aimed to cultivate physicians in general practice at grassroots health institutions in rural areas. Every year, provincial departments of health, with inputs from other related departments, determine the areas of greatest need for employment, the number of necessary health positions, and the overall matriculation of medical students required for the following year to be in accordance with local development plans for the rural health workforce. Provincial departments of education, in consultation with the provincial departments of health and departments of development and reform, also choose the schools to facilitate this development plan. The provincial department of health and department of education jointly sign education agreements with these selected schools, which encourages and supports graduates of the development plan to work at grassroots health entities. This support includes, but is not limited to, providing free medical education tuition as well as the necessary work-place and living conditions.9
Enrollment
Medical students in the program are grouped and selected into either 5-year undergraduate or 3-year junior college (i.e. training beyond secondary school) schools. The targeted enrollment, in accordance to the policy, is integrated with the annual enrollment plans of participating colleges and universities.9 In the first several years, applicants from rural areas enjoyed priority admission, and those from urban areas were also eligible for the program. However, in the beginning in 2016, the Ministry of Education policies stipulate that the national plan only accepts applicants from rural areas.14–16 For each major preference, there are specific entrance score requirements for the students who take the national college entrance examination (CEE). Before admission into the program, medical students are also required to sign a targeted employment agreement with their county’s departments of health and higher education institution.9 This ensures that their registered residency is based on their rural hometown, even while attending school.
Education
Students who participate in this program select either clinical medicine or traditional Chinese medicine (TCM) as their majors. The students who are unable to graduate are required to return tuition fees that were subsidized or waived. Students in the program take classes that are tailored for rural students. However, they are also allowed to take the regular courses as well. According to the needs of rural health, their colleges and universities are asked to develop appropriate teaching plans, strengthen general medicine education, emphasize practical teaching, highlight the training of clinical skills, and appropriately increase time for teaching TCM or ethnomedicine as well as family planning skills.9,17
Preferential Treatment
Through this program, medical students do not need to pay tuition or accommodation fees, and they are offered financial aids for living expenses. The amount of financial aid provided to students is determined by provincial authorities and the funds are financed by the provincial health budget; however, the amount cannot be lower than the national grant disbursements. The central government pledges to train one 5-year medical graduate specializing in general practice for every township health center in central and western China. This resulted in 5000 pledges in the year 2010. The Ministry of Finance provides a financial aid of 6000 yuan (i.e. 900 in 2018 US dollars) per student per year to offset the students’ living expenses.9,18
To ensure a smooth transfer from graduation to employment, in May 2015, the National Health and Family Planning Commission (now the National Health Commission) and five other ministries jointly issued “Suggestions on Further Improving Free Education of Rural Oriented Medical Students”, in which six favored policies were suggested in regard to professional title promotion, salaries, training, retention, and re-employment. The new policy dictates that graduates of the program can be promoted to a medium-grade professional title 1 year in advance and benefit from more lenient requirements on foreign language competences and article publications. With this new policy, the important contributors for professional title promotions rely on improving the volume of clinical receptions, quality of service, and patient satisfaction. Those who obtain a certificate of standardized residency training are prioritized to the general practitioner (GP) special post project. Furthermore, these graduates receive additional professional training so that they can continue to enhance their skills and ability. For those who prefer to stay in the primary health care entities at the end of their service period, employers can ensure that they continue to use and benefit from these established policies.19
Obligatory Service in Rural Areas
Ultimately, all graduates from the program will return to rural areas and work as primary health care providers for 6 years in keeping with targeted employment agreements (i.e. employment contracts), used to manage and outline their roles and responsibilities. During the service period, as defined by the contract, the graduates are allowed to change their employers among rural grassroots health entities within a province. Those who fail to complete their obligatory service are required to return their deducted or waived tuition fees and pay a penalty fee for breaching the agreement. In addition, the breach of agreement will be recorded on a publicized personnel and integrity file, which will be regulated by the provincial departments of health. After finding employment, the graduates also need to participate in the standardized training for general practitioners and pass the national licensing examination for physicians or assistant physicians.9
Implementation
Since 2010, the targeted enrollment of rural-oriented medical students has been implemented across China. Proposed enrollment in the national plan increased from 5000 in 2010 to 6700 in 2019. The majors for these students became more diversified with the inclusion of some ethnic traditions, such as Mongolian medicine, Tibetan medicine, and Uygur medicine (Tables 1 and 2).20–22 From 2010 to 2014, the proportion of students who were admitted with their first preference as medical training comprised of about 95% of the entire applicant pool, of which rural students accounted for over 70% each year.
 |
Table 1 Proposed Enrollment of Medical Students into Rural Practice Supported by the Ministry of Finance: 2010–2019 |
 |
Table 2 Proposed Enrollment in the National Plan by Province and Major: 2019 |
Expansion
Following the implementation of the national plan, some provinces and prefectures, especially those in eastern China (e.g. Jiangsu, Guangdong, Liaoning, and Shandong), have also adopted their own plans for targeted enrollment of rural-oriented medical students according to the economic and educational situation in their own region. Since 2009, Jiangsu province has invested 118 million yuan (i.e. 18 million in 2018 US dollars) for the program from provincial finances and has cultivated 3936 medical professionals to become rural primary health providers.23 In Guangdong province, the planned enrollment of rural-oriented students was 400 per year between 2014 and 2016 and 1000 per year between 2017 and 2018.24 These graduates are expected to go to work at township health centers or village health stations. Liaoning province planned to enroll 65–70 3-year rural-oriented medical students for its township health centers in 2016, followed by 90 students in 2017 and 100 students in 2018. Shandong province decided to annually enroll 1000 5-year rurally oriented medical students between 2017 and 2022 and 300 3-year rural-oriented medical students between 2019 and 2023. Colleges or universities are provided with a subsidy of 10,000 yuan (i.e. 1500 in 2018 US dollars) per student per year from provincial finance.25–27
Challenges
Despite providing many beneficial policies to increase rural-oriented medical school enrollment, the number of students did not meet the projected estimate, and the CEE scores of the admitted students were not satisfactory in certain provinces. In Anhui province of central China, as shown in Table 3, vacancies in the enrollment plan were not completely filled, and in some cases, some enrolled students refused to sign the agreement.28 In Guangdong province of eastern China, 116 out of 1000 vacancies in the enrollment plan were left unfilled in 2017.29 Reasons for this student short-fall could be potentially attributed to missed deadlines or the lack of desire to work in a rural area. However, despite these vacancies, many colleges and universities are unwilling to fill the gaps by lowering the required entrance score in order to prevent compromising the quality of enrolled students.24 Meanwhile, admitted students’ true preference to serve a rural population is of concern because most of them chose to study in the program owing to some external factors, such as low CEE scores, guaranteed job opportunities, free medical education and financial aids, or the opinion of their parents or teachers.30–33 Those who chose to study in the program out of their own personal motivation to serve the rural population accounted for less than 15% of the medical students.24
 |
Table 3 Enrollment Vacancy of Rural-Oriented Medical Students in Anhui Province of Central China: 2010–2013 |
Since rural-oriented and other medical students have different learning motivations, differences in curriculum and pedagogy should be considered. Most educational institutions have created a modular curriculum for the rural-oriented medical students and added modules or courses pertaining to general practice. However, these curricula are typically inadequate in terms of integrating current medical models of care with a rural health focus. While the pedagogy for some courses has been updated to be more hands-on (through problem-based, case-based, and simulation learning), most courses, especially clinical ones, still overly rely on didactic lectures.15 Although the program aims to cultivate physicians for general practice, a nationwide survey of 19 schools found that, on average, there were only two courses on general practice and credit hours for general practice courses only accounted for 2.5% of the total credit hours.34
Because rural-oriented medical students are required to work at specific types of health entities, they not only lose the pressure to find employment but also lose the opportunity to pursue research or choose their specific location of practice. In many cases, this may lead to lower motivation to study and higher absenteeism from class. Examination score statistics shows that rural-oriented students have lower average scores than medical students not in the program.35 Furthermore, rural-oriented students are characterized as having an increasingly negative attitude toward the program as they progress in the curriculum,36 lower self-acceptance,37 and higher learning burn-out rates.22
Although oriented medical students are expected to work in rural areas, many of them are reluctant to serve that population. A survey of rural-oriented medical students in Guangxi autonomous region of western China showed that only 34.7% of respondents were willing to work in rural health care systems.38 In Shaanxi province of western China, 92.6% of the 230 first-cohort students had the intention of breaking the contract and only 1.3% of them intended to continue working in rural areas after the contract expired.39 Similarly, only 7.8% of 1200 rural-oriented students in Xinjiang autonomous region intended to continue their careers in rural areas at the end of their service period.40 The conditions in rural areas are important factors that often discourage graduates from working there. These include unpromising career development, low wages and welfare, harsh living conditions, sub-optimal schooling for their children, poor working circumstance, out-of-date scientific research equipment, and lagging cultural lifestyle opportunities.28,34,41
According to a survey of the first 500 rural-oriented medical graduates in the Sichuan province of western China, 65 (13.0%) of graduates paid the penalty and completed the relevant procedures for breach of agreement as of 2016. The main reasons for breaching the agreement included choosing to study for a master's degree, being offered a position in a comprehensive hospital, or leaving the healthcare sector to pursue individual business activities or independent entrepreneurship.42 Also, during the transition from graduation to employment, several government entities are involved to connect the graduates to an employer. However, due to a lack of clear management and effective coordination, this may lead to graduates facing unguaranteed job opportunities.
Career Determination and Effects on Rural Physician Workforce
The first cohort of medical students in the program graduated in 2013. Most graduates went to rural primary care entities to provide health services in accordance with their signed agreement. Approximately 90% of the more than 10,000 rural-oriented graduates between 2015 and 2016 found a job at township health centers.43 A survey of four medical schools in three provinces found that 90.7% of rural-oriented medical graduates between 2015 and 2016 went to work at township health centers, compared with only 2.8% of other five-year medical graduates who were not in the program.24 The compliance rate for rural placement was 86.1% between 2015 and 2017 at one college in Anhui province.44 As of August 2017, 37,000 five-year medical graduates of the national plan meant that the central government nearly achieved the goal of training one 5-year medical graduate for every township health center in central and western China.45 The program contributes to increasing the number of rural physicians and relieving the shortage of health professionals in rural China. From 2013 to 2017, the total number of rural physicians increased from 1,435,000 to 1,612,000, with an annual increase of about 35,000. The number of rural physicians per 1000 population rose from 1.5 to 1.7 in the same period (Figure 1). The increase in the number of rural physicians was accompanied with a decrease in unmet demand for health care.46
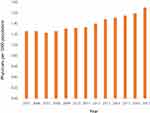 |
Figure 1 Number of physicians per 1000 population in rural China: 2005–2017.53 Notes: Data from National Health Commission of the People's Republic of China. China Health Statistical Yearbook 2018. |
Discussion
Targeted enrollment of medical students and free medical education in exchange for obligatory services have helped to relieve the shortage of physicians in rural China. However, it is still necessary for educational institutions, government entities, and employers to closely cooperate with each other to improve some key elements of the program, including enrollment, education, employment, and career development. In order to attract more students to this program, further publicization of these opportunities and relevant policies needs to occur in order for students to be appropriately informed. For students currently in the program, other incentives and reinforcement mechanisms should be established to encourage motivation.
The program should also consider further integrating rural education and training into the curriculum because rural exposure before graduation is an important factor in motivating medical students to work in rural areas.47 For example, it may be necessary to add courses on rural customs and practices to help students better understand the nature of primary health care in these rural areas. Education on diseases and treatments that are common in rural areas should also be strengthened.
To increase rural employment and retention, polices have been promoted for rural-oriented medical graduates regarding salaries, professional title promotion, in addition to supportive working and living conditions. It is important to ensure these policies are fully implemented. However, the government should also consider issuing additional policies for the graduates, such as providing them with increased opportunities for training at large hospitals and helping them achieve individual career goals. Along with strategies that to increase the placement of medical school graduates in rural areas, strengthening of the rural health system will require an increase in the remuneration of rural doctors to reduce the salary gap between urban and rural primary care providers. Furthermore, other policies should be issued to encourage the bidirectional flow of general practitioners between urban and rural areas.
Although there is a growing consensus in China that the education of doctors should require at least 5 years of undergraduate medical education, this program to enhance rural placements also admits 3-year junior college students. According to China’s Practicing Physician Law, 5-year and 3-year medical graduates are, respectively, eligible to obtain a practicing physician license or an assistant physician license after passing the corresponding licensing examinations.48 Prescriptions from an assistant physician should be signed by a physician to become effective although there are exceptions for those practicing at township or village health settings.49 Although 3-year medical graduates are more likely to practice and stay in rural areas than 5-year graduates, there are concerns about social justice to patients they care for because urban providers seldom hire 3-year graduates and thus urban populations may enjoy better medical services than their rural counterparts.
Most countries, especially developing ones, are faced with the challenge of inadequate numbers of qualified health professionals practicing in rural and remote areas.50 The targeted enrollment of rural-oriented medical students throughout China may be informative to other developing countries in their efforts to address this issue. On one hand, the plan is a combination of evidence-based measures in improving the allocation of health professionals in rural and remote areas, including enrollment of students with a rural background, tuition fees waived or reduced medical education, education provided by local medical schools, obligatory service in rural areas, and policies encouraging rural employment and retention.25,51 The implementation of the plan itself reflects the good translation of study to practice and from academic research to policy. The strong leadership and support of the Chinese government is key to ensure the successful implementation of the plan throughout the country. Indeed, the Chinese government plays an indispensable role in this effort by initiating the plan, providing financial supports, organizing the enrollment of students, and issuing supporting policies. Substantive cooperation among relevant government sectors is also important to the design and implementation of this policy. Therefore, it may be government instead of market forces that should play a bigger role in addressing the shortage of health professionals in rural and remote areas.
Conclusion
As one of the biggest programs for the production of rural doctors in the world, targeted enrollment of medical students and free medical education in exchange for obligatory services contribute to improving the allocation of physicians in rural China. Meanwhile, it is still necessary to improve some key procedures of these educational initiatives, including enrollment, education, employment, and career development. The design and implementation of the policy may be informative to other countries in their efforts to address the shortage of health professionals in rural and remote areas.
Abbreviations
CEE, college entrance examination; CNKI, China National knowledge Infrastructure; GP, general practitioner; TCM, traditional Chinese medicine.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Author Contributions
The first draft was produced by JH and YL under the guidance of MW. LT and JK made substantial contributions to revising the manuscript critically. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Ahmad A, Chang J, Khan M, et al. Can Pharmacy Doctors act as valuable assets in rural areas with a physician shortage?. J Res Pharm Pract. 2014;3(4):109–111. doi:10.4103/2279-042X.145345
2. Kuhn B, Kleij KS, Liersch S, et al. Which strategies might improve local primary healthcare in Germany? An explorative study from a local government point of view. BMC Fam Pract. 2017;18(1):105.
3. Shankar PR, Dubey AK, Nandy A, et al. Student perception about working in rural United States/Canada after graduation: a study in an offshore Caribbean medical school. F1000Research. 2015;3:301. doi:10.12688/f1000research.5927.2
4. Islam N. The dilemma of physician shortage and international recruitment in Canada. Int J Health Policy Manage. 2014;3(1):29–32. doi:10.15171/ijhpm.2014.53
5. National Bureau of Statistics of China. National Yearly Data[EB/OL]. Available from:: http://data.stats.gov.cn/easyquery.htm?cn=C01.
6. Long SL. Rural grass-root health professionals in China: current situation, influential factors, and suggestions. J Med Theo Pract. 2013;7:878–879. doi:10.19381/j.issn.1001-7585.2013.07.018. (in Chinese).
7. Jiang ZH, Wang SZ. Analysis of issues and measures related to rural health manpower in China. J Jiang’xi Trad Chin Med Sch. 2013;3:77–79. doi:10.3969/j.issn.1005-9431.2013.03.026. (in Chinese).
8. Gu DN, Zhang ZM, Zeng Y. Access to healthcare services makes a difference in healthy longevity among older Chinese adults. Soc Sci Med. 2009;68(2):210–219. doi:10.1016/j.socscimed.2008.10.025
9. Liu JY. Investigation on Current Status of Chinese Rural Doctors in 2010. Peking Union Medical College; 2011. (in Chinese).
10. Wei Y, Duan RJ, Bao GX, et al. Analysis on the current status and issues of rural health workforce in Jiangsu province. Mod Prev Med. 2015;45(2):269–272. (in Chinese).
11. Ren S, Liu L, Jiang QC, et al. An analysis of current situation and problems on Chinese rural health human resources. Chin Health Serv Manage. 2013;12:912–914, 955. (in Chinese).
12. Dong SX, Proochista A, Xiao X. An investigation of Chinese rural doctors’ job quit intention: empirical analysis of income satisfaction, hospital organization satisfaction and doctor-patient relationship. Econ Rev. 2013;2:30–39. doi:10.19361/j.er.2013.02.004. (in Chinese).
13. The Central People’s Government of the People’s Republic of China. Notice about issuing suggestions on launching free cultivation Program of Rural-Oriented Medical Students “[EB/OL]. Available from: http://www.gov.cn/zwgk/2010-06/08/content_1623025.htm.
14. General Office of Ministry of Education of China. Notice on enrolling rural oriented medical undergraduate students for middle and western areas with financial support from the central government, 2016. [EB/OL]. Available from: http://www.moe.gov.cn/srcsite/A08/moe_740/s3864/201605/t20160531_247111.html.
15. General Office of Ministry of Education of China. Notice on enrolling rural oriented medical undergraduate students for middle and western areas with financial support from the central government, 2017. [EB/OL]. Available from: http://www.moe.gov.cn/srcsite/A08/moe_740/s3864/201705/t20170527_305984.html.
16. General Office of Ministry of Education of China. Notice on enrolling rural oriented medical undergraduate students for middle and western areas with financial support from the central government, 2018. [EB/OL]. Available from: http://www.moe.gov.cn/srcsite/A08/moe_740/s3864/201805/t20180509_335479.html.
17. Xiong CH, Jiang LL, Yang XM. Comparison of the education scheme of rural order directed medical students in 6 colleges and universities. J Bengbu Med Coll. 2018;43(10):1393–1396. (in Chinese).
18. Xiong CH, Yang XL, Qi YM. Current situation and thoughts about rural oriented free medical students in China. China Higher Med Educ. 2016;1:59–60. doi:10.3969/j.issn.1002-1701.2016.01.030. (in Chinese).
19. Tang C. Solutions for difficulties for oriented students to work in grass-root health entities. China Hosp CEO. 2015;12:38–39. (in Chinese).
20. General Office of Ministry of Education of China. Notice on enrolling rural oriented medical undergraduate students for middle and western areas with financial support from the central government, 2015. [EB/OL]. Available from: http://old.moe.gov.cn/publicfiles/business/htmlfiles/moe/s7955/201503/185039.html.
21. General Office of Ministry of Education of China. Notice on enrolling rural oriented medical undergraduate students for middle and western areas with financial support from the central government, 2015. [EB/OL]. Available from: http://old.moe.gov.cn/publicfiles/business/htmlfiles/moe/s7955/201503/185039.html.
22. General Office of Ministry of Education of China. Notice on enrolling rural oriented medical undergraduate students for middle and western areas with financial support from the central government, 2014. Available from: http://old.moe.gov.cn//publicfiles/business/htmlfiles/moe/s3864/201404/167227.html.
23. Bao YY. Study on free cultivation model of rural-oriented medical students in Jiangsu province—taking Nanjing University of Chinese Medicine as example. Chin Mod TCM Distance Educ. 2015;13(2):91–93. doi:10.3969/j.issn.1672-2779.2015.02.048 (in Chinese).
24. Health Commission of Guangdong Province, Development and Reform Commission of Guangdong Province, Department of Education of Guangdong Province, Department of Finance of Guangdong Province, Department of Human Resources and Social Security of Guangdong Province, Administration of Traditional Chinese Medicine of Guangdong Province. Notice on targeted enrollment of rural oriented medical students, 2014–2018. (in Chinese).
25. Organization Department of CPC committee of Shandong Province, Health Commission of Shandong Province, Office of the Public Sector Reform Commission of Shandong Province, Development and Reform Commission of Shandong Province, Department of Education of Shandong Province, Department of Finance of Shandong Province, Department of Human Resources and Social Security of Shandong Province. Measures on strengthening the development of grass-root health workforce in Shandong Province. 2018[EB/OL]. Available from: http://www.sdwsjs.gov.cn/ywdt/xwtt/201805/t20180531_1337329.html.
26. Health Commission of Shandong Province, Office of the Public Sector Reform Commission of Shandong Province, Development and Reform Commission of Shandong Province, Department of Education of Shandong Province, Department of Finance of Shandong Province, Department of Human Resources and Social Security of Shandong Province, Administration of Traditional Chinese Medicine of Shandong Province. Implementation measures on free medical education in Shandong Province. 2017 [EB/OL]. Available from: http://www.sdwsjs.gov.cn/wzxxgk/tzwj/201702/t20170214_581543.html.
27. Health Commission of Shandong Province, Office of the Public Sector Reform Commission of Shandong Province, Development and Reform Commission of Shandong Province, Department of Education of Shandong Province, Department of Finance of Shandong Province, Department of Human Resources and Social Security of Shandong Province, Administration of Traditional Chinese Medicine of Shandong Province. Implementation measures on free medical education for junior college students in Shandong Province. 2018 [EB/OL]. Available from: http://www.sdwsjs.gov.cn/wzxxgk/tzwj/201810/t20181023_1738924.html.
28. Zhu CB, Wang WR, Chen JZ, et al. Research on rural oriented free medical students training program from the perspective of risk. J Qiqihar Med Coll. 2014;35(9):1362–1363. (in Chinese).
29. Health Commission of Guangdong Province, Department of Education of Guangdong Province, Department of Human Resources and Social Security of Guangdong Province, Administration of Traditional Chinese Medicine of Guangdong Province. Notice on targeted enrollment of rural oriented medical students. [EB/OL]; 2015. Available from: http://zwgk.gd.gov.cn/006940132/201508/t20150814_609058.html.
30. Li WM, Shu QQ, Chen WF, et al. Study on learning intention and influencing factors of rural demand-oriented junior medical students in Yunnan province. Soft Sci Health. 2018;32(5):70–73. doi:10.3969/j.issn.1003-2800.2018.05.018 (in Chinese).
31. Yang L, Li MJ, Zhang H. Analysis on the work willingness of rural order tuition-free medical students under the background of “healthy China” . J Chongqing College Electron Eng. 2018;27(3):83–86. doi:10.13887/j.cnki.jccee.2018(3).21 (in Chinese).
32. Chen KX, Xu SJ, Tao YS, et al. The relationship among professional commitment, academic self-efficacy and learning burnout in rural order-targeted medical students. J Bengbu Med Coll. 2018;43(10):1397–1400. doi:10.13898/j.cnki.issn.1000-2200.2018.10.030 (in Chinese).
33. Hu D, Chen CK, Zhang C, et al. Effectiveness and challenges of targeted admission medical education program in rural China. Chin J Health Policy. 2018;11(9):28–33. doi:10.3969/j.issn.1674-2982.2018.09.005 (in Chinese).
34. Li YH, Hao T, Chen LZ. Medical science undergraduate free training programs specifically designed for rural practice in China. Chin General Pract. 2018;21(16):1989–1992, 1997. doi:10.3969/j.issn.1007-9572.2018.16.017. (in Chinese).
35. Liu Z. Analysis on current status of oriented medical students. Chongqing Med J. 2012;41(16):1668–1670. doi:10.3969/j.issn.1671-8348.2012.16.042. (in Chinese).
36. Zhang TJ, Li YJ. Study on rural-oriented medical students’ acceptance of major and analysis on influencing factors. J Chifeng Univ (Nat Sci Ed). 2018;32(7):106–109. doi:10.13398/j.cnki.issn1673-260x.2018.07.037. (in Chinese).
37. Xie YT, Deng SQ, Shi MH, et al. The status of self-acceptance of rural order oriented medical students and the effect on social comparison. Chin Health Serv Manage. 2018;10:754–755. (in Chinese).
38. Pan XY, Nong HH, Li FL. Survey on the employment intention of oriented free Medical Students in Guangxi Medical Schools to Rural Primary Health Institution. China Rural Health. 2012;Z2:522–523. (in Chinese).
39. Liu JL, Zhang K, Mao Y. Attitude towards working in rural areas: a cross-sectional survey of rural-oriented tuition-waived medical students in Shaanxi, China. BMC Med Educ. 2018;18(1). doi:10.1186/s12909-018-1209-z
40. Li YH, Tang XL, Chen LZ. Analysis on rural-oriented medical undergraduate students’ attitude toward employment in Xinjiang. China Higher Med Educ. 2018;8:43–44. doi:10.3969/j.issn.1002-1701.2018.08.021 . (in Chinese).
41. Cai Y, Liu BZ, Zhou Y, et al. Interview and analysis on the training of Chongqing rural order oriented medical students. Chin J Med Educ Res. 2018;17(7):753–756. doi:10.3760/cma.j.issn.2095-1485.2018.07.023. (in Chinese)
42. Chen JP, Deng HY. Discussion on the reasons and countermeasures for defaulting of oriented free medical students. Lab Med Clin. 2016;13(13):1897–1899. (in Chinese).
43. Dong LWL. Primarily establishing a standardized medical education system with Chinese characteristics: medical education reform makes big progress in China. China Education Daily. 2017 July 11. (in Chinese).
44. Ding NN, Liu F, Zhao R, et al. Investigation and analysis on performance status of order-oriented free medical graduates in rural areas. J Bengbu Med Coll. 2018;43(10):1390–1392. doi:10.13898/j.cnki.issn.1000-2200.2018.10.028 (in Chinese).
45. Bai JF. The number of health professionals steadily increased. People’s Daily. 2018 August 16. (in Chinese).
46. Statistical Information Center, National Commission of Health and Family Planning of China. The Fifth National Health Services Survey Analysis Report. Beijing: Peking Union Medical College Press; 2015. (in Chinese).
47. Budhathoki SS, Zwanikken PA, Pokharel PK, Scherpbier AJ. Factors influencing medical students’ motivation to practise in rural areas in low-income and middle-income countries: a systematic review. BMJ Open. 2017;7:e013501. doi:10.1136/bmjopen-2016-013501
48. Office of National Laws of the Standing Committee of China’s National People’s Congress, Department of Policy and Regulation of Ministry of Health of China, Department of Medical Affairs of Ministry of Health of China. Interpretation of the Practicing Physician Act of the People’s Republic of China. Beijing: China Democracy and Regulation Press; 1998. (in Chinese).
49. Ministry of Health of China. Prescription Management Regulation, 2007 [EB/OL]. Available from: http://www.gov.cn/flfg/2007-03/13/content_549406.htm.
50. Liu J, Zhu B, Mao Y. Association between rural clinical clerkship and medical students’ intentions to choose rural medical work after graduation: a cross-sectional study in western China. PLoS ONE. 2018;13(4):e0195266. doi:10.1371/journal.pone.0195266
51. World Health Organization. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations, 2010 [EB/OL]. Available from: http://www.who.int/hrh/retention/guidelines/en/. (
52. Zhu C, Wang W, Chen J, Wu X. Research on rural oriented free medical students training program from the perspective of risk. J Qiqihar Med Coll. 2014;9:1362–1363. (in Chinese).
53. National Health Commission of the People's Republic of China. China Health Statistical Yearbook 2018. Beijing: Peking Union Medical College Press, 2018. Chinese.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
