Back to Journals » Clinical Pharmacology: Advances and Applications » Volume 15
Systematic Review of Safety of RTS,S with AS01 and AS02 Adjuvant Systems Using Data from Randomized Controlled Trials in Infants, Children, and Adults
Authors Yihunie W , Kebede B, Tegegne BA , Getachew M , Abebe D , Aschale Y, Belew H , Bahiru B
Received 15 December 2022
Accepted for publication 7 March 2023
Published 14 March 2023 Volume 2023:15 Pages 21—32
DOI https://doi.org/10.2147/CPAA.S400155
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Arthur E. Frankel
Wubetu Yihunie,1 Bekalu Kebede,1 Bantayehu Addis Tegegne,1 Melese Getachew,1 Dehnnet Abebe,1 Yibeltal Aschale,2 Habtamu Belew,2 Bereket Bahiru3
1Department of Pharmacy, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia; 2Department of Medical Laboratory Science, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia; 3Department of Pharmacy, College of Medicine and health sciences, Bahir Dar University, Bahir Dar, Ethiopia
Correspondence: Wubetu Yihunie, Department of Pharmacy, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia, Tel +251 910112391, Email [email protected]
Background: Emergence of antimalarial drugs and insecticides resistance alarms scientists to develop a safe and effective malaria vaccine. A pre-erythrocytic malaria vaccine called RTS,S has made great strides.
Aim: The review was aimed to assess the safety of the candidate malaria vaccine RTS,S with AS01 and AS02 adjuvants using data from Phase I–III randomized controlled clinical trials (RCTs).
Methods: This systematic review was conducted based on PRISMA 2020. Regardless of time of publication year, all articles related with safety of RTS,S, RCTs published in the English language were included in the study. The last search of databases, and registry was conducted on 30 May, 2022. Pubmed, Google Scholar, Cochrane Library, Wiley Online Library, and Clinical trials.gov were thoroughly searched for accessible RCTs on the safety of RTS,S malaria vaccine. The studies were screened in three steps: duplicate removal, title and abstract screening, and full-text review. The included studies’ bias risk was assessed using the Cochrane risk of bias tool for RCTs. This systematic review is registered at Prospero (registration number: CRD42021285888). The qualitative descriptive findings from the included published studies were reported stratified by clinical trial phases.
Findings: A total of thirty-five eligible safety studies were identified. Injection site pain and swelling, febrile convulsion, fever, headache, meningitis, fatigue, gastroenteritis, myalgia, pneumonia, reactogenicity, and anemia were the most commonly reported adverse events. Despite few clinical trials reported serious adverse events, none of them were related to vaccination.
Conclusion: Most of the adverse events observed from RTS,S/AS01 and RTS,S/AS02 malaria vaccines were reported in the control group and shared by other vaccines. Hence, the authors concluded that both RTS,S/AS01 and RTS,S/AS02 malaria vaccines are safe.
Keywords: RTS,S/AS01, RTS,S/AS02, safety, systematic review, randomized controlled trials
Introduction
Malaria cases increased from 227 million in 2019 to 241 million in 2020. In the same year, 627000 malaria-related deaths were estimated. Sub-Saharan Africa accounts for the majority of cases and fatalities. Plasmodium falciparum is the most lethal of the five Plasmodium parasite species that cause human malaria.1 To prevent infection, reduce morbidity, and treat malaria, World Health Organization (WHO) recommends use of vector control, chemoprevention, diagnostic testing, and treatment.2
The bulk of pesticides is now ineffective against mosquitoes, putting malaria prevention efforts in jeopardy.3 In addition, Plasmodium parasites become resistant to the antimalarial drugs that are now available. The use of antimalarial drugs kills sensitive plasmodium parasites leaving resistant ones. Hence, resistance plasmodium parasites could be passed on to succeeding people and cause antimalarial drug resistance.4,5 Making malaria vaccinations is thus one way to eradicate the disease.6 RTS,S is the pre-erythrocytic malaria vaccine candidate that has currently made the most strides.7,8
GlaxoSmithKline (GSK) and the Walter Reed Army Institute of Research (WRAIR) developed the RTS,S malaria vaccine in 1987. The National Institutes of Health and WRAIR discovered the genetic structure of the CSP antigen, sequenced it, and created a genetic clone.9–12 The C terminals of the CSP were added, which carry epitopes for both B and T cells, and the Hepatitis B surface antigen was used as a CSP carrier matrix for the NF54 strain of P. falciparum.13 The “R” in the RTS,S vaccine is the core repeat region, which is made up of one chain of N-acylneuraminate-9-phosphatase (NANP) amino acid tandem repeat tetrapeptides. T cells’ immunodominant segregated epitopes and hepatitis B surface antigen are represented by the letters “T” and “S”, respectively.14–16 These antigens were created by expressing a genetically altered yeast strain in Saccharomyces cerevisiae yeast cells that already contained a “S” expression cassette. As a result, the strain produced RTS and S at a 1:4 ratio.17
Researchers at GSK exposed the RTS,S vaccine to a broad variety of adjuvants, and nearly every one of them was successful. RTS,S had been tested with a variety of adjuvants like ASO2A, which is a combination of oil-in-water emulsion (AS02, AS03),18 and AS01, which is the combination of QS-21, liposomes, and Monophosphoryl lipid A (MPL).19
Any vaccine candidate must have its safety profile evaluated by pre-clinical and clinical trial investigations before being approved for human use. This systematic review aimed to provide updated information on the safety of RTS,S/AS01 and RTS,S/AS02 malaria vaccines. In order to investigate the safety of the RTS,S/AS01 and RTS,S/AS02 malaria vaccines, this systematic review looked at papers from phases I, II, and III of randomized controlled trials (RCT) in infants, children, and adults.
Methods
This complete overview of the key findings from the studies carried out to assess the safety of the RTS,S malaria vaccine with AS01 and 02 adjuvants was provided by the systematic review, which was conducted based on PRISMA 2020.20 (Supplementary File 1).
Prospero Registration and Amendments to the Protocol
Eligibility Criteria
Inclusion Criteria
Study setting: This study incorporated researches conducted world wide.
Study units: The study included studies on the safety of RTS,S with AS01 and AS02 adjuvants.
Publication status: The research included published articles.
Language: In this review, researches written in English were incorporated.
Study type: RCTs were included.
Publication year: Regardless of time of publication year, all articles related with safety of RTS,S with AS01 and AS02 adjuvants were included.
Type of article: In this review, only full-text articles were included.
Exclusion Criteria
The analysis rejected studies that did not report the safety of RTS,S with AS01 and AS02 adjuvants, were not available in full text, were not published in English, and were conducted in vitro or on animals.
Information Sources
The last search of databases and registry was performed on 30 May 2022 EC. The studies were discovered using databases such as Pubmed, Google Scholar, Cochrane Library, Wiley Online Library, and Clinical trials.gov registry.
Search Strategy
The articles were searched by WY, BK, BA, MG, DA, YA, HB, and BH using the keywords of (“RTS” OR “RTS,S” OR “RTS,S/AS01” OR “RTS,S/AS02” OR “RTS,S/SBAS2” AND “Vaccine” OR “malaria vaccine” OR “Vaccination” OR “Vaccines” OR “Malaria vaccines’). The same search strategy was used on all the databases.
Risk of Bias Assessment
The Cochrane risk of bias tool for RCTs21,22 was used to evaluate the quality of the included studies. Procedures such as the randomization process, deviations from the intended interventions, measurement of the outcome data, gaps in the outcome analysis, and reported result selection.
Data Selection, and Collection Process
The search results were first filtered using the study title and abstract followed by full texts. The chosen studies were scanned in accordance with the inclusion criteria before the finished papers were included in this review. Reference lists of pertinent publications were also looked through in order to locate further applicable studies. All of the duplicates were removed, but if more than one published study was found on the same current trial, they were all included because the outcomes were evaluated differently in each published study. The finalized articles, were independently screened and extracted the pertinent information. In the screened studies, disagreements were discussed and resolved. Data extraction was done using Microsoft Excel 16 and tables were created using Microsoft Word.
Data Items (Outcomes)
All results related to safety of RTS,S malaria vaccine with AS01 and AS02 adjuvants were sought for screening.
Results
Systematic Search and Study Characteristics
A literature search on different databases and registry (1st April –30th May 2022) yielded a total of 4118 articles. 118 articles were sought after reviewing the titles and abstracts of the articles. Further 83 articles were removed after a full-length review. Finally, 35 RCTs were selected to be included in the review (Figure 1).
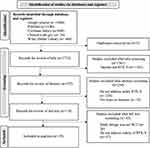 |
Figure 1 Flow diagram of the study selection to assess the safety of RTS,S malaria vaccine. Notes: PRISMA figure adapted from Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. Syst Rev. 2021;10(1):89. Creative Commons.20 |
All of the 35 articles, were studies on RCTs categorized under phases I, I/II, II, III clinical trials with 3 (8.57%), 4 (11.43%), 21 (60.00%), and 7 (20.00%) studies respectively. The studies were conducted on RTS,S/AS01 (16 studies), RTS,S/AS02 (14 studies), and on both vaccines simultaneously (5 studies). The majority of the studies were conducted in Sub-Saharan Africa followed by USA, UK, and Belgium with a total of 26, 927 infants, children and adults. (Table 1)
 |
Table 1 Characteristics of the Included Randomized Controlled Clinical Trial Studies on the Safety of RTS,S |
Quality Assessment
The studies that we used underwent a quality assessment. All of the selected studies had low risks of selection, performance, detection, and reporting biases due to the proper execution of these RCTs, which included the randomization process, deviations from the intended interventions, measurement of the outcome data, gaps in the outcome analysis, and reported result selection. In conclusion, the included studies had high methodological quality and a small likelihood of bias (Figure 2).
 |
Figure 2 Risk of bias assessment of the studies, RTS,S. |
Safety Results of RTS,S/AS01 and RTS,S/AS02
The safety profiles of RTS,S/AS01 and RTS,S/AS02 were examined and published in a total of 35 articles. Each vaccination schedule was well-tolerated and had respectable safety profiles. The RTS,S/AS01 and RTS,S/AS02 safety results have been divided into Phase I, phase I/II, Phase II, and Phase III clinical trials for convenience of understanding. Adverse events reported by over two studies were categorized under clinical trial phases and summarized in Table 2. (Table 2)
 |
Table 2 Commonly Reported Adverse Events Reported by Studies Following RTS,S/AS01 and RTS,S/AS02 Administration |
Safety of RTS,S from Phase I and Phase I/II Clinical Trial Studies
All phase I and Phase I/II clinical trials aimed to study the safety of RTS,S were conducted on AS02 (formerly called SBAS2) adjuvant system. A total of 7 phase I and phase I/II studies were conducted on 564 children aged 1–11 years and 183 adults in USA, Belgium, Gambia, Mozambique, and Kenya. (Table 1)
Kester et al23,24 demonstrated that none of the immunization schedules were found to have caused any major adverse events. The incidence of local and general solicited symptoms was not statistically different between the RTS,S/AS02 and control groups, according to phase I and phase I/II clinical studies carried out in Sub-Saharan African nations, the United States, and Belgium. The local symptoms that were most frequently reported were discomfort and/or edema at the injection site.23–29 Additionally, myalgia was the most often reported general complaint in the Phase 1 investigation, according to Kester et al29 Further, Aide et al28 found that participants in both RTS,S/AS02 and control groups reported upper respiratory tract infections. Furthermore, Bojang et al27 showed that headache and fever were more frequently reported in the RTS,S/AS02 group as compared to control vaccine.
Safety of RTS,S from Phase II Clinical Trial Studies
Both RTS,S/AS01 and RTS,S/AS02 were the subject of phase II clinical trials to examine the safety of the RTS,S malaria vaccine. Phase II clinical trials constituted the majority of the studies examining the safety of RTS,S. (Table 1)
RTS,S/As01
A number of phase II clinical trials were conducted in Sub-Saharan Africa (Gabon, Kenya, Tanzania, Gana, and Malawi), USA (in Walter Reed Army Institute of Research (WRAIR)), and in United Kingdom. (Table 1)
Majority of the studies revealed that all vaccination regimens were well tolerated. The proportions of solicited and unsolicited AEs reported following each dosage of the vaccination were comparable between groups. There were no known vaccine-related serious adverse events (SAEs) or suspected unanticipated significant adverse events. No serious adverse event was determined to be linked to vaccination, and no individual incident occurred with a greater incidence that was clinically significant as compared to the control group in the RTS,S/AS01 vaccine group.30–36
Moreover, the majority of the studies indicated that injection site adverse effects were the most frequently reported solicited local AEs and considered causally related to vaccination.30,31,34,37,38 In addition, Lusingu et al35 reported that drowsiness and loss of appetite were occasionally reported and similar in both RTS,S/AS01, and rabies vaccine groups. Phase II clinical trials conducted on adults in the USA, and UK showed that fatigue and headache,30,31 feverishness, malaise, and myalgia31 were the most frequently reported solicited general AEs. Moreover, Agnandji et al38 found fever was reported more frequently in participants who received RTS,S/AS01 with EPI vaccines, measles, and yellow fever vaccines compared with participants who received EPI vaccines, measles, and yellow fever vaccines without RTS,S/AS01, respectively. Furthermore, studies conducted in Sub-Saharan Africa showed that serious adverse events reported during the study period were pneumonia,35,37 febrile convulsion,32,35,37 gastroenteritis,35,37 P. falciparum malaria,35,37 and upper respiratory tract infections.35
On the other hand, fewer people in the RTS,S/AS01 group than in the rabies group, according to Olotu et al,37 experienced at least one severe adverse event. Three seizures were documented within one month of vaccination, according to Agnandji et al;38 two occurred in RTS,S/AS01 (0, 1, 7) group individuals, and one occurred in a control group subject. In addition, anemia was recorded as a significant adverse event that happened with a similar frequency across groups, according to studies by Asante et al32 and Lusingu et al.35
RTS,S/As02
A total of 7 Phase II clinical trials to study the safety of RTS,S/AS02 were conducted, 3 studies in Mozambique,39–41 2 studies in Gambia,42,43 1 study in each Tanzania44 and USA45 with a total participant of 6527 of whom 340 infants, 5829 1–4 years children and 358 adults. (Table 1)
The malaria vaccine RTS,S/AS02 demonstrated good safety profiles, according to a Phase II experiment conducted by Kester et al45 on the 0, 1, and 3 month and 0, 7, and 28 day immunization schedules. Additionally, other investigations carried out in Sub-Saharan Africa revealed that no fatality or significant adverse event was thought to be connected to vaccination.39,40,42–44 Moreover, numerous investigations revealed that throughout the four-day follow-up period in both cohorts and overall doses, discomfort and/or swelling at the injection site was the most commonly reported local adverse event.40,42,44,45
Additionally, Bojang et al42 and Kester et al45 found that the RTS,S/AS02 group experienced headache more frequently than the control group did. Moreover, Alonso et al40 found that fever, irritability, sleepiness, and anorexia were more common in the RTS,S/AS02 group as compared to the control. Furthermore, Abdulla et al44 found that in both the RTS,S/AS02 and hepatitis B vaccine groups, pneumonia, gastroenteritis, and anemia were the most commonly reported adverse events; though none of the serious adverse effects were linked to vaccination.
RTS,S/AS01 vs RTS,S/AS02
A total of 5 safety studies were conducted in both RTS,S/AS01 and RTS,S/AS02 in Gabon, Kenya, Gana, USA, and Belgium with 720 children and 429 adults.(Table 1) A study of RTS,S/AS01 and RTS,S/AS02 in USA and Ghana by Kester et al46 and Owusu-Agyei et al47 indicated that both vaccines had acceptable safety profiles. On the other hand, different phase II RCT studies on RTS,S/AS01 and RTS,S/AS02 in 1113 children and adults in Gabon, Kenya, Gana, and USA showed that pain and swelling were reported more commonly on RTS,S/AS02 than RTS,S/AS01.14,46–49 Furthermore, a research by Polhemus et al49 on healthy individuals in Kenya revealed that the RTS,S/AS01 and RTS,S/AS02 vaccines had a higher incidence of discomfort and edema than the control. In addition, Leroux-Roels et al14 found that incidences of AEs tended to be lower in RTS,S without the adjuvant system as compared with the adjuvanted vaccine. Furthermore, myalgia which was reported by participants in RTS,S/AS01 group, went away after two days.14
Fatigue and headache were the most often reported general AEs in both groups, according to other investigations by Kester et al46 and Leroux-Roels et al14 conducted in Kenya and the USA. Additionally, Owusu-Agyei et al47 found that fever was reported by participants in RTS,S with both AS01 and AS02 adjuvant systems. Although; deviations of normal hematological and biochemical values were recorded, no grade 3 abnormalities were seen.48 Moreover, Owusu-Agyei et al47 and Leroux-Roels et al14 reported no AEs that were clinically significant alterations in clinical laboratory values.
Safety of RTS,S from Phase III Clinical Trials
Phase III clinical studies on RTS,S/AS01 including 16,521 infants and children were carried out in Sub-Saharan Africa on 16, 521 infants and children. An equal percentage of participants in both the RTS,S/AS01, and the control group reported at least one major adverse event. Overall, both immunization groups had few grade 3 solicited adverse events with similar incidence.50–52
As other phase I and II clinical trial studies, in phase III studies, pain at the RTS,S/AS01 injection site was the most frequently reported AE.50,52,53 A Phase III clinical trial on infants and children by the RTS,S Clinical Trials Partnership,54 conducted in eleven locations across seven African countries, revealed that meningitis of any cause was reported as a serious adverse event in infants more frequently in participants in the RTS,S/AS01 group as compared to the control group. In addition, the studies indicated that meningitis was also recorded as a SAE in both age groups.54 Meningitis occurred more frequently in the RTS,S/AS01 group compared to the control group, although not being temporally linked to vaccination. Meningitis cases were also significantly imbalanced between the RTS,S/AS01 and control groups among children, but not in infants.53,55,56
A Safety study of RTS,S/AS01 in HIV- positive infants and children by Otieno et al,52 revealed that meningitis was more commonly reported in the RTS,S/AS01 than the control in children as compared to infants.
A study conducted by the RTS,S Clinical Trials Partnership53 showed that one of the significant adverse events recorded that was thought to be connected to a study vaccine and more common in the older age group was seizure. Another study by Otieno et al,51 revealed that among the most common serious adverse events in both RTS,S/AS01, and rabies-vaccine recipients was febrile convulsions, with similar events noted in both groups. Furthermore, a study done on HIV-infected infants and children by Otieno et al52 revealed febrile convulsion was reported more commonly in children taking RTS,S/AS01 than the control and it was judged to be associated with vaccination. It also reported that a higher number of deaths was seen in RTS,S/AS01 vaccinated female participants as compared with the control; though it was not observed in males.52
Studies conducted in sub-Saharan African countries showed that pyrexia was another serious adverse event, reported more frequently in the RTS,S/AS01 group than the control group more in children than infants.50,53 In addition, the RTS,S Clinical Trials Partnership53 indicated that Myositis was reported as a serious adverse event in children and it was thought to be connected to vaccination.
In a study carried out in Kenya by Otieno et al51 reported that the most frequent major adverse events were pneumonia and gastroenteritis, with equal percentage of occurrences reported in both groups. Furthermore, Asante et al50 showed that upper respiratory tract infections and diarrhea were reported in the RTS,S coad, RTS,S alone, and Control groups in children; however, none of these events were linked to the study vaccine.
A study conducted in seven sub-Saharan countries revealed that the RTS,S/AS01 booster dose was more reactogenic than the comparator vaccine in both children and young infants.55 Different studies indicated that RTS,S/AS01 vaccine was more reactogenic than the control.51,53,54
Discussion
Antimalarial drugs, and insecticides resistance, pave the way for malaria to claim hundreds of thousands of lives each year, calling attention to develop safe, and effective vaccines.1,3–5 Among different malaria vaccine candidates, RTS,S, is the pre-erythrocytic vaccine that is most progressed.8 Studying the safety of vaccines has to be given high priority at all stages of vaccine development.57 Therefore, This systematic review was aimed to assess the safety of RTS,S with AS02 and AS01 adjuvant systems from RCT studies. RCTs would eliminate concerns about confounding factors, both known and unknown.58
An adverse event following immunization (AEFI), such as an unpleasant or unexpected sign, abnormal laboratory test findings, symptoms, or disease, is an indicator of the safety of a vaccine.59 Unpleasant effects of vaccines can be ascribed to vaccines themselves and their components.60 As a result, it is a must to ensure the safety of the RTS,S malaria vaccine before its approval.
This study tried its best to qualitatively describe the safety of RTS,S malaria vaccine with AS01 and AS02 adjuvant systems from the 35 published RCTs. As a result, the review found that RTS,S/AS01 and RTS,S/AS02 vaccines are safe to humans. Moreover, in most RCT studies, the reported AEFI were comparable between RTS,S and the control. The common AEFI were injection‐site pain and swelling, febrile convulsion, fever, headache, meningitis, fatigue, gastroenteritis, myalgia, pneumonia, reactogenicity, and anemia. Injection site pain and/or swelling was the most frequently reported local symptom in all vaccine groups. Four studies conducted in seven sub-Saharan countries revealed that the RTS,S/AS01 three dose and booster dose was more reactogenic than the comparator rabies vaccine in both children and young infants51,53–55 These adverse effects are also common to other types of vaccines as identified in the investigational phase of clinical trials.58
No matter what components are in a vaccination, all vaccines generate some level of inflammation at the injection site, which is likely to contribute to the symptoms of pain, redness, and swelling. When pyrogenic chemicals are released into the systemic circulation, a series of immunological and neurological system interactions are thought to be activated, including an increase in body temperature.61
Furthermore, in this systematic review, AEs were reported more commonly with the adjuvanted antigen than with the unadjuvanted RTS,S. This demonstrates that adjuvants have their own adverse events. Moreover, studies confirmed that adjuvants are immunostimulants that enhance the immune response to the antigen.62,63
Vaccine antigens set up an immune response that may provide specific disease protection. Immune system stimulation results in a complicated cascade of innate immunological processes, including as phagocytosis, the creation of inflammatory mediators like chemokines and cytokines, complement activation, and cellular recruitment. These inflammatory reactions followed immune system stimulation may lead to the development of signs and symptoms of injection-site reaction (pain, redness, and swelling) in the vaccinated person. The mediators and products of inflammation in the circulation may have systemic negative effects, such as fever, weakness, and headache.61 Fever was reported more frequently in participants who received RTS,S/AS01 in combination with EPI vaccines and measles and yellow fever vaccines compared with participants who received EPI vaccines and measles and yellow fever vaccines alone, respectively.38 This may be due to additive adverse effect of combination of vaccines.
Different phase II RCT studies on RTS,S/AS01 and RTS,S/AS02 in 1113 children and adults in Gabon, Kenya, Gana, and USA showed that pain and swelling were reported more frequently on RTS,S/AS02 than RTS,S/AS01.46–49 Furthermore, AS01’s immunogenicity superiority to AS02,64–66 this strengthened to prefer RTS,S/AS01 to RTS,S/AS02 for further studies (phase III clinical trials8 and pilot implementation67).
In addition, a study carried out on HIV-positive children reported that a higher number of deaths was seen in female children taking RTS,S/AS01 compared with female children in the control group; though it was not observed in male children.52 Furthermore, this was supported by other studies.68,69
A pilot implementation of the four-dose schedule of RTS,S/AS01 was started in Gana, Malawi and Kenya in 2019 to further characterize vaccine safety in the context of a routine immunization program, paying special attention to the safety signals observed in the Phase III trial (meningitis, cerebral malaria, excess mortality in female compared to male children).68 No proof of a connection between the RTS,S/AS01 vaccination and the three potential safety signals from phase III clinical trials was discovered, according to the report.70,71 Following the findings of favorable safety and efficacy profiles from the RTS,S/AS01 malaria vaccine pilot program in Ghana, Kenya, and Malawi, WHO recommended that the RTS,S/AS01 be used widely among children in Sub-Saharan Africa and other regions with moderate to high P. falciparum malaria transmission.72
Strengths and Limitations
This study covered the assessment of the safety of RTS,S with both AS01 and AS02 adjuvant systems in infants, children and adults world-wide. Moreover, it included all RCTs from Phase I–III. However, we have not access to some search engines due to lack of subscription by our affiliate university. In addition, some articles were not full-text and were rejected.
Conclusion
This systematic review was conducted using data from randomized controlled trials. Most of the adverse events observed from RTS,S/AS01 and RTS,S/AS02 malaria vaccines were also shared by other vaccines. Moreover, the safety signals (meningitis, cerebral malaria, excess mortality in female compared to male children), from phase III clinical trials were chance only. Hence, the authors concluded that both RTS,S/AS01 and RTS,S/AS02 malaria vaccines are safe.
Amendments to the Protocol
See Supplementary File 2.
Abbreviations
AE, Adverse Events; AEFI, Adverse Events Following Immunization; CSP, Circumsporozoite protein; GSK, GlaxoSmithKline; NANP, N-acylneuraminate-9-phosphatase; WRAIR, Walter Reed Army Institute of Research; WHO, World Health Organization.
Data Sharing Statement
Unless there are legal or ethical reasons to the contrary, the data will be made available upon request from the corresponding author.
Disclosure
The authors declared that they have no competing interests.
References
1. World Health Organization. World malaria report 2021. Geneva, Switzerland; 2021.
2. World Health Organization. Global technical strategy for malaria 2016–2030; 2015.
3. World Health Organization. Emergency response to artemisinin resistance. regional framework for action 2013–2015; 2013.
4. White NJ. Antimalarial drug resistance. J Clin Invest. 2004;113:1084–1092.
5. Klein EY Antimalarial drug resistance. A Dissertation Presented to the Faculty of Princeton University in Candidacy for the Degree of Doctor of Philosophy Princeton University; 2012.
6. Moorthy VS, Newman RD, Okwo-Bele JM; Malaria Vaccine Technology Roadmap. Malaria vaccine technology roadmap. Lancet. 2013;382(9906):1700–1701.
7. March S, Ng S, Velmurugan S, et al. A microscale human liver platform that supports the hepatic stages of Plasmodium falciparum and vivax. Cell Host Microbe. 2013;14(1):104–115.
8. World Health Organization. Malaria vaccine development; 2016.
9. Han L, Hudgens MG, Emch ME, et al. RTS,S/AS01 malaria vaccine efficacy is not modified by seasonal precipitation: results from a phase 3 randomized controlled trial in Malawi. Sci Rep. 2017;7:7200.
10. Cohen J, Nussenzweig V, Vekemans J, Leach A. From the circumsporozoite protein to the RTS,S/AS candidate vaccine.Human Vaccines. 2010;6(1):90–96. doi:10.4161/hv.6.1.9677
11. Kaslow DC, Biernaux S. RTS,S: toward a first landmark on the malaria vaccine technology roadmap. Vaccine. 2015;33(52):7425–7432. doi:10.1016/j.vaccine.2015.09.061
12. Shehzad A, Lee J, Lee YS. Autocrine prostaglandin E 2 signaling promotes promonocytic leukemia cell survival via COX-2 expression and MAPK pathway. BMB Reports. 2015;48(2):109–114. doi:10.5483/BMBRep.2015.48.2.081
13. Shehzad A, Parveen S, Qureshi M, Subhan F, Lee YS. Decursin and decursinol angelate: molecular mechanism and therapeutic potential in inflammatory diseases. Inflam Res. 2018;67(3):209–218. doi:10.1007/s00011-017-1114-7
14. Leroux-Roels G, Leroux-Roels I, Clement F, et al. Evaluation of the immune response to RTS,S/AS01 and RTS,S/AS02 adjuvanted vaccines.Human Vaccines Immunother. 2014;10(8):2211–2219. doi:10.4161/hv.29375
15. Bojang KA. RTS,S/AS02A for malaria. Expert Rev Vaccines. 2006;5(5):611–615. doi:10.1586/14760584.5.5.611
16. Didierlaurent AM, Collignon C, Bourguignon P, et al. Enhancement of adaptive immunity by the human vaccine adjuvant AS01 depends on activated dendritic cells. J Immunol. 2014;193:1920–1930.
17. Gordon DM, McGovern TW, Krzych U, et al. Safety, immunogenicity, and efficacy of a recombinantly produced Plasmodium falciparum circumsporozoite protein–hepatitis B surface antigen subunit vaccine. J Infect Dis. 1995;171(6):1576–1585.
18. Shehzad A, Qureshi M, Anwar MN, Lee YS. Multifunctional curcumin mediate multitherapeutic effects. J Food Sci. 2017;82:2006–2015.
19. Wang Z-B, Xu J. Better adjuvants for better vaccines: progress in adjuvant delivery systems, modifications, and adjuvant-antigen codelivery. Vaccines. 2020;8:128.
20. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
21. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
22. Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142.
23. Kester KE, McKinney DA, Tornieporth N, et al. Efficacy of recombinant circumsporozoite protein vaccine regimens against experimental Plasmodium falciparum malaria. J Infect Dis. 2001;183(4):640–647.
24. Kester KE, McKinney DA, Tornieporth N, et al. A phase I/IIa safety, immunogenicity, and efficacy bridging randomized study of a two-dose regimen of liquid and lyophilized formulations of the candidate malaria vaccine RTS,S/AS02A in malaria-naive adults. Vaccine. 2007;25(29):5359–5366.
25. Macete EV, Sacarlal J, Aponte JJ, et al. Evaluation of two formulations of adjuvanted RTS,S malaria vaccine in children aged 3 to 5 years living in a malaria-endemic region of Mozambique: a phase I/IIb randomized double-blind bridging trial. Trials. 2007;8(1):1.
26. Macete E, Aponte JJ, Guinovart C, et al. Safety and immunogenicity of the RTS,S/AS02A candidate malaria vaccine in children aged 1–4 in Mozambique. Trop Med Int Health. 2007;12(1):37–46.
27. Bojang KA, Olodude F, Pinder M, et al. Safety and immunogenicity of RTS,S/AS02A candidate malaria vaccine in Gambian children. Vaccine. 2005;23(32):4148–4157.
28. Aide P, Aponte JJ, Renom M, et al. Safety, immunogenicity and duration of protection of the RTS,S/AS02D malaria vaccine: one year follow-up of a randomized controlled phase I/IIb trial. PLoS One. 2010;5(11):e13838.
29. Kester KE, Heppner DG, Moris P, et al. Sequential Phase 1 and Phase 2 randomized, controlled trials of the safety, immunogenicity and efficacy of combined pre-erythrocytic vaccine antigens RTS,S and TRAP formulated with AS02 Adjuvant System in healthy, malaria naive adults. Vaccine. 2014;32(49):6683–6691.
30. Moon JE, Ockenhouse C, Regules JA, et al. A phase IIa controlled human malaria infection and immunogenicity study of RTS,S/AS01E and RTS,S/AS01B delayed fractional dose regimens in malaria-naive adults. J Infect Dis. 2020;222(10):1681–1691.
31. Rampling T, Ewer KJ, Bowyer G, et al. Safety and efficacy of novel malaria vaccine regimens of RTS,S/AS01B alone, or with concomitant ChAd63-MVA-vectored vaccines expressing ME-TRAP. NPJ Vaccines. 2018;3(1):1–9.
32. Asante KP, Abdulla S, Agnandji S, et al. Safety and efficacy of the RTS,S/AS01E candidate malaria vaccine given with expanded-programme-on-immunisation vaccines: 19 month follow-up of a randomised, open-label, phase 2 trial. Lancet Infect Dis. 2011;11(10):741–749.
33. Rampling T, Ewer KJ, Bowyer G, et al. Safety and high level efficacy of the combination malaria vaccine regimen of RTS,S/AS01B with chimpanzee adenovirus 63 and modified vaccinia Ankara vectored vaccines expressing ME-TRAP. J Infect Dis. 2016;214(5):772–781.
34. Witte D, Cunliffe NA, Turner AM, et al. Safety and immunogenicity of seven dosing regimens of the candidate RTS,S/AS01E malaria vaccine integrated within an expanded program on immunization regimen. Pediatr Infect Dis J. 2018;37(5):483–491.
35. Lusingu J, Olotu A, Leach A, et al. Safety of the malaria vaccine candidate, RTS,S/AS01E in 5 to 17 month old Kenyan and Tanzanian children. PLoS One. 2010;5(11):e14090.
36. Olotu A, Fegan G, Wambua J, et al. Seven-year efficacy of RTS,S/AS01 malaria vaccine among young African children. N Engl J Med. 2016;374(26):2519–2529.
37. Olotu A, Lusingu J, Leach A, et al. Efficacy of RTS,S/AS01E malaria vaccine and exploratory analysis on anti-circumsporozoite antibody titres and protection in children aged 5–17 months in Kenya and Tanzania: a randomised controlled trial. Lancet Infect Dis. 2011;11(2):102–109.
38. Agnandji ST, Asante KP, Lyimo J, et al. Evaluation of the safety and immunogenicity of the RTS,S/AS01E malaria candidate vaccine when integrated in the expanded program of immunization. J Infect Dis. 2010;202(7):1076–1087.
39. Alonso PL, Sacarlal J, Aponte JJ, et al. Duration of protection with RTS,S/AS02A malaria vaccine in prevention of Plasmodium falciparum disease in Mozambican children: single-blind extended follow-up of a randomised controlled trial. Lancet. 2005;366(9502):2012–2018.
40. Alonso PL, Sacarlal J, Aponte JJ, et al. Efficacy of the RTS,S/AS02A vaccine against Plasmodium falciparum infection and disease in young African children: randomised controlled trial. Lancet. 2004;364(9443):1411–1420.
41. Aide P, Dobano C, Sacarlal J, et al. Four year immunogenicity of the RTS,S/AS02A malaria vaccine in Mozambican children during a phase IIb trial. Vaccine. 2011;29(35):6059–6067.
42. Bojang KA, Milligan PJ, Pinder M, et al. Efficacy of RTS,S/AS02 malaria vaccine against Plasmodium falciparum infection in semi-immune adult men in The Gambia: a randomised trial. Lancet. 2001;358(9297):1927–1934.
43. Bojang K, Milligan P, Pinder M, et al. Five year safety and immunogenicity of GlaxoSmithKline’s candidate malaria vaccine RTS,S/AS02 following administration to semi-immune adult men living in a malaria-endemic region of The Gambia. Hum Vaccin. 2009;5(4):242–247.
44. Abdulla S, Oberholzer R, Juma O, et al. Safety and immunogenicity of RTS,S/AS02D malaria vaccine in infants. N Engl J Med. 2008;359(24):2533–2544.
45. Kester KE, Cummings JF, Ockenhouse CF, et al. Phase 2a trial of 0, 1, and 3 month and 0, 7, and 28 day immunization schedules of malaria vaccine RTS,S/AS02 in malaria-naive adults at the Walter Reed army institute of research. Vaccine. 2008;26(18):2191–2202.
46. Kester KE, Cummings JF, Ofori-Anyinam O, et al. Randomized, double-blind, phase 2a trial of falciparum malaria vaccines RTS,S/AS01B and RTS,S/AS02A in malaria-naive adults: safety, efficacy, and immunologic associates of protection. J Infect Dis. 2009;200(3):337–346.
47. Owusu-Agyei S, Ansong D, Asante K, et al. Randomized controlled trial of RTS,S/AS02D and RTS,S/AS01E malaria candidate vaccines given according to different schedules in Ghanaian children. PLoS One. 2009;4(10):e7302.
48. Lell B, Agnandji S, Von Glasenapp I, et al. A randomized trial assessing the safety and immunogenicity of AS01 and AS02 adjuvanted RTS,S malaria vaccine candidates in children in Gabon. PLoS One. 2009;4(10):e7611.
49. Polhemus ME, Remich SA, Ogutu BR, et al. Evaluation of RTS,S/AS02A and RTS,S/AS01B in adults in a high malaria transmission area. PLoS One. 2009;4(7):e6465.
50. Asante KP, Ansong D, Kaali S, et al. Immunogenicity and safety of the RTS,S/AS01 malaria vaccine co-administered with measles, rubella and yellow fever vaccines in Ghanaian children: a phase IIIb, multi-center, non-inferiority, randomized, open, controlled trial. Vaccine. 2020;38(18):3411–3421.
51. Otieno L, Oneko M, Otieno W, et al. Safety and immunogenicity of RTS,S/AS01 malaria vaccine in infants and children with WHO stage 1 or 2 HIV disease: a randomised, double-blind, controlled trial. Lancet Infect Dis. 2016;16(10):1134–1144.
52. Otieno L, Mendoza YG, Adjei S, et al. Safety and immunogenicity of the RTS,S/AS01 malaria vaccine in infants and children identified as HIV-infected during a randomized trial in sub-Saharan Africa. Vaccine. 2020;38(4):897–906.
53. RTS,S Clinical Trials Partnership. First results of phase 3 trial of RTS,S/AS01 malaria vaccine in African children. N Engl J Med. 2011;365(20):1863–1875.
54. RTS,S Clinical Trials Partnership. A phase 3 trial of RTS,S/AS01 malaria vaccine in African infants. N Engl J Med. 2012;367(24):2284–2295.
55. RTS,S Clinical Trials Partnership. Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet. 2015;386(9988):31–45.
56. RTS,S Clinical Trials Partnership. Efficacy and safety of the RTS,S/AS01 malaria vaccine during 18 months after vaccination: a phase 3 randomized, controlled trial in children and young infants at 11 African sites. PLoS Med. 2014;11(7):e1001685.
57. Di Pasquale A, Bonanni P, Garçon N, Stanberry LR, El-Hodhod M, Da Silva FT. Vaccine safety evaluation: practical aspects in assessing benefits and risks. Vaccine. 2016;34:6672–6680.
58. Ellenberg SS. Safety considerations for new vaccine development. Pharmacoepidemiol Drug Saf. 2001;10(5):411–415.
59. World Health Organization. Immunization safety surveillance: guidelines for immunization programme managers on surveillance of adverse events following immunization; 2022. Available from: https://iris.wpro.who.int/handle/10665.1/12620.
60. Chen M, Yuan Y, Zhou Y, et al. Safety of SARS‐CoV‐2 vaccines: a systematic review and meta‐analysis of randomized controlled trials. Infect Dis Poverty. 2021;10:94.
61. Hervé C, Laupèze B, Del Giudice G, Didierlaurent AM, Tavares Da Silva F. The how’s and what’s of vaccine reactogenicity. NPJ Vaccines. 2019;4(1):1.
62. Stassijns J, Bollaerts K, Baay M, Verstraeten T. A systematic review and meta-analysis on the safety of newly adjuvanted vaccines among children. Vaccine. 2016;34:714–722.
63. Del Giudice G, Rappuoli R, Didierlaurent AM. Correlates of adjuvanticity: a review on adjuvants in licensed vaccines. Semin Immunol. 2018;39:14–21.
64. Garçon N, Chomez P, Van Mechelen M. GlaxoSmithKline Adjuvant Systems in vaccines: concepts, achievements and perspectives. Expert Rev Vaccines. 2007;6:723–739.
65. Mettens P, Dubois PM, Demoitié MA, et al. Improved T cell responses to Plasmodium falciparum circumsporozoite protein in mice and monkeys induced by a novel formulation of RTS,S vaccine antigen. Vaccine. 2008;26:1072–1082.
66. Stewart VA, McGrath SM, Dubois PM, et al. Priming with an adenovirus 35-circumsporozoite protein (CS) vaccine followed by RTS,S/AS01B boosting significantly improves immunogenicity to Plasmodium falciparum CS compared to that with either malaria vaccine alone. Infect Immun. 2007;75:2283–2290.
67. Adepoju P. RTS,S malaria vaccine pilots in three African countries. Lancet. 2019;393(10182):1685.
68. Guerra Mendoza Y, Garric E, Leach A, et al. Safety profile of the RTS,S/AS01 malaria vaccine in infants and children: additional data from a phase III randomized controlled trial in sub-Saharan Africa. Hum Vaccin Immunother. 2019;15(10):2386–2398.
69. Klein SL, Shann F, Moss WJ, Benn CS, Aaby P. RTS,S malaria vaccine and increased mortality in girls. MBio. 2016;7(2):e00514–16.
70. Mondiale de la Santé O; World Health Organization. Malaria vaccine: WHO position paper–March 2022. Wkly Epidemiol Rec. 2022;97(9):60–78.
71. World Health Organization. Full evidence report on the RTS,S/AS01 malaria vaccine. Geneva, Switzerland: Department of Immunization, Vaccines and Biologicals (IVB), World Health Organization; 2021.
72. World Health Organization. WHO recommends groundbreaking malaria vaccine for children at risk. Historic RTS,S/AS01 recommendation can reinvigorate the fight against malaria; 2021. Available from: https://www.who.int/news/item/06-10-2021-who-recommends-groundbreaking-malaria-vaccine-for-children-at-risk.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
