Back to Journals » Patient Preference and Adherence » Volume 15
Sustainability of Improvement in Oral Health-Related Quality of Life in Children After Dental Treatment
Authors Farsi NJ , Farsi DJ, Aldajani MB, Farsi NM, El-Housseiny AA
Received 24 October 2020
Accepted for publication 6 January 2021
Published 10 February 2021 Volume 2021:15 Pages 271—281
DOI https://doi.org/10.2147/PPA.S288571
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Nada J Farsi,1 Deema J Farsi,2 Mariam B Aldajani,2 Najat M Farsi,2 Azza A El-Housseiny3
1Department of Dental Public Health, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia; 2Department of Paediatric Dentistry, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia; 3Department of Paediatric Dentistry, Faculty of Dentistry, Alexandria University, Alexandria, Egypt
Correspondence: Nada J Farsi
Department of Dental Public Health, Faculty of Dentistry, King Abdulaziz University, P.O. Box 80200, Jeddah, 21589, Saudi Arabia
Tel +966 126400000
Fax +966 126952437
Email [email protected]
Purpose: Dental treatment has been associated with improvement in the oral health-related quality of life (OHRQoL) in children. There is little evidence of whether the effect of treatment is sustainable over time or not. The aim of this study was to determine whether the effect of dental treatment on OHRQoL is maintained or diminishes over time.
Materials and Methods: A consecutive sample of parents of 47 children between 2 and 6 years who received comprehensive dental treatment at a postgraduate dental clinic were recruited. Parents completed the Early Childhood Oral Health Impact Scale (ECOHIS) prior to treatment and at 1 and 4 months after treatment. Parents were also asked three global questions. Score changes (overall and for each section) between time points were analyzed by a repeated-measures analysis of variance and Bonferroni tests.
Results: The children’s mean age was 4.7 ± 1.1, and 60% were females. ECOHIS scores were significantly improved from baseline (22.2 ± 6.9) to 1 month after treatment (8.7 ± 6.8) and were further improved at 4 months after treatment (1.9 ± 2.7), P < 0.001, with large effect sizes (2.8 for the child impact section and 2.2 for the family impact section). Parents’ perception of changes in the OHRQoL of their children obtained from a global question indicated an improvement in OHRQoL that was sustained over the follow-up period; at 1-month and 4-month follow-up, 89% and 94% of mothers reported that their child’s oral health improved a lot after dental treatment, respectively.
Conclusion: The impact of dental treatment on OHRQoL continued to remarkably improve during the 4 months following dental treatment.
Keywords: dental caries, oral health, quality of life, child, dental care
Introduction
Dental caries is the most prevalent childhood disease, affecting about 6.2 million children worldwide.1,2 Early childhood caries (ECC), a form of caries, is a significant chronic multifactorial disease that affects young children around the world and is becoming a significant health problem.3 Left untreated, caries can result in pain, lead to infection, and negatively affect nutrition, speech, learning, communication, and social interactions.4 These undesirable outcomes may impede the child’s normal growth and development.4 Furthermore, untreated caries has been associated with poor oral health-related quality of life (OHRQoL), which relates to the impact of oral health or disease on the individual’s well-being or quality of life.5,6
Recently, an interest in assessing OHRQoL in children has emerged. The notion of OHRQoL refers to the effect of the oral health condition of an individual’s on their well-being, their functioning, and their quality of life.7 Instruments were introduced and validated to study the impact of oral health on the functional, social, and psychological well-being of children and their families. These instruments include the Early Childhood Oral Health Impact Scale (ECOHIS), the Child Oral Health Quality of Life; including the Child Perceptions Questionnaire CPQ 8–10, and CPQ 11–14 (for children 8–10, and 11–14 years, respectively), the Michigan Oral Health-Related Quality of Life Scale–Child Version, and the scale of oral health outcomes for 5-year-old children (SOHO-5).8–12
Over the last few years, not only the clinical outcome but also the psychological impact of treatment has been considered when assessing its success.13,14 In dentistry, the ability of a treatment to enable a person to eat, speak, and socialize without pain, discomfort, or active disease have been indicators of success.15 Furthermore, how long the treatment effect is sustained is an important factor to consider in its risk-benefit assessment.16 In pediatric dentistry, comprehensive dental treatment on the dental chair has been associated with considerable improvement in OHRQoL.6,17 Similarly, full-mouth rehabilitation under general anesthesia has resulted in improved OHRQoL.13,15,18–20
Although dental treatment has been associated with improved OHRQoL, most studies have assessed the change in OHRQoL at only one point in time within 4 weeks of treatment completion.19 Only a few studies have assessed the effect of treatment on OHRQoL beyond 2 months.21–24 Whether this positive effect of treatment is sustainable over time or not remains unknown. The aim of this study, therefore, was to determine the change in OHRQoL over 4 months following comprehensive dental treatment among a sample of 2 to 6 year old children. The conceptual hypothesis was that the improvement would be maintained for up to 4 months.
Materials and Methods
Study Sample and Ethical Approval
The protocol for this longitudinal study was approved by the ethics committee at King Abdulaziz University, Faculty of Dentistry (KAUFD) (#036-13), and the study was conducted in accordance with the Declaration of Helsinki. Between May 2019 and December 2019, we recruited a consecutive sample of parents of children between the ages of 2 and 6 years who attended the postgraduate student clinics at KAUFD. The inclusion criteria were as follows: healthy children who required comprehensive dental treatment, of a parent whose native language was Arabic. Exclusion criteria were: children with special health care needs, those who were scheduled for treatment under general anesthesia, because factors unique to this type of treatment may influence parental feelings (ex. general anesthesia risks, more post-operative complications, less treatment visits, less negative psychological impact on children). Treatment with silver diamine fluoride (SDF) causes unesthetic staining of teeth which is likely to be negatively perceived by parents. At KAUFD, it is not used as a permanent treatment but only as an interim management until the child is able to receive more definitive care. Thus, children treated with SDF were also excluded.
Instrument for OHRQoL Assessment
The ECOHIS measures OHRQoL in children 6 years of age and younger. It was designed by Pahel et al in 2007.8 It comprises 13 questions divided into two sections: a child impact section (CIS) and a family impact section (FIS). The CIS covers four domains: oral symptoms (one question), function (four questions), psychological effects (two questions), and self-image and social interaction (two questions). The FIS covers two domains: parental distress (two questions) and family function (two questions). The scale has been widely used in the field of pediatric dentistry across the world in its original English form, as well as in several other languages.25,26 In the current study, we used the recently validated Arabic version of the ECOHIS, which has demonstrated validity and responsiveness.27,28 On behalf of their children, parents were asked to report on a 6-point scale the frequency that the child or family has experienced for each of the 13 items (never, hardly ever, occasionally, often, very often, and do not know). A demographic section was added to the questionnaire, comprising questions that collected data on health history, age, gender, nationality, parental education, and monthly family income.
Consent Form
A written explanation of the study design and aim was provided to each parent in Arabic, which was adjunctive to a verbal face-to-face description. After all parents’ questions pertaining to the study were answered, a signature was obtained from the parents who were willing to participate.
Data Collection
Each participating parent independently self-completed the two-page ECOHIS before dental treatment to establish the child’s pretreatment OHRQoL status. Parents were encouraged to reflect on the child’s oral health since birth. In addition, parents were asked two global questions preoperatively. The first was “How would you rate the overall oral health of your child?” which was originally introduced to test the convergent validity of the scale.8,27 The aim of this question was to assess each parent’s perception of the child’s overall oral health. The answers were given on a 5-point scale (1, excellent; 2, very good; 3, good; 4, fair; and 5, poor). The second was a knowledge question “How much is your child’s general health affected by his or her oral health?” The aim of this question was to assess each parent’s perception of the relationship between the child’s oral health and general health. This question was answered on a 5-point scale (1, not affected at all; 2, affected a little; 3, affected moderately; 4, affected a lot; and 5, affected greatly).
After obtaining the health history, we performed a comprehensive dental examination of each child (with the aid of radiographs as needed) and calculated the decayed, missing, and filled teeth (dmft) score in accordance with World Health Organization criteria.29 An individualized treatment plan was discussed with the parents and consents for treatment were obtained. In the visits that followed, comprehensive dental treatment was initiated, which consisted of educational sessions (oral hygiene instructions and diet counseling), preventive treatments (prophy/fluoride and pit and fissure sealants), restorative treatments (simple adhesive restorations or pulp therapy/stainless steel crowns), and/or extraction (with or without the placement of space maintainers). Educational/prevention messages were emphasized again in the last visit. Follow-up educational and preventive visits were scheduled every 3–6 months according to patients’ specific needs.
Four weeks after the completion of dental treatment, the children returned for a follow-up visit. The same parents who completed the preoperative questionnaire were asked to independently complete the postoperative questionnaire reflecting on the period since the completion of dental treatment. The knowledge global question was replaced with a global transition rating question, “Overall, how has your child’s oral health changed after dental treatment?”, to assess each parent’s perception of any improvement in their child’s oral health as suggested by Lee et al.20 This question was answered on a 5-point scale (1, improved a lot; 2, improved a little; 3, no change; 4, worsened a little; and 5, worsened a lot). A call was made to parents who did not attend the follow-up appointment to obtain their responses unaided over the telephone. After five failed call attempts over a 10-day period, the parents were excluded.
Three months later, children were scheduled for a 4-month follow-up and the same parents were again asked to independently complete the postoperative questionnaire reflecting on the past 4 months since dental treatment completion; and were also asked to answer the global transition rating question. We attempted to contact the parents who did not attend the follow-up appointment by phone. We made five attempts to reach them, or they were excluded.
Statistical Analysis
The ECOHIS responses were coded as follows: 0 = never, 1 = hardly ever, 2 = occasionally, 3 = often, 4 = very often, and 6 = do not know. “Don’t know” answers were treated as missing. To demonstrate the distribution of the ECOHIS responses, the frequencies and percentages of each ECOHIS question were presented after recategorizing the responses of each question into a binary variable; “never” and “hardly ever” responses were placed in one category, while “occasionally”, “often” and “very often” were placed in another category. Furthermore, an ECOHIS score was calculated by summing the responses of all questions. Scores were also calculated for each domain by adding the scores of the respective domain questions. Questionnaires with more than 30% of the data missing were excluded, and in those with <30% missing, the missing values were imputed by the mean of the rest of the values of the questionnaire.
The normality of the scores was assessed by graphically examining a quantile-quantile (Q-Q) plot, and by assessing results of Skewness and Kurtosis test for normality. To assess the change in ECOHIS scores over the three time points, we conducted a repeated-measures analysis of variance with Bonferroni tests for multiple comparisons. Effect size was calculated by dividing the mean of the score difference between baseline and 4 months after dental treatment by the standard deviation of the baseline score.30 Effect sizes of <0.2 indicated a small change, 0.2–0.7 a moderate change, and >0.7 a large effect.7,18
Sample size calculation was performed for a repeated-measures ANOVA test using G Power software.31 The calculation was based on a significance level of 0.05 and aiming at a statistical power level of 90%. To be conservative we assumed a small effect size of 0.1. It was estimated that 43 participants are required.
A P-value of ≤0.05 was considered statistically significant. Statistical analyses were performed with Stata version 12.1 software (StataCorp LP, College Station, TX, USA).
Results
Initially, 95 parent/child dyads were screened. As shown in the flowchart (Figure 1), 22 were excluded for not meeting the inclusion criteria, and 11 were also not eligible for not completing treatment. A sample of 62 eligible parents were recruited; however, because of missing data (n= 12 at baseline), and loss of follow-up at 4 months (n= 3), the responses of 47 were analyzed, yielding a response rate of 76%. The characteristics of the children are presented in Table 1. The mean age of the children was 4.7 years ± 1.1, and 60% of them were girls. Children required between two and seven visits to complete treatment with an average of 4.4 ± 1.3 visits. The distribution of ECOHIS scores at baseline, 1 month after treatment, and 4 months after treatment are presented in Table 2. Pain was the most frequently reported impact among children at baseline (83% of children) and 1 month after treatment (62% of children). Only 6% of children reported pain 4 months after treatment. Being upset and feeling guilty were the most frequently reported family impacts at the three time points.
 |
Figure 1 Flowchart of participating children from baseline to 4 months. |
 |
Table 1 Characteristics of the Study Participants at Baseline and at 1 Month and 4 Months After Dental Treatment (N= 47) |
 |
Table 2 Distribution of ECOHIS Responses at Baseline and at 1 Month and 4 Months After Dental Treatment (N= 47) |
Figure 2 demonstrates the responses to the global question, “How would you rate the overall oral health of your child?”. As illustrated, perceived oral health status improved over time from baseline to 4 months after treatment. Regarding the knowledge question “How much is your child’s general health affected by his or her oral health?”, 47% of parents reported that their child’s general health was not at all affected by his or her oral health, and 20% reported that there was very little effect or some effect. Only 11% stated that the child’s general health was affected by oral health and 2% that it was very affected. Figure 3 presents the distribution of the parent responses to the question, “Overall, how has your child’s oral health changed after dental treatment?” at 1 month and 4 months after dental treatment. At the 1-month treatment follow-up, 89% of the respondents reported that their child’s oral health had improved a lot, and 94% of them reported the same at 4 months after treatment. A little improvement was reported by 6% of the respondents at the 1-month follow-up and by 4% of the respondents at the 4-month follow-up.
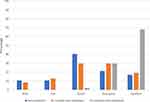 |
Figure 2 Responses to the global question, “How would you rate the overall oral health of your child?”, at baseline, at 1 month and 4 months after dental treatment. |
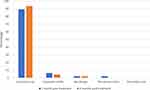 |
Figure 3 Responses to the global question, “Overall, how has your child’s oral health changed after dental treatment?”, at 1 month and 4 months after dental treatment. |
The ECOHIS scores at baseline, 1 month after dental treatment, and 4 months after dental treatment are illustrated in Table 3. The ECOHIS scores of the overall scale and its subscales (CIS and FIS) decreased from baseline to 1 month after dental treatment and even further to 4 months after treatment (<0.001), with large effect sizes. For all of the questionnaire domains, there was a statistically significant reduction in scores from baseline to 1 month and from 1 month to 4 months, except for the self-image and social interaction subdomain, where there was no statistically significant reduction from 1 month to 4 months after treatment. The percentage reduction in ECOHIS scores from baseline to 4 months after dental treatment ranged from 84% for the psychology domain to as high as 97% for the family function domain.
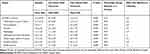 |
Table 3 ECOHIS Scores at Baseline and at 1 Month and 4 Months After Dental Treatment (N = 47) |
Discussion
The current study targeted Arabic-speaking parents of young children seeking dental care at KAUFD, providing an opportunity to assess the impact of dental treatment on the poor quality of life of children with dental caries and their families. OHRQoL was assessed before treatment and then 4 weeks and 4 months after treatment completion by using the ECOHIS. The children demonstrated the lowest OHRQoL at baseline. After treatment, the ECOHIS scores were lower than at baseline, which reflects an improvement in OHRQoL. This improvement was sustained at the 4-month follow-up with even lower ECOHIS scores.
Typically, pediatric patients at KAUFD are from low-income families and are accompanied by low-education mothers who seek free-of-charge treatment provided by faculty-supervised dental students and residents. Children typically complete their treatment in no more than 8 visits with the aid of basic behavior guidance including nitrous oxide sedation as needed. The majority of children are then put on a three-month follow-up schedule as they are considered at high-risk for developing caries. In the current study, mothers comprised the majority of participating parents; most of them were housewives and over one third had not exceeded high school education. From parents’ responses to the knowledge global question, it was evident that the majority of parents did not perceive the relationship between oral and overall general health. More elaboration on this relationship was added to the educational material that will be presented to parents at the beginning and end of treatment along with an emphasis on the long-term effects of neglected oral health.
Dental caries has been shown to significantly negatively impact the quality of life of children and their families.5,6 To quantify caries experience in the current study we measured the dmft score. At baseline, the mean dmft score (SD) was high (10.7 (3.3)). The mean ECOHIS score reflected poor OHRQoL. Most parents reported that their children experienced pain, and around half reported that their children had difficulty eating and drinking at baseline. This finding is in agreement with that of other studies in which the negative impacts reported in the child’s symptoms and function domains were more than those for the psychological and self-image/social interaction domains.6,32 Despite the high frequency of reported symptoms and the high dmft scores at baseline, only a few parents believed that their children’s oral health status preoperatively was “poor” or ”fair”, while the majority rated it as “good”, “very good” or “excellent”. This is contradicting to findings of a previous study in which the majority of parents rated their children’s pretreatment oral health as “poor” and “fair”.28 This may be due to the poor perception of parents in the current study of their children’s oral health status when they are asked about it generally rather than specifically about certain aspects. Another plausible explanation is the higher baseline dmft scores in the previous study (13.2 (3.5)).
Various dental treatments have been associated with an improvement in OHRQoL in children of different ages in different populations, and this improvement is attributed mainly to diminished pain and improved function.6,13,17 Restoring carious lesions seals the dentin and pulp from bacteria present in the oral cavity and thus diminishes sensitivity and pain. Restoring posterior teeth improves masticatory function by eliminating pain upon biting and facilitating mastication. For carious anterior teeth, esthetic restorations can improve function, eliminate pain and also foster social interactions and improve self-esteem. Although extracting carious anterior primary teeth may not be esthetically favorable by parents and children, children adapt well to speech and mastication without them. The association between dental treatment and improved OHRQoL was demonstrated in the current study, as the ECOHIS scores were dramatically decreased from baseline to 1 month after dental treatment and further decreased at 4 months following treatment. The biggest effect sizes were also observed in the oral symptoms (2.4) and function (2.6) domains. Similar improvement trends were observed in all questionnaire domains, except for the self-image and social interaction domain, where there was an improvement from baseline to 1 month after treatment, but not from 1 month to 4 months after treatment. This result was not surprising as 44.6% of children had at least one anterior tooth extraction; the mean number of missing teeth increased from 0.1 ± 0.1 at baseline to 1.6 ± 0.3 after dental treatment (P < 0.001). Children who have anterior teeth extracted are usually affected by negative self-image for some time postoperatively and may require a longer time to adapt to their new appearance. Furthermore, OHRQoL was evaluated by parents who may have been influenced by their negative perception of esthetics related to extracted anterior teeth. This finding is in agreement with other studies that suggested negative changes in relation to the absence of teeth following extractions. It further aligns with an interesting finding by Leal et al33 that showed that the impacts of tooth extraction more negatively affected children’s OHRQoL than did the presence of dental caries.
A 4-week interval between treatment and assessment of OHRQoL is a reasonable time for many post-treatment side effects to have subsided and the children and their families to enjoy a new oral symptom-free life. However, some effects related to recent extractions, especially in the anterior maxilla, may take longer for children to accept. Thus, it is reasonable to assume that children and their families would report fewer symptoms as time passes. On the other hand, it would not have been surprising to see children and families reporting fewer symptoms when the oral symptom-free period is still a novel experience; as they get used to it, they would begin reporting new symptoms with time, especially if new carious lesions develop. In a similar study, a slight decrease in the effect of treatment was observed between the 1-month and 3-month follow-ups that was explained by possible treatment failures or a temporal decrease in the perception of the importance of dental treatment.23 To determine the trend in the improvement of OHRQoL over time, we assessed it again 4 months after treatment. Although OHRQoL for both the child and family domains improved 1 month after treatment, a more considerable improvement was seen 3 months later. These findings indicate that the effect of dental treatment on OHRQoL does not seem to be temporary. In fact, an upward direction in the effect was evident in the first few months after treatment. This may be attributed to the good quality of dental care provided to these children, the improved oral hygiene and dietary choices provided by parents after the educational sessions, complete healing at extraction sites, and children getting used to their restorations, crowns and posterior space maintainers.
The observed improvement in OHRQoL was also perceived by the majority of the parents. Parents gave higher ratings to their children’s oral health post treatment in the first global question. This was further supported by their responses to the global transition rating question. Only one participant reported no change in their child’s oral health at the 1-month follow-up; at the 4-month follow-up, one participant reported a small worsening in oral health. When parents were asked about the status of their children’s oral health at baseline, a few reported that it was excellent, whereas the majority reported that it was excellent at 4 months after treatment. This finding indicates that the perception of the parents regarding their children’s oral health also improved after treatment.
The ECOHIS not only allowed us to assess the effect of oral disease on the child’s quality of life but it also allowed us to assess the effect on the family. In the current study, more than half of the parents reported parental distress (being upset or feeling guilty) at baseline. Family function was affected, too, as about half of the parents reported taking time off work, and more than a fourth reported a financial burden due to their child’s oral health problems. The negative effects of caries on family function and the parental distress it causes are congruent with the findings of previous studies.6,32 In our study, parents reported considerably fewer family impacts 1 month and 4 months after dental treatment than they did at baseline.
This study has potential limitations; a considerable number of children younger than 6 years who seek dental treatment at KAUFD ultimately receive full-mouth rehabilitation in the operating room because of extensive treatment needs. More recently, some of them have been treated with silver diamine fluoride to control caries progression until a more suitable opportunity for a more definitive treatment arises. Furthermore, many children treated at KAUFD come from non-Arabic speaking families. The family demographics and exclusion of children who did not receive conventional dental treatment were reflected in the relatively small final sample size. Nevertheless, the sample size was larger than those in similar studies, and still provided >90% statistical power.20,22 The temporary shut-down of KAUFD due to the COVID-19 pandemic prevented some parents from attending the follow-up visits, but we collected the information over the phone. As with most instruments used with young children, parents served as proxies to give accounts on behalf of their children, and it might be a concern that their responses may not be truly reflective of the children’s actual experiences and feelings. However, it has been shown that the quality of life of children reported by parents can be reliable.34
The strength of the study is that it assessed OHRQoL at two points in time. Although in some studies, assessments were conducted after a longer interval after treatment completion, they were carried out once and the changes in OHRQoL could therefore not be assessed over time.6,22 In the current study, we found increasing improvement after treatment. Also, the close follow-up of participants was reflected on the excellent follow-up response rates; the response rate was 100% in the 1-month follow-up, and 94% in the 4-month follow-up. Furthermore, the instrument used in this study has been validated in Arabic and showed good psychometric properties.27
The current results suggest continued improvement in OHRQoL for 4 months following dental treatment. Further research to assess OHRQoL over longer periods after dental treatment may be useful. In addition, assessing OHRQoL in children older than 6 years old may offer insights into the effects on children of other age groups. Studies that compare different treatment modalities, or treatments of different complexities are also encouraged.
Why This Paper is Important to Pediatric Dentists
- This study affirms the evidence that dental caries has a negative impact on the quality of life of young children and their parents.
- This study highlights the fact that OHRQoL after dental treatment not only improves but continues to improve in the short term.
- Adding global questions to the ECOHIS helped to relate parents’ perspectives to objective findings.
Abbreviations
ECC, Early childhood caries; OHRQoL, oral health-related quality of life; ECOHIS, Early Childhood Oral Health Impact Scale; CPQ, Child Perceptions Questionnaire; KAUFD, King Abdulaziz University, Faculty of Dentistry; CIS, child impact section; FIS, family impact section.
Data Sharing Statement
Data will be provided upon reasonable request.
Ethics Approval
This study was approved by the ethics committee at King Abdulaziz University, Faculty of Dentistry (KAUFD) (#036-13).
Acknowledgments
This project was funded by the Deanship of Scientific Research (DSR), King Abdulaziz University, Jeddah (Fund G523-165-1441). The authors acknowledge with thanks the technical and financial support of the DSR.
Author Contributions
NJF contributed to the conception of the idea, performed the statistical analysis and interpreted the data, participated in writing the manuscript, and critically revised and approved the manuscript. DJF conceived the idea, designed the study, drafted the questionnaire, drafted the manuscript, and wrote most sections of the manuscript, participated in data collection, critically revised and approved the manuscript. MBA contributed to the conception of the idea, collected the data, critically revised and approved the manuscript. NMF revised the questionnaire, designed the study, critically revised and approved the manuscript. AAE revised the questionnaire, designed the study, critically revised and approved the manuscript.
All authors made significant contributions to conception and design of the study, data collection, or statistical analysis and interpretation of results; took part in writing the manuscript or revising it critically for important intellectual content; agreed to submit to this journal; gave final approval of the version to be published; and agree to be responsible for all aspects of the work.
Funding
This project was funded by the Deanship of Scientific Research (DSR), King Abdulaziz University, Jeddah (Fund G523-165-1441).
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. U.S. Department of Health and Human Services. Oral health in America: a report of the surgeon general. Rockville, Md.: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. Available from: https://www.nidcr.nih.gov/sites/default/files/2017-10/hck1ocv.%40www.surgeon.fullrpt.pdf.
2. Kassebaum NJ, Bernabe E, Dahiya M, et al. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94(5):650–658. doi:10.1177/0022034515573272
3. World Health Organization. Expert consultation on public health intervention against early childhood caries: report of a meeting, Bangkok, Thailand. 2016. Available from: https://apps.who.int/iris/handle/10665/255627.
4. American Academy of Pediatric Dentistry. Definition of Dental Neglect 2019–2020. Available from: https://www.aapd.org/globalassets/media/policies_guidelines/d_dentalneglect.pdf.
5. Monse B, Heinrich-Weltzien R, Benzian H, et al. PUFA–an index of clinical consequences of untreated dental caries. Community Dent Oral Epidemiol. 2010;38(1):77–82. doi:10.1111/j.1600-0528.2009.00514.x
6. BaniHani A, Deery C, Toumba J, et al. The impact of dental caries and its treatment by conventional or biological approaches on the oral health-related quality of life of children and carers. Int J Paediatr Dent. 2018;28(2):266–276. doi:10.1111/ipd.12350
7. Malden PE, Thomson WM, Jokovic A, et al. Changes in parent-assessed oral health-related quality of life among young children following dental treatment under general anaesthetic. Community Dent Oral Epidemiol. 2008;36(2):108–117. doi:10.1111/j.1600-0528.2007.00374.x
8. Pahel BT, Rozier RG, Slade GD. Parental perceptions of children’s oral health: the Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual Life Outcomes. 2007;5:6. doi:10.1186/1477-7525-5-6
9. Jokovic A, Locker D, Tompson B, et al. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent. 2004;26(6):512–518.
10. Jokovic A, Locker D, Stephens M, et al. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81(7):459–463. doi:10.1177/154405910208100705
11. Filstrup SL, Briskie D, da Fonseca M, et al. Early childhood caries and quality of life: child and parent perspectives. Pediatr Dent. 2003;25(5):431–440.
12. Tsakos G, Blair YI, Yusuf H, et al. Developing a new self-reported scale of oral health outcomes for 5-year-old children (SOHO-5). Health Qual Life Outcomes. 2012;10:62. doi:10.1186/1477-7525-10-62
13. Farsi DJ, Farsi NJ, El-Housseiny AA, et al. Impact of dental rehabilitation on oral health-related quality-of-life in healthy children and those with special health care needs. J Contemp Dent Pract. 2018;19(4):367–374. doi:10.5005/jp-journals-10024-2268
14. Myles PS, Williams DL, Hendrata M, et al. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth. 2000;84(1):6–10. doi:10.1093/oxfordjournals.bja.a013383
15. Park JS, Anthonappa RP, Yawary R, et al. Oral health-related quality of life changes in children following dental treatment under general anaesthesia: a meta-analysis. Clin Oral Investig. 2018;22(8):2809–2818. doi:10.1007/s00784-018-2367-4
16. Heneghan C, Goldacre B, Mahtani KR. Why clinical trial outcomes fail to translate into benefits for patients. Trials. 2017;18(1):122. doi:10.1186/s13063-017-1870-2
17. Abanto J, Paiva SM, Sheiham A, et al. Changes in preschool children’s OHRQoL after treatment of dental caries: responsiveness of the B-ECOHIS. Int J Paediatr Dent. 2016;26(4):259–265. doi:10.1111/ipd.12192
18. de Souza MC, Harrison M, Marshman Z. Oral health-related quality of life following dental treatment under general anaesthesia for early childhood caries - a UK-based study. Int J Paediatr Dent. 2017;27(1):30–36. doi:10.1111/ipd.12221
19. Knapp R, Gilchrist F, Rodd HD, et al. Change in children’s oral health-related quality of life following dental treatment under general anaesthesia for the management of dental caries: a systematic review. Int J Paediatr Dent. 2017;27(4):302–312. doi:10.1111/ipd.12259
20. Lee GH, McGrath C, Yiu CK, et al. Sensitivity and responsiveness of the Chinese ECOHIS to dental treatment under general anaesthesia. Community Dent Oral Epidemiol. 2011;39(4):372–377. doi:10.1111/j.1600-0528.2010.00604.x
21. Baghdadi ZD. Effects of dental rehabilitation under general anesthesia on children’s oral health-related quality of life using proxy short versions of OHRQoL instruments. ScientificWorldJournal. 2014;2014:308439. doi:10.1155/2014/308439
22. El-Meligy O, Maashi M, Al-Mushayt A, et al. The effect of full-mouth rehabilitation on oral health-related quality of life for children with special health care needs. J Clin Pediatr Dent. 2016;40(1):53–61. doi:10.17796/1053-4628-40.1.53
23. Novaes TF, Pontes LRA, Freitas JG, et al. Responsiveness of the Early Childhood Oral Health Impact Scale (ECOHIS) is related to dental treatment complexity. Health Qual Life Outcomes. 2017;15(1):182. doi:10.1186/s12955-017-0756-z
24. Yawary R, Anthonappa RP, Ekambaram M, et al. Changes in the oral health-related quality of life in children following comprehensive oral rehabilitation under general anaesthesia. Int J Paediatr Dent. 2016;26(5):322–329. doi:10.1111/ipd.12200
25. Bordoni N, Ciaravino O, Zambrano O, et al. Early childhood oral health impact scale (ECOHIS). Translation and validation in Spanish language. Acta Odontol Latinoam. 2012;25(3):270–278.
26. Bekes K, Omara M, Safar S, et al. The German version of early childhood oral health impact scale (ECOHIS-G): translation, reliability, and validity. Clin Oral Investig. 2019;23(12):4449–4454. doi:10.1007/s00784-019-02893-1
27. Farsi NJ, El-Housseiny AA, Farsi DJ, et al. Validation of the Arabic version of the early childhood oral health impact scale (ECOHIS). BMC Oral Health. 2017;17(1):60. doi:10.1186/s12903-017-0353-x
28. Farsi DJ, Farsi NJ, El-Housseiny AA, et al. Responsiveness of the Arabic version of the ECOHIS to dental rehabilitation under general anaesthesia. Int J Paediatr Dent. 2018;28(1):52–61. doi:10.1111/ipd.12307
29. World Health Organization. Oral health surveys: basic methods 4th edition. 1997. Available from: http://apps.who.int/iris/bitstream/10665/41905/1/9241544937.pdf.
30. Tsakos G, Allen PF, Steele JG, et al. Interpreting oral health-related quality of life data. Community Dent Oral Epidemiol. 2012;40(3):193–200. doi:10.1111/j.1600-0528.2011.00651.x
31. Faul F, Erdfelder E, Buchner A, et al. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi:10.3758/BRM.41.4.1149
32. Abanto J, Carvalho TS, Mendes FM, et al. Impact of oral diseases and disorders on oral health-related quality of life of preschool children. Community Dent Oral Epidemiol. 2011;39(2):105–114. doi:10.1111/j.1600-0528.2010.00580.x
33. Leal SC, Bronkhorst EM, Fan M, et al. Untreated cavitated dentine lesions: impact on children’s quality of life. Caries Res. 2012;46(2):102–106. doi:10.1159/000336387
34. Khin Hla T, Hegarty M, Russell P, et al. Perception of pediatric pain: a comparison of postoperative pain assessments between child, parent, nurse, and independent observer. Paediatr Anaesth. 2014;24(11):1127–1131. doi:10.1111/pan.12484
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
