Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Survival Time and Associated Factors Among Adults Living with HIV After Initiation of HAART in South Gondar, Northwest Ethiopia: A Retrospective Cohort
Authors Deres G, Mehari Nigussie Z , Genetu Chanie M , Worku N
Received 2 April 2021
Accepted for publication 2 June 2021
Published 17 June 2021 Volume 2021:14 Pages 1463—1474
DOI https://doi.org/10.2147/JMDH.S314004
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Genzeb Deres,1 Zelalem Mehari Nigussie,2 Muluken Genetu Chanie,3 Nigusu Worku4
1Blood Bank, Debre-Tabor Branch, Amhara National Regional State, Ethiopia; 2School of Public Health, Bahir Dar University, Bahir Dar, Ethiopia; 3Department of Health Systems and Policy, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 4Department of Health Systems and Policy, University of Gondar, Gondar, Ethiopia
Correspondence: Nigusu Worku Email [email protected]
Background: Antiretroviral therapy consistently improves the survival of people living with HIV and contributes to preventing the development of new infections. Studies of antiretroviral therapy programs in Africa have shown a high mortality rate during the first 6 months after initiation of HAART in rural health facilities. This study looks at survival time and associated factors among adults with HIV in south Gondar, Northwest Ethiopia.
Methods: A 5-year retrospective cohort study design was conducted using patient records among 746 adults living with HIV/AIDS. A systematic random sampling technique was used to select respondents after proportional allocation was made for all health facilities included in the study. Epi-info version 7 and STATA 12 were used for data entry and analysis, respectively. Kaplan–Meier survival analysis was used to estimate mean survival time and a life table was used to estimate survival probability after initiation of HAART.
Results: A total of 746 respondents were followed for a median of 60 months. There were 102 (13.67%) deaths yielding an overall mortality rate of 2.59/1,000-person year observation (95% CI=0.02136– 0.031736). Age of respondents > 43 years (AHR=2.790; 95% CI=1.495– 5.206), bedridden (AHR=9.57; 95% CI=3.87– 23.64), past TB treatment (AHR=0.86; 95% CI=0.46– 0.609), baseline WHO stage IV (AHR=3.02; 95% CI=1.77– 5.18), pneumonia after ART start (AHR=3.6; 95% CI=1.4– 9.2), INH prophylaxis (AHR=2.58; 95% CI=1.232– 5.188), ambulatory functional status (AHR=5.86; 95% CI=2.67– 12.86), and disclosure status (AHR=0.423; 95% CI=0.261– 0.685) were significant predictors for survival time after initiation of HAART among adults living with HIV.
Conclusion: The mortality rate was highly (13.67%) observed in the early phase of antiretroviral treatment. Being ambulatory and bedridden, age of respondents > 43 years, past TB treatment, baseline WHO stage IV, pneumonia after HAART, INH prophylaxis, and disclosure status were independent predictors of mortality.
Keywords: survival time, adults, HAART, south Gondar
Background
HIV/AIDS is a term which applies for human immune deficiency virus and human acquired immune deficiency syndrome. HIV infects cells of the immune system, destroying or impairing their function, and it can be transmitted through sexual intercourse, transfusion of contaminated blood, and sharing of contaminated sharp instruments. It is also transmitted from a mother to her child.1
HAART is a combination of three or more antiretroviral drugs used in the treatment of HIV infection and AIDS, and it was introduced in 1996.2
Highly active antiretroviral therapy significantly improves the prognosis of people living with HIV. It reduces the viral loads to undetectable levels (up to 50 copies/mL) and slows down the spread of HIV by increasing CD4 cell count levels (50–100 cells/mL) in the first therapy, delaying progression to AIDS, and reducing mortality.3
In sub-Saharan Africa, ART treatment has been started recently and it is hard to learn the most important factors that can determine the survival of patients on ART due to the limited scope and coverage of information available. Early mortality rates in sub-Saharan Africa are very high; ranging from 8–26% of patients who die in the first year of ART treatment.4
The gains in treatment are largely responsible for a 26% decline in AIDS-related deaths globally since 2010.5
HIV/AIDS remains a public health problem in Ethiopia with an estimated national prevalence of 1.8% in 2017, out of these patients 367,000 were taking ART. In Ethiopia, free ART service was launched to be given in public hospitals in 2005 and primary healthcare centers in 2006 as part of the service scaling-up.6
Many studies indicated that mortality rates of HIV patients were high in the first year of ART treatment in Ethiopia, and around 20,000 people liveling with (PLW) HIV die each year.4
Globally at the end of 2015, 1.1 million people died from AIDS-related illnesses and 35 million people have died from AIDS-related illnesses since the start of the epidemic.2,7
According to study results in Ethiopia and outside Ethiopia, there are several problems or risk factors that result in the low survival of HIV patients.8 Among these risk factors, baseline CD4 count, total lymphocyte count (TLC), higher viral load at baseline, regimen intolerance, previous exposure to ARV drugs, medication adherence, missed clinic visits, malnutrition, delayed ART initiation, TB-HIV co-infection, age group, etc. were the major risk factors indicated.9–11
The prevalence of HIV is different between the urban and rural parts of Ethiopia, so urban HIV prevalence declined from a peak of 14.3% in 2001 to 4.4% in 2012, while rural prevalence peaked in 2003 at 4.1% and remained at 1.9% in 2009 and 1.8% in 2012.12
In Amhara region (2009/10) 64,648 people living with HIV were put on ART, which was a 60.2% coverage of the 107.414 people who were requiring ART, and the mortality rate of adult HIV/AIDS patients was 2.3% of the total adult population.7,12
Many studies were conducted in Ethiopia on the survival time of HIV-infected patients after initiation of HAART, but almost all studies were conducted in hospitals, while the ART service is decentralized to health centers that are less equipped with materials and run with middle-level professionals. This study aimed to estimate the survival time and its predictors among adults living with HIV who started ART treatment.
Methods
Study Design and Setting
A retrospective cohort study design was conducted in the south Gondar zone from September 1, 2010 to September 30, 2014.
South Gondar zone is one of the 13 zones of Amhara national regional state, Ethiopia. Debre Tabor is a city of South Gondar which is 665 km away from Addis Ababa and 102 Km from Bahir Dar (the capital city of Amhara national regional state). According to the zonal health departments, the total population of this zone was 2,781,235.
There are 12 districts, with four hospitals and 19 health centers providing ART services for persons living with HIV in the South Gondar Zone.
Since the ART service has been started there have been 13,935 individuals on the ART clinic service; from these, 9,844 individuals are currently on ART, 3,335 are on pre-ART service and 756 are pediatrics.
Population
All adults’ medical charts in ART clinics of South Gondar zone were the source population, while all adults aged ≥15 years who started ART treatment in health centers of south Gondar zone, and those who started ART from September 1, 2009, to September 30, 2013, were the study population of this study.
Eligibility Criteria
Of all people living with HIV whose age was ≥15 years and started ART treatment at health centers of South Gondar zone, those who started ART from September 1, 2009, to September 30, 2013 were included, while transferred cases, women who were pregnant at the time of ART initiation, and lactating mother were excluded from the study.
Sample Size Determination and Sampling Procedures
The sample size was determined by using EPI info version 7.2.1. The assumptions that type I error 5%, power of 80%, and considering two population proportions on exposure status were considered.4,13,14 The sample size was determined by taking the factors from previous studies such as CD4 cell count, adherence, TB status, whom staging, and total lymphocyte count .15 By so doing the maximum final sample size used for this study after adding 10% for non-respondents was 770.
All ART sites (19 Health centers) in the South Gondar zone were considered and health centers that provide ART services for at least 5 years were included. The number of adults living with HIV who have been taking ARV for at least 5 years was screened and identified from the ART clinics’ logbook of the health centers (total cases are known). Then the entire sample sizes were proportionally allocated to each health center. Medical charts of study participants from each health center were selected by using a simple random sampling method from the ART logbook after putting in order the lists of patients for data collection.
Operational Definitions
Censored: Individuals on HAART, who did not experience death at the end of this study.
Good adherence: if the percentage of missed dose is between >95% (<2 doses of 30 doses or <3 doses of 60 doses) as documented by ART physician.
Lost to follow-up: patients discontinued ART for at least 1–3 months, as recorded by ART physician.
Drop out: patients who discontinued ART for at least 1 month as recorded by the ART physician.
Data Collection Tools, Procedures, and Data Quality Control
A structured data extraction format was adopted from ART intake and follow-up formats of ART clinics. Four ART trained nurses for data collection and two supervisors of health officers were trained for 1 day and recruited. The data was collected by reviewing pre-ART registers, laboratory requests, monthly cohort forms, and follow-up forms, ART intake forms, patients’ cards, and death certificates complemented by registration by home visitors. The recent laboratory results before starting ART were used as a baseline. Data were collected retrospectively from all eligible medical records of adult HIV/AIDS patients from ART clinics using structured data extracting formats.
Data quality control training was given for data collectors and supervisors. The overall procedure was controlled by the principal investigator of the study. All completed data collection forms were examined for completeness and consistency during data management. The data was entered and cleaned by the principal investigator before analysis.
Data Processing and Analysis
Data were entered into Epi-Info v. 7.2.1 for and exported to STATA version 12 for statistical analysis. The data were cleaned and edited before analysis. Data exploration was undertaken to see if some odd codes or items are not logical and then subsequent editing was made. The patients’ characteristics were described in terms of frequency, mean/median value for continuous data, and percentages for categorical data. Finally, the outcome variable of this study was dichotomized into censored or death.
The actuarial life table was used to estimate survival time after initiation of ART, and a Log rank test was used to compare survival curves. Cox proportional hazard regression was used to determine significant factors associated with survival time. Both crude and adjusted hazard ratios (HRs) at 95% confidence intervals were employed, and candidate variables with p<0.25 were exported to the multivariable Cox regression model. Independent variables with p-values of <0.05 in the multivariable Cox regression model were considered statistically significantly associated factors of survival time. The proportional hazards assumption was checked by both graphical and statistical tests of the global goodness-of-fit test (Schoenfeld’s method).
Ethical Considerations
The ethical review was obtained from school of public health, college of medicine and health sciences, Bahir Dar University. Then Permission letters had been received from the Amhara national regional health bureau and public health research institution. As the study was conducted through a review of medical records, patients were not subject to any harm. To preserve the confidentiality, data were collected by ART trained nurse’s/data clerks working in ART clinics of each health center. During data extraction, no personal identification methods were used on data collection formats. All the procedures of the ethical evaluation of this study followed the Helsinki declaration of human research.
Results
A total of 770 charts of people living with HIV who were on ART were included in the study. From the total patients’ records reviewed, 746 records were complete and the data completeness rate was 96.88%. Records were reviewed for the socio-demographic, history of illness, baseline clinical and laboratory information, social and risk behaviors, and follow-up information of HIV patients who started HAART.
Socio-Demographic Characteristics
The median age at the time of HAART initiation was ±35.3 (27–42) years. From the total of patients’ charts, 199 (26.70%) were within the age group of 28–35 years, 347 (46.51%) were males, and 102 (13.67%) patients were found to be dead at the end of the study period. Three hundred and thirty (44.24%) respondents were married and 101 (13.54%) attended secondary school (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Adults Living with HIV Receiving ART in South Gondar Zone, Northwest Ethiopia, 2017 (n=746) |
History of Past Opportunistic Illness (OI)
Out of 746 patients, 172 (23.06%) had a history of Tuberculosis co-infection before initiation of HAART.
The leading opportunistic illness that affected patients in the study period was Tuberculosis (172; 23.06%) followed by all form of Candidiasis (134; 17.96%) (Table 2).
 |
Table 2 History and Current Opportunistic Illnesses Among Adults Living with HIV in South Gondar ART Site Health Centers, Northwest Ethiopia, 2017 (n=746) |
Clinical and Laboratory Related Characteristics
The mean weight at the initiation of ART was 48.14 (±6.47), about 685 (91.82%) being above 40 kg. The mean hemoglobin level was 13.62 (±SD 4.54).
Five hundred and forty-two (72.65%) had been in working functional level, and 43 (5.76%) of them died during the follow-up period. During the initiation of ART, 130 (17.43%) patients were WHO stage IV, out of these 5.23% died during the follow-up period. At the initiation of ART, the mean CD4 count was 215.01 cells/m3 (±127.76) and the mean CD4 cell count significantly increased by 255.24 cells/m3 in 60 months of follow-up (470.25 cells/m3 (±304.398)).
During the follow-up period, Chemoprophylaxis (INH and CPT) was given to 546 (73.19%) patients. Out of these, 63 (14.86%) died (Table 3).
 |
Table 3 Clinical and Laboratory Characteristics of the Adults Living with HIV in South Gondar Zone Northwest Ethiopia, 2017 (n=746) |
Survival Analysis
From a total of 746 adults living with HIV whose charts were reviewed, 102 (13.67%) of them were found to have died during the overall follow-up period of 60 months.
According to Kaplan-Meier survival estimation, the mean survival time was 54.84 (95% CI=53.74–55.74), and the median (SD) survival time was 52.74 (±16.63) months. The total analysis time at risk during follow-up was 39,341 months, with an incidence density of 2.59/1,000 person-years (CI=0.002136–0.0031736).
From the total deaths during the follow-up period, 14 deaths (1.86%) occurred in the 1st month of treatment, 17 deaths at 1–3 months, and two deaths at 6 –12 months of treatment, and also there were 15 deaths between the 3rd and 4th years and 12 deaths between the 4th and 5th year. The remaining study participants were censored for different reasons; 18 patients were lost from the follow-up; 42 patients were transferred to other facilities, and 584 wereon treatment. The mortality rate during the follow-up period was 2.59/1,000 person-years (Table 4).
 |
Table 4 Survival Analysis of the Survival Time and Associated Factors Among Adults Living with HIV in South Gondar Zone, Northwest Ethiopia, 2017 (n=746) |
The survival of adults living with HIV was around 94% in the first month of follow-up, and the mortality of adults living with HIV was 6%; 1%, 2%, and 3% at 1, 20, and 60 months of follow-up, respectively. The hazard rate at the end of the follow-up period was 0.01 (Table 5).
 |
Table 5 Life Table of Adults Living with HIV on HAART in South Gondar Zone Northwest Ethiopia, 2017 (n=746) |
This study showed that the hazard (mortality) of patients increases as time increases during the follow-up period (Figure 1).
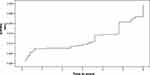 |
Figure 1 Overall Kaplan–Meier hazard of the adults living with HIV on HAART in South Gondar zone, Northwest Ethiopia, 2017 (n=746). |
Patients who disclosed their HIV status survived for a longer time than those who did not disclose their HIV status (Figure 2).
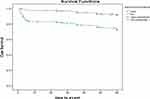 |
Figure 2 Kaplan–Meier survival estimate of time to death of study subjects by their HIV disclosure status in South Gondar zone Northwest Ethiopia, 2017 (n=746). |
Patients’ ART treatment adherence was a significant factor for the survival of patients, as shown in Figure 3. Survival of patients with good ART treatment adherence was longer than patients with poor ART treatment adherence (Figure 3).
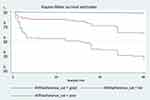 |
Figure 3 Kaplan –Meier survival estimate of time to death of study subjects by recent ART treatment adherence in South Gondar zone North West Ethiopia, 2017 (n=746). |
Factors Analysis of the Survival Time of Adults Living with HIV
Between the baseline and the follow-up periods, significant differences of time to death in long rank test among categorical variables in strata were seen for age (p=0.006), sex (p=0.004), residence (p=0.004), past history of TB (p=0.016), current OI (p<0.001), WHO staging at baseline (p<0.001), recent weight (p<0.001), disclosure status (p=0.001), ART adherence (p<0.001), past prophylaxis (p=0.002), and follow-up prophylaxis (p=0.001).
Bivariable Cox-proportional model was used to determine the relationship between variables and the risk of developing mortality. Before fitting the covariate into the model, proportional hazard assumptions were checked by examining log (-log) S (t) plots.
From the multivariable Cox regression, the significant predictors of time to death were age of respondents >43 years (AHR=2.790; 95% CI=1.495–5.206), bedridden functional status (AHR=9.57; 95% CI=3.87–23.64), past TB treatment (AHR=0.86; 95% CI=0.46–0.609), baseline WHO stage IV (AHR=3.02; 95% CI=1.77–5.18), pneumonia after ART start (AHR=3.6; 95% CI=1.4–9.2), INH prophylaxis (AHR=2.58; 95% CI=1.232–5.188), ambulatory functional status (AHR=5.86; 95% CI=2.67–12.86), and disclosure status (AHR=0.423; 95% CI=0.261–0.685) (Table 6).
 |
Table 6 Multivariable Cox Regression Between Respondent’s Characteristics and Death Among Adults Living with HIV in the South Gondar Zone, Northwest Ethiopia, 2017 (n=746) |
Discussion
This study was conducted to assess survival time and predictors of survival among people living with HIV/AIDS on HAART. The overall probability of survival of adults living with HIV who started HAART in this study was 86.33% at 60 months of follow-up. This result was higher as compared to studies done at Debre Markos Hospital, Ethiopia (57%), Zewditu hospital Addis Ababa (66.4% at 48 months follow-up),16–18 Cameroon (47% at 60 months), and Nepal (9%) at 60 months of follow-up,5,7 respectively. According to a study conducted in Malawi, the probability of being alive on ART at 6, 12, and 18 months was 89.8%, 83.4%, and 78%, respectively.19 In our study, the probability of surviving at 6, 12, and 18 months was 93.28%, 93.01%, and 89.53%, respectively. In this study, 13.67% of patients have died and it was high in the first 6 months of follow-up. The mortality rate in this study was low when compared to a study done in rural Tanzania which reported that the mortality rate during the 5-year study period was 20.2/100 person-years and survival probability at 5 years follow-up was high.20
The mortality rate of this study finding was low as compared to a study conducted on treatment outcomes and their determinants in HIV patients on an Anti-retroviral Treatment program in selected health facilities of Kembata and Hadiya zones, SNNP Region, Ethiopia, during 2015 showed that 68% of deaths occurred in the first 6 months of treatment and the median survival time was 25 months.20
The overall mortality rate was lower when compared to other studies in Ethiopia, such as Debre Markos (22.9%),21 and Zewditu hospital (33.6%),10 and other developing countries such as Cameroon (28.5%)22 and Ukraine (17.5%).23 This difference might be due to the strong care and support provided in hospitals compared to health centers, or the poor management of opportunistic infections at health centers. The finding of this study was similar with the studies conducted in Oromia (10.3%), Nepal (11.7%), and Vietnam (9%).2,15,24 This finding was higher as compared to studies done in Axum (8%) and Canada (5%), which may result from a difference in the quality of care provided.2,25
There was a higher mortality rate in the first 3–6 months of therapy which was similar to findings in studies conducted in different countries,1,26,27 and this might be due to immune reconstitution syndrome associated with the initiation of HAART. The patients who come to health centers may be after developing full-blown AIDS. This may result in early AIDS-related death. This study showed that the difference in survival rate might be due to differences in adherence, risk behavior and financial accessibility, and earlier health-seeking behavior of women.
In this study patients with a baseline weight of ≥43 kg were at higher risk of death compared to those who had ≤27 kg weight. A similar finding was observed in a study done at Tigray and Nepal.17,28 Patients with baseline bed ridden functional status were at high risk of death compared to those with ambulatory and working functional status. This finding was supported by a study done in Nepal.17 Bedridden functional status at HAART initiation reflects the worst health condition of patients. Therefore, the effects of these conditions of patients on mortality indicate that patients died mostly because of their late initiation of HAART when they had the worst health conditions.
Patients who had not disclosed their HIV status were at a 24% higher risk of death on multivariate analysis. The possible explanation for this difference might be those patients may fear stigma and discrimination. Patients with a history of PTB before starting HAART were at high risk of death as compared to those who had no history of TB for this study. This may be due to the relapse of TB during ART immunity is compromised. Poor adherence to HAART leads to virology, immunologic, and clinical failures; it leads to failure to suppress the viral load that leads to the development of opportunistic infections during ART. In this study patients’ pneumonia after the start of ART were at higher risk of death than those who do not develop pneumonia. The development of OIs after initiating HAART may be due to undiagnosed treatment failure. And the reason why needs to be explored. Poor adherence to HAART leads to virology, immunologic and clinical failure; it leads to a failure to suppress that leads to development of opportunistic infection during ART.
Patients taking INH prophylaxis during the follow-up period were at higher risk of death compared to those who were not. This might be due to these patients being more likely to develop.
This study showed a higher risk of death among ambulatory and bedridden patients. Other studies showed that ambulatory and bedridden patients were at higher risk of death than active patients. WHO clinical stage IV has a direct association with the health status of HIV patients.9
A study conducted in Uganda showed that non-adherent participants had a mortality of 43 deaths per 1,000 person-years and, after adjusting for age, sex, and educational level, were 2-times as likely to die as adherent participants.29
Limitation
The use of secondary data was a problem for data incompleteness.
Mortality might be overestimated since the real cause of death may not be investigated so that all deaths were considered as HIV/AIDS-related.
Conclusion
The study finding showed a high overall probability of survival among patients on HAART (86.33%) and mortality was high (13.67%) during the first 6 months of treatment.
Being ambulatory and bedridden functional status, age of respondents >43 years, past TB treatment, baseline WHO stage IV, pneumonia after HAART, INH prophylaxis, and disclosure status were found to be predictors of survival of HIV/AIDS patients.
Patients need to be encouraged to come forward for early HIV testing and counseling, and to initiate early treatment before the disease progresses to the advanced stages, and to disclose their HIV sero-status to their families.
Health workers need to do continual follow-up and focused care to identify and treat opportunistic infections early.
Physical examination and laboratory evaluation with strong counseling and advice regarding the implications of HIV infection and lifelong treatment for ART adherence is needed.
Determinants of death should be considered by health workers to enhance better clinical outcomes of HAART treatment.
Abbreviations
3TC, Lamivudine; ABC, Abacavir; AIDS, Acquired immune-deficiency syndrome; ANC, Ante-natal care; ART, Anti-retro-viral therapy; BMI, Body mass index; CDC, Center for disease control; CI, Confidence interval; CPT, Cotrimoxazole preventive therapy; D4T, Stavudine; DDI, Didanosine; DHS, Demographic health survey; EFV, Efavirenz; GNP, Gross national product; HAART, Highly active antiretroviral therapy; HC, Health center; HEP, Health extension program; Hgb, Hemoglobin; HIV, Human immune deficiency virus; HR, Hazard ratio; HSDP, Health sector development plan; LPV/r, Ritonavir-based Lopinavir; MoH, Ministry of health; NVP, Nevirapine; OIs, Opportunistic infections; PEPFAR, Presidents emergency plan for AIDS relief; POY, Person year per observation; RNA, Ribonucleic acid; SVQ/r, Ritonavir boosted saquinavir; SRS, Simple random sampling; TB, Tuberculosis; TDF, Tenofovir; TLC, Total lymphocyte count; VCT, Voluntary counseling and testing; ZDV, Zidovudine.
Data Sharing Statement
The datasets are available from the corresponding author with reasonable request.
Acknowledgment
We acknowledge the South Gondar zonal health department, and all health centers’ head, and ART clinic staffs cooperativeness during data collection. We would also like to thank the data collectors and supervisor for their hard work.
We would like to express our deepest gratitude to Bahir Dar University, college of medicine, and health science for giving this opportunity.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Self-sponsor.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gallo RC, Salahuddin SZ, Popovic M, et al. Frequent detection and isolation of cytopathic retroviruses (HTLV-III) from patients with AIDS and at risk for AIDS. Science. 1984;224(4648):500–503. doi:10.1126/science.6200936
2. Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16:18734. doi:10.7448/IAS.16.3.18734
3. Gandhi T, Wei W, Amin K, Kazanjian P. Effect of maintaining highly active antiretroviral therapy on AIDS events among patients with late-stage HIV infection and inadequate response to therapy. Clin Infect Dis. 2006;42(6):878–884. doi:10.1086/500210
4. Getachew T, Taye G, Defar A, Taddele T, Teklie H, Bekele A. Predictors of survival in HIV-infected patients under antiretroviral treatment in selected hospitals of Ethiopia. Ethiop J Public Health Nutr. 2020;3(1).
5. Berhane Y, Mekonnen Y, Seyoum E, Gelmon L, Wilson D. HIV/AIDS in Ethiopia—an epidemiological synthesis in World Bank Global HIV. AIDS Program; 2008.
6. World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. World Health Organization; 2015.
7. Alfvén T, Erkkola T, Ghys P, et al. Global AIDS reporting-2001 to 2015: lessons for monitoring the sustainable development goals. AIDS Behav. 2017;21(1):5–14. doi:10.1007/s10461-016-1662-9
8. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF. 2016. Available from: https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf. Accessed June 15, 2021.
9. Obi SN, Ifebunandu NA, Onyebuchi AK. Nutritional status of HIV-positive individuals on free HAART treatment in a developing nation. J Infect Dev Ctries. 2010;4(11):745–749. doi:10.3855/jidc.863
10. Mengesha S, Belayihun B, Kumie A. Predictors of survival in HIV-infected patient after Initiation of HAART in Zewditu Memorial Hospital, Addis Ababa, Ethiopia. Int Sch Res Notices. 2014;2014:1–6. doi:10.1155/2014/250913
11. HAPCO F. Annual performance report of multisectoral HIV/AIDS response 2002 EC (2009/2010). Addis Ababa: Federal HIV/AIDS Prevention and Control Office; 2010.
12. Ethiopia M. Country progress report on the HIV response, 2014. Addis Ababa: Federal Democratic Republic of Ethiopia; 2014.
13. Yirdaw BE, Wencheko E. Survival longevity of adult AIDS patients under ART: a case. Ethiop J Health Dev. 2020;28(2).
14. Abebe T, Chaka T, Misgana G, Adlo A. Determinants of survival among adults on antiretroviral therapy in Adama Hospital Medical College, Oromia Regional state, Ethiopia. J HIV AIDS. 2016;2(1).
15. Aziz N, Sokoloff A, Kornak J, et al. Time to viral load suppression in antiretroviral-naive and-experienced HIV-infected pregnant women on highly active antiretroviral therapy: implications for pregnant women presenting late in gestation. BJOG. 2013;120(12):1534–1547. doi:10.1111/1471-0528.12226
16. Ayele W, Mulugeta A, Desta A, Rabito FA. Treatment outcomes and their determinants in HIV patients on anti-retroviral treatment program in selected health facilities of Kembata and Hadiya zones, Southern Nations, Nationalities and Peoples Region, Ethiopia. BMC Public Health. 2015;15(1):1–13. doi:10.1186/s12889-015-2176-5
17. Bhatta L, Klouman E, Deuba K, et al. Survival on antiretroviral treatment among adult HIV-infected patients in Nepal: a retrospective cohort study in far-western Region, 2006–2011. BMC Infect Dis. 2013;13(1):1–9. doi:10.1186/1471-2334-13-604
18. Abebe N, Alemu K, Asfaw T, Abajobir AA. Survival status of hiv positive adults on antiretroviral treatment in Debre Markos Referral Hospital, Northwest Ethiopia: retrospective cohort study. Pan Afr Med J. 2014;17. doi:10.11604/pamj.2014.17.88.3262
19. Tweya H, Feldacker C, Breeze E, et al. Incidence of pregnancy among women accessing antiretroviral therapy in urban Malawi: a retrospective cohort study. AIDS Behav. 2013;17(2):471–478. doi:10.1007/s10461-012-0150-0
20. Roura M, Busza J, Wringe A, Mbata D, Urassa M, Zaba B. Barriers to sustaining antiretroviral treatment in Kisesa, Tanzania: a follow-up study to understand attrition from the antiretroviral program. AIDS Patient Care STDS. 2009;23(3):203–210. doi:10.1089/apc.2008.0129
21. Tadele A, Shumey A, Hiruy N. Survival and predictors of mortality among adult patients on highly active antiretroviral therapy at debre-markos referral hospital, North West Ethiopia; a retrospective cohort study. J AIDS Clin Res. 2014;5(280):2.
22. Poka-Mayap V, Pefura-Yone EW, Kengne AP, Kuaban C. Mortality and its determinants among patients infected with HIV-1 on antiretroviral therapy in a referral centre in Yaounde, Cameroon: a retrospective cohort study. BMJ Open. 2013;3(7):e003210. doi:10.1136/bmjopen-2013-003210
23. Lin K-Y, Cheng C-Y, Li C-W, et al. Trends and outcomes of late initiation of combination antiretroviral therapy driven by late presentation among HIV-positive Taiwanese patients in the era of treatment scale-up. PLoS One. 2017;12(6):e0179870. doi:10.1371/journal.pone.0179870
24. Rangarajan S, Colby DJ, Bui DD, et al. Factors associated with HIV viral load suppression on antiretroviral therapy in Vietnam. J Virus Erad. 2016;2(2):94–101. doi:10.1016/S2055-6640(20)30466-0
25. Joseph B, Wood E, Hayashi K, et al. Factors associated with initiation of antiretroviral therapy among HIV-positive people who use injection drugs in a Canadian setting. AIDS. 2016;30(6):925. doi:10.1097/QAD.0000000000000989
26. Johannessen A, Naman E, Ngowi BJ, et al. Predictors of mortality in HIV-infected patients starting antiretroviral therapy in a rural hospital in Tanzania. BMC Infect Dis. 2008;8(1):1–10. doi:10.1186/1471-2334-8-52
27. Swain PK, Grover G. Determination of predictors associated with HIV/AIDS patients on ART using accelerated failure time model for interval censored survival aata. Am J Biostat. 2016;6:12–19.
28. Bucciardini R, Fragola V, Abegaz T, et al. Retention in care of adult HIV patients initiating antiretroviral therapy in Tigray, Ethiopia: a prospective observational cohort study. PLoS One. 2015;10(9):e0136117. doi:10.1371/journal.pone.0136117
29. Kunutsor S, Walley J, Katabira E, et al. Improving clinic attendance and adherence to antiretroviral therapy through a treatment supporter intervention in Uganda: a randomized controlled trial. AIDS Behav. 2011;15(8):1795–1802. doi:10.1007/s10461-011-9927-9
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
