Back to Journals » Cancer Management and Research » Volume 13
Survival Effects of Radiotherapy on Patients Newly Diagnosed with Distant Metastatic Nasopharyngeal Carcinoma in Non-High-Incidence Areas
Authors Yang Y, Li X, Zhou P, Deng X, Wang Y, Dang Q, Zheng Y, Yang D
Received 20 August 2021
Accepted for publication 21 October 2021
Published 2 November 2021 Volume 2021:13 Pages 8169—8178
DOI https://doi.org/10.2147/CMAR.S334958
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Yong Teng
Yongqiang Yang, Xiaole Li, Pengcheng Zhou, Xiaoyu Deng, Yingyi Wang, Qianqian Dang, Yingjuan Zheng, Daoke Yang
Department of Radiotherapy, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, Henan, People’s Republic of China
Correspondence: Yingjuan Zheng; Daoke Yang
Department of Radiotherapy, The First Affiliated Hospital of Zhengzhou University, No. 1 Jianshe East Road, Zhengzhou, 450052, Henan Province, People’s Republic of China
Tel +86-15738872856
; +86-15903650068
Email [email protected]; [email protected]
Purpose: To analyze the effects of radiotherapy and its timing on the survival and safety of patients with newly diagnosed distant metastatic NPC in non-high-incidence areas.
Patients and Methods: We retrospectively analyzed 94 newly diagnosed NPC patients with distant metastatic admitted to our hospital from January 2011 to June 2018. They were divided into three groups: no radiotherapy group received chemotherapy alone, early radiotherapy group was combined with radiotherapy during 1 to 3 cycles of chemotherapy, and late radiotherapy group was combined with radiotherapy after 4– 6 cycles of chemotherapy were effective. The efficacy and side effects of the three groups were compared, and the prognostic factors were analyzed.
Results: The 6-month, 1-year and 2-year PFS were 53.6%, 14.3% and 3.6% in no radiotherapy group, 71.0%, 38.7% and 19.4% in early radiotherapy group, 88.6%, 48.6% and 22.9% in late radiotherapy group; the radiotherapy groups were better than the no radiotherapy group, and the difference was statistically significant (P < 0.017). The 1-year, 2-year and 3-year OS were 75.0%, 32.1% and 0 in no radiotherapy group, 77.4%, 54.8% and 12.9% in early radiotherapy group, 85.7%, 71.4% and 31.4% in late radiotherapy group; the radiotherapy groups were better than the no radiotherapy group, and the differences were statistically significant (P < 0.017). There was no significant difference in OS and PFS between the two radiotherapy groups. Univariate and multivariate analysis showed that HBV (P = 0.031), number of metastases (P = 0.002), liver metastases (P = 0.038), radiotherapy (P < 0.001) and treatment response (P = 0.011) were related to OS. There was no significant difference in the incidence of adverse events (P > 0.017).
Conclusion: Early and late combined radiotherapy had similar clinical efficacy and both prolonged PFS and OS for patients with newly diagnosed distant metastatic NPC in non-high-risk areas. If chemotherapy response is expected to be poor, radiotherapy can be received early.
Keywords: radiotherapy, nasopharyngeal carcinoma, metastasis, non-high-incidence area, prognosis
Introduction
Nasopharyngeal carcinoma (NPC) originates from the epithelium of the nasopharyngeal mucosa. More than 70% of new cases worldwide occur in East Asia and Southeast Asia and it is closely related to genetics, race, environment and lifestyle.1 The age-standardized incidence rate by the world standard population (ASIRW) in South China (9.69/100,000) was 11.4 times higher than that in Henan (0.85/100,000), one of the non-high incidence areas in North China.2,3 With the advancement of intensity-modulated radiotherapy (IMRT) and comprehensive diagnosis and treatment technology, the 3-year local control rate of non-metastatic NPC has reached 80% to 90%, and the 5-year overall survival rate has exceeded 80%.4 Distant metastasis has become an important factor in the failure of clinical treatment and the reduction of patient survival. About 4% to 10% of patients with NPC have distant metastases when they are first diagnosed, which is a special and rare type of NPC.1 Compared with secondary metastases after treatment, the prognosis of newly diagnosed patients with metastatic NPC (mNPC) is extremely poor, and there is a big difference in the treatment mode between the two. For metastatic NPC, chemotherapy is still the first choice for treatment. But a study found that radiotherapy combined with chemotherapy for newly diagnosed mNPC patients was associated with longer median overall survival (OS) compared to chemotherapy alone (21.4 vs 15.5 months).5 This effect was also seen in some other metastatic tumors.6,7 However, there has been no detailed study of the effects of radiotherapy on NPC patients in non-high-risk areas. This study retrospectively analyzed the treatment and survival data of patients with newly diagnosed distant mNPC in non-high-incidence areas in northern China, and explored the effects of the presence or absence of radiotherapy and the timing of its application on tumor control and patient survival, and pointed out the direction for its treatment.
Materials and Methods
Patients and Selection Criteria
This study selected newly diagnosed patients with mNPC who came from the non-high-incidence areas and were admitted to our hospital from January 2011 to June 2018. All patients were clearly diagnosed with pathology and were assisted by color Doppler ultrasound, ECT, CT, MRI and PET-CT before treatment to confirm the distant metastasis, and the TNM stage was reclassified according to the 8th edition staging of the American Joint Committee on Cancer (AJCC). Exclusion criteria: (1) merge other tumors; (2) unknown radiotherapy and chemotherapy regimens; (3) incomplete follow-up data; (4) from high-risk areas.
This study was conducted in accordance with the tenets of the Helsinki declaration and was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. Written informed consent was obtained from all participants. All protocols were performed in accordance with the relevant guidelines and regulations.
Grouping and Treatment
All patients were treated with platinum-based combination chemotherapy and divided into 3 groups according to whether they received radiotherapy during chemotherapy and the timing of radiotherapy: no radiotherapy group, early radiotherapy group, and late radiotherapy group. The non-radiotherapy group included patients who received chemotherapy alone, the early radiotherapy group included patients who received radiotherapy during 1 to 3 cycles of chemotherapy, and the late radiotherapy group included patients who received radiotherapy when the tumor achieved complete response (CR), partial response (PR) or stable disease (SD) after 4–6 cycles of chemotherapy. The sequence of radiotherapy and chemotherapy is synchronous, sequential or alternating. Intensity modulated radiotherapy (IMRT) was used for radiotherapy, and the target areas of radiotherapy were nasopharyngeal, positive lymph nodes and cervical lymph node drainage areas. The radiotherapy dose for nasopharyngeal lesions was 59.36–69.96Gy. The target areas were delineated based on the gross tumor after chemotherapy. GTVnx included the primary tumor of the nasopharynx and the invasion area, and GTVnd included the positive lymph nodes in the neck. The clinical target volume (CTV) included CTV1 and CTV2: CTV1 (high-risk area) included the adjacent area that may be invaded around the primary tumor, including the entire nasopharynx, retropharyngeal lymph node area, slope, skull base, parapharyngeal space, pterygopalatine fossa, sphenoid sinus, nasal cavity and posterior 1/3 of the maxillary sinus; CTV2 was defined as low-risk node region outside the CTV1, including areas at risk of harboring microscopic disease and elective lymph node groups.
Patient Evaluation and Follow-Up
Patients were followed up via the medical record system and telephone calls. During treatment, the comprehensive evaluation was conducted every 2 cycles. After treatment, the follow-up was performed every 3 months for the first 2 years and every 6 months after 2 years. The deadline for follow-up was June 2021. The Response Evaluation Criteria in Solid Tumors (RECIST; version 1.1) was used for efficacy evaluation,8 which was divided into CR, PR, SD and progressive disease (PD). The primary endpoint of the study was OS, which was defined as the time from pathological diagnosis to death of the patient or the last follow-up. The secondary endpoints were progression-free survival (PFS) and objective response rate (ORR). PFS was defined as the time from pathological diagnosis to the appearance of imaging confirmed disease progression or death or the last follow-up, and ORR was the proportion of patients evaluated as CR and PR. The safety evaluation was carried out according to the Common Terminology Criteria for Adverse Events (CTCAE; version 4.0).9
Statistical Analysis
We use SPSS (version 21.0) to perform statistical analysis. Comparison of measurement data between groups was performed by t-test, and comparison of counting data between groups was performed by χ2 test or Fisher’s exact probability method; Kaplan–Meier method was used to draw survival curve and Log-rank method was used to compare survival rate differences between groups; ANOVA was used for univariate analysis, the COX proportional hazard regression model for multivariate analysis. P<0.050 was considered statistically significant, and the differences of pairwise comparisons between three groups are considered to be statistically significant when P<0.017 according to Bonferroni correction.
Results
General Clinical Data
According to the criteria, 94 patients were included in the analysis, including 73 males and 21 females, with a median age of 48.5 years. They all came from the local area. A total of 37 patients received local treatment for metastases, 89 patients received 4 or more chemotherapy cycles, and 15 patients received targeted therapy such as nimotuzumab or apatinib. The patients were divided into groups according to the treatment method. There were 28 patients in the no radiotherapy group, 31 in the early radiotherapy group, and 35 in the late radiotherapy group. The clinical data of the patients in each group are shown in Table 1. Except for the sequence of radiotherapy and chemotherapy, the other differences were not statistically significant, and they were clinically comparable.
 |
Table 1 Clinical Characteristics and Comparison of the Three Groups of Patients (n=94) |
Survival
Until the follow-up deadline, 15 (16.0%) of all 94 patients had a follow-up time of 36 months or longer, including 4 in the early radiotherapy group and 11 in the late radiotherapy group; and there were 2 (2.1%) patients reaching 48 and 55 months, respectively, only existing in the late radiotherapy group. The OS of all patients reached more than 6 months. The 1-year, 2-year and 3-year OS rates were 75.0%, 32.1% and 0 in the no radiotherapy group, 77.4%, 54.8% and 12.9% in the early radiotherapy group, 85.7%, 71.4% and 31.4% in the late radiotherapy group, respectively. Compared to the OS of three groups, the late radiotherapy group was better than the early radiotherapy group (χ2=4.132, P=0.042) and the no radiotherapy group (χ2=21.864, P<0.001), and the early radiotherapy group was better than the no radiotherapy group (χ2=7.403, P=0.007). After Bonferroni correction, the difference of OS between the late radiotherapy group and early radiotherapy group was not statistically significant. Detailed survival data and comparison were shown in Table 2 and Figure 1A. Univariate analysis showed that targeted therapy (P=0.024), HBV infection (P=0.043), N classification (P=0.010), multiple organ metastases (P=0.011), the number of distant metastatic lesions (P<0.001), liver metastases (P=0.002), local treatment of metastases (P=0.001), radiotherapy (P<0.001), the number of chemotherapy cycles (P=0.018) and treatment response (P<0.001) were related to the patient’s OS. Multivariate analysis showed that HBV infection (P=0.031), the number of distant metastatic lesions (P=0.002), liver metastases (P=0.038), radiotherapy (P<0.001) and treatment response (P=0.011) were related to the patient’s OS, as illustrated in Table 3.
 |
Table 2 Treatment Efficacy (n=94) |
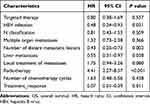 |
Table 3 Multivariate Analysis of Prognostic Factors for OS |
At the end of the treatment, the ORRs of the no radiotherapy group, the early radiotherapy group, and the late radiotherapy group were 60.7%, 83.9% and 91.4%, respectively. There were 5 patients in the no radiotherapy group and 1 patient in the early radiotherapy group who had disease progression during initial treatment and received other treatment. The remaining patients had disease progression during follow-up. The PFS of 15 patients reached two years or more, including 1 case in the no radiotherapy group, 6 cases in the early radiotherapy group and 8 cases in the late radiotherapy group. And there were 2 patients whose PFS reached three years or more in the late radiotherapy group. The 6-month, 1-year and 2-year PFS rates were 53.6%, 14.3% and 3.6% in the no radiotherapy group, 71.0%, 38.7% and 19.4% in the early radiotherapy group, 88.6%, 48.6% and 22.9% in the late radiotherapy group, respectively. The PFS of the late radiotherapy group was significantly better than that of the no radiotherapy group (χ2=19.633, P<0.001), and the PFS of the early radiotherapy group was also better than that of the no radiotherapy group (χ2=8.224, P=0.004). After Bonferroni correction, the differences were statistically significant. The PFS of the late radiotherapy group was better than that of the early radiotherapy group according to the survival rate data, but the difference was not statistically significant (χ2=2.622, P=0.105). Detailed survival data and comparison are shown in Table 2 and Figure 1B.
Adverse Events
A total of 94 patients in the three groups were included in the safety analysis. In terms of hematological toxicity, leukopenia was prominent among high-grade toxicity. The proportions of grade 3–4 leukopenia in the no radiotherapy group, early radiotherapy group and late radiotherapy group were 14.3%, 32.3% and 20.0%, respectively, which were higher than other blood toxic reaction. Overall, the proportions of grade 2 and grade 3–4 adverse reactions in the early radiotherapy group and the late radiotherapy group were higher than that of the no radiotherapy group, but there was no significant difference among the three groups (P>0.017). The gastrointestinal toxicity and hepatotoxicity were mainly low-level reactions, and there was no statistically significant difference in the data of each group (P>0.050). There was no obvious nephrotoxicity in the three groups. Radiotherapy-related adverse reaction was mucositis, and only occurred in radiotherapy groups. The main reactions were grade 0–1 and grade 2. There were 3 cases (9.7%) and 2 cases (5.7%) of grade 3–4 mucositis in the early radiotherapy group and late radiotherapy group, respectively, and the difference was not statistically significant (P>0.050). Detailed data and comparison are shown in Table 4.
 |
Table 4 Adverse Events and Comparison of the Three Groups of Patients (n=94) |
Discussion
NPC has the highest metastatic potential for head and neck malignant tumors, and its distant metastasis is the main reason for reducing the survival of patients. In this study, 51.1% of patients had multiple organ metastases and 59.6% of patients had more than 3 distant metastatic lesions at the time of diagnosis. Bone, liver and lung were the most common metastatic organs. Almost all patients had neck lymph node metastasis. Systemic chemotherapy is the first choice for the treatment of metastatic NPC, but the results of monotherapy are not satisfactory. A survival analysis of newly diagnosed mNPC patients from the NCDB database showed that radiotherapy can significantly improve patients’ survival, and a later T stage predicts poor OS.5 A multi-center Phase 3 clinical trial conducted by You et al10 showed that chemotherapy combined with radiotherapy can increase the 2-year OS rate of newly diagnosed mNPC patients from 54.5% to 76.4% compared with chemotherapy alone, and PFS had also been significantly improved. These findings suggest that local tumor invasion is an important factor affecting the survival of NPC patients, and strengthening local control of nasopharyngeal primary tumors through radiotherapy and other methods can improve the long-term survival of newly diagnosed mNPC patients. However, most of current studies focus on patients in the high-incidence area. The incidence and death of NPC patients have regional and population differences.1,11,12 Therefore, the treatment response of newly diagnosed metastatic patients in non-high-incidence areas still remains uncertain. This study included 94 newly diagnosed NPC patients with distant metastasis from the low-risk areas in northern China. Twenty-two patients who were followed up for more than 3 years were from the radiotherapy group. The PFS and OS of the early radiotherapy group and the late radiotherapy group were significantly better than those of the no radiotherapy group. This is the first time that chemotherapy combined with radiotherapy can improve long-term survival of newly diagnosed mNPC patients in a non-high-incidence area. The possible mechanism of radiotherapy to prolong PFS and OS in newly diagnosed distant mNPC patients is to reduce the tumor burden of the primary tumor, improve the local control rate of the tumor, while systemic treatment, and reduce the possibility of re-metastasis; another possible mechanism may be that local radiotherapy may promote the production and release of certain cytokines to inhibit the proliferation and metastasis of primary and metastatic tumor cells, which is called the abscopal responses.13
The role of radiotherapy in newly diagnosed mNPC is gradually being recognized, but there are still some controversies about the timing of radiotherapy. Some consensuses recommend that patients who achieve CR/PR/SD after platinum-based systemic chemotherapy could choose to continue chemotherapy or receive nasopharyngeal and neck radiotherapy.14,15 The clinical trial of You et al10 selected patients who achieved CR/PR after 3 cycles of PF chemotherapy to be enrolled in the group, and then received local radiotherapy after 6 cycles of PF chemotherapy. However, it should be noted that not all patients can achieve the desired effect in early chemotherapy, and there are still a certain proportion of patients who do not respond well to chemotherapy or even progress. In one study, the proportion of patients who failed to achieve CR/PR after palliative chemotherapy accounted for 36.9%, and local radiotherapy for this part of patients had little effect on their survival.16 The above results show that if clinical practice was carried out according to the current expert consensus, patients with unsatisfactory early chemotherapy results would lose the opportunity to benefit from radiotherapy; on the other hand, the combined modes of radiotherapy and chemotherapy for newly diagnosed mNPC patients included in the NCDB database are mainly synchronized chemoradiotherapy and induction chemotherapy followed by radiotherapy, these two modes have significantly improved the survival of patients compared with chemotherapy alone.5 However, the analysis is based on NPC patients in the United States, and there is no comparative study of the two modes and timing of radiotherapy. Radiotherapy and chemotherapy are the standard treatment options for stage II and locally advanced NPC. Among different sequences, concurrent chemoradiotherapy has the best effect.17 Therefore, whether early combined radiotherapy can change the unsatisfactory outcome of patients who are not sensitive to early chemotherapy alone, so that patients can achieve long-term survival. Based on that, this study compared the survival difference between the non-radiotherapy group and the early radiotherapy group. The results showed that the PFS and OS of the early radiotherapy group were better than those of the no radiotherapy group and similar to the late radiotherapy group. This suggests that early radiotherapy can also improve survival and may change the survival outcome of patients who are not sensitive to early chemotherapy.
Such patients who do not respond well to chemotherapy require more personalized treatment, but they are often ignored in clinical practice and research. Therefore, the ability to identify these patients with the help of some indicators or scoring systems so that the new NPC patients can be stratified before the treatment, is very important for the rational choice of radiotherapy timing and the development of personalized treatment plans. Four independent prognostic factors including nutritional risk index, C-reactive protein level, alkaline phosphatase level, and lactate dehydrogenase level in newly diagnosed patients with mNPC were used to construct a scoring system for evaluating the efficacy of first-line chemotherapy.18 For those patients who are predicted to be less effective in chemotherapy, it should be recommended to receive radiotherapy early to better control the disease and increase follow-up for early detection of tumor progression. In addition, some studies have found that for newly diagnosed mNPC patients without liver metastasis, regardless of the number of metastases, they can benefit from chemotherapy combined with radiotherapy, but this benefit is not obvious to patients with liver metastases.19 Patients whose EBV DNA turns negative after palliative chemotherapy have more obvious benefits from radiotherapy.16 Therefore, even patients with better chemotherapy effects still need to undergo further screening. The model established by Li et al20 is to predict suitable candidates for radiotherapy based on palliative chemotherapy, which is of great significance to the individualization and precision of radiotherapy.
The commonly used TNM classification is based on the invaded anatomy and is widely used in patients with non-metastatic NPC, but the classification of distant metastases is not detailed enough. The M1 sub-classification system established based on the number of metastatic organ and metastatic foci is closely related to the prognosis of patients. This is an important basis for stratifying, guiding treatment, and prognostic judgment of metastatic patients.19,21 It is consistent with the analysis results of this study. Plasma EBV-DNA levels are closely related to NPC, and have important clinical prognostic value for patients with non-metastatic, metastatic and recurrent NPC,22–24 and are also closely related to the prognosis of patients with newly diagnosed mNPC.25 Differentially expressed gene models established based on metastatic and non-metastatic NPC tissue26 and liver metastasis subgroup,27 as well as serum lactate dehydrogenase, EBV and HPV, PET/CT metabolic indicators, etc.16,28,29 are useful for predicting the prognosis and risk of metastasis. Sun et al25 established a risk score and grouping system based on age, N stage, EBV-DNA level, number of metastases and metastatic organs, which is closely related to the 3-year and 5-year OS of patients, and are useful for judging the prognosis. In addition to the above-mentioned existing indicators, this study shows that whether or not to be infected with HBV and radiotherapy are related to OS, and treatment response is also an important reference for judging OS.
For those patients who have chemotherapy failure or are expected to have poor chemotherapy response, it is necessary to find appropriate treatments to prolong survival. The combination of immune checkpoint inhibitors and chemotherapy shows good anti-tumor activity and can significantly prolong PFS in patients with recurrent or metastatic NPC,30 but the effect on long-term survival still needs further observation. Patients with low levels of EBV DNA (≤30,000 copies/mL) before treatment can benefit from capecitabine maintenance treatment.31 Stereotactic ablative radiotherapy (SABR) for oligometastasis has been preliminarily proven to improve patient survival.32,33 For newly diagnosed NPC patients with metastatic tumors, radiotherapy for metastases or local radiotherapy for patients with oligometastasis regardless of chemotherapy response may be an opportunity,34 but this needs further research to confirm.
There are several limitations to this study. First, this was a retrospective study, and selection bias and other variables might affect the results. Second, there was a lack of research on patients’ quality of life and EBV DNA. Third, the low incidence resulted in a small number of patients enrolled, and the patients all came from one treatment center. Therefore, it is necessary to further verify the results through multi-center prospective studies, including more cases and more detailed clinical data.
Conclusion
To sum up, compared with chemotherapy alone, early combined radiotherapy and late combined radiotherapy had similar clinical efficacy and both prolonged PFS and OS for patients with newly diagnosed distant mNPC in non-high-risk areas. Early combined radiotherapy benefited these patients who were estimated to be insensitive to early chemotherapy alone.
Acknowledgments
We acknowledge the support of the Department of Radiotherapy. The views expressed in this publication are those of the authors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chen YP, Chan ATC, Le QT, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394(10192):64–80. doi:10.1016/S0140-6736(19)30956-0
2. Wei KR, Zheng RS, Zhang SW, Liang ZH, Li ZM, Chen WQ. Nasopharyngeal carcinoma incidence and mortality in China, 2013. Chin J Cancer. 2017;36(1):90. doi:10.1186/s40880-017-0257-9
3. Huifang CQ, Yin L, Shuzheng L, et al.Analysis of incidence and mortality of nasopharyngeal carcinoma in Henan Province, 2016. Chin J Oncol Prev Treat. 2021;13(3):262–266.
4. Wang F, Jiang C, Wang L, et al. Different risk target volumes for nasopharyngeal carcinoma treated with simultaneous integrated boost intensity-modulated radiotherapy. J Cancer. 2020;11(17):5210–5222. doi:10.7150/jca.45767
5. Rusthoven CG, Lanning RM, Jones BL, et al. Metastatic nasopharyngeal carcinoma: patterns of care and survival for patients receiving chemotherapy with and without local radiotherapy. Radiother Oncol. 2017;124(1):139–146. doi:10.1016/j.radonc.2017.03.019
6. Zhang CH, Pan YB, Zhang QW, et al. The influence of local therapy on the survival of patients with metastatic rectal cancer: a population-based, propensity-matched study. J Cancer Res Clin Oncol. 2017;143(9):1891–1903. doi:10.1007/s00432-017-2442-2
7. Wang CJ, Christie A, Lin MH, et al. Safety and efficacy of stereotactic ablative radiation therapy for renal cell carcinoma extracranial metastases. Int J Radiat Oncol Biol Phys. 2017;98(1):91–100. doi:10.1016/j.ijrobp.2017.01.032
8. Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer (Oxford, England: 1990). 2009;45(2):228–247. doi:10.1016/j.ejca.2008.10.026
9. National Cancer Institute (US). Common terminology criteria for adverse events (CTCAE) v4.0. 2009.
10. You R, Liu YP, Huang PY, et al. Efficacy and safety of locoregional radiotherapy with chemotherapy vs chemotherapy alone in de novo metastatic nasopharyngeal carcinoma: a multicenter phase 3 randomized clinical trial. JAMA Oncol. 2020;6(9):1345–1352. doi:10.1001/jamaoncol.2020.1808
11. Yu MC, Garabrant DH, Huang TB, Henderson BE. Occupational and other non-dietary risk factors for nasopharyngeal carcinoma in Guangzhou, China. Int J Cancer. 1990;45(6):1033–1039. doi:10.1002/ijc.2910450609
12. Yuan JM, Wang XL, Xiang YB, Gao YT, Ross RK, Yu MC. Non-dietary risk factors for nasopharyngeal carcinoma in Shanghai, China. Int J Cancer. 2000;85(3):364–369. doi:10.1002/(SICI)1097-0215(20000201)85:3<364::AID-IJC12>3.0.CO;2-C
13. Golden EB, Chhabra A, Chachoua A, et al. Local radiotherapy and granulocyte-macrophage colony-stimulating factor to generate abscopal responses in patients with metastatic solid tumours: a proof-of-principle trial. Lancet Oncol. 2015;16(7):795–803. doi:10.1016/S1470-2045(15)00054-6
14. Lang J, Gao L, Guo Y, et al. Comprehensive treatment of squamous cell cancer of head and neck: Chinese expert consensus 2013. Future Oncol (London, England). 2014;10(9):1635–1648. doi:10.2217/fon.14.44
15. Lang J, Hu C, Lu T, Pan J, Lin T. Chinese expert consensus on diagnosis and treatment of nasopharyngeal carcinoma: evidence from current practice and future perspectives. Cancer Manag Res. 2019;11:6365–6376. doi:10.2147/CMAR.S197544
16. Sun X-S, Liu L-T, Liu S-L, et al. Identifying optimal candidates for local treatment of the primary tumor among patients with de novo metastatic nasopharyngeal carcinoma: a retrospective cohort study based on Epstein-Barr virus DNA level and tumor response to palliative chemotherapy. BMC Cancer. 2019;19(1):92. doi:10.1186/s12885-019-5281-5
17. Bhattacharyya T, Babu G, Kainickal CT. Current role of chemotherapy in nonmetastatic nasopharyngeal cancer. J Oncol. 2018;2018:3725837. doi:10.1155/2018/3725837
18. Li WZ, Hua X, Lv SH, et al. A scoring system based on nutritional and inflammatory parameters to predict the efficacy of first-line chemotherapy and survival outcomes for de novo metastatic nasopharyngeal carcinoma. J Inflamm Res. 2021;14:817–828. doi:10.2147/JIR.S296710
19. Zou X, You R, Liu H, et al. Establishment and validation of M1 stage subdivisions for de novo metastatic nasopharyngeal carcinoma to better predict prognosis and guide treatment. Eur J Cancer (Oxford, England: 1990). 2017;77:117–126. doi:10.1016/j.ejca.2017.02.029
20. Li WZ, Lv SH, Liu GY, et al. Development of a prognostic model to identify the suitable definitive radiation therapy candidates in de novo metastatic nasopharyngeal carcinoma: a real-world study. Int J Radiat Oncol Biol Phys. 2021;109(1):120–130. doi:10.1016/j.ijrobp.2020.08.045
21. Shen LJ, Wang SY, Xie GF, et al. Subdivision of M category for nasopharyngeal carcinoma with synchronous metastasis: time to expand the M categorization system. Chin J Cancer. 2015;34(10):450–458. doi:10.1186/s40880-015-0031-9
22. Wang WY, Twu CW, Chen HH, et al. Long-term survival analysis of nasopharyngeal carcinoma by plasma Epstein-Barr virus DNA levels. Cancer. 2013;119(5):963–970. doi:10.1002/cncr.27853
23. Wang W-Y, Twu C-W, Chen -H-H, et al. Plasma EBV DNA clearance rate as a novel prognostic marker for metastatic/recurrent nasopharyngeal carcinoma. Clin Cancer Res. 2010;16(3):1016–1024. doi:10.1158/1078-0432.CCR-09-2796
24. An X, Wang FH, Ding PR, et al. Plasma Epstein-Barr virus DNA level strongly predicts survival in metastatic/recurrent nasopharyngeal carcinoma treated with palliative chemotherapy. Cancer. 2011;117(16):3750–3757. doi:10.1002/cncr.25932
25. Sun XS, Liang YJ, Liu SL, et al. Establishment and validation of a nomogram for predicting survival in patients with de novo metastatic nasopharyngeal carcinoma. Oral Oncol. 2019;94:73–79. doi:10.1016/j.oraloncology.2019.05.015
26. Tang XR, Li YQ, Liang SB, et al. Development and validation of a gene expression-based signature to predict distant metastasis in locoregionally advanced nasopharyngeal carcinoma: a retrospective, multicentre, cohort study. Lancet Oncol. 2018;19(3):382–393. doi:10.1016/S1470-2045(18)30080-9
27. Han C, Yang JL, Yao KT. [Gene expression profiling of nasopharyngeal carcinoma cell line 5-8F-EGFP and the liver metastatic 5-8F-H3B-EGFP cells]. Nan Fang Yi Ke Da Xue Xue Bao = Journal of Southern Medical University. 2011;31(3):473–477. Chinese.
28. Zhou GQ, Tang LL, Mao YP, et al. Baseline serum lactate dehydrogenase levels for patients treated with intensity-modulated radiotherapy for nasopharyngeal carcinoma: a predictor of poor prognosis and subsequent liver metastasis. Int J Radiat Oncol Biol Phys. 2012;82(3):e359–e365. doi:10.1016/j.ijrobp.2011.06.1967
29. Chua MLK, Wee JTS, Hui EP, Chan ATC. Nasopharyngeal carcinoma. Lancet (London, England). 2016;387(10022):1012–1024. doi:10.1016/S0140-6736(15)00055-0
30. Yang Y, Qu S, Li J, et al. Camrelizumab versus placebo in combination with gemcitabine and cisplatin as first-line treatment for recurrent or metastatic nasopharyngeal carcinoma (CAPTAIN-1st): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2021;22:1162–1174. doi:10.1016/S1470-2045(21)00302-8
31. Sun X-S, Liu S-L, Liang Y-J, et al. The role of capecitabine as maintenance therapy in de novo metastatic nasopharyngeal carcinoma: a propensity score matching study. Cancer Commun (Lond). 2020;40(1):32–42. doi:10.1002/cac2.12004
32. Palma DA, Olson R, Harrow S, et al. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet. 2019;393(10185):2051–2058. doi:10.1016/S0140-6736(18)32487-5
33. Palma DA, Olson R, Harrow S, et al. Stereotactic ablative radiotherapy for the comprehensive treatment of oligometastatic cancers: long-term results of the SABR-COMET phase II randomized trial. J Clin Oncol. 2020;38(25):2830–2838. doi:10.1200/JCO.20.00818
34. McDowell L, Rischin D, Lee AWM. Locoregional radiation therapy for de novo metastatic nasopharyngeal cancer: one size fits all? Int J Radiat Oncol Biol Phys. 2021;109(1):131–133. doi:10.1016/j.ijrobp.2020.10.001
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

