Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 12
Survival and Predictors of Mortality Among Neonates Admitted to Neonatal Intensive Care Unit at Bombe Primary Hospital, Southern Ethiopia: Institution-Based Retrospective Cohort Study
Authors Berhanu B, Oljira L , Demana M, Negash B, Mamo Ayana G , Beshir Raru T , Haile D
Received 23 January 2021
Accepted for publication 28 April 2021
Published 18 May 2021 Volume 2021:12 Pages 239—249
DOI https://doi.org/10.2147/PHMT.S303158
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Bizuayehu Berhanu,1 Lemessa Oljira,2 Melake Demana,3 Belay Negash,4 Galana Mamo Ayana,3 Temam Beshir Raru,3 Dereje Haile5
1Department of Maternal and Child Health Core Process, Wolaita Zone, Southern Ethiopia, Ethiopia; 2Department of Reproductive Health, School of Public Health, Haramaya University, Harar, Ethiopia; 3Department of Epidemiology and Biostatistics, School of Public Health, Haramaya University, Harar, Ethiopia; 4Department of Public Health and Health Policy, School of Public Health, College of Health and Medical Science Haramaya University, Harar, Ethiopia; 5Department of Reproductive Health and Nutrition, School of Public Health, College of Medicine and Health Science, Wolaita Sodo University, Sodo, Ethiopia
Correspondence: Dereje Haile PO Box=135, Sodo, Southern Ethiopia, Ethiopia
Email [email protected]
Belay Negash PO Box=235, Harer, Eastern Ethiopia, Ethiopia
Email [email protected]
Background: Neonatal mortality includes all deaths of neonate occurring before the 28th day of life. Neonatal mortality has been declining over two decades in Sub-Saharan Africa, including Ethiopia. The foremost causes of death are preventable and treatable. Regardless, recognizing the predictors may be a crucial step in lowering neonatal mortality. However, evidences on the survival status of neonates and/or neonatal death predictors were limited in Ethiopia, particularly in the study area. Thus, this study aimed to answer these questions.
Methods: An institution-based retrospective cohort study was done among 380 Neonates admitted to the Neonatal Intensive Care Unit at Bombe Primary Hospital from January 1, 2018, to December 31, 2019. Bivariable and multivariable Cox regression analyses were conducted to identify predictors of mortality. Association was summarized using adjusted hazard ratio (AHR), and statistical significances were declared at 95% CI and P-value < 0.05. Proportionality assumption was tested by a global test based on Schoenfeld residuals analysis.
Results: The overall incidence of neonatal mortality was 20.8 (95% CI: 15.2, 28.5) per 1000 neonatal days. Late initiation of early breastfeeding (EBF) after 1 hr. [AHR: 2.9; 95% CI: 1.32, 6.37], 5th min APGAR score < 5 [AHR: 3; 95% CI: 1.32; 6.88], low birth weight [AHR: 2.59; 95% CI: 1.1,6.26], hypothermia [AHR: 2.6; 95% CI: 1.1, 6.22] and mothers’ time of rupture of membrane > 12 hours before delivery [AHR: 2.49; 95% CI: 1.25, 4.97] were increased the risk of neonatal mortality, while cesarean section delivery 91.6% [AHR= 0.084; 95% CI: 0.10, 0.65] and antenatal care (ANC) utilization 61% [AHR: 0.39; 95% CI: 0.15– 0.91] decreased the risk of neonatal mortality.
Conclusion: The incidence of neonatal mortality rate was high at the Bombe primary hospital. Therefore, to improve neonatal survival, it is recommended that complications and low birth weight be managed, that early exclusive breastfeeding be initiated, that service quality be improved, and that a continuum of care be ensured.
Keywords: neonatal mortality, Wolaita Zone, neonatal intensive care unit, neonate
Background
The neonatal period refers to the first 28 days of life, which are the most critical for a child’s survival.1,2 Globally, 2.4 million children died in the first month of life in 2019. Among the approximated 6700 per day neonatal deaths, about 33% die within the first day of birth, close to 75% die within the first week of life.1,2
Low- and middle-income countries contribute most of the neonatal deaths, about 80% of neonatal deaths occurred in South Asia and sub-Saharan Africa.3 Five sub-Saharan African countries (Ethiopia, Nigeria, DR Congo, Uganda and Tanzania) account for about 50% of neonatal mortality.4 Ethiopia is one of the ten countries that account for nearly 66% of global neonatal deaths, as well as one of the six countries that account for half of all deaths among children under the age of five.5 The neonatal mortality rate was 30 per 1000 live births, according to the Ethiopian Demographic Health Survey (EDHS (2019)). Neonatal deaths account for more than 50% of all deaths among Ethiopian children under the age of five.6
A child in Sub Saharan Africa or in southern Asia is nine times more likely to die in the first month than a child in a high-income country. At the country level, half of all neonatal deaths are concentrated in five countries, namely, India (24%), Pakistan (10%), Nigeria (9%), Democratic republic of Congo (4%) and Ethiopia (3%). Among the sustainable development Goal (SDG) Regions, neonatal mortality was highest in sub-Saharan Africa (38%) and southern Asia (39%), each reported 28 deaths per 1000 live births (WHO UNICEF World Bank group, 2017).
According to estimates by WHO and the Maternal and Child Epidemiology Estimation group in 2017, of all neonatal deaths were attributed to (35%) preterm birth, 24% intra-partum events (such as birth asphyxia), 14% sepsis or meningitis and 11% congenital anomalies.7 Almost half of the under-five deaths can be prevented by reaching high coverage of quality antenatal care, skilled care at birth, postnatal care for mother and baby, and care of small and sick newborns.5
There are profound global initiatives either to end or reduce newborn deaths. The sustainable development goals (SDGs) are one of the continued agenda of the MDGs, the SDG 3 target 3.2 aims at reducing neonatal mortality to 12 per 1000 live births by the year 2030.8 Every Newborn Action Plan (ENAP) has the initiative to end preventable stillbirth and newborn death.9 However, achieving this aim will necessitate increased efforts, especially in the high-burden regions of South Asia and Sub-Saharan Africa, to enable continued improvements in child survival.10
The global neonatal death rate fell by more than half from 36.6 deaths per 1000 live births in 1990 to 17 per 1000 live births in 2019,2 that accounts for 47% all under-five deaths.11 In addition, major progress has been made in reducing infant deaths in Sub-Saharan Africa, which has the world’s highest under-five mortality rate.10
Ethiopia is in a similar situation. It has made significant progress in lowering the mortality rate for children under the age of five. According to the UN Inter-agency Group for Child Mortality Estimation (UN-IGME) report from 2019, Ethiopia was one of eight high-mortality countries where under-five mortality decreased by two-thirds, achieving MDG4 three years ahead of schedule.5
The causes of neonatal mortality are not well known in Ethiopia mainly at institutional level, but there are few studies that come up with causes such as sepsis, asphyxia, preterm birth, congenital malformations.12,13 It is possible to avoid by identifying risk factors, with a special focus on improving newborn child care. Neonatal intensive care units (NICUs) are one of the most powerful tools for reducing newborn mortality in this region.14 The Ethiopian government has used a combination of health, nutrition, and non-health activities to minimize neonatal mortality, but the rate remains high.15
There have been few previous studies in Ethiopia on neonatal survival and/or neonatal death predictors, and most of the studies have focused on preterm babies. Furthermore, in the research field, information on neonatal survival and/or neonatal death predictors is not well studied and reported Boloso Bombe Woreda, Bombe Primary Hospital. Therefore, to gain accelerated reduction in neonatal mortality in Ethiopia, determining the survival of neonates and identifying the predictors of their mortality in the local context is very crucial and currently issued.
Methods
Study Design and Period
An institution-based retrospective cohort study was undertaken to identify the survival and predictors of mortality among Neonates admitted to the NICU at Bombe Primary Hospital from August 15–30, 2020.
Study Area and Population
This study was conducted at the Bombe Primary Hospital, Bombe woreda, Wolaita zone, Southern Ethiopia. In this study, the source population was all neonates at NICU at Bombe Hospital. The study population was all neonates’ admission record at the NICU at Bombe Hospital admitted from January 1, 2018- December 31, 2019. All neonates’ admission records at the NICU at Bombe Hospital during the study period were included in the study; whereas neonates’ admission records with incomplete information, revisits, and any neonates’ records with withdrawal from a treatment or history of self-discharge were excluded from the study.
Sample Size and Sampling Procedure
The sample size was calculated using the double population formula by Epi info considering the following assumptions: Z (1-α⁄2) at 95% CI: 1.96; 80% power; 1:1 ratio of unexposed to exposed; anticipated proportion of mortality rate among neonates who did not initiate early breastfeeding EBF (p1, Exposed) = 30%; neonates who initiated EBF (p2, unexposed) = 16.6%; adjusted hazard ratio (AHR) =1.816 and adding for 10% incompleteness. Hence, the final sample size was obtained to be 374. But, all 380 newborns admitted at the NICU at Bombe primary hospital from January 1, 2018 to December 31, 2019 were included in the study.
Data Collection Procedures
The data were collected on a data collection checklist by reviewing the neonates’ admission records starting from August 15–30, 2020.
Statistical Analysis
After data collection, each questionnaire was checked for completeness and consistency by the principal investigator and supervisor. Data were cleaned, edited, coded and entered into Epi-info version 7 and then exported to STATA version 14 for Windows, then Exploratory data analysis was carried out to check the levels of missing values, presence of influential outliers, multi-colinearity, normality and proportionality of hazards over time.
Cox regression model for its fitness to the data and its adequacy was checked by graphing residual plots like the Cox-Snell residual. Bi-variable analysis was done to identify associations between dependent and independent variables. Crude hazard ratio and adjusted hazard ratio, 95% CI and p-value were used to assess the strength of association and statistical significance.
Kaplan-Meier survival curve together with the log rank test was fitted to test the survival time of the neonates. To classify independent predictors of mortality, variables significant at p or equal to 0.25 levels in the Bivariable analysis, biological plausibility, and previous studies were considered and included in the final Cox-regression analysis. The backward stepwise regression method was applied to get a list of best predictors and any statistical test is considered significant at p-value < 0.05. Covariates were checked for interaction effect. The data were presented with text, tables and figures.
Ethical Approval
Ethical approval was obtained from Haramaya University College of Health and Medical Sciences' Institutional Health Research Ethics Review Committee (IHRERC). Letters of permission and support were provided to the Zonal Health Department and head of the hospital. Prior to starting data collection, the objectives of the study were clearly explained for head of the hospital. Then, informed, voluntary, written and signed consent was also obtained from the head of the hospital in accordance with Declaration of Helsinki. Moreover, the IHRERC of the Haramaya University has not required the patient parental consent to review their medical records since it is retrospective nature of the study. Information obtained from patient medical record was kept confidential and used only for this particular study.
Results
Response Rate and Neonatal Characteristics
Out of 380 reviewed records, 367(96.5%) were included in the data analysis. More than half, 205 (55.8%) of the neonate enrolled in the study were male. The sex ratio was 1 female to 1.3 males. The median age of the neonates was 5 days (Inter Quartile Range (IQR): 1–9 days)). Nearly three-fourth, 264 (71.9%) of the neonates had a normal birth weight (2500–4000g). The median and IQR of birth weight and gestational age were 3300g (IQR=2800g–3600g) and 38 weeks(37weeks–39weeks), respectively. Of the total, 268 (67.6%) neonates had started breastfeeding within 1hour and 42 (11.3%) neonates were large for gestational age. One-thirds of neonates, 113 (30.8%) were hypothermic upon admission, and 71 (19.3%) suffered from birth asphyxia at 5 min. (based on the 5 min. APGAR score) (Table 1).
 |
Table 1 Neonatal Characteristics of Neonates Admitted in NICU at Bombe Primary Hospital, Wolaita Zone, Southern Ethiopia, 2020 |
Maternal and Obstetric Characteristics
The maternal age ranged from 16–43 years with a mean age of 29 ± 6.1 years. Among 367 neonates included in the study, 340 (92.6%) born from mothers who had antenatal care (ANC) follow-up and, of them, 143 (43.2%), had four or above ANC visits. Three hundred seven (83.6%) neonates were delivered from multiparous mothers and 324 (88.3%) neonates were full-term at birth. Three hundred forty-two (93.2%) were singleton. Nearly, nine from ten, 317 (86.4%) of mothers were delivered through spontaneous vaginal delivery. Of them, the maximum duration of labor was 22 hours and the minimum duration was 1 hour with a median of 12 (IQR=9–13). Near to three from ten 103 (28%) had a complication of prolonged labor (Table 2).
 |
Table 2 Maternal and Obstetric Characteristics of Mothers Whose Neonates Were Admitted to the NICU of Bombe Primary Hospital, Southern Ethiopia,2020 |
Causes of Neonatal Admission and Mortality
The leading causes of neonatal admission were neonatal sepsis 179 (48.77%), followed by respiratory distress 68 (18.53%), birth asphyxia 41 (11.17%) and preterm 38 (10.8%). The most common causes of neonatal mortality were complications of preterm 12 (30.7%), followed by birth asphyxia 11 (28.2%) and neonatal infection 7 (17.9%) (Figure 1)
 |
Figure 1 The percentages of causes of neonatal admission and mortality. |
Survival Analysis and Outcome of the Follow-Up
A total of 367 neonates was followed for different periods: a minimum of 1 day and maximum of 19 days with a median follow-up period of 5 days. The total time at risk for 367 neonates was 1867 neonatal days. During follow-up, 39 (10.6% [95% CI: 7.8, 14.2]) neonates had died, 320 (87.2% [95% CI: 83.3, 90.2] had got cured and discharged and 8(2.18) had referred to other hospitals. The overall incidence of neonatal mortality was 20.8 (95% CI: 15.2, 28.5) per 1000 neonatal days. From all deaths, about 25% of the neonates died in the first 24 hours and almost 95% of the neonatal deaths occurred in the first 1 week of life. The cumulative proportion of survival at the end of the first, seventh and 14th days was 97.2%, 83.6% and 67%, respectively, with the difference between categories of variables, whereas the overall mean survival time was 15.60 (95% CI =13.7,17.5) (Figure 2).
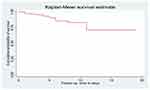 |
Figure 2 Survival analysis and outcome of the follow-up. |
Estimate of Mean Survival Time
The findings of the log rank test revealed that the survival trend or period to neonatal mortality has substantially differed across the categories of neonatal mortality: GA (Log rank test, 43), low 5th minute APGAR (Log rank test,
43), low 5th minute APGAR (Log rank test,  54.76), ANC (Log rank test,
54.76), ANC (Log rank test,  25.62), lower birth weight (Log rank test,
25.62), lower birth weight (Log rank test,  64.24) and Initiation of EBF (Log rank test
64.24) and Initiation of EBF (Log rank test  =27.38) (Figure 3).
=27.38) (Figure 3).
 |
Figure 3 Estimate of mean survival time. |
Predictors of Neonatal Mortality
Bivariate Cox regression analysis showed that; low birth weight, low 5th APGAR score, preterm birth, sex, ANC visit, hypothermia, initiation EBF, time of rupture of membranes and mode of delivery were found to be a significant predictor of death at a p-value < 0.25. However, in the final multivariate Cox-Proportional Hazard model; low birth weight, low 5thAPGAR score, ANC visit, hypothermia, initiation EBF, time of rupture of membranes, and mode of delivery were found to be independent predictors of death (Table 3). The overall Schoenfeld global test of the full model was checked for Proportional Hazard (PH) assumption and it was met (p-value= 0.7806). All covariates are met the proportional-hazard assumption (Table 3).
 |
Table 3 Bivariate Cox-Proportional Hazard Regression for Predictors of Neonatal Mortality Among Neonates Admitted to NICU of Bombe Primary Hospital, South Ethiopia, 2020 |
The risk of death among newborns with a low 5 min. APGAR score was three times higher hazard to die compared with 5 min. APGAR score of greater than five. The hazard of death among neonates born to mothers who had received ANC was 61% lower risk of death compared with those neonates born to mothers who had not received ANC. The risk of death of neonates for whom breastfeeding was not initiated within 1 hr. of birth was three times higher risk of death than neonates who start within hours. Low birth weight neonates had 2.6 times higher hazard of death compared to neonates with normal birth weight. Besides, neonates who had hypothermic at admission had 2.6 times higher risk of death as compared with normo-thermic neonates. Neonates born by cesarean section had 91.6% lower risk of mortality as compared with spontaneous vaginal delivery. Moreover, neonates born from mothers whose rupture of the membrane was ruptured for more than 12 hours of delivery have 2.5 times higher hazard of neonatal mortality than the counterparts whose mother’s membrane ruptured within 12 hours of delivery (Table 4).
 |
Table 4 Multivariate Cox-Proportional Hazard Regression for Predictors of Neonatal Mortality Among Neonates Admitted to NICU of Bombe Primary Hospital, South Ethiopia, 2020 |
Discussion
The most common causes of neonatal mortality were complications of preterm 12 (30.7%), followed by birth asphyxia 11 (28.2%) and neonatal infection 7 (18.9%). During follow-up, 39 (10.6%) neonates had died. The median follow-up period was 5 days. From all deaths, about 25% of the neonates died in the first 24 hrs. The cumulative proportion of survival at the end of the first, seventh and 14th days was 97.2%, 83.61% and 67%, respectively, with the difference between categories of variables. The overall mean survival time was 15.6.
The overall incidence rate of neonatal mortality was 20.8 deaths per 1000 neonates which is lower than the reports of the study conducted by13,17,18 and (Gudayu et al, 2020). However, higher than the results reported by.19–24 This discrepancy might be attributed to differences in study design, period and area, socioeconomic status, sample size and follow-up time. Unlike the current research, several previous studies were community-based where low-risk neonates were also included in the denominator.
In this study, 25% of all neonatal deaths occurred within the first 24 hrs and the first 3 days hold (36%) of all deaths. Almost 95% of the neonatal deaths occurred in the first 1 week of life consistent with studies conducted at Gondar Comprehensive Specialized,25 and in Amhara region referral hospitals.18 Evidences indicate in Ethiopia that more than three-quarter of neonatal mortality occurred in the first six days of life13,20,26,27 which could be related to the conditions of labor, intra-partum and the immediate newborn care practices.
The current study finding revealed that the risk of death among newborns with a low 5th min. APGAR score were three times higher compared with 5th min. APGAR score of greater than five which is consistent with a study conducted at Arba Minch general hospital16 and at Debre Markos Referral Hospital.17 A five-minute Apgar score less than seven was the only predictor of Neonatal Mortality in Cameroon.28 This could be because of neonates who have 5th min APGAR score of less than or equal to 5 were severely asphyxiated and it could be also related to labor and pregnancy complications.
The risk of death was three times higher for neonates who did not start breastfeeding within one hour of birth than for their counterparts. This is consistent with findings from other Ethiopian studies.13,17,19 This may be due to the fact that breastfeeding lowers the risk of neonatal mortality due to infections and hypothermia, especially in preterm and low birth weight babies (ie sepsis, pneumonia, tetanus, and diarrhea).29–31 In fact, neonates who are sick might not be able to suck breast milk as compared to healthier neonates; this might be overestimating the true association.
The hazard of death among neonates born to mothers who had not received ANC was 39% higher compared with those neonates born to mothers who had received ANC. This is similar to previous studies done in Ethiopia21,32 which might be attributed to the benefit of the ANC visit in saving the life of neonates.33,34
The risk of dying for low birth weight neonates had 2.6 times higher compared to neonates with normal birth weight. This finding is agreed with studies done in Ethiopia, Eritrea and Ghana.14,23,24,35,36 The possible reason could be preterm and low birth weight babies are more likely not to suck breast milk in turn being prone to the risk of death.37
Besides, neonates who had hypothermia at admission had 2.6 times higher hazard of death as compared with normal-thermic neonates. Hypothermia increased the hazard of mortality by 50% in another study,13 Despite these results, a study in eastern Ethiopia found that hyperthermia raised the risk of death.21 This may be because sepsis-affected neonates are vulnerable to hypothermia and hyperpyrexia, both of which are signs of impaired metabolism, and the mortality associated with these changes is high.38
Neonates born by cesarean section had 91.6% lower risk of death as compared with spontaneous vaginal delivery. This finding is comparable with studies conducted in WolaitaSodo university teaching referral hospital13 and in Addis Ababa among public hospitals.1 The possible explanation might be timely decision rather than waiting for vaginal delivery, delivering by C/S can reduce the risk of death by decreasing the complications due to prolonged labor.
Other studies have revealed that Caesarian section was not reported to be a significant predictor in reducing neonatal death,14,20,39,40 This may be due to deliance in the decision-making process during prolonged labour, inadequate standard of operation procedure, and women’s aversion to cesarean section. It may also be linked to the outcome of C/S, which could make breastfeeding difficult. Surprisingly, a Nepalese study found that cesarean section delivery raised the risk of neonatal sepsis and mortality.41 This might be babies delivered by caesarean section are at particular risk of developing hypothermia.
Moreover, neonates born from mothers whose rupture of the membrane was ruptured for more than 12 hours of delivery have 2.5 times higher hazard of neonatal mortality than the counterparts whose mother’s membrane ruptured within 12 hours of delivery. This is similar with previous studies conducted in different part of Ethiopia.11,15,21 This may be because as the time between the rupture of the membrane and delivery gets closer, the risk of infection, being in shortness of breathing, pulmonary hyperplasia, and preterm labor rises.42,43
Some limitations of this study have seen since the study is a retrospective cohort study and based on the secondary data, first it did not allow inferences to be drawn with respect to the temporal relationship among variables and association does not imply causation. Secondly, it might be subjected to information bias.
Conclusion
This study founded a high neonatal mortality rate in the NICU at Bombe primary hospital. Low birth weight, lower 5th minute Apgar score, hypothermia, failure to early initiation of breastfeeding and mothers’ time of rupture of membrane >12 hours before delivery were independent predictors of neonatal mortality. Therefore, increased efforts should be undertaken to tackle the problem and enabling environment has to be focused for continued improvements in child survival.
Acknowledgments
The authors would like to acknowledge Haramaya University and Bombe Primary Hospital administration their cooperation and study participants for providing information.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Getiye Y, Fantahun M. Factors associated with perinatal mortality among public health deliveries in Addis Ababa, Ethiopia, an Unmatched Case Control Study. BMC Pregnancy Childbirth. 2017;17(245). doi:10.1186/s12884-017-1420-7
2. UNICEF. Neonatal mortality; 2020. Available from: https://data.unicef.org/topic/child-survival/neonatal-mortality/.
3. Hug L, Sharrow D, You D. Levels and Trends in Child Mortality: Report 2017. The World Bank; 2017.
4. Afolabi BM. Sub-Sahara African neonates–ghosts to statistics. J Neonatal Biol. 2017;6(1):2167–2897. doi:10.4172/2167-0897.1000246
5. IGME U, United Nations Inter-Agency Group for Child Mortality Estimation (UN IGME). Levels & Trends in Child Mortality: Report. Vol. 2019. New York: Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation’,United Nations Children’s Fund; 2019.
6. EPHI, ICF, Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. Rockville, maryland, USA: EPHI and ICF; 2019.
7. World Health Organization. Maternal and child epidemiology estimation group: child causes of death 2000–2017; 2018. Available from: https://www.who.int/healthinfo/global_burden_disease/estimates/en/index2.html.
8. SDGs. United Nation: sustainable development goals. 2015.
9. World Health Organization. WHO every newborn: an action plan to end preventable deaths. 2016.
10. Hug L, Alexander M, You D, Alkema L. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health. 2019;17(6):e710–720. doi:10.1016/S2214-109X(19)30163-9
11. Endale T, Fentahun N, Gemada D, Hussen MA. Maternal and fetal outcomes in term premature rupture of membrane. World J Emerg Med. 2016;7(2):147–152. doi:10.5847/wjem.j.1920-8642.2016.02.011
12. Tewabe T, Mohammed S, Tilahun Y, et al. Clinical outcome and risk factors of neonatal sepsis among neonates in Felege Hiwot referral Hospital, Bahir Dar, Amhara Regional State, North West Ethiopia 2016: a retrospective chart review. BMC Res Notes. 2017;10(1):265. doi:10.1186/s13104-017-2573-1
13. Orsido TT, Asseffa NA, Berheto TM. Predictors of neonatal mortality in neonatal intensive care unit at referral hospital in Southern Ethiopia: a Retrospective Cohort Study. BMC Pregnancy Childbirth. 2019;19(1):83. doi:10.1186/s12884-019-2227-5
14. Andegiorgish MK, Andemariam M, Temesghen S, Ogbai L, Ogbe Z, Zeng L. Neonatal mortality and associated factors in the specialized neonatal care unit Asmara, Eritrea. BMC Public Health. 2020;20(10). doi:10.1186/s12889-019-8118-x
15. UNICEF. WHO The World Bank UNPD. Levels and trends in child mortality. 2013.
16. Dessu S, Gebremeskel F, Alemu G, Seman B. Survival status and predictors of neonatal mortality among neonates who were admitted in neonatal intensive care unit at Arba Minch General Hospital, Southern Ethiopia. Pediatr Ther. 2018;8(3). doi:10.4172/2161-0665.1000352
17. Alebel A, Wagnew F, Petrucka P, et al. Neonatal mortality in the neonatal intensive care unit of Debre Markos referral hospital, Northwest Ethiopia: a Prospective Cohort Study. BMC Pediatr. 2020;20(72). doi:10.1186/s12887-020-1963-z
18. Mengistu BA, Yismaw AE, Azene ZN, Mihret MS. Incidence and predictors of neonatal mortality among neonates admitted in Amhara regional state referral hospitals, Ethiopia: Prospective Follow Up Study. BMC Pediatr. 2020;20(142). doi:10.1186/s12887-020-02031-x
19. Limaso AA, Dangisso MH, Hibstu DT. Neonatal survival and determinants of mortality in Aroresa district, Southern Ethiopia: a Prospective Cohort Study. BMC Pediatr. 2020;20(1):33. doi:10.1186/s12887-019-1907-7
20. Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region, Northern Ethiopia: Prospective Cohort Study. BMC Pregnancy Childbirth. 2016;16(1):202. doi:10.1186/s12884-016-0994-9
21. Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in Jimma Zone, Southwest Ethiopia: a Multilevel Analysis of Prospective Follow Up Study. PLoS One. 2014;9(9):e107184–e107184. doi:10.1371/journal.pone.0107184
22. Desta BN, Assefa N, Damte T, Hordofa LO. Neonatal Mortality and its risk factors in Eastern Ethiopia: a prospective cohort study in Kersa health and demographic surveillance system (Kersa HDSS). Epidemiol Biostat Public Health. 2016;13(4).
23. Tessema ZT, Tesema GA. Incidence of neonatal mortality and its predictors among live births in Ethiopia: gompertz gamma shared frailty model. Ital J Pediatr. 2020;46(1):138. doi:10.1186/s13052-020-00893-6
24. Seid SS, Ibro SA, Ahmed AA, et al. Causes and factors associated with neonatal mortality in Neonatal Intensive Care Unit (NICU) of Jimma University Medical Center, Jimma, South West Ethiopia. Pediatric Health Med Ther. 2019;10:39–48. doi:10.2147/PHMT.S197280
25. Gudayu TW, Zeleke EG, Lakew AM. Time to death and its predictors among neonates admitted in the intensive care unit of the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. Res Rep Neonatology. 2020;10:1–10. doi:10.2147/RRN.S233828
26. Gizaw M, Molla M, Mekonnen W. Trends and risk factors for neonatal mortality in Butajira District, South Central Ethiopia, (1987–2008): a Prospective Cohort Study. BMC Pregnancy Childbirth. 2014;14(1):64. doi:10.1186/1471-2393-14-64
27. Yismaw AE, Gelagay AA, Sisay MM. Survival and predictors among preterm neonates admitted at University of Gondar comprehensive specialized hospital neonatal intensive care unit, Northwest Ethiopia. Ital J Pediatr. 2019;45(4). doi:10.1186/s13052-018-0597-3
28. Ndombo PK, Ekei QM, Tochie JN, et al. A cohort analysis of neonatal hospital mortality rate and predictors of neonatal mortality in a sub-urban hospital of Cameroon. Ital J Pediatr. 2017;43(1):52. doi:10.1186/s13052-017-0369-5
29. Debes AK, Kohli A, Walker N, Edmond K, Mullany LC. Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. BMC Public Health. 2013;13(3):S19. doi:10.1186/1471-2458-13-S3-S19
30. Mersha A, Worku T, Shibiru S, et al. Neonatal sepsis and associated factors among newborns in hospitals of Wolaita Sodo Town, Southern Ethiopia. Res Rep Neonatology. 2019;9:1–8. doi:10.2147/RRN.S193074
31. Khan J, Vesel L, Bahl R, Martines JC. Timing of breastfeeding initiation and exclusivity of breastfeeding during the first month of life: effects on neonatal mortality and morbidity—a systematic review and meta-analysis. Matern Child Health J. 2015;19(3):468–479. doi:10.1007/s10995-014-1526-8
32. Mersha A, Bante A, Shibiru S. Neonatal mortality and its determinates in public hospitals of Gamo and Gofa Zones, Southern Ethiopia: Prospective Follow Up Study. BMC Pediatr. 2019;19(1):499. doi:10.1186/s12887-019-1881-0
33. Al-Ateeq MA, Al-Rusaiess AA. Health education during antenatal care: the need for more. Int J Womens Health. 2015;7:239–242. doi:10.2147/IJWH.S75164
34. Opportunities for Africa’s newborns: Practical data, policy and programatic support for newborn care in Africa. joy Lawn and Kate Kerber, eds.PMNCH, Cape Town, 2006. https://www.who.int/media/oanfullreport.pdf
35. Roro EM, Sisay MM, Sibley LM. Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa Zone, Oromia Region, Ethiopia: Community Based Nested Case Control Study. BMC Public Health. 2018;18(1):888. doi:10.1186/s12889-018-5757-2
36. Owusu BA, Lim A, Makaje N, Wobil P, SameAe A. Neonatal mortality at the neonatal unit: the situation at a teaching hospital in Ghana. Afr Health Sci. 2018;18(2):369–377.
37. Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Neonatal hypothermia and associated risk factors among newborns of southern Nepal. BMC Med. 2010;8(1):43. doi:10.1186/1741-7015-8-43
38. Cavallin F, Calgaro S, Brugnolaro V, et al. Impact of temperature change from admission to day one on neonatal mortality in a low-resource setting. BMC Pregnancy Childbirth. 2020;20(1):646. doi:10.1186/s12884-020-03343-7
39. Roro EM, Tumtu MI, Gebre DS. Predictors, causes, and trends of neonatal mortality at Nekemte Referral Hospital, East Wollega Zone, Western Ethiopia (2010–2014). Retrospective Cohort Study. PLoS One. 2019;14(10):e0221513. doi:10.1371/journal.pone.0221513
40. Kebede B, Gebeyehu A, Sharma HR, Yifru S. Prevalence and associated factors of neonatal mortality in North Gondar Zone, Northwest Ethiopia. Ethiop J Health Dev. 2012;26(2):66–71.
41. Thapa B, Thapa A, Aryal DR, et al. Neonatal sepsis as a major cause of morbidity in a tertiary center in Kathmandu. J Nepal Med Assoc. 2013;52(192):549–556. doi:10.31729/jnma.2424
42. Mohan SS, Thippeveeranna C, Singh NN, Singh LR. Analysis of risk factors, maternal and fetal outcome of spontaneous preterm premature rupture of membranes: a Cross Sectional Study. Int J Reprod Contracept Obstet Gynecol. 2017;6(9):3781–3787. doi:10.18203/2320-1770.ijrcog20173623
43. Amulya MN, Ashwini MS. Maternal outcome in term premature rupture of membranes. Int J Reprod Contracept Obstet Gynecol. 2018;8(2):576–579.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
