Back to Journals » Research and Reports in Urology » Volume 12
Surgical Management of Urolithiasis of the Upper Tract – Current Trend of Endourology in Africa
Authors Cassell A III , Jalloh M , Ndoye M , Mbodji M, Gaye O , Thiam NM, Diallo A, Labou I, Niang L, Gueye S
Received 10 April 2020
Accepted for publication 19 June 2020
Published 6 July 2020 Volume 2020:12 Pages 225—238
DOI https://doi.org/10.2147/RRU.S257669
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jan Colli
Ayun Cassell III,1,2 Mohamed Jalloh,1 Medina Ndoye,1 Mouhamadou Mbodji,1 Oumar Gaye,1 Ngor Mack Thiam,1 Abdourahmane Diallo,1 Issa Labou,1 Lamine Niang,1 Serigne Gueye1
1Department of Urology and Andrology, Hospital General De Grand Yoff, Dakar, Senegal; 2Department of Surgery, Liberia College of Physicians and Surgeons, Monrovia, Liberia
Correspondence: Ayun Cassell III
Department of Urology and Andrology, Hospital General De Grand Yoff, Dakar, Senegal
Tel +221770135805
Email [email protected]
Abstract: Urolithiasis is a global pathology with increasing prevalence rate. The lifetime recurrence of urolithiasis ranges from 10– 75% creating a public health crisis in affected regions. The epidemiology of urolithiasis in most parts of Africa and Asia remains poorly documented as incidence and prevalence rates in these settings are extrapolated from hospital admissions. The surgical management of kidney and ureteral stones is based on the stone location, size, the patient’s preference and the institutional capacity. To date, the available modalities in the management of urolithiasis includes external shock wave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL), ureterorenoscopy (URS) including flexible and semirigid ureteroscopy. However, regarding the lack of endourological equipment and expertise in most parts of Sub-Saharan Africa (SSA), most urological centers in these regions still consider open surgery for kidney and ureteral stones. This review explores the current trend and surgical management of upper tract urolithiasis in SSA with insight on the available clinical guidelines.
Keywords: endourology, kidney stones, ureteral stones, urolithiasis
Background
Nephrolithiasis is a very common pathology globally with prevalence rates ranging from 7–13% in North America, 5–9% in Europe, and 1–5% in Asia.1 In the United States alone, kidney stones have been reported to affect 8.8% of the population.2 A contemporary review by Romero et al revealed that stone prevalence has been increasing by age in Iceland, Iran, Germany, Turkey, Greece and the United States3 with a peak incidence in the third or fourth decade of life in most countries.3,4 The stone burden seems to be slightly higher in males than females at a ratio of 2:1.4
The epidemiology of urolithiasis in most parts of Africa and Asia remains poorly documented as incidence and prevalence rates in these settings are extrapolated from hospital admissions.4 Countries along the Afro–Asia belt including North Africa, Middle East, and South East Asia have shown a higher incidence of urolithiasis due to the rising temperatures of global warming. In these regions, urolithiasis constitute about 40–50% of urological cases managed.4 The growing trend of urolithiasis in these regions have also alluded to the progressive change in dietary habits and sedentary lifestyle being adopted in parts of Africa and Asia.5 The exact incidence of urolithiasis in Sub-Saharan Africa is unknown. The underreporting and lack of large epidemiological studies on urinary stones disease have challenged the profiling of this subject. Recent studies have shown the rise in the incidence of kidney stones over the past 30 years in developing nations.5
The lifetime recurrence of urolithiasis ranges from 10–75% creating a public health crisis in affected regions.6 Kidney stones are a common cause of chronic kidney disease leading to end stage renal failure in about 2–3% of the population. In India, approximately 12% of the population is affected by urolithiasis of the upper urinary tract and 50% may be complicated by loss of renal function.5 Kidney stones have also been closely related to cardiovascular diseases and metabolic syndrome.7
The surgical management of kidney and ureteral stones is based on the stone location, size, the patient’s preference and the institutional capacity.8 Over past decades, there has been a paradigm shift from open surgery to endourology in the management of upper tract urolithiasis. To date, the available modalities in the management of urolithiasis include external shock wave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL), ureterorenoscopy (URS) including flexible and semirigid ureteroscopy. These procedures single or combined are recommended by most guidelines including the American Urological Association (AUA), European Association of Urology (EAU) and the Urological Association of Asia clinical guideline for upper tract urinary stone disease.9,10 However, regarding the lack of endourological equipment and expertise in most parts of Sub-Saharan Africa (SSA), most urological centers in these regions still consider open surgery for kidney and ureteral stones.
This review explores the current trend and surgical management of upper tract urolithiasis in SSA with insight on the available clinical guidelines. The review intends to identify and highlight the gaps in endourology for urinary stone disease in SSA and provide relevant recommendations to improve the standard of care.
Methodology
A review of published literature was conducted from 1990 to 2020 using medical search engines and academic databases PubMed, Google Scholar and African Journals Online. The English and French publications were searched using the medical search heading (MeSH) appended with keywords (Management of Upper Urinary Tract stone/Urolithiasis of the upper Tract). These keywords were indexed with the following: Africa, Sub-Saharan Africa, Senegal, Niger, Burkina, Chad, Nigeria, Congo, Kenya, Ghana, Mali, Mauritania. From the results of these search terms, publications that included urolithiasis of upper tract were included in the review. Text exclusively on the management of lower tract stones were excluded from the study. Sub-Saharan publications on upper tract urolithiasis involving less than 50 subjects were not included the tables for analysis but rather in the main text of the discussion.
Fifteen published online data from SSA were extracted for cross tabulation. These papers were analyzed quantitatively and qualitatively for demographics, age parameters, composition of stones, location of stones, laterality and clinical presentation, risk factors, presence of infection, imaging, management and outcome of upper tract urolithiasis. Stones reported along the renal calyces or pelvis were all categorized as renal stones. All stones along the ureters to ureterovesical junction were grouped as ureteric stones for the reviewed data.
The result from the data synthesis was reflected in the body of the results and main text.
The discussion was constructed using summaries of the American Urological Association (AUA), European Association of Urology (EAU) and the Urological Association of Asia clinical guidelines for urinary stone disease. The current standard of care in these guidelines was compared to the surgical management of upper tract urolithiasis in the Sub-Saharan region identifying gaps and need for further improvement.
Results
After vetting the online publications, only 53 research articles were included for the review which contained, guidelines, randomized trials, meta-analyses, review articles, prospective and retrospective designs. The 15 extracted texts were publications from Senegal, Congo Brazzaville, Nigeria, Burkina Faso, Kenya, Central African Republic (CAR), Mali, Benin, and Chad.11,25 A quantitative analysis of the review reported 1480 patients managed for urolithiasis, mean age of 39.1 years with age ranging from 0.2– 88 years (Table 1). Calcium oxalate was the most common stone composition as reported from Congo Brazzaville, Nigeria, Burkina Faso, and Kenya.16,18,20 The distribution of urolithiasis along the upper tract was 48.3% renal stones and 34.1% ureteric stones. About 42.9% of the stones were located along the right upper urinary tract, 34.1% on the left and an average of 4.2% bilaterally. Typical clinical presentations of urolithiasis reported by most authors from the SSA region were renal colic, low back pain, hematuria, dysuria, fever, urinary retention (especially studies with both upper and lower tract urolithiasis) as well as complications of hydronephrosis and pyelonephritis. Data from Burkina Faso, Mali, and Chad reported the stenotic complication of urinary schistosomiasis as a common etiological association of urolithiasis ranging from 4.7– 61.1% of patients.17,22,24,25 Other associated risk factors reported for urolithiasis included urethral stricture, family history of stone disease, urinary tract infection (UTI), pelvic ureteral junction (PUJ) obstruction, dairy product, metabolic syndrome and sickle cell disease (Table 2). A pooled analysis of six reports from the SSA showed that Escherichia coli was a common isolate in patients with urolithiasis and UTI ranging from 2.7– 37.5%. Other isolates from urine culture included Staphylococcus, Klebsiella, Proteus and Acinetobacter species.
 |
Table 1 Demographics, Biodata and Stone Composition Amongst Patients from Sub-Saharan Africa |
 |
Table 2 Clinical Presentation of Urolithiasis Amongst Sub-Saharan Africa |
Eight out 15 publications from (Senegal, Nigeria, Benin, Kenya, and Chad) reported the use of computed tomography scan (CT-scan) as part of the diagnostic imaging modality for urolithiasis. The use of transabdominal ultrasound, intravenous urography and plain abdominal film were the principle diagnostic imaging modalities in other regions of SSA where CT-scan was not available. The sizes of stones managed in the series ranged from 5–95 mm.16,23,47,49 The rate of open surgery for upper tract urolithiasis was about 69.5% in the review with nephrolithotomy 20.8%, pyelolithotomy 37.9%, ureterolithotomy 29.9% and nephrectomy 7.9%. Authors from Senegal (Diallo et al; /Kane et al)11,12 and Kenya (Ngugi et al; Wathigo et al)19,20 reported a considerable use of endoscopic surgery for upper tract urolithiasis. These endoscopic procedures included the use of PCNL, flexible ureteroscopy + laser fragmentation, semi-rigid ureteroscopy + lithotripsy as well as the use of ESWL alone or in conjunction with endoscopy.
The rate of surgical site infection following open surgery for urolithiasis in the region ranged from 0.8–15%. Other complications following the open surgical management of upper tract urolithiasis included pyonephrosis, urinary fistulas, urinoma, urinary peritonitis and even a mortality of 1.4% and 4.4% according to Hounnasso et al23 and Odzebe et al13,14 respectively (Table 3).
 |
Table 3 Treatment and Complication of Urolithiasis in Sub-Saharan Africa |
Discussion
Classification of Stones
Urolithiasis can be classified based on the location, radiological characteristics, size, etiology of formation, composition, and risk of recurrence. According to the EAU Guidelines on Urinary Stones of the upper tract, the sizes of stone can be stratified as either ≤5 mm, 5–10 mm, 10 mm–20 mm or >20 mm.9 These stones can be found anywhere along the urinary tract including the calyxes (upper, middle, lower), renal pelvis, ureter (proximal, middle, distal) and the urinary bladder. The composition and density of urinary stones can be assessed by noncontrast-enhanced CT-scan which is crucial for the treatment plan.
Approximately 80% of urinary stones are calcium stones making it the most predominant.5 Most of these calcium stones occur as calcium oxalate which is present in the majority of renal stones. Calcium oxalate can exist as monohydrate (whewellite, CaC2O4·H2O), and dihydrate (weddellite, CaC2O4·2H2O).26 It may occur as a combination of both whewellite and weddellite in more than 60% of the population affected. Calcium stones have a higher rate of recurrence than other stone composition.
Struvite stones (magnesium ammonium phosphate) account for 10–15% of urinary stones occurring mostly in patients with chronic urinary tract infection in the presence of urea splitting pathogens like Proteus mirabilis, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Enterobacter.27 The precipitation of phosphate precipitates on to the insoluble ammonium products can cause large staghorn calculi formation.5,27 These stones are more frequent in females.
Most uric acid stones are idiopathic and constitute 3−0% of urolithiasis.5 They are found in patients with gouty arthritis or high consumers of animal protein. Cysteine stones are closely associated with metabolic or genetic disorders and comprising 2% of stone disease.26,27 Drug induced stones account for only 1% of urolithiasis. Some lithogenic drugs include protease inhibitor indinavir sulphate, guaifenesin, triamterene, atazanavir and sulfa drugs.26,27
The epidemiology of urinary stone composition in SA is yet to be fully explored. A quantitative analysis of four publications in the region displayed that calcium oxalate was the commonest stone composition. An analysis of urinary stone amongst a multiethnic population in Kenya by Wathigo et al showed that calcium and oxalate accounted for 72% of the stone’s composition when analyzed.20 A five-year epidemiological study of urolithiasis involving 828 patients in Morocco found that calcium oxalate was the commonest stone composition at 66.6% after stone analysis with infrared spectroscopy.28 Stone disease in Africa was initially thought to be rare and usually due to infection. Recent studies are suggesting that obesity, change in diet, dairy products and the hot weather are now contributing factors of urolithiasis in some parts of SSA.11,23,24
Diagnosis and Imaging
The diagnosis of urinary stones starts with a thorough medical history and appropriate imaging as physical exams are helpful in mostly complicated urolithiasis. Patients with renal or ureteral stones may be asymptomatic or present with flank pain, vomiting and sometimes fever reflecting UTI. Patient with acute flank pain, solitary kidney or fever will require immediate imaging. It is also essential to rule out a foreign body when assessing the upper tract because they have the potential to calcify. Previous history of open, laparoscopic or robotic surgery should be ascertained if suspicion of foreign body is held.29
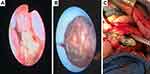
Ultrasound is usually the initial imaging of choice because it is cheap, safe and without radiation. It can identify stones along the renal collecting system as well as documenting hydronephrosis. However, ultrasound has a specificity of 88% and sensitivity of 45% for renal stones and a specificity of 94% and sensitivity of 45% for ureteric stones.9,30 However, ultrasound has a specificity of 88% and sensitivity of 45% for renal stones and a specificity of 94% and sensitivity of 45% for ureteric stones.9,30 The EAU guidelines suggest that kidney-ureter-bladder (KUB) radiography should not be performed if noncontrast CT-scan is being considered. Noncontrast-enhanced CT-scan (NCCT) is currently the gold standard for the diagnosis of urolithiasis presenting with acute renal or ureteral colic (Figure 1A–C). Over the years, NCCT has replaced intravenous urography (IVU) because it can estimate the diameter and density of stones which are essential for treatment options. A meta-analysis of several prospective studies31 has shown that low-dose CT diagnosed urolithiasis with a pooled sensitivity of 93.1% and a specificity of 96.6%.
The AUA guideline on stones recommended CT imaging over ultrasound when planning ESWL or URS. Stone density less than 1000 Hounsfield units are better candidates for ESWL. Patients with chronic kidney disease, complex stones/staghorn calculi with altered renal function should receive a nuclear renal scan to assess for renal function. Further imaging using CT-urography and MRI-urography are essential to diagnose complex urinary tract anatomy like ectopic kidney, duplicated collecting system, diverticulum, ureteral strictures, ureteroceles or megaureters.2
Diagnosis in children and pregnancy requires special attention to radiation dose and teratogenicity. Ultrasound is usually a safe alternative during pregnancy due to the absence of radiation. MRI can be considered second line during pregnancy to identify obstruction and outline stones as filling defects. New protocols using a low-dose CT-scan can reduce the radiation and should be offered as a last option for imaging in pregnant women.32 Ultrasound is the preferred modality in children due to its safety profile but can miss stones in about 40% of children.9 Recent low-dose CT-scan protocols are being adopted for children, but stones can escape detection in about 5% of children.33
Patients with urolithiasis awaiting intervention should receive a biochemical workup including electrolytes, creatinine, and urinalysis. A complete blood count (CBC) can assess for leukocytosis, anemia and thrombocytopenia. Preprocedural international normalized ratio (INR) is recommended in patients at risk of hemorrhage. Positive urine culture should be treated before intervention. Urine samples can also be collected intraoperatively for culture and sensitivity when urinary tract infection is suspected.2
With the increase in the incidence of urolithiasis in SSA, the diagnostic armamentarium of urinary stone is rapidly evolving. Major urological centers in Senegal, Benin, Nigeria, Kenya, and Chad have reported the use of CT-scan as a usual imaging modality for the diagnosis of kidney and ureteral stones. Most urological units in Africa still use ultrasound, KUB or IVU for the management of urinary stones. Ultrasound is cheaper and relatively available in many treatment centers, but the lower sensitivity remains a challenge for both kidney and ureteral stones especially. KUB radiography is present in hospitals in SSA but very limited as a diagnostic choice for uric acid or cysteine stones. The diagnostic algorithm for urolithiasis in pediatric and pregnant patients in SSA is not well published. Hospital based studies have estimated the rate of pediatric urolithiasis to range from 0.6–1.36% of hospital admissions with an incidence of 7.1 cases per year.34,35 Few retrospective reviews by Ouédraogo et al and Odzebe et al solely on the management of pediatric urolithiasis have reported the use of KUB radiography, IVU and ultrasound as the main diagnostic imaging for urinary stones in children.34,35 The use of CT-scan has been mentioned but with less detail on the protocol to reduce radiation.
Treatment
General Management Principle of Urolithiasis
The management of upper tract urinary stones depends on the size, location, and composition of the stone. However, most patients may present for the first time needing emergency attention.
The EAU guidelines suggest that patients presenting with acute renal colic should be offered relief by nonsteroidal anti-inflammatory (NSAID) drugs because of the better analgesic profile compared to opioids.9 The AUA guidelines also recommend observation or medical expulsive therapy for ureteral stones less than 10 mm using an alpha blocker (tamsulosin) to achieve spontaneous passage with greatest benefits seen along the distal ureters. Studies have shown that stones that do not pass within six weeks are most likely to require intervention.2
Oral chemolitholysis using potassium citrate to alkalinize the urine to treat uric acid stones has also been advocated.
Emergency presentation with obstructive stones and suspicion of urinary tract infection requires drainage with a ureteral stent or a nephrostomy tube. A urine sample for culture and sensitivity should be sent and an appropriate course of antibiotic treatment can be completed before plans for definitive stone therapy. If purulent urine is encountered during an endoscopic procedure (PCNL, URS), the procedure should be aborted, appropriate drainage should be performed, and urine is sampled for culture/sensitivity with appropriate antibiotic started.2
Bleeding diathesis should be corrected in patients receiving thromboprophylaxy before proceeding to surgery for urinary stones. These patients are at significant risk of hemorrhage or perinephric hematoma following ESWL, PCNL, percutaneous nephrostomy or surgery. In cases where anticoagulation is inevitable or bleeding diathesis not corrected, URS is preferred over ESWL and PCNL due to lesser risk of hemorrhage.2,9,10
Surgical Management of Renal Stones in the Renal Pelvis, Upper and Middle Calyx
There are various treatment options for stones along the renal pelvis, upper and middle calyx. Patients who failed observation, medical expulsive therapy or with stones less than 20 mm can benefit from ESWL. However, ESWL may require several courses to achieve acceptable stone-free rates therefore endourological procedures are warranted. Retrograde renal surgery (RIR), ureterorenoscopy has been shown to provide better stone-free rates for stones less than 20 mm and may require fewer or a single procedure for stone clearance unlike ESWL.2,9,10 For stones greater than 20 mm, PCNL is the first-line treatment option if there is no contraindication. The success rate of PCNL is less affected by stone density or composition compared to URS or ESWL. Ureterorenoscopy is another option but has a lesser stone-free rate than PCNL (Figure 2A).
Most complex renal stones including partial and complete staghorn calculi can be treated by PCNL. PCNL is the preferred modality due to its lower intraoperative and postoperative morbidity (smaller incision, shorter hospital stays) compared to open surgery.2,9 Evidence has shown favorable results with combined PCNL and retrograde renal surgery providing acceptable stone-free rates.36 However, if failure rates and the need for multiple procedures precludes the success of minimally invasive procedures (PCNL, URS, ESWL) to achieve optimal stone-free rates then, open, laparoscopic or robotic-assisted surgery is a viable option. Documented indications of open, laparoscopic, or robotic-assisted surgery include cases of anatomic abnormalities, with large or complex stones, or those requiring concomitant reconstruction. Patients with urolithiasis and ipsilateral negligible renal function confirmed by renal scan as well as laboratory testing should undergo ipsilateral nephrectomy to prevent persistent infection, pain and pyelonephritis.2,9,10 However, the function of the contralateral kidney should be assessed before proceeding to a nephrectomy.
Surgical Management for Renal Stone in the Lower Renal Calyx
Although ESWL is a noninvasive treatment choice for renal stones, it is not recommended as the first treatment choice for lower calyx stones less than 20 mm. Even when these stones are fragmented, the fragments may often remain in the lower calyx and re-calcify.9 The stone-free rate of ESWL ranges from 25–95% for lower calyx renal stone. For lower renal calyx stone, studies have shown that the median success rate for ESWL was 58% compared to the median success rate of 81% for URS and 87% for PCNL.2 Other barriers to successful stone clearance with ESWL include steep infundibular-pelvic angle, long calyx, long skin-to-stone distance, narrow infundibulum37 as well as stone density greater than 900 to 1000 Hounsfield units. Therefore, PCNL or ureterorenoscopy remains the best option for lower calyx stone despite the size (Figure 2B). Patients should be informed that although PCNL provides better stone free rates, it presents with a higher morbidity. With the advent of miniPCNL or microPCNL, some of these complications as well as a need for routine nephrostomy tube placement has been reduced.38
Surgical Management of Ureteral Stones
For proximal ureteral calculi <10 mm, ESWL is the first-line treatment option according to the EAU guidelines. ESWL is associated with the least morbidity compared to other treatment options. However, in obese patients and calculi >10 mm in the proximal ureter, URS is a better option with better stone-free rates thus requiring fewer sessions for stone removal.9,10 Studies have shown that stones ≤10 mm in size stratified by stone location, the median stone-free rates are superior for URS over SWL at all locations in the ureter (85% vs 66.5% for proximal ureteral stones respectively; 91% vs 75%, for middle ureteral stones respectively; and 94% vs 74%, for distal ureteral stones respectively).2
Both ESWL and URS are options for distal ureteral stones. ESWL is noninvasive without anesthesia but the retreatment rate is high. Ureteroscopy has a higher stone-free rate but requires anesthesia with a higher rate of ureteral trauma and sepsis. Women of child-bearing age with middle and distal ureteral stone will require URS because the effect of shock waves on the ovaries has not been full evaluated (Figure 3).2
 |
Figure 3 Flowchart reveals the EAU guideline summary of the management of proximal and distal ureteral stones. |
Uric acid stones are radiolucent and cysteine stones are faintly radiopaque making fluoroscopic guided shock wave lithotripsy difficult.2 Therefore, URS with intracorporeal lithotripsy is the best management of uric acid and cysteine stones as well as any ureteric stone regardless of composition.39
Routine ureteral stenting is discouraged in individuals undergoing ESWL as there is insufficient evidence to prove its benefit. Following URS, patients without renal impairment, abnormal contralateral kidney, ureteric injury, ureteric stricture or anatomical anomaly should not receive routine ureteral stenting.40 To reduce stent-related morbidity, the AUA guidelines recommend three to seven days of stenting following an uncomplicated ureteroscopic stone intervention. The use of antimuscarinic agents and alpha blockers have shown to reduce stent related discomfort in many clinical trials.2
Patients presenting with complex ureteral stones where URS or ESWL cannot achieve stone-free rates within a reasonable amount of procedures alternative procedures should be considered. Percutaneous antegrade URS has shown to provide optimal stone clearance for proximal impacted ureteric stone.2,9,10 When ureterolithotomy is being considered, laparoscopic and robotic-assisted ureterolitholithomy have equal efficacy to open surgery with lesser morbidity.
Semirigid ureteroscopy with pneumatic or ultrasonic lithotripter can be ideal for middle and distal ureteral stones; but ureteral access becomes more difficult above the iliac vessels due to torque of the ureters putting the instruments at risk of damage. This difficulty can be overcome by using flexible ureteroscopes which are ideal for proximal ureteral stones.41 Working channels for flexible ureteroscopes are best adapted with holmium laser or thulium laser fiber and have proven to provide better success rate for stones <20 mm.
Stone Management in the Pediatric Population
Uncomplicated ureteral stones ≤10 mm in the pediatric population can undergo observation with or without MET using alpha blockers. Results from controlled trials have shown some benefit of MET with alpha blockers over observation alone.42 Parents should be reminded that stone sizes closer to 10 mm are least likely to achieve spontaneous passage. Patients that fail observation or MET should be offered SWL or URS to alleviate symptoms, avoid infection or preserve renal function.2,9 Results from a meta-analysis showed that stone-free rates in pediatric patients with ureteral calculi <10 mm are high for both ESWL (87%) and URS (95%) but lower for larger ureteral calculi greater than 10 mm.2
Pediatric patients with renal stone burden <20 mm can benefit from ESWL as a first option as studies have demonstrated stone-free rates as high as 85% with minimum complication.43 Even though URS has displayed similar stone-free rates, it is associated with complication rates ranging from 12.4–20.5%.44
Renal stones >20 mm occurring in the pediatric population should be treated with PCNL or ESWL with success rate at 90% and 83% respectively.2 Pediatric patients undergoing ESWL for renal stones >20 mm should receive concomitant ureteral stenting or nephrostomy tube to avoid postoperative renal obstruction. The complications following PCNL in children have also been minimized with the introduction of miniPCNL or microPCNL.45
Open or laparoscopic surgery for upper tract urolithiasis should not be routinely performed in the pediatric population except when there is a need for correction of a coexisting anatomic anomaly like pelvic uretero junction obstruction (PUJO).2
Stone Management in Pregnant Patients
The management of upper tract stones in pregnant patients is complicated. Every pharmacological or surgical intervention should be coordinated both by the urologist and the obstetrician. The primary concern is to avoid the teratogenic effect of radiation to the fetus or the distorted anatomy in pregnant patient complicating proper diagnosis. Pregnant patients with ureteral stones presenting with controlled symptoms should undergo observation as the first line of treatment even though the spontaneous passage rate of stones has not been documented.2,9 There is also the lack of evidence to support the use of MET for stones in pregnant patients. Pregnant patients with ureteral stones that fail observation can benefit URS as it offers definitive clearance of stone. URS should be considered only if the entity has facility for maternal and fetal support. If URS is not feasible, ureteral stent or percutaneous nephrostomy to decompress the collecting system can provide temporary relief.2,9,10 Definitive treatment should proceed following delivery as indicated.
Treatment of Urolithiasis in Sub-Saharan Africa
In many of the high-income and middle-income countries, endourology have revolutionized the treatment of urinary stones. However, many of low-income countries are still reliant on open stone surgery. A pooled analysis from the review of 15 publications from SSA revealed the rate of open surgery for upper tract urolithiasis to be 69.5% with nephrolithotomy 20.8%, pyelolithotomy 37.9%, ureterolithotomy 29.9% and nephrectomy 7.9%. The size of stone ranged from the high usage of open surgery for urinary stones can be alluded to the lack of endourology equipment or expertise; the absence or limited amount of urologist; and the poor maintenance or replacement of equipment if broken. Omisanjo et al, a retrospective study of 76 patients with urolithiasis reported that almost all the patients with upper tract stones were treated with open surgery except for one intracorporeal lithotripsy which was a demonstration.15
In low-income countries where the minimum wage is inadequate, most individuals may not afford the cost of stone treatment resulting obstructive renal failure. The rate of nephrectomy in the review ranged from 1.9–17.9% signifying a disease burden that needs urgent public health attention. A retrospective study of 450 patients with urolithiasis in Burkina Faso showed that 8.9% of patients presented with obstructive renal failure.46 A study by Kane et al reported the cost of a single endourological intervention for urinary stones in Senegal was almost US$1000 while open surgery was three times cheaper.12
Despite these pitfalls, some institutions in SSA have maintained a novel approach to urinary stone management. A recent study by Yaméogo et al in Ouagadougou Burkina Faso published the use of ureteroscopy and holmium laser lithotripsy for upper tract urinary stones.47 A similar report from Kenya reviewing 67 patients with upper tract urolithiasis showed that 77.6% of cases were managed with laser lithotripsy.20 Another retrospective study by Adusei et al in Ghana, evaluating 42 patients who underwent intracorporeal lithotripsy, revealed that the commonest procedure was ureteroscopy. Ureteral mucosal injury was the commonest complication in the review. This denotes that some level of endourology is being practiced in SSA.48
Endourology has been a milestone for urological practice in Senegal for over a decade now. Many tertiary hospitals have adopted standard urological practice for stone management including the use of ESWL, PCNL, ureteroscopy and holmium laser lithotripsy or pneumatic lithotripsy for upper tract stones. A study by Ondo et al in Senegal reported the use of ESWL for patients with upper tract stones using the Allengers Urolith Extracorporeal Lithotriptor.49 The Former General Hospital of Grand Yoff (now Hopital General Idrissa Pouye) in Dakar has been the reference center of endourology in West Africa, training many urologists around Africa (Figure 4A–C). In 2017, the IVU-med an international charitable urological organization introduced the use of laparoscopic urology in Senegal. This included a group of laparoscopic urological surgeons from the UK who came to train local urologists at the Hopital General Idrissa Pouye in Dakar, Senegal to perform basic laparoscopic urological procedures, including laparoscopic varicocelectomy and renal cyst decortication. The goal was to stimulate the use of laparoscope regarding the benefits of reduced intraoperative blood loss; early mobilization; decreased risk of ileus and wound complications; less requirement for analgesia; reduced length of hospital stay; and faster convalescence and return to work.50 This laparoscopic training has now been instituted in Senegal and is currently ongoing. In 2009, UROLINK, a subcommittee of the British Association of Urological Surgeons established an endourological training center at the Hawassa Referral Hospital in Ethiopia. The local urological team was trained to use both flexible and rigid endoscopic equipment.51
Challenges to Endourology in Africa
The training and practice of urology in SSA have been challenged for decades with poverty, political instability and lack of basic infrastructures.52 The majority of people in the region live below the poverty line. Most of the hospitals are underfunded and the few available are found in urban settings. Endoscopic materials are very costly and will require adequate funding to be maintained in the region. Most patients cannot afford to be investigated for urolithiasis using CT-scan or endoscopic tools. Ultrasound and radiograph may be available in some African regions but comes with limitations for the management of urolithiasis. Some urological training programs in SSA have minimum endoscopic training capacities52 and trainees have to seek additional training in Europe, Asia, or America for proficiency.
Recommendations
To date, there is no African guideline for the management of urolithiasis. A systematic review by Zumstein et al of 61 member states of the Societé Internationale d’Urologie (SIU) found no guidelines for urolithiasis amongst Sub-Saharan states.8
All African national urological associations including the Pan African Urological Surgeon Association (PAUSA) should formulate a guideline that is evidence-based but adaptable to SSA. The demographics, socioeconomic status and cost of treatment should be considered during this process.
National governments in Africa, urological institutions along with other health partners should direct funding to the creation of a center excellence for endourology and the management of urolithiasis in SSA.
There is some evidence to suggest the use of endoscopy for urolithiasis in some parts of SSA but documentation and reporting of published data on those activities are lacking. Therefore, the current trend of endourological management is difficult to follow. It is incumbent upon every urologist and training institution in the region to carefully document and publish their experiences with the management of urinary stones. This can help to identify gaps and create plans for improvement in the field of stone management.
Preventive Measure
All patients with urinary stone disease require a strict adherence to a preventive guideline to avoid urinary stone recurrence. Studies have shown that the adequate fluid intake (>2.5 L daily) and the reduction of carbonated drinks reduced stone recurrence.53 The intake of fruit, vegetables and fiber should be encouraged. Vegetables tend to increase urine PH thus preventing the formation of urinary stones. Excess animal protein and precursors of oxalates should be avoided due to their lithogenicity. Sodium intake should be reduced to 3–5 g daily.9 High sodium intake leads to sodium urate crystal formation. Calcium intake should not be restricted normally due to its inverse relation to stone formation. However older patients requiring calcium supplements will be advised for adequate fluid intake. Weight reduction and control of arterial hypertension are essential for prevention of stone recurrence.
Conclusion
The management of upper tract stones has gained novelty globally by the introduction of endourology. The international guidelines on the management of stones have been widely adopted in most high-income and middle-income countries with endourology being the gold standard for urinary stone treatment. In low resource settings, open surgery is still the major treatment option for upper tract urinary stones. The limited number of specialists and lack of minimally invasive equipment have increased the amount of obstructive renal failure. Nevertheless, other urological institutions in the region have maintained an acceptable standard of stone management. Urolithiasis should be regarded an emerging public health concern to attract resources to improve the current standard of care.
Acknowledgment
Special thanks to the Department of Urology and Andrology.
Author Contributions
All authors have made considerable contributions to conception and design, acquisition of data, analysis and interpretation of data; engaged in drafting the article or revising it critically for essential intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest regarding this article.
References
1. Sorokin I, Mamoulakis C, Miyazawa K, Rodgers A, Talati J, Lotan Y. Epidemiology of stone disease across the world. World J Urol. 2017;35(9):1301–1320. doi:10.1007/s00345-017-2008-6
2. Assimos D, Krambeck A, Miller NL, et al. Surgical management of stones: american urological association/endourological society guideline, PART I. J Urol. 2016;196(4):1153–1160. doi:10.1016/j.juro.2016.05.090
3. Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol. 2010;12(2–3):86–96.
4. Rizvi SA, Naqvi SA, Hussain Z, et al. The management of stone disease. BJU Int. 2002;89:62–68. doi:10.1046/j.1465-5101.2001.134.x
5. Alelign T, Petros B. Kidney stone disease: an update on current concepts. Adv Urol. 2018;2018:1–12. doi:10.1155/2018/3068365
6. Moe OW. Kidney stones: pathophysiology and medical management. lancet. 2006;367(9507):333–344. doi:10.1016/S0140-6736(06)68071-9
7. Rule AD, Roger VL, Melton LJ, et al. Kidney stones associate with increased risk for myocardial infarction. J Am Soc Nephrol. 2010;21(10):1641–1644. doi:10.1681/ASN.2010030253
8. Zumstein V, Betschart P, Abt D, Schmid HP, Panje CM, Putora PM. Surgical management of urolithiasis–a systematic analysis of available guidelines. BMC Urol. 2018;18(25):1–8. doi:10.1186/s12894-018-0332-9
9. Turk C, Skolarikos A, Neisius A, Petrik A EAU guidelines on urolithiasis 2019. Available from: https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Urolithiasis-2019.pdf.
10. Taguchi K, Cho SY, Ng AC, et al. The Urological Association of Asia clinical guideline for urinary stone disease. Int J Urol. 2019;26(7):688–709.
11. Diallo Y, Kouka SC, Kane R, et al. Lithiase du haut appareil urinaire: aspects épidémiologiques, cliniques et thérapeutiques dans la région de Thiès, Sénégal. Rev Méd Madag. 2015;5(1):520–525.
12. Kane R, Diallo Y, Niang L, et al. Upper Urinary tract calculi in senegal: a comparative study between open surgery and endoscopy, a review of 89 cases. Open J Urol. 2015;5(09):142–146. doi:10.4236/oju.2015.59022
13. Odzebe AS, Bouya PA, Berthe HJ, Omatassa FR. Chirurgie A ciel ouvert de la lithiase urinaire au chu de brazzaville: analyse de 68 cas. Open surgery of the urinary tract calculi at the university hospital of brazzaville: analysis of 68 cases. Mali Med. 2010;25(2):32–35.
14. Odzebe AW, Bouya PA, Koutouba E. Lithiase urinaire chez l’enfant au Centre Hospitalier Universitaire de Brazzaville. Rev Afr d’Urologie Et d’Andrologie. 2015;1(4):183–187.
15. Omisanjo O, Bioku M, Williams O, Akinola O, Balogun F, Ikuerowo S. A 5-year review of the presentation and management of urolithiasis in a nigerian teaching hospital. J Surg. 2019;7(5):143–147. doi:10.11648/j.js.20190705.16
16. Odoemene CA, Okere PC, Ugonabo MC. Ureterolithiasis: management in an environment with limited facilities. Niger J Clin Pract. 2017;20(5):622–628. doi:10.4103/njcp.njcp_14_16
17. Kambou T, Traore AC, Zango B, Bonkoungou B, Ouattara T, Sanou A. Lithiase du haut appareil urinaire au Centre Hospitalier Universitaire Sanou Souro de Bobo-Dioulasso (Burkina Faso): aspects épidémiologiques, cliniques et thérapeutiques: A propos de 110. Afr J Urol. 2005;11(1):55–60.
18. Ouédraogo I, Napon AM, Bandré E, Ouédraogo FS, Tapsoba WT, Wandaogo A. Les calculs urinaires de l’enfant au Burkina Faso: à propos de 67 cas [Urinary calculi in children in Burkina Faso: about 67 cases]. Pan Afr Med J. 2015;20(352):1–6.
19. Ngugi PM, Magoha GA, Kiptoon D. Urolithiasis in Nairobi, Kenya. East Afr Med J. 2010;87(10):395–399.
20. Wathigo FK, Hayombe A, Maina D. Urolithiasis analysis in a multiethnic population at a tertiary hospital in Nairobi, Kenya. BMC Res Notes. 2017;10(158):1–5. doi:10.1186/s13104-017-2474-3
21. Mobima T, Songrou F, Debato L. Lithiases urinaires à Bangui (République Centrafricaine): contribution du couple ASP-échographie et de l’UIV. J Afr d’Imagerie Méd. 2018;9(4):175–179.
22. Ouattara Z, Effoé A, Tembely A, Sanogo Z, Yena S, Doumbia D. Etude de 72 cas de lithiases du haut appareil urinaire au service d’urologie de l’hopital du Point G. Mali Méd. 2004;1:14–17.
23. Hounnasso PP, Avakoudjo JD, Paré AK, et al. Symptomatic urinary lithiasis: epidemiology and management at urology department of university hospital of cotonou. Open J Urol. 2015;5(02):7–12. doi:10.4236/oju.2015.52002
24. Rimtebaye K, Sillong FD, Tashkand AZ, Kaboro M, Niang L, Gueye SM. Urolithiasis: diagnostic and therapeutic aspects in urology department of n’djamena in chad. Open J Urol. 2015;5(11):199–206. doi:10.4236/oju.2015.511032
25. Mahamat MA, Diarra A, Kassogué A, et al. Renal colic: epidemiological, clinical etiological and therapeutic aspects at the urology department of the national reference general hospital of n’djamena (Chad). Open J Urol. 2020;10(02):25–33. doi:10.4236/oju.2020.102004
26. Skolarikos A, Straub M, Knoll T, et al. Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines. Eur Urol. 2015;67(4):750–763. doi:10.1016/j.eururo.2014.10.029
27. Barbas C, Garcıa A, Saavedra L, Muros M. Urinary analysis of nephrolithiasis markers. J Chromatogr B. 2002;781(1–2):433–455. doi:10.1016/S1570-0232(02)00557-3
28. Bouatia M, Benramdane L, Idrissi MO, Draoui M. An epidemiological study on the composition of urinary stones in Morocco in relation to age and sex. Afr j Urol. 2015;21(3):194–197. doi:10.1016/j.afju.2015.02.006
29. Cassell AK, Jalloh M, Mbodji MM, et al. Management Challenges of Ureteral Foreign Body-Clinical Vignette and Review of Literature. J Endoluminal Endourol. 2019;2(3):12–17. doi:10.22374/jeleu.v2i3.47
30. Ray AA, Ghiculete D, Pace KT, Honey RJ. Limitations to ultrasound in the detection and measurement of urinary tract calculi. Urology. 2010;76(2):295–300. doi:10.1016/j.urology.2009.12.015
31. Niemann T, Kollmann T, Bongartz G. Diagnostic performance of low-dose CT for the detection of urolithiasis: a meta-analysis. Am j Roentgenology. 2008;191(2):396–401. doi:10.2214/AJR.07.3414
32. Masselli G, Derme M, Bernieri MG, et al. Stone disease in pregnancy: imaging-guided therapy. Insights Imaging. 2014;5(6):691–696. doi:10.1007/s13244-014-0352-2
33. Palmer JS, Donaher ER, O’RIORDAN MA, Dell KM. Diagnosis of pediatric urolithiasis: role of ultrasound and computerized tomography. J Urol. 2005;174(4Part 1):1413–1416. doi:10.1097/01.ju.0000173133.79174.c8
34. Ouédraogo I, Napon AM, Bandré E, Ouédraogo FS, Tapsoba WT, Wandaogo A. Urinary calculi in children in Burkina Faso: about 67 cases. Pan Afr Med J. 2015;20(352):1–6. doi:10.11604/pamj.2015.20.1.5568
35. Odzebe AW, Bouya PA, Koutouba E. Lithiase urinaire chez l’enfant au Centre Hospitalier Universitaire de Brazzaville. Rev Afr d’Urologie Et d’Andrologie. 2015;1(4):183–187.
36. Bryniarski P, Paradysz A, Zyczkowski M, Kupilas A, Nowakowski K, Bogacki R. A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2 cm in diameter. J Endourol. 2012;26(1):52–57. doi:10.1089/end.2011.0235
37. Manikandan R, Gall Z, Gunendran T, Neilson D, Adeyoju A. Do anatomic factors pose a significant risk in the formation of lower pole stones? Urology. 2007;69(4):620–624. doi:10.1016/j.urology.2007.01.005
38. Bhattu AS, Mishra S, Ganpule A, et al. Outcomes in a large series of minipercs: analysis of consecutive 318 patients. J Endourol. 2015;29(3):283–287. doi:10.1089/end.2014.0290
39. Lasser MS, Pareek G. Smith’s Textbook of Endourology.
40. Al-Ba’adani T, Ghilan A, El-Nono I, Alwan M, Bingadhi A. Whether post-ureteroscopy stenting is necessary or not. Saudi Med J. 2006;27(6):845–848.
41. Castro EP, Osther PJ, Jinga V, et al., CROES Ureteroscopy Global Study Group. Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol. 2014;66(1):102–109. doi:10.1016/j.eururo.2014.01.011
42. Mokhless I, Zahran AR, Youssif M, Fahmy A. Tamsulosin for the management of distal ureteral stones in children: a prospective randomized study. J Pediatr Urol. 2012;8(5):544–548. doi:10.1016/j.jpurol.2011.09.008
43. Brinkmann OA, Griehl A, Kuwertz-Bröking E, Bulla M, Hertle L. Extracorporeal shock wave lithotripsy in children. Eur Urol. 2001;39(5):591–597. doi:10.1159/000052509
44. Sen H, Seckiner I, Bayrak O, Erturhan S, Demirbağ A. Treatment alternatives for urinary system stone disease in preschool aged children: results of 616 cases. J Pediatr Urol. 2015;11(1):34–e1. doi:10.1016/j.jpurol.2014.11.010
45. Dede O, Sancaktutar AA, Dağguli M, Utangaç M, Baş O, Penbegul N. Ultra-mini-percutaneous nephrolithotomy in pediatric nephrolithiasis: both low pressure and high efficiency. J Pediatr Urol. 2015;11(5):253–e1. doi:10.1016/j.jpurol.2015.03.012
46. Kaboré FA, Kambou T, Zango B, et al. Épidémiologie d’une cohorte de 450 lithiases urinaires au CHU Yalgado Ouédraogo de Ouagadougou (Burkina Faso). Progrès en urologie. 2013;23(12):971–976. doi:10.1016/j.purol.2013.04.014
47. Yaméogo CA, Ky B, Ouattara A, Kirakoya B, Kaboré FA. Holmium laser ureteroscopy in the treatment of the upper urinary tract stones: concerning 54 cases in the surgical department of the saint camille hospital of ouagadougou (burkina faso). Open J Urol. 2019;10(02):17–24. doi:10.4236/oju.2020.102003
48. Adusei B, Mante S, Yegbe P, Amegbor J. Urolithiasis and intracorporeal lithotripsy in 37 Military Hospital, Accra, Ghana. Ghana Med J. 2019;53(4):304–307. doi:10.4314/gmj.v53i4.9
49. Ondo CZ, Fall B, Sow Y, et al. La lithotripsie extracorporelle: expérience d’un centre Sénégalais. Afr J Urol. 2018;24(4):319–323. doi:10.1016/j.afju.2018.03.001
50. Aslam Z Is laparoscopic urological training in Sub-Saharan Africa a goal worth pursuing? Observations from my experience with IVUmed in Senegal 2019 Sept 01. Available from: https://www.urologynews.uk.com/features/features/post/is-laparoscopic-urological-training-in-sub-saharan-africa-a-goal-worth-pursuing-observations-from-my-experience-with-ivumed-in-senegal.
51. Biyani CS, Bhatt J, Taylor J, Gobeze AA, McGrath J, MacDonagh R. Introducing endourology to a developing country: how to make it sustainable. J Clin Urol. 2014;7(3):202–207. doi:10.1177/2051415813514971
52. Olapade-Olaopa EO, Onawola KA. Challenges for urology in sub-Saharan Africa in 2006. J Men’s Health Gender. 2006;Mar(1):109–116. doi:10.1016/j.jmhg.2006.01.004
53. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535–543. doi:10.7326/0003-4819-158-7-201304020-00005
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.