Back to Journals » Open Access Surgery » Volume 15
Surgical Management of Giant Toxic Multinodular Goiter with Compressive Symptoms in Setup with Scarce Resources: A Case Report
Authors Taeme G/tsion M , Tibebu Shumargaw A
Received 13 September 2022
Accepted for publication 17 December 2022
Published 28 December 2022 Volume 2022:15 Pages 101—108
DOI https://doi.org/10.2147/OAS.S389685
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Luigi Bonavina
Mulugeta Taeme G/tsion,1 Aschalew Tibebu Shumargaw2
1Department of Surgery, School of Medicine, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia; 2Department of Surgery, Dessie Comprehensive Specialized Hospital, Dessie, Ethiopia
Correspondence: Mulugeta Taeme G/tsion, Department of Surgery, School of Medicine, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia, Email [email protected]
Introduction: Toxic multinodular goiter (TMNG) usually occurs in older individuals, who often have a lengthy history of nontoxic multinodular goiter. The cases of giant multinodular goiter are rare clinical conditions nowadays. Thyroidectomy is generally the preferred treatment option because it resolves both toxic and compressive symptoms.
Case Report: We present here a case of giant toxic multinodular goiter successfully treated at Dessie comprehensive specialized hospital. A 60-year-old female presented with anterior neck swelling of 30 years and toxic symptoms of 3 years duration. She had breathing difficulty in a supine position. On physical examination, there was a huge anterior neck mass measuring 27× 24 cm in the largest dimensions. Based on TFT, FNAC, and ultrasound, she was diagnosed with a giant toxic multinodular goiter. After medical treatment with antithyroid drugs, a total thyroidectomy was performed and the gland was dissected successfully.
Discussion: The most effective treatment of giant toxic multinodular goiter is total thyroidectomy which avoids recurrence and subsequent complication rates with repeat surgery.
Conclusion: Due to difficulty during intubation, the presence of altered anatomy, and adhesions to the surrounding structures associated with giant toxic MNG, it will be a challenge to do a thyroidectomy.
Keywords: case report, giant goiter, thyroid-stimulating hormone, toxic multinodular goiter, total thyroidectomy
Introduction
Goiter, enlarged thyroid, a common condition worldwide in general and in Ethiopia. This is mainly due to benign thyroid disease caused by iodine deficiency.1 Thyroid enlargement is either diffuse or nodular. Because of its functionality, it can also be non-toxic (euthyroid), toxic (hyperthyroid), or underactive (hypothyroid).2
Toxic multinodular goiter (TMNG) usually occurs in older individuals, who often have a lengthy history of nontoxic multinodular goiter. Over several years, enough thyroid nodules become autonomous to cause hyperthyroidism.3
Giant goiter weighing more than 500 grams can cause compression symptoms affecting the trachea, esophagus, and recurrent laryngeal nerve. This is usually associated with a malignant goiter, as opposed to a benign thyroid enlargement. There is also a surgical challenge due to possible tracheomalacia, retrosternal extension, difficulty in intubation, and intraoperative dissection of the thyroid.4
Treatment options for TMNG are radioiodine ablation and thyroidectomy, which depend on patient preference, symptoms, nodule volume, comorbidities, speed of recovery, side effects, and cost. Thyroidectomy is generally the preferred treatment because it resolves both toxic and compressive symptoms. But lifelong levothyroxine replacement therapy and possible complications such as the risk of permanent hypoparathyroidism or recurrent laryngeal nerve injury are confounding factors.5,6
In this case report, we have diagnosed a patient with giant toxic MNG, managed by total thyroidectomy. This case report has been reported in line with the SCARE criteria.7
Case Report
Patient Information
The patient is 60-year-old female, housewife and Muslim. Presented with a 30-year-old anterior neck swelling that had gradually increased in size but had progressively worsened over the past 3 years to surgical OPD at Dessie comprehensive specialized hospital. She has also had palpitations, intolerance to heat, and hand tremors for the past 3 years. In addition to this, she had shortness of breathing in a supine position. Otherwise, the patient had no concomitant morbidity, no surgical or medical history, and no other relevant family history. The patient took about 30 years to seek medical attention since she thought it is untreatable About two and half years was required to make euthyroid state before got surgical management.
Clinical Findings
On physical examination, the PR was 122 beats per minute and 27×24 cm measuring anterior neck mass in its largest dimensions representing a multidirectional enlargement with multinodular goiter covering the entire anterior and left lateral part of the neck with no ocular signs (Figures 1–3).
 |
Figure 1 Giant multinodular goiter (left lateral view). |
 |
Figure 2 Giant multinodular goiter (right lateral view). |
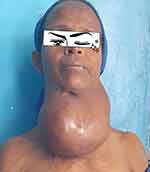 |
Figure 3 Giant multinodular goiter (anterior view). |
Diagnostic Assessment
The thyroid function test showed low TSH and increased free T4 and T3. FNAC and neck ultrasound were determined with the result of the colloid feature and TIRADS 2 (benign goiter) respectively.
With a working diagnosis of giant toxic multinodular goiter, she was treated for two and a half years with propylthiouracil (PTU) and beta-blockers. After toxicity was controlled, she was prepared for surgery.
Before surgery, she received Lugol’s iodine solution for one week and a neck x-ray was taken, which showed significant right-sided tracheal deviation and some central calcifications (Figures 4 and 5).
 |
Figure 4 Lateral neck x-ray showing huge anterior neck mass with central calcification. |
 |
Figure 5 AP neck x-ray showing huge anterior neck mass with right side tracheal displacement. |
Therapeutic Intervention
After informed consent was taken, total thyroidectomy was performed by a general surgeon with assistance of final year surgery residents under general anesthesia and the intubation was uncomplicated. An extended collar incision was performed (Figure 6). For better visualization, strap and sternocleidomastoid muscles were transected since the thyroid gland was giant in size. The carotid sheath was displaced posterolaterally on both sides. Middle thyroid veins, superior poles, and inferior poles were dissected, identified, and sectioned closer to the thyroid tissue. Meticulous dissection was done to identify and preserve recurrent laryngeal nerve and parathyroid glands. Then the giant thyroid, which weighed about 850 grams, was extracted and completely removed (Figures 7 and 8). Bilateral drains were left in the thyroid bed and severed muscles were repaired. Intraoperatively, there was bleeding from any thyroid tissue surface, requiring a transfusion of 2 units postoperatively. The patient was immediately extubated and transferred to the recovery room after fully awakening and producing normal sounds. The total duration of surgery was two and half hours.
 |
Figure 6 Extended collar incision. |
 |
Figure 7 Specimen of removed giant thyroid gland (anterior view). |
 |
Figure 8 Specimen of removed giant thyroid gland (posterior view). |
Follow-Up and Outcomes
On her immediate post operative day, she had tachycardia, pale conjunctiva and decreased red blood cell count for which two units of blood transfusion was required to stabilize her. -Grade II Clavien-Dindo complication classification.
The patient was discharged on the 4th postoperative day without complications. Follow-up visits at 2nd weeks, 1st, 3rd, and 6th months with no significant complications. But there was hyperpigmented and some superfluous skin, which was removed under local anesthesia. The patient finally received thyroid hormone replacement therapy with levothyroxine after hypothyroidism was confirmed and has regular follow up every three to six months at outpatient department.
Discussion
The cases of giant multinodular goiter are rare clinical conditions nowadays. Toxic multinodular goiters usually occur in older individuals, who often have a prior history of nontoxic multinodular goiter. This is mainly caused by iodine deficiency (endemic goiter) but medication, growth-stimulating antibodies, and inherited defects in thyroid hormone synthesis are considered possible reasons for etiology. Most patients present with huge goiter with compressive symptoms like dyspnea and dysphagia associated with symptoms and signs of hyperthyroidism but extrathyroidal manifestations are absent unlike Graves’ disease.8
Radioiodine therapy (RAT) is effectively used in toxic MNG resulting in improvement of pressure symptoms in the majority of patients that need medical therapy to be continued for several months for better improvement. But the success rate is lower than when it is used in case of graves’ disease which has 85–90% of effectiveness.5,6
Surgery as total thyroidectomy is strongly recommended for toxic MNG to avoid recurrence and consequently increased complication rates with repeat surgery. Besides it is rapid, reliable, removes any coexisting malignancy, and requires no retreatment.8
Those patients with goiter should undergo TFT (T3, T4, TSH) measurement, ultrasound of the neck, and FNA as a diagnostic modality. A neck x-ray and CT scan can be done when the patient diagnosed with a giant goiter.9
Surgery is challenging in such cases and the majority of patents needs carful surgical approach not have complication like bleeding, recurrent laryngeal nerve injury, tracheomalacia, hematoma, and permanent hypocalcemia because of the presence of altered anatomy, and adhesions to the surrounding structures.10
In this case report, we presented a patient with a giant TMNG, which was compressing the trachea with significant right-side deviation. After confirming the toxicity is controlled, a total thyroidectomy was done. Since we are working in a resource-limited setup, we did not perform preoperative direct or indirect laryngoscopy for vocal cord assessment prior to thyroidectomy and we did not use a nerve monitor rather bilateral recurrent laryngeal nerves were identified and preserved intraoperatively with meticulous surgical technique. Since her huge goiter was too vascularized, there was bleeding from its surface until thyroid vessels were ligated which required blood transfusion. Parathyroid glands were identified and preserved too. Postoperatively there was no voice change and serum calcium were normal. Finally, the patient was discharged on the 4th postoperative day. Her subsequent follow-up was uneventful and has regular follow up every three to six months at outpatient department. The patient is adherent for her lifelong levothyroxine replacement treatment.
Conclusion
It is challenging to do thyroidectomy in patients with giant goiter because of difficulty during intubation, the presence of altered anatomy, and adhesions to the surrounding structures that increase the risk of complications. Recognizing and treating these kinds of cases are important because they constitute a preventable cause of mortality if they are predicted pre-operatively and meticulous techniques of thyroidectomy implemented.
Ethical Approval
The ethical approval was exempted as the case reports do not require.
Consent
Informed written consent was obtained from the patient for publication of this case report and accompanying images.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yisihak S, Suga Y, Abebe E. Patterns of surgically treated thyroid disease: a two years review at St. Paul hospital millennium medical college, Addis Ababa, Ethiopia. Ethiopian J Health Sci. 2020;30(1):1–6.
2. Alaguvelsamy S, Singh SP, Ramalingam R, Kombupalayam R, Gounder K. CASE REPORT – OPEN ACCESS International Journal of Surgery Case Reports Giant toxic multinodular goiter with dyspnea: a case report. Int J Surg Case Rep. 2020;73:190–195. doi:10.1016/j.ijscr.2020.07.017
3. Brunicardi F, Andersen D, Billiar T, et al. Schwartz’S Principles of Surgery. Vol. 2. McGraw-hill; 2019:1625–1698.
4. Abraham D, Singh N, Lang B, Chan W-F, Lo C-Y. Benign nodular goitre presenting as acute airway obstruction. ANZ J Surg. 2007;77(5):364–367. doi:10.1111/j.1445-2197.2007.04061.x
5. Mumtaz M, Lin LS, Hui KC, Sharifuddin A, Khir M. Radioiodine I-131 for the therapy of graves’ disease radioiodine I-131 for the therapy of graves. Disease. 2009;16:25.
6. Ross DS. Radioiodine therapy for hyperthyroidism. 2011.
7. Agha RA, Borrelli MR, Farwana R, et al. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg. 2018;60:132–136. doi:10.1016/j.ijsu.2018.10.028
8. Alimoglu O, Akdag M, Sahin M, Korkut C, Okan I, Kurtulmus N. Comparison of surgical techniques for treatment of benign toxic multinodular goiter. World J Surg. 2005;924:921–924. doi:10.1007/s00268-005-7767-3
9. Hajmanoochehri F, Rabiee E. FNAC accuracy in diagnosis of thyroid neoplasms considering all diagnostic categories of the Bethesda reporting system: a single-institute experience. J Cytol. 2015;32:238. doi:10.4103/0970-9371.171234
10. Nada A, Ahmed AM, Vilallonga R, Armengol M, Moustafa I, Report C. Case report A giant euthyroid endemic multinodular goiter with no obstructive or compressive symptoms. Case Rep Med. 2011;2011:1–4. doi:10.1155/2011/620480
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
