Back to Journals » International Medical Case Reports Journal » Volume 15
Surgical Management of Aneurysmal Bone Cyst of the Pubis: A Case Report and Review of Literature
Authors Dawod MS , Alisi MS , Rabab'a H , Abdulelah AA , Almaaitah HW , Haddad B
Received 6 April 2022
Accepted for publication 31 May 2022
Published 14 June 2022 Volume 2022:15 Pages 287—292
DOI https://doi.org/10.2147/IMCRJ.S369073
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Mohd Said Dawod,1 Mohammed S Alisi,2,3 Hammam Rabab’a,4 Ahmed A Abdulelah,4 Huthaifa W Almaaitah,4 Bassem Haddad2
1Department of Special Surgery, Division of Orthopaedics, School of Medicine, Mutah University, Al Karak, Jordan; 2Department of Special Surgery, Division of Orthopaedics, School of Medicine, The University of Jordan, Amman, Jordan; 3Faculty of Medicine, Islamic University of Gaza, Gaza, Palestine; 4School of Medicine, The University of Jordan, Amman, Jordan
Correspondence: Mohammed S Alisi, The University of Jordan, School of Medicine, Queen Rania Al Abdullah St 266 Al Jubaiha, Amman, 11942, Jordan, Tel +962790983284, Email [email protected]
Introduction: Aneurysmal bone cysts (ABC) are expansile, lytic, and benign but locally aggressive lesions. Pelvic ABCs are rare and sometimes difficult to manage surgically.
Case Report: A 17-year-old female presented with progressive pain and swelling in the right inguinal region. Pelvis radiograph showed a lytic expansile lesion of the superior pubic ramus. A multiloculated cystic lesion was evident on magnetic resonance imaging, and postoperative histopathological evaluation confirmed the diagnosis of ABC. The patient was treated successfully with an intralesional curettage and bone grafting. The postoperative course was uncomplicated with complete healing and no recurrence after 14 months of follow-up.
Conclusion: ABC of the pubic ramus is a rare entity. Complete intralesional curettage and bone grafting is an effective treatment for pubic ABC. An individualized management approach considering the surgical team expertise, tumor size, and proximity to neighboring structures is recommended..
Keywords: aneurysmal bone cyst, ABC, curettage, pelvic, pubic ramus, pubis
Introduction
An aneurysmal bone cyst (ABC) is a benign blood-filled osteolytic lesion associated with rapid growth potential and locally aggressive behavior. It accounts for 1–2% of all primary bone tumors.1 The majority of ABCs (70%) arise as a primary bone lesion, while 30% are reactive and arise secondary to a pre-existing osseous disease such as giant cell tumor, chondroblastoma, and eosinophilic granuloma.2,3 ABC can be observed at any age but is commonly present in skeletally immature individuals with a peak incidence during the first two decades of life. ABCs can affect any bone but have a predilection for the spine, pelvis, and long bones.3
The pathophysiology of these tumors remains under discussion and may be vascular, traumatic, or genetic.3 Genetic abnormalities involving osteoblast cadherin 11 gene (CDH11) and Ubiquitin Specific Peptidase 6 gene (USP6) have been reported in cases of primary ABCs.4 The classic imaging features include an expansile radiolucent lesion with fluid–fluid levels visible on magnetic resonance imaging (MRI).2,3
The symptoms of ABC typically involve pain, swelling, and in rare instances, the development of pathological fractures due to the destructive nature of the lesion.5–7 Nonetheless, the presenting symptoms may vary according to the site of the tumor.
Several treatment modalities have been proposed, ranging from curopsy and percutaneous therapy to complete surgical excision, with surgery remaining as the mainstay of treatment.1,8,9 However, despite the variety of the proposed treatment options, tumor recurrence may reach up to 50%, with the rate varying depending on the treatment modality.5,10
We report a rare case of a 17-year-old female patient presenting with a 9-month history of right atraumatic groin pain. Imaging studies revealed an expansile osseous mass consistent with an aneurysmal bone cyst in the right superior pubic ramus. A preliminary diagnosis of ABC was made, and the patient underwent extensive curettage of the lesion and bone grafting.
ABC of the pubis is extremely rare; we found only 8 published cases on PubMed library. To the best of our knowledge, this is the first case of a pubic ABC to be reported in Jordan. Institutional review board approval was not required for this case report. The patient and her family signed an informed consent to publish their data and images.
Case Presentation
A 17-year-old healthy female patient presented to the orthopedic clinic complaining of right-groin pain for 9 months. The patient initially started complaining of right-groin pain upon walking long distances. She had no history of trauma. The pain gradually progressed, and eventually also occurred at night. This pain was associated with an increased swelling in the same region. The patient denied any constitutional symptoms.
Physical examination revealed a mildly tender, hard, localized swelling over the right pubic area with no overlying pulsations or skin changes. The range of motion of the right hip was within normal.
A pelvic radiograph revealed an expansile lytic lesion involving the right superior pubic ramus (Figure 1). A pelvic MRI showed an expansile multicystic bony lesion measuring 6.8 × 3.3 × 4.5 cm with multiple fluid–fluid levels involving the right pubic ramus (Figure 2).
 |
Figure 1 Showing an expansile lytic lesion in the right superior pubic ramus on the pre-operative pelvic radiograph. |
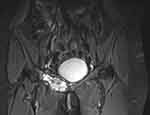 |
Figure 2 Showing an expansile osseous mass with multiple cystic components in the right superior pubic ramus as appeared on the pre-operative pelvic MRI. |
Routine hematological investigations including complete blood count (CBC), kidney function tests, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and alkaline phosphatase were within normal ranges.
Based on these clinical and radiological features, the patient was preliminarily diagnosed with an aneurysmal bone cyst of the right superior pubic ramus. Following a discussion of the initial diagnosis, prognosis, and treatment options with the patient and her parents, the patient was scheduled for curettage and grafting of the right superior pubic ramus.
We started the procedure by taking a percutaneous biopsy. The frozen section confirmed the benign nature of the lesion. Afterwards, using a modified Stoppa approach, an extensive curettage of the cyst was done followed by irrigation with alcohol and saline (Figure 3). Demineralized bone matrix and synthetic biphasic calcium phosphate granules bone graft were subsequently impacted (Figure 4A). The cyst components were sent for histopathological evaluation. The final histopathology result revealed blood-filled cystic spaces lined with multinucleated giant cells and separated by cellular septae containing fibroblasts, giant cells, and woven bones with hemosiderin deposition consistent with an aneurysmal bone cyst.
 |
Figure 3 Showing complete curettage of the lesion as appeared on the intra-operative pelvic radiograph. |
 |
Figure 4 Showing the pelvic radiograph at different follow-up stages ((A) postoperative day 0, (B) postoperative day 17, (C) 8 months post-operatively, (D) 12 months post-operatively). |
The patient was followed up for 14 months, she progressed to full weight-bearing and was symptom-free. The follow-up pelvic radiographs at 17 days, 8 months, and 12 months post-operatively demonstrated that the bone grafted site has matured satisfactorily as shown in Figures 4B–D, respectively. The patient is planned to be followed-up in an orthopedic clinic for at least five years after the surgery.
Discussion
The typical age of presentation of ABC is in the first 2 decades of life with approximately 80% of cases presenting in that period. It has slight female predominance.5 Our case followed the general trend of ABC presentation.
The most commonly affected bones are humerus, femur, tibia, pelvis, and fibula, respectively.10 ABCs rarely involve bones such as the clavicle, scapula, rib, carpal, and tarsal bones.10–14 The occurrence of ABC in the superior pubic ramus is also extremely rare, with this rarity being emphasized by the presence of only 8 reported cases in the literature based on a literature review conducted using PubMed.15–20 Table 1 summarizes the treatment modalities and outcomes of the published cases of pubic ABCs.
 |
Table 1 Summarizes the Treatment Modalities and Outcomes of the Published Cases of Pubic ABC |
Unicameral bone cysts, telangiectatic osteosarcoma, giant cell tumor, and eosinophilic granuloma are among the differential diagnoses of ABC.21 It is highly important to rule out telangiectatic osteosarcoma before diagnosing ABC as the proposed treatment options and subsequent prognosis differ drastically between the two.3 Recent genetic tests to detect translocations of USP6 and CDH11 genes helped in differentiating between primary and secondary ABCs.4
Imaging studies, particularly plain radiographs and MRI, are of paramount importance in diagnosing ABC and aiding in excluding possible differential diagnoses despite not providing a definitive diagnosis. The appearance of ABC on plain radiographs is referred to as “soap bubble appearance” due to the multi-locular appearance resulting from trabeculations within the radiolucent lesion. MRI is required to supplement the radiographs as it reveals the appearance of an expansive lesion with internal septations and edema in the presence of multiple fluid levels that are suggestive of ABC.22 However, histological examination of biopsy remains crucial for the diagnosis of ABC as the clinical symptomatology and imaging findings of ABC are not specific and overlap with other tumors, particularly telangiectatic osteosarcoma.22 In our patient, the imaging studies showed the typical appearance of an ABC. Nonetheless, we initially confirmed the benign nature of the lesion via a frozen section. Then, we proceeded to the formal surgical procedure.
Several treatment modalities have been described for the treatment of ABC. Less invasive therapies include curopsy, intralesional injection (sclerotherapy or doxycycline), systemic bisphosphonate and denosumab, percutaneous curettage and local grafting, and selective arterial embolization.7,9,22 More invasive therapies include intralesional curettage with or without grafting and en bloc resection. Intralesional curettage with or without grafting remains the standard of care for treatment of ABC.22
Although en bloc surgical resection can result in 0% recurrence rate in some reports, it is associated with significant morbidity.23 Adjuvant therapy could be utilized to target microscopic remnants in order to lower recurrence rate. However, the use of adjuvant therapy has been debated due to the lack of comparative studies investigating its efficacy.3
There remains a lack of consensus regarding the preferred type of management for ABC of the superior pubic ramus, evidently due to the limited cases reported in the literature.
There was a wide variation in treatment for the published cases of pubic ABC (Table 1). Kónya & Szendröi reported complete ossification of 3 cases of pubic ABC after treatment with transcatheter superselective embolization.15 We did not try transcatheter embolization in our case because of having no experience in such cases.
Delloye et al16 used a minimally invasive approach to inject a bone paste made of autogenic bone marrow and allogenic bone powder without curettage of the lesion. In contrast, Khan et al17 did curette the lesion with a high-speed burr and reconstructed the bone defect using iliac crest cancellous graft. More invasive management has been reported by Rao et al18 using complete surgical excision without grafting. They reported no recurrence at 2 years, yet a persistent bone gap. Also, Nayak et al19 had not used any graft after intralesional curettage, with no recurrence at 6 months follow-up.
Interestingly, the size and location of the lesion in our case were similar to what was reported by Downey et al.20 Our treatment included the same surgical technique of complete curettage and grafting but without fixing the hemipelvis using a plate, in contrast to what Downey had done. In our opinion, the procedure we used did not affect the stability of the pelvis, so we did not need to augment by plate fixation that also might require another extensive procedure to be removed later on.
We recommend giving the patient the best chance of complete healing of the lesion with a procedure of lowest recurrence rate without increasing the morbidity in such a risky region.
The surgical approach for ABCs of the superior pubic ramus is regarded to be of significant difficulty due to the close proximity to an arterial anastomosis present in the posterior aspect of superior pubic ramus, known as corona mortis, that could potentially complicate the procedure if iatrogenically injured.24
Based on the different treatment modalities that have been used in previously reported cases, the lack of consensus dictates an individualized approach in the management of ABC of superior pubic ramus taking into consideration the surgical team expertise, tumor size, and proximity to neighboring structures and organs.
Unfortunately, the limited number of published cases precludes doing comparative studies about long-term outcomes of different treatment modalities.
Conclusion
ABC of the pubic ramus is a rare entity. Complete intralesional curettage and bone grafting is an effective treatment for pubic ABC. An individualized management approach considering the surgical team expertise, tumor size, and proximity to neighboring structures is recommended.
Funding
No financial support was required for this article.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Mendenhall WM, Zlotecki RA, Gibbs CP, Reith JD, Scarborough MT, Mendenhall NP. Aneurysmal bone cyst. Am J Clin Oncol. 2006;29(3):311–315. doi:10.1097/01.coc.0000204403.13451.52
2. Hakim DN, Pelly T, Kulendran M, Caris JA. Benign tumours of the bone: a review. J Bone Oncol. 2015;4(2):37–41. doi:10.1016/j.jbo.2015.02.001
3. Rapp TB, Ward JP, Alaia MJ. Aneurysmal bone cyst. J Am Acad Orthop Surg. 2012;20(4):233–241. doi:10.5435/JAAOS-20-04-233
4. Oliveira AM, Perez-Atayde AR, Inwards CY, et al. USP6 and CDH11 oncogenes identify the neoplastic cell in primary aneurysmal bone cysts and are absent in so-called secondary aneurysmal bone cysts. Am J Pathol. 2004;165(5):1773–1780.
5. Deventer N, Deventer N, Gosheger G, de Vaal M, Vogt B, Budny T. Current strategies for the treatment of solitary and aneurysmal bone cysts: a review of the literature. J Bone Oncol. 2021;30:100384. doi:10.1016/j.jbo.2021.100384
6. Hauschild O, Lüdemann M, Engelhardt M, et al. Aneurysmal bone cyst (ABC): treatment options and proposal of a follow-up regime. Acta Orthop Belg. 2016;82(3):474–483.
7. Alisi MS, Abu hassan F, Hammad Y, Khanfar A, Samarah O. Percutaneous curettage and local autologous cancellous bone graft: a simple and efficient method of treatment for benign bone cysts. Arch Bone Jt Surg. 2022;10(1):104–111. doi:10.22038/ABJS.2021.55189.2747
8. Muratori F, Mondanelli N, Rizzo AR, et al. Aneurysmal bone cyst: a review of management. Surg Technol Int. 2019;35:325–335.
9. Cruz GS, Cuevas-Suárez CE, Saavedra JPA, Giorgis R, Teixeira MRK, Muniz FWMG. Percutaneous treatments of primary aneurysmal bone cysts: systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2021;31(7):1287–1295.
10. Bavan L, Wijendra A, Kothari A. Efficacy of treatment interventions for primary aneurysmal bone cysts: a systematic review. Bone Jt Open. 2021;2(2):125–133. doi:10.1302/2633-1462.22.BJO-2020-0168
11. Alrabayah M, Alisi MS, Abdulelah AA, Atiyat B, Alnawaiseh H. A large aneurysmal bone cyst of the clavicle in a 5-year-old child: a case report and review of literature. Curr Orthop Pract. 2021;32(3):290–293. doi:10.1097/BCO.0000000000000989
12. Atalay İB, Yapar A, Öztürk R. Primary aneurysmal bone cyst of the scapula in adult patient: two case reports and a review of the literature. Arch Orthop Trauma Surg. 2020;140(10):1367–1372. doi:10.1007/s00402-019-03327-z
13. Bingol O, Ozdemir G, Yasar NE, Deveci A. Aneurysmal bone cyst of the medial cuneiform: a case report. J Am Podiatr Med Assoc. 2021;111(1):
14. Aksu AE, Üstün GG, Uzun H, Gedikoğlu G. Aneurysmal bone cyst of pisiform bone: diagnosis and treatment of a rare entity: case report and a review of the literature. J Hand Surg Asian Pac Vol. 2021;26(4):722–727. doi:10.1142/S2424835521720231
15. Kónya A, Szendröi M. Aneurysmal bone cysts treated by superselective embolization. Skeletal Radiol. 1992;21(3):167–172. doi:10.1007/BF00242130
16. Delloye C, De Nayer P, Malghem J, Noel H. Induced healing of aneurysmal bone cysts by demineralized bone particles. A report of two cases. Arch Orthop Trauma Surg. 1996;115(3–4):141–145. doi:10.1007/BF00434541
17. Khan AQ, Siddiqui YS, Parameshwar A, Anwar-Sherwani MK. Aneurysmal bone cyst of pubis. A rare presentation. Saudi Med J. 2010;31(3):317–320.
18. Rao A, Samant PD, Varshneya A. Aneurysmal bone cyst of pubic ramus: a rare entity. J Orthop Case Rep. 2013;3(4):42–45. doi:10.13107/jocr.2250-0685.131
19. Nayak A, Kulkarni S, Kulkarni A, Natesh K, Bami M. Aneurysmal bone cyst of the pubis: a case report. J Clin Diagn Res. 2013;7(8):1740–1742. doi:10.7860/JCDR/2013/5514.3254
20. Downey C, Daly A, Molloy AP, O’Daly BJ. Atraumatic groin pain secondary to an aneurysmal bone cyst: a case report and literature review. World J Orthop. 2020;11(3):197–205. doi:10.5312/wjo.v11.i3.197
21. Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res. 2015;101(1 Suppl):S119–S127. doi:10.1016/j.otsr.2014.06.031
22. Park HY, Yang SK, Sheppard WL, et al. Current management of aneurysmal bone cysts. Curr Rev Musculoskelet Med. 2016;9(4):435–444. doi:10.1007/s12178-016-9371-6
23. Campanacci M, Capanna R, Picci P. Unicameral and aneurysmal bone cysts. Clin Orthop Relat Res. 1986;204:25–36.
24. Darmanis S, Lewis A, Mansoor A, Bircher M. Corona mortis: an anatomical study with clinical implications in approaches to the pelvis and acetabulum. Clin Anat. 2007;20(4):433–439. doi:10.1002/ca.20390
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
