Back to Journals » Clinical Ophthalmology » Volume 14
Surgical Management for Silicone Oil Barrier of Traumatic Aniridia with Aphakia: Suturing of Temporary Iris-Diaphragm Prior to Final Iris-Lens-Diaphragm Implantation
Authors Mayer CS, Baur I , Storr J, Markard A, Khoramnia R
Received 1 October 2020
Accepted for publication 24 November 2020
Published 21 December 2020 Volume 2020:14 Pages 4439—4450
DOI https://doi.org/10.2147/OPTH.S284159
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Christian S Mayer,1,* Isabella Baur,1,* Julia Storr,2 Alexander Markard,1 Ramin Khoramnia1
1Department of Ophthalmology, University Hospital Heidelberg, University of Heidelberg, Heidelberg, Germany; 2Department of Ophthalmology, Technical University Munich, Munich, Germany
*These authors contributed equally to this work
Correspondence:Christian S Mayer
Department of Ophthalmology, University Hospital Heidelberg, University of Heidelberg, Im Neuenheimer Feld 400, Heidelberg 69120, Germany
Email [email protected]
Purpose: Patients with traumatic aniridia, aphakia and retinal complications can require silicone oil endotamponade. In the absence of compartmentalization, there is a risk of silicone oil migrating to the anterior chamber which can cause long-term complications. We report a two-step procedure in trauma cases, using sutures for silicone oil retention in primary care and subsequently prior to secondary artificial iris (AI) and intraocular lens (IOL) implantation, to achieve a reconstruction of the anterior and posterior chamber.
Material and Methods: Seven patients with loss of the iris-lens-diaphragm after an ocular trauma and the need for silicone oil endotamponade underwent a primary intervention including wound closure, placement of silicone oil retention sutures and silicone oil filling. Four of those underwent secondary reconstruction with silicone oil removal and AI and IOL implantation and could be included in this retrospective observational study. All main outcome measures were evaluated after the first and after the second surgery. The main outcome measures were morphological findings, subjective impairment from glare, subjective cosmetic disfigurement, patient satisfaction and intraocular pressure (IOP) as well as best-corrected distance visual acuity and objective refraction.
Results: The retention sutures could effectively prevent silicone oil migration into the anterior chamber in the first surgery. Silicone oil emulsifications in the anterior chamber were observed in one patient. In two patients, pigment deposition at the sutures was seen. Subjective impairment from glare and subjective cosmetic disfigurement could be reduced after the second surgery compared to the evaluation after the first surgery. IOP and best-corrected distance visual acuity remained stable. No eye needed silicone oil refilling after the secondary reconstruction surgery.
Conclusion: Our two-step approach is viable and provides good functional and aesthetic results. We observed a high patient satisfaction.
Keywords: aniridia, aphakia, trauma, open globe injury, retinal detachment
Introduction
Traumatized eyes can show multiple structural damage. In many cases, the anterior and posterior segment of the eye are affected, including iris, lens, vitreous cavity and retina. Most of the injuries result from hitting the eye from anterior: due to the direction of the impact the trauma can affect the cornea, iris and lens. In more severe cases the posterior segment of the eye is also affected, including vitreous body, retina and sclera. It is sometimes challenging to reconstruct these functional and anatomical structures. Often, multiple surgeries are necessary. During primary trauma surgery, the most critical steps are primary wound closure, control of bleeding, and reattachment of the retina to stabilize the globe. Secondary reconstruction of the iris, lens and cornea has to be planned to achieve recovery of the visual acuity. One of the most frequently employed endotamponades in trauma surgery of the posterior segment is a silicone oil tamponade.1 During primary intervention, silicone oil instillation is frequently needed. The negative effect of long-term contact between silicone oil and corneal endothelium is well-documented.2 Silicone oil is toxic to the endothelial cells and contact should be prevented. If there is no longer a physiological barrier, eg an iris-lens-diaphragm, between the anterior and posterior segment, the silicone oil will invariably make contact with the endothelium leading to corneal decompensation with endothelial cell loss, corneal edema and/or band keratopathy developing.2,3 To prevent this, a variety of options can be implemented:
- Use of gas - if possible - instead of silicone oil as endotamponade.
- Surgical peripheral basal iridectomies can be applied in aphakic eyes that retain a mostly intact iris.4,5
- In aphakia and aniridia, various artificial intraocular lenses (IOL) and/or artificial irises can be implanted – effectively forming a new iris-lens-diaphragm.6,7
- Use of special sutures can prevent the contact between silicone oil and the endothelium, serving as a substitute for an iris-lens-diaphragm.8
In 1985, Ando described the technique of an inferior peripheral iridectomy in aphakic eyes with an intact iris diaphragm to prevent the prolapse of silicone oil and development of a pupillary block.4 But in patients with traumatic aniridia and aphakia, this technique is not applicable. We describe an effective approach of reconstructing the iris-lens-diaphragm using a two-step method: In a primary care situation, using silicone oil retention sutures may be a solution to prevent silicone oil from entering the anterior chamber and to avoid contact with the corneal endothelium in aphakic eyes with iris loss. A secondary iris-lens-diaphragm is implanted in a planned subsequent procedure. There are several implants available to create an iris-lens-diaphragm, but they are either made of a rather rigid material9 or provide inferior aesthetic results as they cannot be customized.10 Other implants are designed for prevention of phthisis bulbi, not functional reconstruction.6,7,11 In our study, patients with aphakia and aniridia as well as the need for silicone oil endotamponade were treated. With no aniridia implant available in the primary care situation, the approach using silicone oil retention sutures we describe in this manuscript was the method of choice. Several techniques have been described for silicone oil retention sutures,12–14 but to our knowledge, there are no published cases of patients treated with the two-step approach we describe in this study.
Materials and Methods
Seven consecutive patients between 2016 and 2019 s with (1) a loss of iris-lens-diaphragm and (2) the need for silicone oil tamponade were treated with temporary iris-diaphragm sutures. Three patients were lost of follow-up before secondary reconstruction. We included 4 patients in this retrospective observational study who received temporary iris-diaphragm sutures for silicone oil barrier prior to final iris-lens-diaphragm implantation. All eyes had suffered a severe blunt or sharp globe trauma. All procedures were performed under general anesthesia and by the same surgeon (CM).
All procedures were part of an at least two-step intervention with primary wound closure and secondary reconstruction surgery:
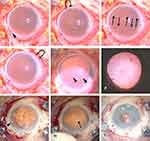
Description of Primary Care Surgical Procedure Using the Grid-Weaved-Iris-Suture (Figure 1A–F)
All patients were aphakic and had a traumatic iris defect after ocular trauma. A priority was to achieve primary wound closure and pressurization of the globe by implementation in primary care intervention of a grid-like suture in place of an iris-lens-diaphragm, using a non-absorbable 10–0 polypropylene “Prolene” monofilament suture with a long 16 mm needle (Johnson & Johnson Inc., New Brunswick, New Jersey, USA). After opening the conjunctiva and performing primary wound closure, the grid-pattern suture can be started from any suitable position at 1.2 to 1.5 mm from the limbus (Figure 1A), leading the needle vertically across the anterior chamber and exiting, 180 degrees round the corneal periphery, on the corresponding opposite side. Afterwards, the second stitch is placed in the opposite direction parallel to the first one (Figure 1B and C). After four to five stitches the direction changes by 90 degrees to horizontal. Another 4 to 5 stitches are done in the same manner (Figure 1D), with the last one exiting near the starting point, for the closure knot. Thus, we created a two-dimensional net of threads to make a barrier between the anterior and posterior segment, with a grid spacing of 2–3 mm (Figure 1E). In all cases, the posterior segment was filled with 2000 centistoke silicone oil, Siluron 2000 (Fluoron GmbH, Ulm, Germany) (Figure 1F) and the anterior chamber was filled with balanced salt solution (BSS).
Description of Secondary Reconstruction Surgical Procedure Using an IOL and Artificial Iris
In the secondary reconstruction procedure, the silicone oil was removed by a standard 23G vitrectomy. After opening the conjunctiva, and incising a sclerocorneal tunnel of approximately 7 mm, scleral flaps were prepared in the 3 and 9 o’clock position, followed by removal of the silicone oil (Figure 1G, arrowhead) and the iris sutures (Figure 1H, arrowheads). In order to treat aphakia and aniridia simultaneously, we implanted an artificial intraocular lens in combination with an artificial iris:15 Although almost any commercially available artificial lens could be implanted, we decided to use a flexible acrylic IOL, the Aspira MC6125AS-Y IOL (HumanOptics AG, Erlangen, Germany), which is suitable for sewing and cutting due to the soft material, as well as a flexible ArtificialIris (AI) implant from HumanOptics. The surface of the prosthesis was individually handcrafted with colored silicone, based on a photographic documentation of the iris of the patients’ healthy fellow eye. The backside consisted of a smooth, opaque and black silicone layer. The artificial iris featured an overall diameter of 12.8 mm and a fixed pupil aperture of 3.35 mm and was individually trepanned to the required diameter. Two prophylactic iridectomies were added. The artificial iris was fixed with 10–0 polypropylene sutures to our standard IOL. The sutures went through the haptic close to the optic from the posterior direction; they were turned around on the front side to go back through the iris. A knot was placed on the posterior of the connected AI and IOL device. The suturing of the IOL to the AI takes about 2 minutes. To reduce the size of the combined iris and IOL implant and to keep the incision size as small as possible, the distal parts of the haptics were severed. The scleral-fixation sutures were then attached at the 3 and 9 o’clock position. We made sure to set the attachment points in opposite directions to achieve a centered pupil. The combined AI and IOL was then inserted as a folded “sandwich” through the tunnel. The implant was placed into the ciliary sulcus and fastened with 10–0 polypropylene sutures to the sclera. The combined artificial iris and intraocular lens were implanted through a sclerocorneal incision and sutured to the sclera at the 3 and 9 o’clock position (Figure 1I, asterisk). At the end of the surgery, the eye was filled with sterile air.
All main outcome measures were evaluated after the first as well as after the second surgery: morphological changes, subjective impairment from glare, subjective cosmetic disfigurement, patient satisfaction and intraocular pressure (IOP) measured by Goldmann applanation tonometry. Corrected distance visual acuity (CDVA) was a secondary outcome measurement. Postoperative refraction was determined using objective refractometry. The study was approved by the institutional review board and performed in accordance with the tenets of the Declaration of Helsinki.
The patients were asked to rate their sensitivity to glare and the discontent with their eye’s appearance on a 1 to 10 numerical scale, with 1 standing for low and 10 standing for high severity. This assessment was done after primary care and after secondary reconstruction. At the postoperative follow-up after secondary reconstruction surgery, patients were asked to additionally rate their overall satisfaction with the result on a similar numerical scale from 1 to 10, with 1 for very low satisfaction and 10 for maximum satisfaction. Patients were also asked if they would undergo the same procedure again if they had the choice.
Results
The iris sutures effectively prevented (Figure 2) migration of silicone oil to the anterior chamber in all seven patients receiving the temporary iris-diaphragm sutures for silicone oil barrier. Over time, pigment appeared to attach to the sutures (resembling seaweed on a fishing-net) (Figure 2B and D, arrowheads). We observed silicone oil emulsification in one case after primary care (Figure 2B, asterisk). In another eye, a fibrinous membrane developed between the suture-grid (Figure 2C, arrowheads).
Table 1 shows the patient characteristics and outcomes of the 4 patients who were included in this study. The mean time between the two surgical procedures was 11.3 months, ranging from 2 to 19 months. The mean follow-up time after secondary reconstruction surgery was 12.5 months, ranging from 5 to 23 months. Mean IOP was 11.75 ± 5.3 mmHg after primary care and 12.3 ± 3.8 mmHg after secondary reconstruction. Mean subjective impairment from glare was reduced from 7.7 ± 1.9 after the first surgery to 4.0 ± 2.5 after the second surgery. Mean subjective cosmetic disfigurement improved from 4.7 ± 3.9 after primary care to 2.25 ± 1.6 after secondary reconstruction. Mean overall satisfaction with the final result was 7.5 ± 1.8. All patients stated that they would undergo the same treatment again if they had the choice.
 |
Table 1 Patients Characteristics and Outcomes of the Four Patients Included in this Study |
Mean corrected distance visual acuity (CDVA) was 1.68 ± 0.78 logMAR after primary care and 1.37 ± 0.74 logMAR after secondary reconstruction surgery. The manifest refraction of each patient after secondary reconstruction is shown in Table 1.
Our two-step approach was successful in all patients (Figures 3–6). We did not meet any complications with the grid suture.
 |
Figure 6 Case 4: (A) shows a close up of the right eye after primary care surgery and (B) after secondary reconstruction. (C) shows binocular photographs after the first and (D) second surgery. |
Discussion
When dealing with severely traumatized eyes (where there is loss of lens and iris, and a need for silicone oil tamponade) the two-step approach is useful. In a first step, the globe is stabilized to minimize further complications, then a second intervention can be planned to achieve the best possible visual acuity and cosmetic result.
In primary care surgery, a final iris-lens-diaphragm to prevent the silicone oil from touching the endothelium is often not available. In contrast, the grid-iris-lens-diaphragm is quickly available, cheap, fast and easy to apply, removable and reversible. It does not require a large incision and thus may limit inflammation. The idea of using sutures to protect the endothelium is not new: retention sutures have been used in anterior segment surgery to prevent IOLs or tubing used in glaucoma surgery from touching the endothelium.16–19 When applied to eyes filled with silicone oil, the method makes use of the physical properties of the endotamponade and its interaction with the aqueous fluid. The oil/water interfacial tension, determined from theoretical models is assumed to be relatively high (50 erg/cm2), the gas/water interfacial tension is 70 erg/cm2 for comparison.20 This high interfacial tension in silicone oil’s contact with aqueous humor is the main principle that makes the sutures work as a barrier. It results from intermolecular forces and causes the silicone oil to maintain its integrity as a spheroidal shape in the eye.21 Ultrasound biomicroscopy imaging shows the convex shape of the silicone oil interacting with the retention sutures and the aqueous, illustrating the high interfacial tension.8 Thus, the use of high viscosity silicone oils is important in these cases, as the oil-water interfacial tension is a critical point. The sutures enhance the natural barrier that exists between the oil and the aqueous. The grid size and the surface properties of the sutures are important factors when using the grid barrier approach. As the sutures rely on an intact silicone oil/aqueous interface, this technique cannot be used in cases with an overfill of silicone oil and/or inadequate aqueous production. This implies that, at the end of the surgery, there must be aqueous left in the anterior chamber.8,22 It has been shown that retention sutures can effectively prevent contact between silicone oil and the corneal endothelium using different suturing techniques.8,12–14,23,24 This means, that the sutures can be placed differently from case to case, allowing the surgeon to react to special circumstances such as scleral thinning.25 Even preexisting sclerotomy wounds can be used as a base to create the retention sutures, allowing a needle-free approach.26 In our experience, a grid size of 2–3 mm is sufficient to prevent silicone oil migration into the anterior chamber and at the same time does not cause visual disturbances.
No patient complained about visual problems due to the sutures. It should be considered, however, that visual acuity was reduced due to aphakia, silicone oil filling and aniridia in all patients and that the sutures are only an intermediate stage before the final reconstruction.
Over time, we observed increasing amounts of pigment attached to the sutures. The origin of the pigment remains unclear as there is no pigmented iris tissue that could be a possible source of pigment. Although we did not observe any negative effects associated to the pigment deposition, it cannot be ruled out that it may have a negative impact on visual acuity or intraocular pressure.
We did not observe a significant amount of silicone oil in the anterior chamber in any patient. Small oil bubble emulsifications occurred in one case, but this is also described in reports on surgery with intact iris-lens-diaphragms. We could not link this to a defect in the retention sutures.27–29
We observed the formation of fibrinous membrane in one patient. This has also been previously observed in patients with silicone oil retention sutures and it has been suggested, that laser capsulotomy might be employed in cases where the membrane might occlude the optical axis.12
In total, sutures can prevent silicone-oil coming in contact with the corneal endothelium in cases of deficient iris-lens-diaphragm. It is an effective way of preventing contact of the silicone oil with the corneal endothelium for as long as the silicone tamponade is necessary. It is effective in temporary use but can also serve as a long-lasting option. In our patients, the sutures were left in place for 11.3 months on average. There is no medical reason to remove these sutures in the long term. This is of particular importance if the patient is satisfied with the result, if another surgery is considered too risky or if the patient is not willing to undergo an additional surgery – in any one of these scenarios the iris sutures can stay in place.
However, to achieve a better outcome cosmetically and functionally, it is possible to perform a second surgery. For secondary iris-lens-diaphragm implantation procedures various implant devices are available to choose from and their implantation is challenging. The most elaborated iris-lens-diaphragms take some time to manufacture and deliver. Therefore, they are seldom available for primary care surgery and a planned second surgery is needed. In this second step – when time has passed and the eye is stable – the final reconstruction can be planned as an elective surgery procedure.
There are several, ready-to-use implants:
(1) the closed silicone iris-diaphragm for permanent silicone-oil use (MICROSIL® DIAPHRAGM DP 4128 HumanOptics AG, Erlangen, Germany). The functional limitation of this device is its lack of a lens and it is also not aesthetically appealing. In cases with ocular hypotension, however, these implants can be used for sequestration and prevention of phthisis bulbi.11
(2) An alternative is the Morcher aniridia implant (Morcher GmbH, Stuttgart, Germany). It provides good functional results,9,30 but the iris reconstruction IOLs are only available in black color. Furthermore, the Morcher aniridia implants are made of non-flexible polyethylmethacrylate (PEMA) which is not be an ideal material for our technique, although individual suturing of a PEMA IOL onto the sclera can also be done.
(3) The Ophtec iris reconstruction lens (Ophtec BV, Groningen, The Netherlands) is made in a limited set of colors.10 Typically, the cosmetic result is not as aesthetically pleasing as the implant that we used, which is hand painted using a photograph which allows the artist to match the device color with the iris of the fellow eye. De Grande et al described a case similar to those described in this study in which the Ophtec iris reconstruction lens was used for secondary reconstruction after primary care including silicone oil retention sutures. In this case, the sutures were left in place and supported the sclera fixated IOL.31
(4) Other implants, like the open iris diaphragm used by Heimann et al6 and the closed iris diaphragm described by Thumann et al7 were made of PMMA and also sutured to the sulcus. Thumann et al observed greater effectivity of the closed iris diaphragm.7 Hermann et al found that the closed type of the iris diaphragm can help to prevent phthisis bulbi in cases of severely damaged eyes.32 Both types of iris diaphragm can prevent silicone-corneal contact in approximately 50% of the cases.7 The cosmetic results cannot be expected to be particularly good as the implants are transparent.
We decided to use the artificial iris from HumanOptics in combination with an IOL because we had previous good experience with this device. It is flexible, aesthetically appealing, and combinable with various IOLs. The AI implantation significantly reduces the pupillary aperture and can therefore reduce the sensitivity to glare and improve contrast sensitivity.33,34 It also provides excellent aesthetic results as it is customized to match the patient’s iris tissue and as a result patient satisfaction with the functional and cosmetic result is very high.33,35–37 An advantage of this device is the fact that any commercially available artificial lens can be sutured to the posterior side of the silicone-iris. This is convenient for simultaneous IOL and AI implantation in patients with aphakia and aniridia.
We made two peripheral iridectomies at the 6 and 12 o’clock positions to allow for repeated silicone oil tamponade if necessary in the future. It remains unclear if this combined, individually created iris-lens-diaphragm could effectively compartmentalize the eye and prevent silicone oil from entering the anterior chamber. However, in patient 3 and in two other cases – that were not part of this study – this kind of diaphragm proved to be an effective barrier for silicone oil. Szurman et al also used the AI successfully in a patient with silicone oil endotamponade to create an intact iris-lens-diaphragm.38
The two-step procedure we described allows one to achieve an individual, functional and aesthetically appealing result for the patient with traumatic injury (Figures 3D, 4D,5D, 6D).
Abbreviations
AI, artificial iris; IOL, intraocular lens; IOP, intraocular pressure; CDVA, corrected distance visual acuity; PMMA, polymethylmethacrylate.
Data Sharing Statement
The datasets used during the current study are available from Christian Mayer ([email protected]) on reasonable request.
Ethics Approval and Informed Consent
The study was approved by the local Ethics Committee (Fakultät für Medizin, Ethikkommission, Technische Universität München, IRB no. 535/15 S) and performed in accordance with the tenets of the Declaration of Helsinki.
Consent for Publication
Full written consent has been obtained from the patients. All patients were informed about the purpose of the study.
Acknowledgments
We would like to thank Mr. Donald J. Munro for review of this report. Christian S Mayer and Isabella Baur are co-first authors in this study.
Funding
The Department of Ophthalmology of the University of Heidelberg was supported by the Klaus Tschira Foundation.
Disclosure
CSM received travel grants and lecture fees from HumanOptics. IB, JS, AM and RK declare that they have no competing interests.
References
1. Azen SP, Scott IU, Flynn HW
2. Sternberg P, Hatchell DL, Foulks GN, Landers MB. The effect of silicone oil on the cornea. Arch Ophthalmol. 1985;103(1):90–94. doi:10.1001/archopht.1985.01050010096027
3. Federman JL, Schubert HD. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology. 1988;95(7):870–876. doi:10.1016/S0161-6420(88)33080-0
4. Ando F. Intraocular hypertension resulting from pupillary block by silicone oil. Am J Ophthalmol. 1985;99(1):87–88. doi:10.1016/S0002-9394(14)75878-7
5. Beekhuis W, Ando F, Zivojnović R, Mertens D, Peperkamp E. Basal iridectomy at 6 o’clock in the aphakic eye treated with silicone oil: prevention of keratopathy and secondary glaucoma. Br j Ophthalmol. 1987;71(3):197–200. doi:10.1136/bjo.71.3.197
6. Heimann K, Konen W. Artificial iris diaphragm and silicone oil surgery. Retina. 1992;12(3):S90–S94. doi:10.1097/00006982-199212031-00019
7. Thumann G, Kirchhof B, Bartz-Schmidt KU, et al. The artificial iris diaphragm for vitreoretinal silicone oil surgery. Retina. 1997;17(4):330–337. doi:10.1097/00006982-199707000-00009
8. Gentile RC, Eliott D. Silicone oil retention sutures in aphakic eyes with iris loss. Arch Ophthalmol. 2010;128(12):1596–1599. doi:10.1001/archophthalmol.2010.300
9. Phillips PM, Shamie N, Chen ES, Terry MA. Transscleral sulcus fixation of a small-diameter iris-diaphragm intraocular lens in combined penetrating keratoplasty and cataract extraction for correction of traumatic cataract, aniridia, and corneal scarring. J Cataract Refract Surg. 2008;34(12):2170–2173. doi:10.1016/j.jcrs.2008.06.048
10. Miller AR, Olson MD, Miller KM. Functional and cosmetic outcomes of combined penetrating keratoplasty and iris reconstruction lens implantation in eyes with a history of trauma. J Cataract Refract Surg. 2007;33(5):808–814. doi:10.1016/j.jcrs.2007.01.018
11. Kirchhof B. Prophylaxe der Silikonkeratopathie durch die Implantation eines Irisdiaphragmas. Ophthalmo-Chirurgie. 2017;29:159–162.
12. Wong R, Lee E, Shunmugam M. Novel technique for silicone oil retention suture with secondary auto capsulotomy of fibrin membrane. Eye. 2013;27(2):280–281. doi:10.1038/eye.2012.266
13. Du W, Chen F, Zhu J, Xie Z. Application of modified silicone oil retention sutures in traumatic aphakic eyes with iris loss. Retina. 2020.
14. Barak Y, Gambrell JD, Tezel TH. Modification of silicone oil retention sutures in aphakic eyes with iris loss. Arch Ophthalmol. 2012;130(9):1231–1232. doi:10.1001/archophthalmol.2012.1211
15. Mayer C, Tandogan T, Hoffmann AE, Khoramnia R. Artificial iris implantation in various iris defects and lens conditions. J Cataract Refract Surg. 2017;43(6):724–731. doi:10.1016/j.jcrs.2017.06.003
16. Freedman J. Management of the Molteno silicone tube in corneal transplant surgery. Ophthalmic Surg Lasers Imaging Retina. 1998;29(5):432–434.
17. Wilson RP, Moster MR. The chamber-retaining suture revisited. Ophthalmic Surg Lasers Imaging Retina. 1990;21(9):625–627.
18. Simcoe CW. Retaining devices for protection of corneal endothelium. J Am Intraocul Implant Soc. 1979;5(3):234–236. doi:10.1016/S0146-2776(79)80124-X
19. Seo M-S, Nah H-J, Yang K-J, Park Y-G. Triangular transchamber suture. J Cataract Refract Surg. 2001;27(1):172–173. doi:10.1016/S0886-3350(00)00650-7
20. de Juan E
21. Petersen J. The physical and surgical aspects of silicone oil in the vitreous cavity. Graefe’s Arch Clin Exp Ophthalmol. 1987;225(6):452–456. doi:10.1007/BF02334175
22. Yüksel K, Pekel G, Alagöz N, Alagöz C, Baz Ö, Yazc AT. Silicone oil barrier sutures in aphakic eyes with iris defects. Retina. 2016;36(6):1222–1226. doi:10.1097/IAE.0000000000000856
23. Rao RC, Cohen SR, Mian SI. Silicone oil retention sutures for retinal detachment repair following traumatic aniridia, aphakia, and ruptured globe. JAMA Ophthalmol. 2015;133(9):e151433–e151433. doi:10.1001/jamaophthalmol.2015.1433
24. Gurmizov E. Retention sutures in traumatic retinal detachment surgery complicated by absence of an irido-lenticular diaphragm. Ophthalmol Russia. 2014;9(2):22–23.
25. Gentile RC, Eliott D. Modification of silicone oil retention sutures in aphakic eyes with iris loss—reply. Arch Ophthalmol. 2012;130(9):1231–1232. doi:10.1001/archophthalmol.2012.1616
26. Syed R, Jusufbegovic D, Schaal S, Needle-Free Minimally A. Invasive Surgical Technique for the placement of silicone oil retention sutures. Retina. 2016;36(5):1032–1034. doi:10.1097/IAE.0000000000000984
27. Toklu Y, Cakmak HB, Ergun SB, Yorgun MA, Simsek S. Time course of silicone oil emulsification. Retina. 2012;32(10):2039–2044. doi:10.1097/IAE.0b013e3182561f98
28. Light DJ. Silicone oil emulsification in the anterior chamber after vitreoretinal surgery. Optometry J Am Optometric Assoc. 2006;77(9):446–449. doi:10.1016/j.optm.2006.04.119
29. Valone J
30. Mashor RS, Bahar I, Kaiserman I, Berg AL, Slomovic A, Rootman DS. Combined penetrating keratoplasty and implantation of iris prosthesis intraocular lenses after ocular trauma. J Cataract Refract Surg. 2011;37(3):582–587. doi:10.1016/j.jcrs.2010.10.038
31. De Grande V, Rosenthal K, Reibaldi M, Gentile RC. Artificial iris–intraocular lens implantation for traumatic aniridia and aphakia assisted by silicone oil retention sutures. J Cataract Refract Surg. 2012;38(11):2045–2048. doi:10.1016/j.jcrs.2012.08.043
32. Hermann MM, Muether PS, Kuhn L, Kirchhof B, Fauser S. Clinical outcome of the artificial iris diaphragm in silicone oil surgery. Br j Ophthalmol. 2012;96(7):1008–1011. doi:10.1136/bjophthalmol-2011-300983
33. Mayer CS, Reznicek L, Hoffmann AE. Pupillary reconstruction and outcome after artificial iris implantation. Ophthalmology. 2016;123(5):1011–1018. doi:10.1016/j.ophtha.2016.01.026
34. Bonnet C, Miller KM. Safety and efficacy of custom foldable silicone artificial iris implantation: prospective compassionate-use case series. J Cataract Refract Surg. 2020;46(6):893–901.
35. Mayer CS, Hoffmann AM, Prahs P, Reznicek L, Khoramnia R. Functional outcomes after combined iris and intraocular lens implantation in various iris and lens defects. BMC Ophthalmol. 2020;20(1):1–7. doi:10.1186/s12886-020-01621-8
36. Mayer C, Son H-S, Labuz G, Yildirim TM, Auffarth GU, Khoramnia R. In vitro optical quality assessment of a monofocal IOL sutured to an artificial iris. J Cataract Refract Surg. 2020;46(8):1184–1188. doi:10.1097/j.jcrs.0000000000000287
37. Yildirim TM, Khoramnia R, Masyk M, Son H-S, Auffarth GU, Mayer CS. Aesthetics of iris reconstruction with a custom-made artificial iris prosthesis. PLoS One. 2020;15(8):e0237616. doi:10.1371/journal.pone.0237616
38. Szurman P, Jaissle G. Artificial iris. Der Ophthalmologe. 2011;108(8):720. doi:10.1007/s00347-011-2367-0
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.