Back to Journals » Open Access Emergency Medicine » Volume 13
Successful Application of Extracorporeal Membrane Oxygenation in an Acute Tonsillitis Patient Complicated with Acute Respiratory Distress Syndrome: A Case Report
Received 3 September 2021
Accepted for publication 2 November 2021
Published 18 November 2021 Volume 2021:13 Pages 499—502
DOI https://doi.org/10.2147/OAEM.S337568
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Hans-Christoph Pape
Zhufeng Zhang,1 Dongmei Guo,2 Qi Ren3
1Emergency Department of Sandun District of Zhejiang Hospital, Hangzhou, Zhejiang, People’s Republic of China; 2Radiology Department of Sandun District of Zhejiang Hospital, Hangzhou, Zhejiang, People’s Republic of China; 3Qi Ren Intensive Care Unit of Sandun District of Zhejiang Hospital, Hangzhou, Zhejiang, People’s Republic of China
Correspondence: Qi Ren
Intensive Care Unit of Sandun District of Zhejiang Hospital, 1229th Gudun Road, Xihu District, Hangzhou, Zhejiang, 310030, People’s Republic of China
Tel +86-18600754832
Email [email protected]
Abstract: Cases of acute tonsillitis, a common disease in the emergency department, are mostly mild and those complicated by severe pneumonia and acute respiratory distress syndrome are rarely reported.
Keywords: acute tonsillitis, severe pneumonia, acute respiratory distress syndrome, extracorporeal membrane oxygenation, case report
Introduction
A large number of patients with acute tonsillitis will present to the emergency department (ED), and most incidents of the disease occur in school-age children; however, people of any age can be affected.1 The majority of acute tonsillitis cases are considered to be mild and self-limiting.2 Here, we describe an adult patient of acute tonsillitis complicated with severe pneumonia and acute respiratory distress syndrome (ARDS).
Case Presentation
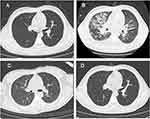
On March 19th, 2020, a 30-year-old man was admitted to the ED as “acute tonsillitis” with fever and pain in the left neck. Four days before admission, the case had no obvious cause of pain in the left neck, accompanied by fever (maximum temperature 40.2°C) and chills. The symptoms did not significantly relieve after taking ibuprofen and amoxicillin. The patient had a free previous medical history. The patient, at the time of admission, had obvious pharyngeal congestion, enlarged tonsil and enlarged lymph nodes with tenderness on both side of the neck; the lung auscultation breath sound was clear, and no obvious dry and wet rales were heard; the patient’s temperature was 39.5°C, heart rate was 118 beats/min, respiratory rate was 20 breaths/min, with blood pressure 113/77 mm Hg; the laboratory examination showed that the percentage of neutrophils (NE%) was 84.0%, white blood cell count (WBC) was 12.0×109/L and hypersensitive C-reactive protein (Hs-CRP) was 236.85 mg/L; the result of chest CT was normal (Figure 1A). The CURB-65 score was 0 and clear consciousness and moderate spirit was recorded. The patient was ordered moxifloxacin for anti-infection. The blood culture results completed at the time of admission showed that the patient was infected with gram-positive cocci.
On March 21st, the patient complained of dyspnea, palpitation and shortness of breath. The effect was not good after increasing the oxygen flow, and the SpO2 decreased to 84%. Chest CT showed: the progress was faster than that when admitted on day 1, multiple ground glass opacity in both lungs, and a small amount of pleural effusion on both sides and pericardial effusion (Figure 1B). After completing CT examination, the patient returned to the ward and his blood pressure (BP) decreased and fluctuated between 74–88/45–62mm Hg. Norepinephrine was given rapidly to maintain his BP. The patient was undergoing a critical condition and the CURB-65 score was 3 at the same time. The usage of fraction of inspiration O2 (FiO2) was 100%, however the oxygenation was still difficult to maintain; PaCO2 was 52.8mm Hg and respiratory distress symptoms were obvious. Considering the patient complicated with severe pneumonia, ARDS, respiratory failure and shock symptoms of hemodynamic instability, we prescribed to pump norepinephrine with 0.1 μg/kg/min, meanwhile, venovenous ECMO adjuvant treatment was given with the setting as centrifugal pump speed at 3775 rpm, blood flow about 5.0L/min and oxygen flow as 15L/min with FiO2 100%. After 30 minutes of ECMO combined with ventilator, the vital signs of the patient gradually stabilized with HR 110 beats/min, RR 25 breaths/min, BP122/73mm Hg and SpO2 98–100%.
On March 27th, the patient self-reported a normal status, with a FiO2 of 35%, BP 128/71mm Hg, SpO2 100%, HR 78 beats/min and RR 16 breaths/min. Consulting the result of chest CT re-examination (Figure 1C), ECMO was removed since the condition had an obvious improvement on March 28th. The patient was transferred to the general ward of the respiratory department, and discharged after 3 days’ observation. One month after discharge, the chest CT re-examination of the patient showed normal (Figure 1D).
Discussion
ARDS is a kind of acute pulmonary edema induced by non-cardiogenic factors, which is characterized by respiratory distress and refractory hypoxemia.3 It is often secondary to severe pneumonia and its related infectious shock, and the mortality rate can be high.4 For ARDS patients with respiratory failure, hemodynamic uncertainty and other shock manifestations due to severe acute tonsillitis, ECMO should be used as early as possible when conventional ventilator-assisted breathing is ineffective.5 Based on avoiding hyperoxia and ventilator-associated lung injury, ECMO can improve hypoxemia as soon as possible, correct respiratory failure, stabilize circulation and ensure organ perfusion for patients with acute tonsillitis.
The patient was stable at the time when he was admitted to hospital, but his condition progressed into critically ill rapidly. The patient’s blood routine examination after antibiotic treatment on day 1 of admission showed a trend of continuous deterioration; cooling treatment and antibiotics treatment were also ineffective. Since the patient had an infectious disease, we had to pay close attention to changes in his condition, increase the frequency of inspection, understand the changes in his condition, and pay more attention to his response to treatment on a timely basis.6
Patients with severe pneumonia, ARDS, or other multiple organ failure, should be cared for with a targeted implementation, individualized nursing care and timely dynamic assessment of the condition.7 In this case, the ventilator-assisted breathing could not relieve the symptoms of dyspnea with unstable hemodynamics, and the drug maintenance effect was unhelpful. The opportunity to take the ventilator-assisted breathing and ECMO combined treatment scheme immediately was necessarily estimated between the cooperation of doctors and nurses. For the patient, we paid attention to humanistic care in the process of nursing treatment, carried out effective psychological communication and established a good nurse–patient relationship.8 When the patient’s condition changes, we should fully inform their family, especially the possible causes of the disease changes and the advantages and disadvantages of the treatment plan, so that the patient and his family can actively cooperate with the treatment plan and strive for the best treatment opportunity for the patient’s recovery.
We make full use of the advantages of multidisciplinary cooperation, follow the principle of gradual and individualized treatment, and work together with the rehabilitation department to develop an individualized exercise plan that is from passive to active, from weak to strong, from short to long, and improve the exercise time and intensity in the case that patients can tolerate.9 During the combined treatment of ventilator-assisted breathing and ECMO, the nurses gave the patients passive movement in bed and guided the patient’s active movement when their condition was stable.10 After ECMO was withdrawn on March 27th, rehabilitation professionals formulated a rehabilitation nursing plan suitable for the patient in bed. On March 28th, after the ventilator-assisted breathing was withdrawn, active and passive rehabilitation nursing at the bedside was carried out as soon as the patient’s body permitted, so as to promote the recovery of his various functions.11 No venous thrombosis occurred in this patient.
Conclusions
This was an acute tonsillitis patient complicated with severe pneumonia and ARDS in an emergency department. as the disease rapidly progressed, the patient was treated by endotracheal intubation and ECMO. Close nursing to observe the condition and active monitoring should be considered when acute tonsillitis patients suffer complications, which may reveal effective therapy for the patients in a timely manner and prevent progression to severe status.
Data Sharing Statement
Data sharing not applicable – no new data generated.
Ethical Approval
This present case report was approved by the institutional ethics board of Zhejiang Hospital. A written informed consent to publish the medical details and images had been signed by the patient.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sidell D, Shapiro NL. Acute tonsillitis. Infect Disord Drug Targets. 2012;12(4):271–276. doi:10.2174/187152612801319230
2. Bird JH, Biggs TC, King EV. Controversies in the management of acute tonsillitis: an evidence-based review. Clin Otolaryngol. 2014;39(6):368–374. doi:10.1111/coa.12299
3. Thompson BT, Chambers RC, Liu KD. Acute respiratory distress syndrome. N Engl J Med. 2017;377(19):1904–1905. doi:10.1056/NEJMc1711824
4. Sarda C, Palma P, Rello J. Severe influenza: overview in critically ill patients. Curr Opin Crit Care. 2019;25(5):449–457. doi:10.1097/MCC.0000000000000638
5. Menk M, Estenssoro E, Sahetya SK, et al. Current and evolving standards of care for patients with ARDS. Intensive Care Med. 2020;46(12):2157–2167. doi:10.1007/s00134-020-06299-6
6. Swol J, Belohlávek J, Brodie D, et al. Extracorporeal life support in the emergency department: a narrative review for the emergency physician. Resuscitation. 2018;133:108–117. doi:10.1016/j.resuscitation.2018.10.014
7. Bruni A, Garofalo E, Grande L, et al. Nursing issues in enteral nutrition during prone position in critically ill patients: a systematic review of the literature. Intensive Crit Care Nurs. 2020;60:102899. doi:10.1016/j.iccn.2020.102899
8. Penconek T, Tate K, Bernardes A, et al. Determinants of nurse manager job satisfaction: a systematic review. Int J Nurs Stud. 2021;118:103906. doi:10.1016/j.ijnurstu.2021.103906
9. Salna M, Abrams D, Brodie D. Physical rehabilitation in the awake patient receiving extracorporeal circulatory or gas exchange support. Ann Transl Med. 2020;8(13):834. doi:10.21037/atm.2020.03.151
10. Zwischenberger JB, Pitcher HT. Extracorporeal membrane oxygenation management: techniques to liberate from extracorporeal membrane oxygenation and manage post-intensive care unit issues. Crit Care Clin. 2017;33(4):843–853. doi:10.1016/j.ccc.2017.06.006
11. Rocha G, Soares P, Gonçalves A, et al. Respiratory care for the ventilated neonate. Can Respir J. 2018;2018:7472964. doi:10.1155/2018/4923062
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.