Back to Journals » International Medical Case Reports Journal » Volume 12
Subcutaneous sparganosis mimicking soft tissue tumor: a case report
Authors Hwang JM , Hwang DS, Kang C , Lee JW
Received 30 October 2018
Accepted for publication 16 January 2019
Published 19 February 2019 Volume 2019:12 Pages 47—50
DOI https://doi.org/10.2147/IMCRJ.S192764
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas

Jung-Mo Hwang, Deuk-Soo Hwang, Chan Kang, Jae-Won Lee
Department of Orthopaedic Surgery, Chungnam National University Hospital, Daejeon, South Korea
Background: Sparganosis is a rare parasitic disease of humans caused by invasion of human tissue by plerocercoid tapeworm larvae (spargana) of the genus Spirometra species. This parasite commonly invades subcutaneous tissue but can appear in any tissue of the body.
Case presentation: Here, we report a case of a 33-year-old woman presented with a migrating painful swelling and erythema in right thigh for 6 months, which was initially misdiagnosed as soft tissue tumor. Magnetic resonance imaging revealed a multiple elongated tubular tracts in the medial aspect of right thigh, from which a long, wrinkled, whitish worm was surgically removed. The parasite was histopathologically identified as Spirometra mansoni.
Conclusion: Sparganosis is rare and physicians have little experience, so if suspected, should be included among the list of differential diagnosis and special serological test should be recommended before surgery.
Keywords: Spirometra mansoni, sparganosis, subcutaneous, thigh
Introduction
Sparganosis is a rare parasitic disease of humans caused by invasion of human tissue by plerocercoid tapeworm larvae (spargana) of the genus Spirometra species. The human is an accidental transport host. Although in humans sparganosis is usually observed as a subcutaneous nodules somewhere on the body, it is less frequently observed as an internal infection of the intestines, breast tissue, eyes, spinal cord, and rarely, the peritoneopleural cavity.1 We report a case of subcutaneous sparganosis in the thigh that was initially misdiagnosed as soft tissue tumor. Since this infection is rare and physicians have little experience of sparganosis, the diagnosis is still frequently confused with other diseases until the worm is confirmed from the mass lesion.
Case presentation
A 33-year-old woman presented with a migrating painful swelling and erythema in the medial aspect of right thigh for 6 months, which had recently grown in size. She was referred to our hospital with suspected soft tissue tumor from the private clinic. She had previously noticed a small migrating mass in the right thigh area some 20 years previously, but she ignored as the condition was asymptomatic. The pain was intermittent and worsened after a long period of walking but improved with resting. She had no history of leg trauma and denied ingesting raw snake or frog. But she lived in China in childhood, and sometimes drank spring water from the mountain.
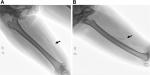
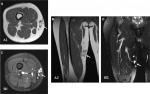
Physical examination revealed swelling, tendernes, and erythema, but local heatness was not found in the medial aspect of right thigh. Routine laboratory examination revealed no abnormal findings, and no leukocytosis and no eosinophilia was detected in the peripheral blood. Plain radiographs of the right femur showed multiple irregular radiopaque densities (Figure 1). Magnetic resonance imaging (MRI) showed multiple elongated tubular tracts in subcutaneous tissue of thigh. Lesions showed low signal intensity on T1-weighted images, and high signal intensity on T2-weighted images (Figure 2).
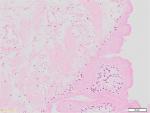
Special laboratory investigations and ultrasonographic examination were not performed, because the patient decided to undergo surgery rapidly to clarify the etiology of the tumorous lesion and we did not suspect spargana infection. Under the clinical impression of soft tissue tumor, total surgical excision was performed. A long, wrinkled, whitish worm ~24 cm in length and 3 mm in width was removed (Figure 3). The parasite was histopathologically identified as Spirometra mansoni (Figure 4).
  | Figure 3 (A and B) Total surgical excision was performed. Notes: A long, wrinkled, whitish worm ~24 cm in length and 3 mm in width was removed from the medial aspect of right thigh. |
She was concerned about whether another worm was still living in her body after the surgery. Therefore, we measured the anti-sparganum IgG antibody using a microplate ELISA using the peripheral blood at 6 months after surgery without oral treatment for the parasite. The serum titer of the anti-sparganum IgG antibody revealed within normal range (0.18, reference range 0–0.99) and no recurrence was noticed in 12 months follow-up.
Discussion
Sparganosis is a rare parasitic disease of humans caused by invasion of human tissue by plerocercoid tapeworm larvae (spargana) of the genus Spirometra species. Sparganosis is found worldwide, however, the majority of cases occur in East Asia, including Korea.1 The routes of spargana infection involve either drinking water contaminated with plerocercoid-infected copepods or consumption of undercooked meat of plerocercoid-infected snakes or frogs. Additionally, infection can occur by placement of poultices that use the skin of infected snakes or frogs.2 After ingestion, the spargana migrate to the subcutaneous tissues, where they become encapsulated in inflammatory nodules that can develop into abscesses. These abscesses can occur anywhere in the body, as spargana have the ability to migrate to any tissues and organs, such as subcutaneous connective tissue, muscle, breast, lungs, and the central nervous system.3 The parasite can live for up to 30 years inside their host, and their length can vary from a few millimeters to a few centimeters. In discussing the risk of acquiring an infection in this case, she had no history of leg trauma and denied ingesting raw snake or frog. But she drank spring water from the mountain in childhood, it is possible that she became infected by ingesting plerocercoid larvae because there were no other causes.
Sparganosis may be diagnosed by clinical symptoms and habit of eating the raw, but the definite diagnosis is only made by detecting the larvae in an operative field, which is definitive treatment modality. In some cases of subcutaneous sparganosis, however, imaging techniques have provided useful information before surgery. Plain radiographs showed calcification in a few cases.4 Ultrasonography showed hyperechoic, hypoechoic, and anechoic lesions with internal serpinginous tubular structures and elongated hyperechoic masses with hypoechoic signals in the central portion.5 MRI showed low-signal, bundle-like structures and high-signal structures on T1- and T2-weighted images, respectively.6 Thus, imaging techniques may provide diagnostic hints, but these methods do not allow a definitive diagnosis and leave a broad range of differential diagnoses to be considered, including infections with other metacestodes and soft tissue tumors. In case of worm necrosis or impossible extirpation, it is difficult to make a pathological diagnosis. In such cases, the serological diagnosis may be effective. The ELISA can be effectively used in that it shows the elevation of the anti-sparganum IgG antibody titer, and the detection of declining anti-sparganum IgG antibody titer after removal of the larvae to confirm a complete resection has also been shown.7
Retrospective investigation of images for our patient revealed similar findings mentioned above. The plain radiograph revealed multiple irregular soft tissue calcifications. On MRI, bundle-like structures, whose signal was low on T1-weighted images and high on T2-weighted images surrounded by an unclear marginal mass, was observed. This finding is a relatively nonspecific signal feature. But morphologically, it is just characteristic finding of sparganosis. Special serological test for diagnosis was not carried out in our patient before surgery, since parasitic infection was not suspected. But we measured the anti-sparganum IgG antibody using a microplate ELISA at 6 months after surgery and the serum titer of anti-sparganum IgG antibody revealed within normal range and no recurrence was noticed.
On the basis of our experience with this case, we concluded that subcutaneous sparganosis mimicked a soft tissue tumor in terms of clinical manifestations and radiological findings.
Conclusion
Sparganosis is rare and physicians have little experience, so if suspected, should be included among the list of differential diagnosis and special serological test should be recommended before surgery.
Ethics approval and consent to participate
We informed the patient this study in advance. We collected clinical and medical data under patient’s consent. The patient was aware that her result and images would be used in the study and subsequent publications. Ethics approval for this study was obtained from the Chungnam National University Hospital Ethics Committee (IRB No. 2017-08-009).
Data sharing statement
The datasets supporting the conclusions of this article are included within the article and its additional files.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that there are no potential conflict of interest relevant to this article.
References
Cho SY, Bae JH, Seo BS. Some aspects of human sparganosis in Korea. Korean J Parasitol. 1975;13(1):60–77. | ||
Griffin MP, Tompkins KJ, Ryan MT. Cutaneous sparganosis. Am J Dermatopathol. 1996;18(1):70–72. | ||
Liu Q, Li MW, Wang ZD, Zhao GH, Zhu XQ. Human sparganosis, a neglected food borne zoonosis. Lancet Infect Dis. 2015;15(10):1226–1235. | ||
Cho JH, Lee KB, Yong TS, et al. Subcutaneous and musculoskeletal sparganosis: imaging characteristics and pathologic correlation. Skeletal Radiol. 2000;29(7):402–408. | ||
Park JH, Chai JW, Cho N, et al. A surgically confirmed case of breast sparganosis showing characteristic mammography and ultrasonography findings. Korean J Parasitol. 2006;44(2):151–156. | ||
Sarukawa S, Kawanabe T, Yagasaki A, Shimizu A, Shimada S. Case of subcutaneous sparganosis: use of imaging in definitive preoperative diagnosis. J Dermatol. 2007;34(9):654–657. | ||
Kim H, Kim SI, Cho SY. Serological diagnosis of human sparganosis by means of micro-ELISA. Korean J Parasitol. 1984;22(2):222–228. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.