Back to Journals » Drug Design, Development and Therapy » Volume 13
Subcutaneous bortezomib might be standard of care for patients with multiple myeloma: a systematic review and meta-analysis
Authors Ye Z , Chen J , Xuan Z, Yang W, Chen J
Received 13 December 2018
Accepted for publication 3 April 2019
Published 16 May 2019 Volume 2019:13 Pages 1707—1716
DOI https://doi.org/10.2147/DDDT.S198117
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Qiongyu Guo
Ziqi Ye,1,* Jie Chen,2,* Zixue Xuan,3 Wenchao Yang,4 Jing Chen5
1Department of Pharmacy, the First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, People’s Republic of China; 2Department of Pharmacy, the Second Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, People’s Republic of China; 3Department of Pharmacy, Zhejiang Provincial People’s Hospital, Hangzhou, People’s Republic of China; 4Department of Pharmacy, Traditional Chinese Medical Hospital of Zhuji, Zhuji, People’s Republic of China; 5Department of Medical Oncology, the First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Background: Administration of subcutaneous (SC) bortezomib in patients with multiple myeloma (MM) has increased in recent years. Yet, it is unclear whether there is sufficient evidence to support the use of SC bortezomib as a standard of care.
Methods: A systematic review of 4 randomized controlled trials and 8 retrospective trials comparing SC to intravenous (IV) bortezomib among 1,857 MM patients was performed. Embase, PubMed, Clinical Trials.gov, Cochrane Library and reference lists were searched for relevant studies from inception until August 2018. Outcomes of interest included 1-year overall survival (OS), 1-year progression-free survival (PFS), objective response rate (ORR) and adverse events (AEs). Random events meta-analyses were performed. We also performed sensitivity analysis to examine whether the results of the meta-analysis were robust.
Results: Compared to IV administration, SC bortezomib had a significantly lower incidence of some all-grade or grade 3–4 AE, such as peripheral sensory neuropathy, leukopenia and thrombocytopenia (p<0.05). There was no statistical difference in 1-year OS, 1-year PFS, ORR between SC and IV bortezomib (p>0.05).
Conclusion: The data presented so far consistently show that SC bortezomib has become a standard of care for patients with MM.
Keywords: subcutaneous bortezomib, intravenous bortezomib, multiple myeloma, efficacy, adverse events, systematic review
Introduction
Multiple myeloma (MM) is characterized by the neoplastic proliferation of plasma cells producing a monoclonal immunoglobulin. MM accounts for approximately 1–2% of all cancers and slightly more than 17% of hematologic malignancies in the United States.1 Worldwide, there are approximately 154,000 cases and 101,000 deaths per year attributed to MM.2 Proteasome inhibitor bortezomib-based treatment has been used in both newly diagnosed MM3 and relapsed or refractory MM4 and elicited a high response rate. Despite their widespread use, adverse events (AEs) (eg, peripheral neuropathy) are common and there are still questions concerning their optimal regimen.
Initially, bortezomib is administered through intravenous (IV) infusion from the time of diagnosis of MM until patients are eligible for autologous hematopoietic cell transplantation.5 This administration route was compared to the subcutaneous (SC) bortezomib in studies performed on patients with MM. Given the concerns regarding the toxicity of bortezomib, there has been increasing interest from oncologists and patients in finding the optimal administration route.
A previous meta-analysis showed that a number of studies have investigated the efficacy and safety of SC bortezomib administered through IV administration route, but some studies are only abstract, with the outcomes of efficacy being only in objective response rate (ORR). Also, one trial included6 was different from the other trials (in one trial the SC bortezomib was administered once a week, but the others were twice a week); these might affect the final results.7 As there is now more data available, a systematic review and meta-analysis were performed in order to assess whether or not the SC administration route of bortezomib should be considered as a standard of care in patients with MM.
Methods
Search strategy
To obtain the studies that compared SC and IV bortezomib, we conducted a comprehensive literature search on Embase, PubMed, the Clinicaltrials.gov (
Inclusion criteria and exclusion criteria
Studies were selected according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.8 Clinical trials that met the following criteria were included as follows:
(1) Randomized phaseⅡ, Ⅲ, and Ⅳ trials
(2) Patients with MM (newly diagnosed, relapsed, or refractory)
(3) Participants who received SC bortezomib compared to IV bortezomib
(4) Events and event rates and sample sizes available for drug efficacy and safety
Exclusion criteria were as follows: (1) animal research; (2) reviews; (3) only have abstracts; (4) overlapping data; (5) studies without risk ratio (RR), OR or HR with 95% CIs.
Data extraction and quality assessment
Two reviewers independently conducted the literature screening, data extraction and quality assessment of the trials. A third reviewer intervened when reviewers disagreed until a consensus was reached. We extracted the following information from each article: first author’s name, year of publication, study type, disease type, the number of patients, trial phase, treatment and control arms, the number of patients with 1-year overall survival (OS), 1-year progression-free survival (PFS), ORR and AEs. If the studies did not provide the 1-year OS or PFS data, we estimated those values from the Kaplan–Meier curve by using Engauge Digitizer software. The quality of the methodology in prospective trials was assessed by the Jadad criteria.9 The quality of each trial was graded, with high-quality trials (score ≥3) and low-quality trials (score ≤2). The Newcastle–Ottawa Scale criteria (
Statistical analysis
Data of patients with 1-year OS, 1-year PFS, ORR and AEs were extracted from all of the included trials. RR and 95%CI were calculated to assess the association strength of these two regimens with outcomes. The Q statistic and I2 statistic were used to assess the heterogeneity. I2>50% indicated statistically significant heterogeneity. The random-effect model was used in these meta-analyses for conservative statistics. A funnel plot was used to assess the publication bias. We also performed sensitivity analysis to examine whether the results of the meta-analysis were robust. Begg adjusted rank correlation test10 and Egger regression test.11 A statistical test with a p<0.05 was considered significant. STATA statistical version 12.0 was used to perform all the statistical analyses (Stata Corporation, College Station, Texas, USA). All p-values were two-sided.
Results
Characteristics of studies included in this study
Our search yielded a total of 1,187 potentially relevant clinical trials on SC or IV administration of bortezomib in patients with MM. After reviewing and screening, 12 primary studies, which included 1,857 subjects, met our inclusion criteria12-22 and were pooled for the meta-analyses (Figure 1). The baseline characteristics of each trial are shown in Table 1; 4 RCTs and 8 retrospective trials were included. All trials included were open label. The number of enrolled patients ranged from 24 to 584. The quality of the included RCTs (Jadad scores) ranged from 2 to 3 and retrospective trials (NOS scores) ranged from 7 to 8 stars. According to the eligibility criteria of the majority of the trials, patients with impaired hepatic, renal or bone marrow function were excluded and most of the patients had Eastern Cooperative Oncology Group performance-status scores of 0 or 1. This systematic review followed the guidelines of the PRISMA statement.
 | Table 1 Characteristics of all studies |
 | Figure 1 Flow chart for eligible studies. Abbreviations: SC, subcutaneous injection; IV, intravenous infusion; MM, multiple myeloma. |
Findings: 1-year OS, 1-year PFS and ORR
A total of 771 subjects who were treated with SC or IV bortezomib in 5 trials were used for the analysis of 1-year OS. Data from the 1-year OS between SC bortezomib and IV bortezomib arms produced a summary RR of 1.02 (95%CI: 0.95, 1.09, I2=0%) (Figure 2A). The results showed no statistical difference in 1-year OS between SC and IV bortezomib (p=0.617).
A total of 670 subjects who were treated with SC or IV bortezomib in 4 trials were used for the analysis of 1-year PFS. Data from 1-year PFS between SC bortezomib and IV bortezomib arms produced a summary RR of 1.00 (95%CI: 0.88, 1.13, I2=0%) (Figure 2B). The results showed no statistical difference in 1-year PFS between SC and IV bortezomib (p=0.967).
A total of 1,635 subjects treated with SC or IV bortezomib in 11 trials were used for the analysis of ORR. Data for ORR between SC bortezomib and IV bortezomib arms produced a summary RR of 0.99 (95%CI: 0.95, 1.03, I2=0%) (Figure 2C). The results showed no statistical difference in ORR between SC and IV bortezomib (p=0.676).
Findings: adverse events
A number of different AEs and toxicities were reported. In the meta-analysis, patients treated with SC or IV bortezomib from 10 studies were included for analysis of all-grade or grade 3–4 AEs. As shown in Table 2, the overall RR of all-grade peripheral sensory neuropathy, leukopenia, asthenia, fatigue, infection, hepatobiliary disorders and thrombocytopenia between SC and IV bortezomib arms were 0.72 (95% CI: 0.62, 0.84, I2=13.8%), 0.77 (95% CI: 0.60, 0.99, I2=68.3%), 0.85 (95% CI: 0.72, 1.00, I2=0%), 0.65 (95% CI: 0.51, 0.83, I2=27.1%), 0.64 (95% CI: 0.46, 0.89, I2=0%), 0.53 (95% CI: 0.35, 0.81, I2=0%), and 0.68 (95% CI: 0.50, 0.94, I2=70.3%). The overall RR of grade 3–4 peripheral sensory neuropathy, diarrhea, leukopenia, constipation, fatigue, neuralgia and thrombocytopenia between SC and IV bortezomib arms were 0.36 (95% CI: 0.25, 0.52, I2=0%), 0.37 (95% CI: 0.20, 0.72, I2=0%), 0.41 (95% CI: 0.28, 0.62, I2=10.1%), 0.27 (95% CI: 0.10, 0.73, I2=0%), 0.45 (95% CI: 0.23, 0.85, I2=0%), 0.36 (95% CI: 0.13, 0.97, I2=0%), and 0.59 (95% CI: 0.38, 0.92, I2=60.8%). The results showed that SC bortezomib had a significant lower incidence of the above all-grade and grade 3–4 AEs compared to IV administration of bortezomib (p<0.05). Even so, the results showed no statistical difference from other related all-grade and grade 3–4 AEs listed in Table 2 between SC and IV bortezomib arms (p>0.05).
 | Table 2 Meta-analysis results of the associations between bortezomib treatment and adverse events in MM patients |
Sensitivity analysis
The results showed that no particular study affected the overall significance of the pooled estimates, and the results of the meta-analysis were robust (Figure 3).
 | Figure 3 Sensitivity analysis of all clinical trials included. |
Publication bias
The shape of the funnel plot did not display any evidence of apparent asymmetry. Furthermore, the formal tests also showed no substantial publication bias (p=0.222 for the Egger’s test; p=0.626 for the Begg’s test) (Figure S1).
Discussion
The increasing interest from oncologists and patients in identifying the optimal administration route of bortezomib has been driven mainly by concerns regarding the efficacy and toxicity.23–26 In phase III trials analyzed both for relapse cases12 and for the newly diagnosed MM patients,15 SC bortezomib was equally effective as the IV administration route and was associated with a reduction in the rate of peripheral neuropathy. The results of a pharmacokinetic study showed that SC bortezomib had a similar AUC (155 vs 151 ng·h/ml), but lower Cmax (20.4 vs 223 ng/mL) and longer Tmax (30 vs 2 mins) compared to IV bortezomib.27 The difference of pharmacokinetic parameters might be a reason why SC bortezomib had a similar efficacy but better tolerated than the IV route of administration. SC bortezomib is also more convenient and less time-consuming to the patient and institution.28 But until now, the results from clinical trials are not compelling enough to support any definitive conclusions about the superiority of SC bortezomib. Here, we performed a systematic review and meta-analysis on the efficacy and safety of SC and IV bortezomib in both newly diagnosed and relapsed MM patients, based on 4 RCTs and 8 retrospective trials which included total 1,857 MM patients. Our results indicated that 1) there was no statistical difference in 1-year OS, 1-year PFS and ORR between SC and IV bortezomib; 2) SC bortezomib had a significantly lower incidence of all-grade peripheral sensory neuropathy, leukopenia, asthenia, fatigue, infection, hepatobiliary disorders, thrombocytopenia than IV administration route, but there was no statistical difference in risk of all-grade diarrhea, pyrexia, nausea/vomiting, weight decrease, constipation, pneumonia, renal and urinary disorders, neuralgia, anemia and neutropenia; 3) SC bortezomib had a significantly lower incidence of grade 3–4 peripheral sensory neuropathy, diarrhea, leukopenia, constipation, fatigue, neuralgia and thrombocytopenia than IV administration route, but there was no statistical difference in risk of grade 3–4 pyrexia, nausea/vomiting, asthenia, weight decrease, infection, pneumonia, renal and urinary disorders, hepatobiliary disorders, anemia and neutropenia.
The results of our study are partly in agreement with those performed by Mu et al7. In that meta-analysis, it was found that SC bortezomib had similar efficacy, lower incidence of peripheral neuropathy and thrombocytopenia to IV administration route of bortezomib. Nontheless, some studies are only abstract; the outcomes of efficacy were only ORR, and one trial included6 was different from other trials (in one trial SC bortezomib was administered once a week, but others were twice a week), and these might affect the final results. Until now, the results of studies published for comparing the efficacy and safety of SC and IV bortezomib in MM patients remain uncertain. Our study compared the efficacy and safety of the two administration routes, and a meta-analysis was performed to draw more comprehensive results. Our study included more relevant articles, and although the number of the trials was still small, our findings might stimulate further investigations.
OS, PFS and ORR are the most important outcomes for evaluating the efficacy of treatments. The results of the meta-analysis for the patients with on-study 1-year OS, 1-year PFS and ORR showed no evidence of a significant difference between SC and IV bortezomib arms (p>0.05). SC administration results in equivalent bortezomib plasma exposure (such as mean AUC) to IV infusion. This pharmacokinetic study of SC and IV bortezomib might partly explain the results of similar efficacy between two administration routes arms.27
Another potential benefit of SC bortezomib would be the reduction of the frequencies of AEs and toxicity. The individual studies suggested that bortezomib was associated with peripheral neuropathy, nausea/vomiting, diarrhea, anemia, thrombocytopenia and leukopenia.29–31 Peripheral nerve damage is one of the most significant nonhematologic toxicities of bortezomib. The painful sensory neuropathy elicits most concerns by clinicians, which not only seriously affect the quality of life of patients, but also one of the reasons for the non-compliance to treatment.32–34 Overall, it appears that SC bortezomib caused a significantly lower incidence of peripheral neuropathy compared to IV administration, in both all-grade and grade 3–4 (p<0.001). The results of this systematic review also suggested that SC bortezomib caused a significantly lower incidence of some AE, such as leukopenia and thrombocytopenia, which indicated that SC bortezomib might be a better choice for some patients with higher AE risk factors.
Heterogeneity was an important concern in the meta-analysis. The heterogeneity might not be totally ruled out in this study, and so the sensitivity analysis was used to identify the robustness of our findings. The results displayed that no study affected the overall significance of the pooled estimates, and the results of our findings were robust. Publication bias might introduce false positives in the meta-analysis.11 To avoid the possible bias, the studies included were all properly assessed. Egger’s and Begg’s tests used in detecting publication bias were performed and no evident bias was found. The results of publication bias and sensitivity analysis indicated that conclusions of our study are credible.
The following limitations merit consideration, and hence, the present meta-analysis should be interpreted with caution. First, there were few studies, especially due to the lack of sufficient high-quality RCTs. Second, although the dosage and schedule of the two drugs in all trials included were consistent, additional rigorously designed experiments are required. Third, the trials included in our analysis were open label, which might affect the outcomes.
Conclusion
In summary, compared to IV administration, SC bortezomib showed equivalent efficacy but caused a significantly lower incidence of some all-grade or grade 3–4 AEs, such as peripheral sensory neuropathy, leukopenia and thrombocytopenia. The data presented so far has consistently shown that SC bortezomib has become a standard of care for patients with MM.
Acknowledgments
This work was supported by the Natural Science Foundation of Zhejiang Province, China (Grant number LYY18H310002).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. doi:10.3322/caac.21442
2. Fitzmaurice C, Allen C, Barber RM, et al;
3. Durie BG, Hoering A, Abidi MH, et al. Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOG S0777): a randomised, open-label, phase 3 trial. Lancet. 2017;389(10068):519–527. doi:10.1016/S0140-6736(16)31594-X
4. Popat R, Oakervee H, Williams C, et al. Bortezomib, low-dose intravenous melphalan, and dexamethasone for patients with relapsed multiple myeloma. Br J Haematol. 2009;144(6):887–894. doi:10.1111/j.1365-2141.2008.07572.x
5. Attal M, Lauwers-Cances V, Hulin C, et al. Lenalidomide, bortezomib, and dexamethasone with transplantation for myeloma. N Engl J Med. 2017;376(14):1311–1320. doi:10.1056/NEJMoa1611750
6. Minarik J, Pavlicek P, Pour L, et al. Subcutaneous bortezomib in multiple myeloma patients induces similar therapeutic response rates as intravenous application but it does not reduce the incidence of peripheral neuropathy. PLoS One. 2015;10(4):e0123866. doi:10.1371/journal.pone.0123866
7. Mu S-D, Ai L-S, Qin Y, Hu Y. Subcutaneous versus intravenous bortezomib administration for multiple myeloma patients: a meta-analysis. Curr Med Sci. 2018;38(1):43–50. doi:10.1007/s11596-018-1844-y
8. Rubin GJ, Amlôt R, Page L, Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. Bmj. 2009;339:b2535. doi:10.1136/bmj.b2651
9. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
10. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101.
11. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–634.
12. Moreau P, Pylypenko H, Grosicki S, et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. Lancet Oncol. 2011;12(5):431–440. doi:10.1016/S1470-2045(11)70081-X
13. Moreau P, Coiteux V, Hulin C, et al. Prospective comparison of subcutaneous versus intravenous administration of bortezomib in patients with multiple myeloma. Haematologica. 2008;93(12):1908–1911. doi:10.3324/haematol.13285
14. Arnulf B, Pylypenko H, Grosicki S, et al. Updated survival analysis of a randomized phase III study of subcutaneous versus intravenous bortezomib in patients with relapsed multiple myeloma. Haematologica. 2012;97(12):1925–1928. doi:10.3324/haematol.2012.067793
15. Merz M, Salwender H, Haenel M, et al. Subcutaneous versus intravenous bortezomib in two different induction therapies for newly diagnosed multiple myeloma: an interim analysis from the prospective GMMG-MM5 trial. Haematologica. 2015;100(7):964–969. doi:10.3324/haematol.2015.124347
16. Xu Y, Deng S, Mao X, et al. Tolerance, kinetics, and depth of response for subcutaneous versus intravenous administration of bortezomib combination in Chinese patients with newly diagnosed multiple myeloma. Clin Lymphoma Myeloma Leuk. 2018;18(6):422–430. doi:10.1016/j.clml.2018.03.006
17. Koh Y, Lee SY, Kim I, et al. Bortezomib-associated peripheral neuropathy requiring medical treatment is decreased by administering the medication by subcutaneous injection in Korean multiple myeloma patients. Cancer Chemother Pharmacol. 2014;74(3):653–657. doi:10.1007/s00280-014-2555-0
18. Lamm W, Drach-Schauer B, Eder S, Drach J. Bortezomib administered subcutaneously is well tolerated in bortezomib-based combination regimens used in patients with multiple myeloma. Oncology. 2013;85(4):223–227. doi:10.1159/000355197
19. Wu S, Zheng C, Chen S, et al. Subcutaneous administration of bortezomib in combination with thalidomide and dexamethasone for treatment of newly diagnosed multiple myeloma patients. Biomed Res Int. 2015;2015:927105. doi:10.1155/2015/927105
20. St-Pierre Y, Sidana S, Narkhede M, et al. Neuropathy and efficacy of once weekly subcutaneous bortezomib in multiple myeloma and light chain (AL) amyloidosis. PLoS One. 2017;12(3):e0172996. doi:10.1371/journal.pone.0172996
21. Liu H, Fu CC, Xue SL, et al. Efficacy and safety study of subcutaneous injection of bortezomib in the treatment of de novo patients with multiple myeloma. Zhonghua Xue Ye Xue Za Zhi. 2013;34(10):868–872. doi:10.3760/cma.j.issn.0253-2727.2013.10.009
22. Wang YS, Ding SH, Wu F, Wang ZT, Wang QS. Safety and efficacy of subcutaneous administration of bortezomib in the treatment of multiple myeloma. Sichuan da xue xue bao Yi xue ban. 2014;45(3):529–532.
23. Sonneveld P, Schmidt-Wolf IG, van der Holt B, et al. Bortezomib induction and maintenance treatment in patients with newly diagnosed multiple myeloma: results of the randomized phase III HOVON-65/GMMG-HD4 trial. J Clin Oncol. 2012;30(24):2946–2955. doi:10.1200/JCO.2011.39.6820
24. Jagannath S, Barlogie B, Berenson JR, et al. Updated survival analyses after prolonged follow-up of the phase 2, multicenter CREST study of bortezomib in relapsed or refractory multiple myeloma. Br J Haematol. 2008;143(4):537–540. doi:10.1111/j.1365-2141.2008.07359.x
25. Dispenzieri A. Bortezomib for myeloma – much ado about something. N Engl J Med. 2005;352(24):2546–2548. doi:10.1056/NEJMe058059
26. Richardson PG, Sonneveld P, Schuster MW, et al. Safety and efficacy of bortezomib in high-risk and elderly patients with relapsed multiple myeloma. Br J Haematol. 2007;137(5):429–435. doi:10.1111/j.1365-2141.2007.06585.x
27. Moreau P, Karamanesht II, Domnikova N, et al. Pharmacokinetic, pharmacodynamic and covariate analysis of subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma. Clin Pharmacokinet. 2012;51(12):823–829. doi:10.1007/s40262-012-0010-0
28. Barbee MS, Harvey RD, Lonial S, et al. Subcutaneous versus intravenous bortezomib: efficiency practice variables and patient preferences. Ann Pharmacother. 2013;47(9):1136–1142. doi:10.1177/1060028013503122
29. Richardson PG, Xie W, Mitsiades C, et al. Single-agent bortezomib in previously untreated multiple myeloma: efficacy, characterization of peripheral neuropathy, and molecular correlations with response and neuropathy. J Clin Oncol. 2009;27(21):3518–3525. doi:10.1200/JCO.2008.18.3087
30. Lonial S, Waller EK, Richardson PG, et al. Risk factors and kinetics of thrombocytopenia associated with bortezomib for relapsed, refractory multiple myeloma. Blood. 2005;106(12):3777–3784. doi:10.1182/blood-2005-03-1173
31. Wu KL, Heule F, Lam K, Sonneveld P. Pleomorphic presentation of cutaneous lesions associated with the proteasome inhibitor bortezomib in patients with multiple myeloma. J Am Acad Dermatol. 2006;55(5):897–900. doi:10.1016/j.jaad.2006.06.030
32. Richardson PG, Briemberg H, Jagannath S, et al. Frequency, characteristics, and reversibility of peripheral neuropathy during treatment of advanced multiple myeloma with bortezomib. J Clin Oncol. 2006;24(19):3113–3120. doi:10.1200/JCO.2005.04.7779
33. Badros A, Goloubeva O, Dalal JS, et al. Neurotoxicity of bortezomib therapy in multiple myeloma: a single-center experience and review of the literature. Cancer. 2007;110(5):1042–1049. doi:10.1002/cncr.22921
34. Argyriou AA, Iconomou G, Kalofonos HP. Bortezomib-induced peripheral neuropathy in multiple myeloma: a comprehensive review of the literature. Blood. 2008;112(5):1593–1599. doi:10.1182/blood-2008-04-149385
Supplementary material
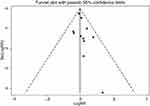 | Figure S1 Publication bias risk. Abbreviations: RR, risk ratio; s.e., standard error of the mean. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

