Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Subcision for Atrophic Acne Scarring: A Comprehensive Review of Surgical Instruments and Combinatorial Treatments
Authors Vempati A , Zhou C , Tam C , Khong J , Rubanowitz A, Tam K , Hazany S, Vasilev R , Hazany S
Received 16 November 2022
Accepted for publication 22 December 2022
Published 18 January 2023 Volume 2023:16 Pages 125—134
DOI https://doi.org/10.2147/CCID.S397888
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Abhinav Vempati,1 Crystal Zhou,1 Curtis Tam,1 Jeffrey Khong,2 Aaron Rubanowitz,3 Kevin Tam,1 Sarah Hazany,1 Ruslan Vasilev,1 Salar Hazany1
1Scar Healing Institute, Los Angeles, CA, USA; 2Johns Hopkins School of Medicine, Baltimore, MD, USA; 3Geisel School of Medicine, Hanover, NH, USA
Correspondence: Abhinav Vempati, Scar Healing Institute, Los Angeles, CA, USA, Tel +1 424 225 2453, Fax +1 310 571 8435, Email [email protected]
Abstract: Subcutaneous incisionless surgery, also known as subcision, is a minimally invasive procedure that is commonly indicated for the treatment of atrophic acne scars. In recent years, many new techniques have been developed to maximize results from this procedure. This review article aims to identify an updated list of instruments and combinatorial treatments available for atrophic acne scar patients undergoing subcision. We constructed a comprehensive PubMed search term and performed triple-blinded screening on all resulting studies for mentions of subcision as indicated by acne scarring. Our results show that there are four main categories of subcision tools that are commonly employed to treat atrophic acne scars: needles, cannulas, wires, and blunt-blade instruments. Usage of these devices varies by scar depth, personal preference, and combinatorial treatment options. Overall, subcision is a particularly effective treatment for atrophic acne scars, and there is vast potential for further innovation with this technique.
Keywords: subcutaneous incisionless surgery, acne scar, depressed scars, CROSS, Taylor liberator
Introduction
Acne vulgaris is a prevalent skin disease that predominantly afflicts adolescent populations. Its pathophysiology is characterized by the hyperkeratinization and androgen-mediated overproduction of sebum in the pilosebaceous unit (PSU), leading to the proliferation of Cutibacterium acnes (formerly classified as Propionibacterium acnes).1–4 Acne scarring subsequently occurs due to aberrant perifollicular inflammation and extracellular matrix (ECM) remodeling mechanisms.5 First, severe and prolonged inflammation leads to the destruction of the PSU and deeper tissues. Second, an imbalance of ECM protein synthesis and degradation fails to maintain the structural integrity of the skin post-acne resolution. Such processes result in atrophic acne scarring in the majority of cases.5
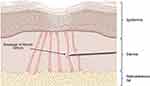
Atrophic acne scars are more common than hypertrophic or keloid scars and are generally classified as ice pick, boxcar, or rolling scars (Figure 1, Table 1).6,7 Given the differing morphologies between these scar types, a variety of treatments were developed to improve them, such as chemical peels, filler injections, laser resurfacing, and microneedling.7 A more recent technique invented to treat acne scarring is subcutaneous incisionless surgery (“subcision”), which was first coined by Orentreich and Orentreich in 1995.7,8 Subcision describes the insertion of an instrument into the skin to manually detach dermal scars adhering to the underlying subcutaneous layer (Figure 2).9 It is effective relative to other treatment modalities because the fibrotic attachments in the dermal-subcutaneous junction that pull down the skin surface are physically shredded apart. The proposed mechanism for the lifting effect of subcision is as follows: first, the dermis is detached from underlying tissues and elevates as a result.10–12 Second, controlled injury induced by subcision stimulates wound healing factors that promote connective tissue growth, which quickly fills the dermal pocket in the treated areas. Third, fat lobules are homogenized and subcutaneous tension forces are evenly redistributed, minimizing contour deformities caused by acne-induced lipoatrophy.8,9,12
 |
Figure 1 Visual representation of atrophic acne scar subtypes. Notes: (A) Ice pick scars are narrow atrophic scars that can extend into the reticular dermis and, in some cases, down to the hypodermis. (B) Boxcar scars are oval- or rectangular-shaped depressions with vertical walls and a flat base. Shallow boxcar scars can extend into the papillary dermis but more severe boxcar scars can penetrate through the reticular dermis. (C) Rolling scars are the widest but shallowest scar type, rarely reaching down to the reticular dermis. They have a wavy or slope-like appearance on the skin. Reproduced with permission from Dove Medical Press. Tam C, Khong J, Tam K, et al. Review of non-energy-based treatments for atrophic acne scarring. Clin Cosmet Investig Dermatol. 2022;15:455–4697 and created with Biorender.com. |
 |
Table 1 Atrophic Acne Scar Subtypes |
Since subcision has been shown to improve all three atrophic acne scar types, clinicians have increasingly preferred this treatment as a primary option in their clinical approach.13 The more frequent use of subcision is also important because the clinical management of acne vulgaris and any subsequent scarring and disfigurement can lead to long-term negative effects on self-esteem and exacerbate common psychiatric disorders such as depression, anxiety, and body dysmorphia.14 Additionally, individuals who suffer from acne scarring may find greater difficulties in socializing and workplace functioning.14 Developing and optimizing successful clinical strategies for acne scar management is thus also essential to ameliorate the distressing psychosocial effects associated with acne scarring. This comprehensive literature review therefore characterizes all advancements in subcision tools to treat atrophic acne scars, with particular emphasis on the past three years.
Methods
We created an initial PubMed search term for all papers relating to subcision for acne scars, written in English, and pertaining to human subjects. Articles that were not original research or relevant review papers, did not analyze human subjects, or only described subcision for non-acne related scars were excluded. Each article was then screened and extracted by three independent reviewers for title, abstract, full text, and reference content. Additional relevant articles listed in reference sections were later added, screened, and extracted in a second review round.
Results
Our initial search resulted in 79 studies. After screening, a total of 47 studies remained. 17 were specific to the subcision tools themselves, while 19 articles described the tools in conjunction with combinatorial treatments. The remaining 11 articles were general review papers comparing various combination treatments. An additional 20 studies were added in a second review round.
Discussion
Our findings revealed that subcision is commonly performed with four different instruments: needles, cannulas, surgical wires, and blunt-blade instruments. The following sections describe each instrument type in detail and are organized by the relative order in which they were developed.
Needles
Before the term “subcision” was popularized, physicians were already using needles to treat atrophic acne scars. Spangler published a study in 1957 evaluating the use of a Bowman iris needle followed by fibrin foam injections for lifting pitted facial scars.15 Later, other researchers used 18- and 20-gauge hypodermic needles to perform the fibrin injection technique.16,17 However, none of these studies fully evaluated the effects of lifting acne scars without simultaneously administering injectables.8 Orentreich and Orentreich, the first authors to publish doing so, performed subcision with the use of sterile, tri-beveled hypodermic 22-gauge needles.8 In their approach, a topical antiseptic such as povidone-iodine or chlorhexidine gluconate is initially applied, followed by local anesthetic injections with 1% or 2% lidocaine with 1:100,000 epinephrine. Once lidocaine infiltration is complete, the needle is inserted into the dermal-subcutaneous junction and moved in a lancing or fanning motion to perforate the fibrotic tethers.8,9 Orentreich and Orentreich also reported using needles as thin as 25- to 27-gauge (sometimes even 30-gauge) for finer facial scars and as thick as 16-gauge for larger depressions.8 This finding has been confirmed by many subsequent studies, indicating that gauge thickness should be selected based on scar depth, fibrotic tether thickness, and personal preference.6,18–20
Several more modifications have also been introduced to needle subcision procedures since this pioneering study to improve efficiency and precision. For instance, Khunger and Khunger described a simple modification in which they used artery forceps to bend a hypodermic needle 90 degrees. Using this L-shaped instrument enables them to maintain a consistent horizontal orientation in the skin during subcision.21 Additionally, Afra et al plugged the open hub of a needle with cotton gauze to prevent blood from leaking throughout the surgical field.22 They proposed this technique as a more ergonomic alternative to attaching a syringe to a needle to prevent blood leakage, which can restrict maneuvering of the probe.
Other types of needles have also been used. Jacob et al reported that an 8-gauge, 1.5-inch Nokor needle could more effectively cut through fibrotic tethers due to its scalpel-like triangular tip.6 While the Nokor needle is often attached to a syringe, some physicians reported using a needle holder to reduce the number of entry points and allow for more horizontal cuts.23 Ayeni et al reported that Nokor needles are sometimes not sharp enough and demonstrated that a 20-gauge microvitreoretinal (MVR) cataract blade can be used as an alternative for particularly challenging scars.24
Needles are the most versatile instruments for subcision. However, multiple sessions are often needed to obtain optimal results and hematomas are quite frequent due to their sharp bevels.12,25
Cannulas
Cannula subcision was introduced as an alternative to needle subcision because needles were reported to have moderate to mild efficacy, with many patients regressing significantly within a few weeks.19,26 A pilot clinical study by Nilforoushzadeh et al in 2015 compared blunt cannula subcision with hypodermic needle subcision in 8 patients.26 They reported a higher patient satisfaction rate and lower average number of hypertrophic lesions with an 18- and 21-gauge metal type spinal cannula compared to hypodermic needles.26 Moreover, they reported that the relative length and flexibility of the cannula enabled them to bend the probe as they advanced it under the skin.27 Thus, only one incision point near the hairline was required to reach most scars, reducing the probability of adverse events associated with multiple entry points.19,20
Cannulas have also been reported to be more effective than Nokor needles. Gheisari et al discovered in a split-face study that both physician and patient satisfaction scores were higher for areas treated with blunt cannula subcision than for those treated with needle subcision, especially at a three-month follow-up assessment.28 However, satisfaction was similar at a 6-month follow-up, implying that the results obtained with cannula subcision may have regressed over time. Like needle subcision, cannula subcision also requires multiple sessions to achieve the desired effect.28 The need for repeated treatments is possibly due to the fact that these instruments merely puncture the fibrotic tethers, as opposed to completely severing them.29 For deeper and more extensive scarring, a more robust instrument is needed to facilitate more thorough subdermal undermining of the scars.
Surgical Wires
Traditional subcision performed with high-gauge hypodermic rodlike instruments, such as needles and cannulas, often provide suboptimal release of adherent scar tissue. Results are often lackluster because these instruments merely perforate the fibrotic tethers as opposed to fully releasing them at the dermal-subcutaneous interface.29
Sulamanidze et al was the first to introduce the use of scalpel wires as an alternative instrument for subcision.30 In this approach, the wire is introduced subdermally through the skin at the apex of the surgically marked areas and removed through the opposite end.30 Then it is reintroduced through the same exit and passed back through the skin at the original entry point (Figure 3). The wire is sawed back-and-forth within the subdermal plane until all the skin depressions are released.30
A retrospective study performed by Graivier et al also showed that wire-based subcision is an effective treatment approach for the correction of deep nasolabial folds, marionette lines, cheek lines, and acne scars.31 In this study, 27 out of 38 patients simultaneously underwent subcision with autologous fat, calcium hydroxylapatite, or poly-l-lactic acid injections.31 All treated scars reportedly “maintained complete correction” at 1- to 19-month follow-ups. There were only three cases of overcorrection, all of which occurred in patients who underwent combined wire subcision and autologous fat transfer.
Results are immediately observed after complete release of the tethers, after which additional improvement can be seen through augmentative tissue fibrosis.32 Combining wire subcision and filler injections seems logical, given that these grafts can serve as a spacer for preventing retethering of the released scars. However, there is a lack of split-face studies showing evidence of this additional benefit.
Blunt-Blade Instruments (Liberators)
The blunt-blade instrument, commonly known as a liberator, is the most recent addition to the surgical armamentarium for subcision. It resembles a long, notched screwdriver with a W-shaped tip designed to effectively capture fibrotic tethers attaching the dermis to the subcutaneous layer (Figure 4).33 When using the instrument, the surgeon can effectively locate these tethers by feeling for resistance to the motion of the instrument.34 Greater force is then applied to push the blunt probe through the tethers, which can be heard in the form of popping or tearing sounds.9
 |
Figure 4 Common Subcision Instruments. Notes: (A) From top to bottom: the Taylor liberator, a blunt cannula, and a hypodermic needle. (B) Magnified images of each instrument tip. |
In 2016, Dr. Mark Taylor et al published a retrospective, uncontrolled, unblinded study detailing the novel use of this instrument to perform extensive subcision of acne scars.34 A 4-mm incision was made near the hairline using a No. 11 or No. 15 blade, followed by tumescent anesthetic infiltration in the treatment areas, effectively separating the skin from the deeper fat and muscle tissues.34 The liberator was then inserted through the entry point and moved in a to-and-fro motion to sever all tethers. The authors reported a mean acne scar improvement of 2.9 (out of 4) in 114 patients when using this liberator along with a superficial chemical peel and fractional carbon dioxide (CO2) laser resurfacing performed in the same session.34
Since then, blunt-blade subcision with tumescent anesthesia has been the norm for performing subcision on deeper, wider scars.9,35,36 Tumescent dissection is particularly important because it expands the mid-subcutaneous plane, offering easier device manipulation and greater distance from deeper underlying tissues.37 Although hydrodissection results in temporary post-operative swelling, the separation of the target layer from underlying tissue minimizes risk of neurovascular injury.33 Asilian et al demonstrated this added safety benefit after finding that 28 patients treated with blunt-blade subcision had fewer adverse events and higher satisfaction at 2-week, 1-month, and 3-month follow-ups when compared to 28 patients treated with a Nokor needle.38
Combinatorial Treatments
Subcision is constantly evolving and has been proven to be an effective treatment for atrophic scarring alone. However, many subjects have been shown to benefit more from combinatorial treatments involving subcision than from subcision alone, especially for patients with severe and mixed acne scar profiles. Below are descriptions of the most common options for combinatorial treatments.
Platelet-Rich Plasma (PRP) and Autologous Fat Grafts
Platelet-rich plasma (PRP) therapy is the most common treatment implemented with subcision. PRP contains potent regenerative and angiogenic properties that promote accelerated healing, increased collagen production, and healthy tissue remodeling in treated scars.39,40 Studies also report that PRP can be safely injected in the same session as 18- to 30-gauge hypodermic or Nokor needle subcision (Figure 5A).39,40 Long et al demonstrated that PRP combined with subcision led to significantly better clinical results than either subcision alone or subcision combined with microneedling.41,42
PRP has also been compared with other autologous injections in combination with subcision, such as autologous fat and activated PRP plasma gel.40 Autologous fat injections following subcision produced more significant results than combined subcision and PRP therapy, while plasma gel injection yielded no difference immediately after subcision but better long-term satisfaction at a 6-month follow-up assessment.40,43
Dermal Fillers
Dermal fillers are another popular addition to subcision protocols, used to restore dermal volume and keep the skin’s surface lifted following subcision-mediated release of fibrotic tethers (Figure 5B).44 A split-face comparison of cross-linked hyaluronic acid (HA) injections with poly-L-lactic acid (PLLA) threads showed that injecting HA after wire subcision resulted in significant clinical improvement in 94.1% of treated patients, while injecting PLLA after wire subcision resulted in significant clinical improvement in 82.4% of treated patients.45 However, both combinations were more effective than subcision alone, which showed clinical improvement in only 67.3% of treated patients.45 In a separate study, subcision was performed followed by subdermal implantation of size 0 absorbable sutures under the subcised scars. Mild improvement was obtained for the majority of subjects but no additional benefit was observed with this combinatorial treatment.46 On the other hand, Sasaki et al demonstrated significantly greater improvement for patients who underwent combined and autogenous or xenograft filler injections than for those who underwent subcision alone.47
Chemical Peels
Chemoexfoliation with strong acids, such trichloroacetic acid (TCA) or phenol, is frequently performed with subcision. One technique that is often utilized is chemical reconstruction of skin scarring (CROSS), in which chemical agents are focally applied to the scar tissue alone while sparing the surrounding healthy skin.48 CROSS induces neosynthesis of collagen and elastin and has proven to be an effective standalone treatment for ice pick acne scarring.49,50 TCA and phenol CROSS were found to be safe and effective when used in conjunction with subcision for atrophic scarring across all studies evaluated, but it was noted that TCA may cause widening of scars if applied improperly. The majority of studies showed marked improvement in combinatorial subcision and CROSS treatments in patients presenting with a mixture of ice pick, rolling, and boxcar scars, except for one split-face study by Kamel et al where TCA did not provide an additional clinical benefit.34,49,51 Therefore, it is possible that combination treatment with the subcision technique particularly targets rolling scars and has tentatively yielded greater results in patients with mixed atrophic scar types.52
Energy-Based Treatments
Energy-based treatments, notably laser resurfacing, are commonly used to improve the appearance of atrophic acne scars through direct thermal ablation of the skin.48,53 Subcision, which elevates scars closer to the level of the surrounding healthy skin, minimizes the extent of ablation required to achieve a more even skin texture, protecting against excessive dermal thinning and other associated side effects from these treatments.53 In one comprehensive review, Nd:YAG, Er:YAG, and CO2 lasers were combined with needle subcision safely and effectively across all included studies.51,53–57 Overall, significant reduction in acne scar severity was more consistently for rolling and boxcar scars than for ice pick scars. Two other studies investigated CO2 laser in combination with CO2 gas subcision, both of which led to significantly improved results compared to CO2 laser alone.58,59 Histological assessment following combined CO2 laser resurfacing and subcision also confirmed significant increases in dermal collagen content and dermal thickness, as well as the straightening of elastic fibers in the reticular dermis.58,60
One split-face study evaluated radiofrequency-guided subcision but found no significant improvement in scar severity compared to unguided subcision upon clinical assessment, despite patient self-assessment scores favoring the radiofrequency-guided subcision side.61,62
Microneedling
Fernandes was the first to describe percutaneous collagen induction, also known simply as microneedling, as a viable treatment for skin rejuvenation.63 In this method, a handheld roller or stamp studded with 0.5- to 2.0-mm long needles is applied to the skin to create microscopic punctures in the skin, leading to collagen and elastin production. Numerous studies have demonstrated the clinical efficacy and high safety profile of microneedling for atrophic acne scarring. For example, both Bhargava et al and Garg and Baveja independently demonstrated that combined subcision and microneedling produced an “excellent” response in the majority of patients with Grade 3 to 4 scarring on the Goodman and Baron severity scale.64,65 In another study, it was shown that topically applying PRP immediately after patients have undergone subcision and microneedling provides an additional benefit, especially in rolling and shallow boxcar scars.66 However, less significant correction was observed for deep boxcar and ice pick scars, which require more sessions and other more invasive interventions to achieve better results.67
Rullan et al proposed another triple combination treatment consisting of phenolic CROSS, cannula subcision, and microneedling.68 Unlike many other studies which space out their combinatorial treatments, subjects in these studies underwent all three interventions in one sitting. Subcision in this study was performed with the aid of either a Nokor needle or a blunt 70-mm, 18-gauge cannula. High patient satisfaction was achieved with this combinatorial approach, although there was no data comparing the efficacy of Nokor needle subcision with that of cannula subcision.
Nevertheless, there is a dearth of controlled studies that support the additional improvement from combining subcision with microneedling. One study comparing the efficacy of subcision and fractionated microneedling radiofrequency with subcision alone showed significant improvement in both intervention groups but greater patient satisfaction in the former intervention group.69 However, only short-term follow-up results were reported. Interestingly, in another split-face study, subcision combined with cryorolling produced a 57% improvement in patients versus 40% in patients who underwent subcision and dermarolling.70
Suctioning
Suctioning, or vacuum-assisted massage therapy, for scarring is a simple at-home treatment that mechanically lifts scars. It exerts its action by releasing tension in contracted scars and biomechanically stimulating fibroblast activity.71 Harandi et al incorporated suction sessions that began on the 3rd day after subcision and continued at least every other day for 2 weeks. This protocol resulted in a mean improvement of 71.73% in acne scar patients, compared to 43.75% in patients with limited or no suctioning.71 However, this is the only published study evaluating suctioning as an adjuvant therapy, and more data is required to understand the full effects of the subcision-suction method.
Conclusion
The available literature presents several promising subcision combinatory therapies for the treatment of atrophic scarring, but robust clinical guidelines cannot be formulated without first developing standardized operating protocols for each treatment modality. Additionally, treatment modalities are often combined based on a physician’s personal preference, and an individual may be treated with one or more of the options mentioned in this section. Therefore, more controlled, comparative split-face studies with rigorous statistical measurements are necessary to ascertain which combinations are optimal for patients of different scarring severities and scar types.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Connolly D, Vu HL, Mariwalla K, Saedi N. Acne scarring-pathogenesis, evaluation, and treatment options. J Clin Aesthetic Dermatol. 2017;10(9):12–23.
2. Oge’ LK, Broussard A, Marshall MD. Acne vulgaris: diagnosis and treatment. Am Fam Physician. 2019;100(8):475–484.
3. Chilicka K, Rogowska AM, Szyguła R, Dzieńdziora-Urbińska I, Taradaj J. A comparison of the effectiveness of azelaic and pyruvic acid peels in the treatment of female adult acne: a randomized controlled trial. Sci Rep. 2020;10(1):12612. doi:10.1038/s41598-020-69530-w
4. Chilicka K, Rusztowicz M, Rogowska AM, Szyguła R, Asanova B, Nowicka D. Efficacy of hydrogen purification and cosmetic acids in the treatment of acne vulgaris: a preliminary report. J Clin Med. 2022;11(21):6269. doi:10.3390/jcm11216269
5. Fabbrocini G, Annunziata MC, D’Arco V, et al. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080. doi:10.1155/2010/893080
6. Jacob CI, Dover JS, Kaminer MS. Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol. 2001;45(1):109–117. doi:10.1067/mjd.2001.113451
7. Tam C, Khong J, Tam K, et al. Review of non-energy-based treatments for atrophic acne scarring. Clin Cosmet Investig Dermatol. 2022;15:455–469. doi:10.2147/CCID.S350040
8. Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21(6):543–549. doi:10.1111/j.1524-4725.1995.tb00259.x
9. Dadkhahfar S, Robati RM, Gheisari M, Moravvej H. Subcision: indications, adverse reactions, and pearls. J Cosmet Dermatol. 2020;19(5):1029–1038. doi:10.1111/jocd.13308
10. Ahramiyanpour N, Rastaghi F, Parvar SY, Sisakht AK, Hosseini SA, Amani M. Subcision in acne scarring: a review of clinical trials. J Cosmet Dermatol. 2022. doi:10.1111/jocd.15480
11. Alam M, Omura N, Kaminer MS. Subcision for acne scarring: technique and outcomes in 40 patients. Dermatol Surg. 2005;31(3):310–317; discussion 317. doi:10.1111/j.1524-4725.2005.31080
12. Zaleski-Larsen LA, Fabi SG, McGraw T, Taylor M. Acne scar treatment: a multimodality approach tailored to scar type. Dermatol Surg. 2016;42(Suppl 2):S139–S149. doi:10.1097/DSS.0000000000000746
13. Werschler WP, Few JW, Jacob CI, Joseph JH, Spencer JM, Taub AF. Advancing the care of post-acne scarring: expert insights into new treatment options. J Drugs Dermatol. 2016;15(5):518–525.
14. Tan J, Beissert S, Cook-Bolden F, et al. Evaluation of psychological well-being and social impact of atrophic acne scarring: a multinational, mixed-methods study. JAAD Int. 2022;6:43–50. doi:10.1016/j.jdin.2021.11.006
15. Spangler AS. New treatment for pitted scars; preliminary report. AMA Arch Dermatol. 1957;76(6):708–711. doi:10.1001/archderm.1957.01550240026005
16. Millikan L, Banks K, Purkait B, Chungi V. A 5-year safety and efficacy evaluation with fibrel in the correction of cutaneous scars following one or two treatments. J Dermatol Surg Oncol. 1991;17(3):223–229. doi:10.1111/j.1524-4725.1991.tb03635.x
17. Treatment of depressed cutaneous scars with gelatin matrix implant: a multicenter study. J Am Acad Dermatol. 1987;16(6):1155–1162. doi:10.1016/S0190-9622(87)70150-9
18. Vaishnani JB. Subcision in rolling acne scars with 24G needle. Indian J Dermatol Venereol Leprol. 2008;74(6):677–679. doi:10.4103/0378-6323.45133
19. Ebrahim HM, Artima AY, Elardi A, Mohamed Morsi H. Clinical and histopathological evaluation of different tools for the subcision of atrophic acne scars. J Cosmet Dermatol. 2022;21(3):1127–1134. doi:10.1111/jocd.14562
20. Lima EVDA. Dermal tunneling: a proposed treatment for depressed scars. An Bras Dermatol. 2016;91(5):697–699. doi:10.1590/abd1806-4841.20164959
21. Khunger N, Khunger M. Subcision for depressed facial scars made easy using a simple modification. Dermatol Surg. 2011;37(4):514–517. doi:10.1111/j.1524-4725.2011.01925.x
22. Afra TP, Razmi TM, Tarun N, Dogra S. Plug the needle hub during subcision for a bloodless field. J Cosmet Dermatol. 2020;19(5):1179–1181. doi:10.1111/jocd.13117
23. Al Ghamdi KM. A better way to hold a Nokor needle during subcision. Dermatol Surg. 2008;34(3):378–379. doi:10.1111/j.1524-4725.2007.34073.x
24. Ayeni O, Carey W, Muhn C. Acne scar treatment with subcision using a 20-G cataract blade. Dermatol Surg. 2011;37(6):846–847. doi:10.1111/j.1524-4725.2011.02010.x
25. Boen M, Jacob C. A review and update of treatment options using the acne scar classification system. Dermatol Surg. 2019;45(3):411–422. doi:10.1097/DSS.0000000000001765
26. Nilforoushzadeh M, Lotfi E, Nickkholgh E, Salehi B, Shokrani M. Can subcision with the cannula be an acceptable alternative method in treatment of acne scars? Med Arch Sarajevo Bosnia Herzeg. 2015;69(6):384–386. doi:10.5455/medarh.2015.69.384-386
27. Nilforoushzadeh MA, Lotfi E, Heidari-Kharaji M, Nickhah N, Alavi S, Mahmoudbeyk M. Comparing cannula-based subcision with the common needle method: a clinical trial. Skin Res Technol. 2020;26(1):39–44. doi:10.1111/srt.12761
28. Gheisari M, Iranmanesh B, Saghi B. Blunt cannula subcision is more effective than Nokor needle subcision for acne scars treatment. J Cosmet Dermatol. 2019;18(1):192–196. doi:10.1111/jocd.12523
29. Basta-Juzbašić A. Current therapeutic approach to acne scars. Acta Dermatovenerol Croat. 2010;18(3):171–175.
30. Sulamanidze MA, Salti G, Mascetti M, Sulamanidze GM. Wire scalpel for surgical correction of soft tissue contour defects by subcutaneous dissection. Dermatol Surg. 2000;26(2):146–150;discussion 150–151. doi:10.1046/j.1524-4725.2000.99127.x
31. Graivier M. Wire subcision for complete release of depressions, subdermal attachments, and scars. Aesthet Surg J. 2006;26(4):387–394. doi:10.1016/j.asj.2006.05.004
32. Ant JG, Branman RL. The treatment of acne scarring using a wire scalpel. Am J Cosmet Surg. 2006;23(1):13–16. doi:10.1177/074880680602300104
33. Barikbin B, Akbari Z, Yousefi M, Dowlati Y. Blunt blade subcision: an evolution in the treatment of atrophic acne scars. Dermatol Surg. 2017;43(Suppl 1):S57–S63. doi:10.1097/DSS.0000000000000650
34. Taylor MB, Zaleski-Larsen L, McGraw TA. Single session treatment of rolling acne scars using tumescent anesthesia, 20% trichloracetic acid extensive subcision, and fractional CO2 laser. Dermatol Surg. 2017;43(Suppl 1):S70–S74. doi:10.1097/DSS.0000000000000895
35. Ramadan SAER, El-Komy MHM, Bassiouny DA, El-Tobshy SA. Subcision versus 100% trichloroacetic acid in the treatment of rolling acne scars. Dermatol Surg. 2011;37(5):626–633. doi:10.1111/j.1524-4725.2011.01954.x
36. Swinehart JM. Case reports: Surgical therapy of acne scars in pigmented skin. J Drugs Dermatol. 2007;6(1):74–77.
37. Hussein A, Convery C. Taylor liberator full field subcision of acne scarring under tumescent anaesthesia. J Clin Exp Dermatol Res. 2021;12(1):1.
38. Asilian A, Faghihi G, Asemi Esfahani A, Mokhtari F, Nilforoushzadeh M, Mozafarpoor S. Comparison of two methods of subcision Nokor and blunt blade in acne scars treatment. J Cosmet Dermatol. 2019;18(6):1788–1793. doi:10.1111/jocd.12981
39. Deshmukh NS, Belgaumkar VA. Platelet-rich plasma augments subcision in atrophic acne scars: a split-face comparative study. Dermatol Surg. 2019;45(1):90–98. doi:10.1097/DSS.0000000000001614
40. Nassar A, El-Shaarawy W, Salah E. Autologous plasma gel injection combined with scar subcision is a successful technique for atrophic post-acne scars: a split-face study. J Dermatol Treat. 2022;33(2):829–835. doi:10.1080/09546634.2020.1782322
41. Long T, Gupta A, Ma S, Hsu S. Platelet-rich plasma in noninvasive procedures for atrophic acne scars: a systematic review and meta-analysis. J Cosmet Dermatol. 2020;19(4):836–844. doi:10.1111/jocd.13331
42. Hassan AS, El-Hawary MS, Abdel Raheem HM, Abdallah SH, El-Komy MM. Treatment of atrophic acne scars using autologous platelet-rich plasma vs combined subcision and autologous platelet-rich plasma: a split-face comparative study. J Cosmet Dermatol. 2020;19(2):456–461. doi:10.1111/jocd.13048
43. Shetty VH, Bhandary SN, Bhandary R, Suvarna C. A comparative study of efficacy and safety of autologous fat grafting versus platelet-rich plasma in the treatment of post-acne scars. J Cosmet Dermatol. 2021;20(11):3454–3461. doi:10.1111/jocd.14503
44. O’Daniel TG. Multimodal management of atrophic acne scarring in the aging face. Aesthetic Plast Surg. 2011;35(6):1143–1150. doi:10.1007/s00266-011-9715-y
45. Ebrahim HM, Nassar A, ElKashishy K, Artima AYM, Morsi HM. A combined approach of subcision with either cross-linked hyaluronic acid or threads in the treatment of atrophic acne scars. J Cosmet Dermatol. 2022;21(8):3334–3342. doi:10.1111/jocd.14675
46. Balighi K, Robati RM, Moslehi H, Robati AM. Subcision in acne scar with and without subdermal implant: a clinical trial. J Eur Acad Dermatol Venereol. 2008;22(6):707–711. doi:10.1111/j.1468-3083.2008.02583.x
47. Sasaki GH. Comparison of results of wire subcision performed alone, with fills, and/or with adjacent surgical procedures. Aesthet Surg J. 2008;28(6):619–626. doi:10.1016/j.asj.2008.10.005
48. Ward RE, Sklar LR, Eisen DB. Surgical and noninvasive modalities for scar revision. Dermatol Clin. 2019;37(3):375–386. doi:10.1016/j.det.2019.03.007
49. Kamel MM, Hegazy RA, Hegazy AA, Fotoh OMAE, Amer MA. Combined subcision, autologous platelet-rich plasma, and CROSS technique in the treatment of atrophic acne scars: prospective split face study. Clin Dermatol. 2021;39(6):1018–1024. doi:10.1016/j.clindermatol.2021.07.003
50. Abdel-Magiud EM, Taha EA, Bakr RM, et al. Effects of different therapeutic modalities for postacne scars on circulating collagen III. J Cosmet Dermatol. 2020;19(6):1517–1521. doi:10.1111/jocd.13184
51. Taylor MB, Koron N. Combined treatment of rolling acne scars in ethnic skin using extensive subcision, trichloracetic acid peel, and fractional ablative erbium laser. Dermatol Surg. 2021;47(4):496–499. doi:10.1097/DSS.0000000000002858
52. Al-Dhalimi MA, Arnoos AA. Subcision for treatment of rolling acne scars in Iraqi patients: a clinical study. J Cosmet Dermatol. 2012;11(2):144–150. doi:10.1111/j.1473-2165.2012.00616.x
53. Anupama YG, Wahab AJ. Effectiveness of CO(2) laser with subcision in patients with acne scars. J Cosmet Laser Ther. 2016;18(7):367–371. doi:10.1080/14764172.2016.1188213
54. Fulchiero GJJ, Parham-Vetter PC, Obagi S. Subcision and 1320-nm Nd:YAG nonablative laser resurfacing for the treatment of acne scars: a simultaneous split-face single patient trial. Dermatol Surg. 2004;30(10):1356–1359; discussion 1360. doi:10.1111/j.1524-4725.2004.30411.x
55. Kang WH, Kim YJ, Pyo WS, Park SJ, Kim JH. Atrophic acne scar treatment using triple combination therapy: dot peeling, subcision and fractional laser. J Cosmet Laser Ther. 2009;11(4):212–215. doi:10.3109/14764170903134326
56. Kroepfl L, Emer JJ. Combination therapy for acne scarring: personal experience and clinical suggestions. J Drugs Dermatol. 2016;15(11):1413–1419.
57. Lanoue J, Goldenberg G. Acne scarring: a review of cosmetic therapies. Cutis. 2015;95(5):276–281.
58. Lee SJ, Suh DH, Chang KY, et al. The efficacy and safety of subcision using CO(2) gas combined with fractional laser for acne scars: clinical and microscopic evaluation. J Cosmet Laser Ther. 2016;18(7):417–420. doi:10.1080/14764172.2016.1202418
59. Abdel Kareem IM, Fouad MA, Ibrahim MK. Effectiveness of subcision using carboxytherapy plus fractional carbon dioxide laser resurfacing in the treatment of atrophic acne scars: comparative split face study. J Dermatol Treat. 2020;31(3):296–299. doi:10.1080/09546634.2019.1595505
60. Cooper JS, Lee BT. Treatment of facial scarring: lasers, filler, and nonoperative techniques. Facial Plast Surg. 2009;25(5):311–315. doi:10.1055/s-0029-1243079
61. Kaur M, Sharma VK, Sethuraman G, Arava S, Gupta S. A split-face randomized controlled study comparing the efficacy and safety of intralesional radiofrequency-assisted subcision vs conventional subcision in postacne scars. J Cosmet Dermatol. 2020;19(5):1086–1092. doi:10.1111/jocd.13384
62. Yadav S, Gupta S. Radiofrequency-assisted subcision for postacne scars. J Am Acad Dermatol. 2018;78(1):e9–e10. doi:10.1016/j.jaad.2017.07.037
63. Fernandes D. Minimally invasive percutaneous collagen induction. Oral Maxillofac Surg Clin N Am. 2005;17(1):51–63. doi:10.1016/j.coms.2004.09.004
64. Garg S, Baveja S. Combination therapy in the management of atrophic acne scars. J Cutan Aesthet Surg. 2014;7(1):18. doi:10.4103/0974-2077.129964
65. Bhargava S, Kumar U, Varma K. Subcision and microneedling as an inexpensive and safe combination to treat atrophic acne scars in dark skin: a prospective study of 45 patients at a tertiary care center. J Clin Aesthetic Dermatol. 2019;12(8):18–22.
66. Bhargava S, Kroumpouzos G, Varma K, Kumar U. Combination therapy using subcision, needling, and platelet-rich plasma in the management of grade 4 atrophic acne scars: a pilot study. J Cosmet Dermatol. 2019;18(4):1092–1097. doi:10.1111/jocd.12935
67. Savita K, Ranagol A, Hosthota A, Pujar RV, Koregol AC. Dermaroller as an inexpensive and excellent therapeutic modality in the treatment of acne scars along with subcision and punch floatation. IP Indian J Clin Exp Dermatol. 2020;4(4):319–323. doi:10.18231/2581-4729.2018.0066
68. Rullan PP, Olson R, Lee KC. A combination approach to treating acne scars in all skin types: carbolic chemical reconstruction of skin scars, blunt bi-level cannula subcision, and microneedling-A case series. J Clin Aesthetic Dermatol. 2020;13(5):19–23.
69. Faghihi G, Poostiyan N, Asilian A, et al. Efficacy of fractionated microneedle radiofrequency with and without adding subcision for the treatment of atrophic facial acne scars: a randomized split-face clinical study. J Cosmet Dermatol. 2017;16(2):223–229. doi:10.1111/jocd.12346
70. Gadkari R, Nayak C. A split-face comparative study to evaluate efficacy of combined subcision and dermaroller against combined subcision and cryoroller in treatment of acne scars. J Cosmet Dermatol. 2014;13(1):38–43. doi:10.1111/jocd.12071
71. Aalami Harandi S, Balighi K, Lajevardi V, Akbari E. Subcision-suction method: a new successful combination therapy in treatment of atrophic acne scars and other depressed scars. J Eur Acad Dermatol Venereol. 2011;25(1):92–99. doi:10.1111/j.1468-3083.2010.03711.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.