Back to Journals » Journal of Multidisciplinary Healthcare » Volume 8
Structured nursing communication on interdisciplinary acute care teams improves perceptions of safety, efficiency, understanding of care plan and teamwork as well as job satisfaction
Authors Gausvik C, Lautar A, Miller L, Pallerla H, Schlaudecker J
Received 13 August 2014
Accepted for publication 29 September 2014
Published 14 January 2015 Volume 2015:8 Pages 33—37
DOI https://doi.org/10.2147/JMDH.S72623
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Christian Gausvik,1 Ashley Lautar,2 Lisa Miller,2 Harini Pallerla,3 Jeffrey Schlaudecker4,5
1University of Cincinnati College of Medicine, 2The Christ Hospital, Cincinnati, OH, USA; 3Department of Family and Community Medicine, 4Division of Geriatric Medicine, University of Cincinnati, Cincinnati, OH, USA; 5Geriatric Medicine Fellowship Program, University of Cincinnati/The Christ Hospital, Cincinnati, OH, USA
Abstract: Efficient, accurate, and timely communication is required for quality health care and is strongly linked to health care staff job satisfaction. Developing ways to improve communication is key to increasing quality of care, and interdisciplinary care teams allow for improved communication among health care professionals. This study examines the patient- and family-centered use of structured interdisciplinary bedside rounds (SIBR) on an acute care for the elderly (ACE) unit in a 555-bed metropolitan community hospital. This mixed methods study surveyed 24 nurses, therapists, patient care assistants, and social workers to measure perceptions of teamwork, communication, understanding of the plan for the day, safety, efficiency, and job satisfaction. A similar survey was administered to a control group of 38 of the same staff categories on different units in the same hospital. The control group units utilized traditional physician-centric rounding. Significant differences were found in each category between the SIBR staff on the ACE unit and the control staff. Nurse job satisfaction is an important marker of retention and recruitment, and improved communication may be an important aspect of increasing this satisfaction. Furthermore, improved communication is key to maintaining a safe hospital environment with quality patient care. Interdisciplinary team rounds that take place at the bedside improve both nursing satisfaction and related communication markers of quality and safety, and may help to achieve higher nurse retention and safer patient care. These results point to the interconnectedness and dual benefit to both job satisfaction and patient quality of care that can come from enhancements to team communication.
Keywords: interprofessional teams, patient- and family-centered care, structured interdisciplinary bedside rounds, ACE unit, health care teams
Introduction
Interdisciplinary team rounds allow a group of health care professionals to come together for patient care. These teams have already been shown to improve quality by reducing events such as hospital-related falls1 and by increasing other aspects of the culture of safety on a hospital unit.2 More specifically, nurse–physician communication on an interdisciplinary team has been shown to support positive patient outcomes. Validated tools such as “situation, background, assessment, and recommendation” provide structure to these interactions,3 but there is opportunity for continued improvement. The Joint Commission identified communication as one of the root causes in over 60% of reported sentinel events in 2013,4 and another study found communication to be one of the top two contributing factors in an analysis of over 70 medical mishaps.5
Structured interdisciplinary bedside rounds (SIBR) provide the validated structure that operationalizes interdisciplinary communication while bringing together many care providers involved in the patients care at the bedside, including an emphasis on including the patient and family. The SIBR model was developed by Dr Jason Stein of Emory University with the goal of improving quality and patient outcomes.6 This interaction with the health care team provides an opportunity for anyone to raise questions and concerns in a level-playing field, one hallmark of a strong culture of safety in a hospital. This study examines staff perceptions of the SIBR process on an acute care for the elderly (ACE) unit in a 555-bed metropolitan community hospital awarded Magnet certification in 2011 for excellence in nursing innovation and practice in Cincinnati, OH.
An ACE unit provides acute care to geriatric patients in the hospital where the goal is to prevent functional decline and reduce rates of hospital-related adverse events. Geriatric patients represent an ever-increasing proportion of the population and of hospitalizations in the US.7,8 These patients are particularly susceptible to functional declines and increases in frailty.9 ACE units have been shown to improve outcomes, decrease length of stay,10 and reduce costs,11 even while serving a more frail population. The five common ACE unit characteristics include a focus on early rehabilitation and discharge planning, geriatric-based medical review, patient-centered care, and a hospital environment designed to promote functional independence. The Christ Hospital opened a ten-bed ACE unit in September 2013 with a focus on interdisciplinary care and team-based bedside rounds. The unit accepts patients over 70 years of age admitted from home and requiring acute hospitalization. The interdisciplinary ACE team includes a nurse practitioner, geriatrician, social worker, nurses, physical and occupational therapists, as well as patient care assistants (PCAs). Dietary and speech and language therapists are consulted on an as needed basis. The interdisciplinary teams and SIBR are key components to delivering this quality of care on our ACE unit.
Methods
This study was granted exempt status by the institutional review board at the University of Cincinnati College of Medicine and The Christ Hospital. Since the ACE unit was newly created with the SIBR in place from the outset, a comparison study was chosen to look for changes in staff perceptions of SIBR. In order to measure those perceptions on the ACE unit, surveys were developed and administered to ACE unit staff, which included nurses, social workers, physical and occupational therapists, and PCAs. A separate survey was developed for these same staff groups on four non-intensive care hospital units (medical/surgery and telemetry units) to be used as control groups. This control survey focused on standard physician-centric rounds, in which the attending physician examines computerized laboratory and vital sign information, examines and talks to the patient, and enters a note in the electronic health record, which may or may not involve the physician discussing issues with nursing staff. In contrast to SIBR, there is no operationalized method for physicians to draw information in a multidirectional manner of communication from nursing staff.
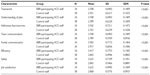
Volunteer subjects were informed of the purpose of the study and made aware of the anonymity of the results before completing the items. All surveys included Likert-style statements with options to strongly agree, agree, disagree, or strongly disagree. These questions focused on how SIBR impacted staff perception of hospital care across a broad range of modalities. All surveys also included an optional comment section. Some of the key areas about which perceptions were measured include teamwork, communication, efficiency, job satisfaction, and patient safety (Table 1). Staff surveys were administered to a convenience sample by visiting the units each afternoon during a 2-week period. The surveys were offered voluntarily but completed by all staff offered (Figure 1).
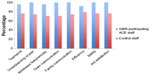  | Figure 1 Percentage of each group agreeing or strongly agreeing on selected topics. |
Quantitative results were compiled for each of the four surveys, and the comments were compiled as well. Likert data were tabulated; statistical comparisons were made with IBM SPSS 22 between SIBR staff on the ACE unit and control groups using a Mann–Whitney U test. Comparisons were based on common themes in the questions to look for significant differences between the groups. The categories included teamwork, understanding the plan for the day, addressing fears and worries, team communication, family communication, efficiency, safety, and job satisfaction (Table 1).
Results
Survey results were collected from 24 SIBR staff (patient-/family-centric ACE unit) and 38 control unit staff (physician-centric rounds). The survey found that staff rated the interdisciplinary nature of SIBR significantly better in all eight distinct areas described above when compared to staff in the control units. 100% of ACE staff agreed or strongly agreed that they felt comfortable to bring up concerns about the patient during SIBR, and 96% of ACE staff said they agreed or strongly agreed that they were working in a team to take care of the patient compared to only 76% of non-ACE staff when asked about their teamwork. Furthermore, 100% of ACE staff agreed or strongly agreed that they understood the patient plan for the day based on rounds, compared to 74% of the control. When asked whether SIBR on ACE improved communication between the team and with family, 100% of SIBR-participating staff on the ACE unit agreed or strongly agreed, while only 71% and 74% of control unit staff gave the same responses, respectively. 92% and 79% of SIBR and control unit staff, respectively, agreed or strongly agreed that their respective rounds improved efficiency of care. Similarly, 100% of SIBR-participating staff on the ACE unit agreed or strongly agreed that SIBR improved safety for their patients, while only 76% of control unit staff said the same for the rounds on their unit. 100% of SIBR respondents agreed or strongly agreed that interdisciplinary bedside rounds increased their own job satisfaction, while only 76% of control units agreed.
One ACE staff member wrote in the comments section of the survey: “I feel like I am part of a team dynamic that is really invested in the patient – not just checking off my to-do list.”
Other staff recognized SIBRs utility in all settings: SIBR is an excellent idea for patients of all age ranges. It should most definitely be implemented in more hospital settings in order to keep patients informed of their health.
Discussion
Interprofessional team care has been associated with higher levels of nursing job satisfaction.12 Collaboration with medical staff and other members of the care team has received some attention, including in a 2009 study by Chang et al, which found that collaborative interdisciplinary relationships were one of the most important predictors of job satisfaction for all health care providers.13
Nurse recruitment and retention are critically important to maintaining a sufficient supply of practicing nurses in the US. Job satisfaction is a key factor to both recruitment and retention, and sources of job satisfaction are varied.14 It has been reported that up to one fifth of nurses in the US plan to leave their jobs in the next 12 months,15 and that almost half of the nurses are dissatisfied with their jobs. Broadly defined sources of nursing job satisfaction include working conditions, interpersonal interactions, and psychological factors.14 Working conditions related to nursing satisfaction include opportunities for promotion and self-promotion, professional training, demands and variety in the job itself, and remuneration.14 Interpersonal interactions related to nursing satisfaction include relationships with coworkers, managers, and patients. Psychological factors associated with increased nursing job satisfaction include autonomy, job security perception, and the presence of rewards such as praise and encouragement.14
A healthy work environment is defined as including a collaborative practice culture, a communication-rich culture, a culture of accountability, expert team members, shared decision making, and recognition of contributions of others.16 Magnet status is awarded to hospitals that provide quality patient care, and achieve nursing excellence and innovation in professional nursing practice. Magnet hospitals are those that have demonstrated healthy work environments, promoting retention and decreasing medical errors. Our study hospital achieved Magnet status in 2011, and generally, is felt to have a healthy environment. The addition of team-based, high-SIBR on the geriatric ACE unit demonstrated significant improvements in many variables related to positive work environments. Job satisfaction was higher among staff on the ACE unit than within control units perhaps due to the higher ratings on teamwork, communication aspects of patient care, and improvements in efficiency.
Improved communication for staff was also investigated with questions about specific areas of patient care. Staff participating in SIBR on the ACE unit felt that they were better able to address the fears and worries of their patients following the team-based rounds. Also, staff understanding of the plan was felt to be higher among SIBR-participating staff members. Ability of staff to communicate with members of the patient’s family was also significantly improved among staff on the ACE unit. These results point to the interconnectedness and dual benefit to both job satisfaction and patient quality of care that can come from enhancements to team communication.
Sample size was a limitation of this study. While the sample size was sufficient to achieve significant results, the study was limited to a 2-week time period of data collection, and it was not possible to collect data from every member of the nursing staff. Though patients and families were surveyed, the 2-week period yielded only three surveys, and it was not sufficient for inclusion in the study. Additionally, the survey results may not be generalizable to all hospital types and settings. Further research should seek to explore what aspects of SIBR are most beneficial, and which aspects of communication are key to the significant results shown here. Further research should aim to tie these results to patient safety and quality data. The SIBR method seemed to also increase patient and family satisfaction, and future studies should seek to explore that effect as well.
Conclusion
Within a large, urban, community hospital, the institution of SIBR on a geriatric ACE unit was associated with significantly higher ratings for teamwork, communication, and efficiency by participating staff, compared to several control units within the same hospital. These results demonstrate the ability of interprofessional team-based rounds (SIBR) to improve staff perceptions of care quality, even at a hospital already awarded Magnet certification for excellence in nursing innovation and practice. These include an increased sense of teamwork, increased staff understanding of plan of care, enhanced communication abilities with team members, increased ability to address patient fears and worries, improvements in staff efficiency, improvements in patient safety, and improved job satisfaction. Taken together, these variables would seem to contribute to higher quality of care.
Given the demonstrated importance of communication in maintaining a safe hospital environment, these changes not only increase job satisfaction and potentially decrease job turnover, but they are also a key step toward breaking down the hospital hierarchies that often diminish effective and safe communication. The significant differences in perceptions of safety and self-efficacy in this study show a well-rounded picture of cultural change contributing to improved safety metrics and staff satisfaction.
The practice of operationalizing structured bedside rounds was perceived as highly beneficial to patient care and job satisfaction by participating nurses. The opportunity for interdisciplinary professionals to work together as a team in real time at the bedside of the patient was perceived by participating staff to positively impact several markers of overall hospital quality. In the future, additional research is warranted to examine ways to cultivate open communication that occurs in structured ways and actively involve patients and families as partners in health care.
Acknowledgments
The authors wish to thank the nurses, PCAs, therapists, nutritionists, members of the hospital leadership team, and all those involved in the exceptional care of older adults on the ACE unit.
Disclosure
The authors have no financial disclosures to report. The authors report no conflicts of interest in this work.
References
von Renteln-Kruse W, Krause T. Incidence of in-hospital falls in geriatric patients before and after the introduction of an interdisciplinary team-based fall-prevention intervention. J Am Geriatr Soc. 2007;55(12):2068–2074. | |
Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM. Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 pt 2):369–374. | |
Crawford CL, Omery A, Seago JA. The challenges of nurse-physician communication: a review of the evidence. J Nurs Adm. 2012;42(12):548–550. | |
The Joint Commission. Sentinel Event Data – Root Causes by Event Type. Oakbrook Terrace, IL: The Joint Commission; 2014. | |
Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194. | |
Whitcomb W. A conversation About Team-Based, Unit-Focused Care With Emory Hospitalist Jason Stein, MD. Philadelphia, PA: Society of Hospital Medicine; 2014. | |
Table 3-H. Percent distribution of the projected population by selected age groups and sex for the United States: 2015 to 2060 (NP2012-T3H). US Census Bureau: Population Division; May 2013. | |
Russo CA, Elixhauser A. Hospitalizations in the Elderly Population, 2003: Statistical Brief #6. Rockville, MD: Agency for Healthcare Research and Quality; 2006. | |
Gordge L, De Young J, Wiechula R. Reducing functional decline of older people in an acute-care setting: are we providing adequate care to maintain/optimise the functional status of our elder patients? Int J Evid Based Healthc. 2009;7(3):181–186. | |
Ahmed N, Taylor K, McDaniel Y, Dyer CB. The role of an acute care for the elderly unit in achieving hospital quality indicators while caring for frail hospitalized elders. Popul Health Manag. 2012;15(4):236–240. | |
Barnes DE, Palmer RM, Kresevic DM, et al. Acute care for elders units produced shorter hospital stays at lower cost while maintaining patients’ functional status. Health Aff (Millwood). 2012;31(6):1227–1236. | |
Kalisch BJ, Lee H, Rochman M. Nursing staff teamwork and job satisfaction. J Nurs Manag. 2010;18(8):938–947. | |
Chang WY, Ma JC, Chiu HT, Lin KC, Lee PH. Job satisfaction and perceptions of quality of patient care, collaboration and teamwork in acute care hospitals. J Adv Nurs. 2009;65(9):1946–1955. | |
Lu H, Barriball KL, Zhang X, While AE. Job satisfaction among hospital nurses revisited: a systematic review. Int J Nurs Stud. 2012;49(8):1017–1038. | |
Aiken L, Clarke S, Sloane D, et al. Nurses’ reports on hospital care in five countries. Health Affairs. 2001;20:43–53. | |
Ritter D. The relationship between healthy work environments and retention of nurses in a hospital setting. J Nurs Manag. 2011;19(1):27–32. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.