Back to Journals » Psychology Research and Behavior Management » Volume 10
Stress and its predictors in pregnant women: a study in Saudi Arabia
Authors Ahmed AE , Albalawi AN, Alshehri AA, AlBlaihed RM, Alsalamah MA
Received 2 January 2017
Accepted for publication 17 March 2017
Published 10 April 2017 Volume 2017:10 Pages 97—102
DOI https://doi.org/10.2147/PRBM.S131474
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Anwar E Ahmed,1 Alhanouf N Albalawi,2 Asmaa A Alshehri,3 Rand M AlBlaihed,2 Majid A Alsalamah4
1King Abdullah International Medical Research Center/College of Public Health and Health Informatics, King Saud bin Abdulaziz University for Health Sciences - MNGHA, Riyadh, Kingdom of Saudi Arabia; 2Riyadh Colleges of Dentistry and Pharmacy, Riyadh, Kingdom of Saudi Arabia; 3College of Dentistry, King Khalid University, Abha, Kingdom of Saudi Arabia; 4College of Medicine, King Saud bin Abdulaziz University for Health Sciences – MNGHA, Riyadh, Kingdom of Saudi Arabia
Background: Although stress during pregnancy has negative effects on children’s development and pregnant women’s health, no study has assessed stress and its predictors among pregnant Saudi women. The aim of this study was to assess stress and identify its predictors in a sample of pregnant Saudi women.
Methods: A correlational study was carried out at King Abdulaziz Medical City in Riyadh, Kingdom of Saudi Arabia, on 438 pregnant women who attended the obstetrics/gynecology clinic. We collected data on their sociodemographic and oral health status. Stress was assessed using the Perceived Stress Scale (PSS).
Results: The sample mean age was 30.6±5.4 years, and 33.4% of the sample reported high stress levels (PSS ≥20). The study revealed significantly high stress levels in women with no or low income, chronic disease, sleep deprivation, no teeth brushing, irregular eating patterns, gestational diabetes, and no family support (P<0.05). Self-reported oral health problems were significantly associated with high stress levels (P<0.05). A multiple linear regression model showed that no teeth brushing, chronic disease, sleep deprivation, gestational diabetes, and gingival redness predicted an increase in stress by a score of 3.6, 2.4, 2.1, 1.4, and 1.4, respectively.
Conclusion: It was estimated that three in ten pregnant women in King Abdulaziz Medical City reported high stress levels. Our study shed light on the relationship between healthy habits, oral health status, and perceived stress in pregnant women. This research may help health care practitioners who provide care to pregnant women, to educate them in regard to healthy habits, and to develop a program to reduce stress.
Keywords: psychosocial stress, oral health, gingivitis, gestational diabetes, pregnant women
Introduction
According to the World Health Organization (WHO), neurological, mental, and substance use disorders are responsible for 14% of the global burden of disease in both men and women.1 Women are more deeply affected by family responsibilities and tended to report higher stress levels than men.2 The lifestyle of women during pregnancy has long-term effects on their overall health, and pregnancy is identified as a sensitive period of increased risk for psychosocial symptoms and poor oral health.3
Stress is very common among women during pregnancy,4 and it can cause adverse birth outcomes such as low birth weight.5,6 According to the literature, several studies reported the rates of psychosocial symptoms during pregnancy for the developed world as between 10 and 15%,7–10 while in developing countries, the rate was found to be 33%.11 There is an association between psychological symptoms and oral health-related problems.12 Psychological symptoms during pregnancy do exist, are prevalent, and are known to have a range of serious effects on women’s health and their born babies.13–15
One study reported that pregnant women adversely affected by psychological symptoms are at high risk for oral diseases.16 Another study reported that up to 30% of pregnant women are impacted by periodontal disease,17 while two more studies showed a positive relationship between stress and periodontal disease-related hormonal changes.12,18 Oral pain during pregnancy had an adverse effect on low-income pregnant Brazilian women and their quality of life, and the study concludes that without maintaining good oral hygiene, oral complications will lead to difficulty in maintaining emotional balance in eating.19 Since oral health affects overall body health, it is important to emphasize maintaining good oral health among pregnant women and promote oral health within this vulnerable population.
Worldwide, many women experience stress during pregnancy.4–10 The current study was undertaken because no study has assessed stress and its predictors among pregnant women in the Kingdom of Saudi Arabia. In this study, we assessed stress using the Perceived Stress Scale (PSS).20 The main aim of the study was to assess the relationships between sociodemographic characteristics, self-reported oral health problems, and perceived stress in a sample of pregnant Saudi women. We hypothesized that self-reported oral health problems and sociodemographic factors may positively increase stress during pregnancy.
Methods
Subjects
A cross-sectional research design was conducted in a sample of pregnant women who visited the obstetrics/gynecology department for a routine checkup at King Abdulaziz Medical City (KAMC) in Riyadh, Kingdom of Saudi Arabia, during the study period (August 14–31, 2016). KAMC is one of the largest tertiary hospitals in the Kingdom of Saudi Arabia.
Ethical considerations
The study was approved by the institutional review board of King Abdullah International Medical Research Center (KAIMRC), Kingdom of Saudi Arabia: research protocol RSS16/003. Each participant received the survey and a letter explaining the aims of the study and a question on whether they wanted to participate in the study. A total of 510 pregnant women were recruited, 438 verbally consented to participate in the study and completed the questionnaire, a response rate of 85.9%. No identifiable information was collected from respondents.
Data collection
A self-report questionnaire was used to gather the data from participants. The study subjects were recruited from the KAMC obstetrics/gynecology outpatient clinic. Data were collected by three dental students. The questionnaire includes sociodemographic and clinical data and dental characteristics: age, educational levels, employment status, income levels, number of children, pregnancy trimester, gestational diabetes, hypertension, sleep deprivation, regular eating patterns, frequently eaten fruits and vegetables, family support, morning sickness, vomiting, dry mouth, gingival redness, gingival bleeding, gingival swelling, pregnancy gingivitis, mouth malodor, dental caries, and dental pain. We assessed symptoms of stress using a translated Arabic version of the PSS-10.21 The Arabic version of the PSS-10 showed high validity and reliability and is a suitable tool to assess stress in Arabic people.21 Subjects were asked to rate each of the following statements (all beginning with: “In the last month”): “how often have you been upset because of something that happened unexpectedly?”; “how often have you felt that you were unable to control the important things in your life?”; “how often have you felt nervous and ‘stressed’?”; “how often have you felt confident about your ability to handle your personal problems?”; “how often have you felt that things were going your way?”; “how often have you found that you could not cope with all the things that you had to do?”; “how often have you been able to control irritations in your life?”; “how often have you felt that you were on top of things?”; “how often have you been angry because of things that were outside of your control?”; and “how often have you felt difficulties were piling up so high that you could not overcome them?” Items were rated on a 5-point Likert scale ranging from 0 – never to 4 – almost always. The PSS-10 ranged between 0 (low stress levels) and 40 (high stress levels). A high-perceived stress level was determined for a score of 20 or higher.20 The questionnaire was found to be reliable in our population with a Cronbach’s alpha of 0.74.
Statistical analysis
Data were analyzed using SPSS version 23 software. We performed univariate analyses and descriptive statistics on all variables (Table 1). Subgroup analyses (independent t-test/analysis of variance test) were used to assess the differences in perceived stress by sociodemographic, clinical, and dental characteristics (Table 1). A multiple linear regression model was employed to identify those predictors that correlated with perceived stress. A P-value of ≤0.05 was considered significant.
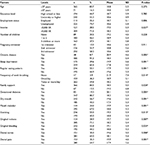  | Table 1 Differences in perceived stress by sociodemographic and clinical data (N=438) Note: *Independent sample t-test is significant at α=0.05. Abbreviations: SD, standard deviation; SR, Saudi Riyal. |
Results
Data from 438 pregnant women were included in the analysis. The mean age of our sample was 30 (± standard deviation [SD] 5.4), with age ranging between 18 and 45 years. Table 1 describes the sample characteristics. More than half (55.3%) of the pregnant women studied had a university degree, 20.5% reported being pregnant with their first child, and 74.7% were unemployed. Table 1 illustrates differences in perceived stress by sociodemographic and clinical data. The prevalence of high-perceived stress in the population studied was (145/434) 33.4% (95% confidence interval: 29.0%, 38.1%). Four participants did not respond to the PSS scale.
Of the sample, 56.9% reported being upset because of something that happened unexpectedly, 65.0% reported being unable to control the important things in their lives, 78.6% felt nervous and “stressed”, 53.0% felt confident about their ability to handle personal problems, 34.7% felt that things were going their way, 76.7% reported that they could not cope with all the things they had to do, 34.3% reported that they were able to control irritations in their lives, 40.2% felt on top of things, 87.9% reported being angry because of things that were outside of their control, and 63.8% felt difficulties were piling up so high that they could not overcome them. There was a non-significant negative correlation between age and perceived stress in pregnant women (r=-0.1, P-value =0.169).
Significant high-perceived stress was reported in women with no or low income, chronic disease, sleep deprivation, irregular eating patterns, no teeth brushing, no family support, and gestational diabetes. Higher perceived stress was found in women with dry mouth, mouth malodor, vomiting, gingival redness, gingival bleeding, dental caries, and dental pain. After adjustment for all possible predictors (Table 2), the stress level of pregnant women with chronic disease, sleep deprivation, no teeth brushing, gestational diabetes, and gingival bleeding was predicted to increase by a score of 2.4, 2.1, 3.6, 1.4, and 1.4, respectively.
Discussion
The study assessed the perceived stress in pregnant women and its predictors. Stress during pregnancy can have long-term effects on the health of the unborn baby, the mother, and offspring development.22,23 This is the first investigation to assess stress in a sample of pregnant Saudi women. The level of perceived stress was relatively high in our sample, with a mean score of 18.6 (± SD 5.3) and a rate of high-perceived stress of 33.4%. Our findings were consistent with other studies using the same PSS-10 version. Slykerman et al24 reported similar mean PSS scores of 18.4 and a similar rate of high-perceived stress of 33.0%. Iranzad et al25 studied social support and its relation to perceived stress in pregnant Iranian women, reporting a mean perceived stress level of 11.5 (± SD 5.5). Reducing stress among pregnant women may require intervention programs.
In our study, no or low income was considered as a determinant of high-perceived stress in pregnant Saudi women. Low household income has been associated with high-perceived stress during pregnancy in Hispanic women.26 Another study reported high stress levels in pregnant Hispanic women who did not know – or refused to report – their household income.27 After adjusting for other predictors, the stress in pregnant women was associated with the presence of chronic diseases and gestational diabetes, which were predicted to increase stress by a score of 2.4 and 1.4, respectively. These findings are consistent with Silveira et al,27 who reported that the odds of gestational diabetes mellitus were 2.6 times higher in women with high stress levels than in those with low stress. In our findings, sleep deprivation was correlated positively with perceived stress. There was evidence to support this statement: a study reported that 90.5% of pregnant women experienced poor sleep quality. Further, the study has linked stress, sleep quality, and unplanned cesarean section among pregnant women.28
In pregnant women, stress may play an important role in their oral health. In our study, several dental problems were reported by pregnant Saudi women, including dry mouth (56.7%), mouth malodor (33%), vomiting (55%), gingival redness (28.9%), gingival bleeding (55.8%), dental caries (35%), and dental pain (35.3%). Subgroup analyses have shown that perceived stress was higher among women with oral health problems (dry mouth, mouth malodor, vomiting, gingival redness, gingival bleeding, dental caries, and dental pain). Similar findings were noted in previous studies, stress has been associated with periodontal disease, including oral pain.12,16–19 It is a novel finding that we have established associations between several oral health problems and stress patterns. Multivariate analysis has shown that gingival redness predicted to increase perceived stress by a score of 1.4. This could help health care practitioners, as oral health is an important component of pregnant women’s health, and should be managed and maintained appropriately during pregnancy, along with stress.
The study has a number of limitations. We measured stress based on the PSS scale and not by a psychologist or mental health care specialist. We used a cut-off point of 20 or higher to identify women with high stress levels, a cut-off recommended by Cohen et al.20 Findings of the study must be interpreted with caution as they represent associations but not causations. Further research studies are warranted to evaluate the stress and oral health status of Saudi women before, during, and after pregnancy. Our findings may only represent pregnant Saudi women attending the KAMC obstetrics/gynecology department for a routine checkup.
Conclusion
The findings were consistent with previous international studies indicating that the rate of perceived stress level during pregnancy was high: three in ten pregnant Saudi women in KAMC reported high stress levels. Pregnant women with no or low income, chronic disease, sleep deprivation, no family support, irregular eating patterns, gestational diabetes, and poor oral health reported high levels of stress. This research may benefit health care practitioners who provide care for pregnant women, to educate such women regarding oral health and healthy eating habits, and to develop programs to reduce stress in this population.
Acknowledgments
The authors would like to thank King Abdullah International Medical Research Center (KAIMRC), Riyadh, Kingdom of Saudi Arabia, for approving and partially funding this study. The abstract of this paper was presented at the OMICS International 3rd Annual Congress & Medicare Expo on Primary Healthcare April 17–19, 2017, Dubai, UAE as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in OMICS Oral Health Dental Management 2016. The abstract of this paper was presented at the OMICS 17th World Congress on Oral Care and Probiotics November 14–16, 2016 in Orlando, USA as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in OMICS Oral Health Dental Management 2016. The abstract of this paper was presented at the OMICS 15th Euro Congress on Dental & Oral Health October 24–26, 2016 in Rome, Italy as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in OMICS Dentistry 2016.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Scaling up care for mental, neurological, and substance use disorders: mental health Gap Action Programme (mhGAP). World Health Organization; 2008. Available from: www.who.int/mental_health/mhgap_final_english.pdf. Accessed March 20, 2017. | ||
Herrero SG, Saldaña MÁ, Rodriguez JG, Ritzel DO. Influence of task demands on occupational stress: gender differences. J Safety Res. 2012;43(5–6):365–374. | ||
Vamos CA, Walsh ML, Thompson E, Daley EM, Detman L, DeBate R. Oral-systemic health during pregnancy: exploring prenatal and oral health providers’ information, motivation and behavioral skills. Matern Child Health J. 2015;19(6):1263–1275. | ||
Woods SM, Melville JL, Guo Y, Fan MY, Gavin A. Psychosocial stress during pregnancy. Am J Obstet Gynecol. 2010;202(1):61.e1–e7. | ||
Newton RW, Hunt LP. Psychosocial stress in pregnancy and its relation to low birth weight. Br Med J (Clin Res Ed). 1984;288(6425):1191–1194. | ||
Loomans EM, Van Dijk AE, Vrijkotte TG, et al. Psychosocial stress during pregnancy is related to adverse birth outcomes: results from a large multi-ethnic community-based birth cohort. Eur J Public Health. 2013;23(3):485–491. | ||
Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. 2001;323(7307):257–260. | ||
Heron J, O’Connor TG, Evans J, Golding J, Glover V; ALSPAC Study Team. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80(1):65–73. | ||
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–1024. | ||
Meijer JL, Beijers C, van Pampus MG, et al. Predictive accuracy of Edinburgh postnatal depression scale assessment during pregnancy for the risk of developing postpartum depressive symptoms: a prospective cohort study. BJOG. 2014;121(13):1604–1610. | ||
Gausia K, Fisher C, Ali M, Oosthuizen J. Antenatal depression and suicidal ideation among rural Bangladeshi women: a community-based study. Arch Womens Ment Health. 2009;12(5):351–358. | ||
Peruzzo DC, Benatti BB, Ambrosano GM, et al. A systematic review of stress and psychological factors as possible risk factors for periodontal disease. J Periodontol. 2007;78(8):1491–1504. | ||
Evans J, Heron J, Patel RR, Wiles N. Depressive symptoms during pregnancy and low birth weight at term: longitudinal study. Br J Psychiatry. 2007;191:84–85. | ||
Wadhwa PD, Sandman CA, Porto M, Dunkel-Schetter C, Garite TJ. The association between prenatal stress and infant birth weight and gestational age at birth: a prospective investigation. Am J Obstet Gynecol. 1993;169(4):858–865. | ||
Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, Meyer BA. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol. 2008;27(5):604–615. | ||
Silveira ML, Whitcomb BW, Pekow P, Carbone ET, Chasan-Taber L. Anxiety, depression, and oral health among US pregnant women: 2010 Behavioral Risk Factor Surveillance System. J Public Health Dent. 2016;76(1):56–64. | ||
Kumar J, Samelson R. Oral health care during pregnancy and early childhood: practice guidelines. New York, NY: New York State Department of Health; 2006. | ||
Laine MA. Effect of pregnancy on periodontal and dental health. Acta Odontol Scand. 2002;60(5):257–264. | ||
de Oliveira BH, Nadanovsky P. The impact of oral pain on quality of life during pregnancy in low-income Brazilian women. J Orofac Pain. 2006;20(4):297–305. | ||
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. | ||
Chaaya M, Osman H, Naassan G, Mahfoud Z. Validation of the Arabic version of the Cohen Perceived Stress Scale (PSS-10) among pregnant and postpartum women. BMC Psychiatry. 2010;10:111. | ||
Huizink AC, Robles de Medina PG, Mulder EJ, Visser GH, Buitelaar JK. Stress during pregnancy is associated with developmental outcome in infancy. J Child Psychol Psychiatry. 2003;44(6):810–888. | ||
Van Assche FA, Holemans K, Aerts L. Long-term consequences for offspring of diabetes during pregnancy. Br Med Bull. 2001;60:173–182. | ||
Slykerman RF, Thompson JM, Pryor JE, et al. Maternal stress, social support and preschool children’s intelligence. Early Hum Dev. 2005;81(10):815–821. | ||
Iranzad I, Bani S, Hasanpour S, Mohammadalizadeh S, Mirghafourvand M. Perceived social support and stress among pregnant women at health centers of Iran-Tabriz. J Caring Sci. 2014;3(4):287–295. | ||
Silveira ML, Pekow PS, Dole N, Markenson G, Chasan-Taber L. Correlates of high perceived stress among pregnant Hispanic women in Western Massachusetts. Matern Child Health J. 2013;17(6):1138–1150. | ||
Silveira ML, Whitcomb BW, Pekow P, et al. Perceived psychosocial stress and glucose intolerance among pregnant Hispanic women. Diabetes Metab. 2014;40(6):466–475. | ||
Ko YL, Lin PC, Chen SC. Stress, sleep quality and unplanned Caesarean section in pregnant women. Int J Nurs Pract. 2015;21(5):454–461. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

