Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Stimulus intensity determined by dose-titration versus age-based methods in electroconvulsive therapy in Thai patients
Authors Ittasakul P , Likitnukul A , Pitidhammabhorn U, Waleeprakhon P, Goldman MB
Received 14 September 2018
Accepted for publication 4 January 2019
Published 7 February 2019 Volume 2019:15 Pages 429—434
DOI https://doi.org/10.2147/NDT.S187589
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Yuping Ning
Pichai Ittasakul,1 Apichaya Likitnukul,1 Umporn Pitidhrammabhorn,1 Punjaporn Waleeprakhon,1 Morris B Goldman2
1Department of Psychiatry, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 2Department of Psychiatry and Behavioral Sciences, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
Objectives: This study aimed to compare the accuracy of the stimulus intensity (SI) calculated by age-based methods with that using the dose-titration method.
Methods: The initial seizure threshold (IST) was determined using a standardized dose titration in hospitalized Thai patients treated with right unilateral (RUL, n=32) and bilateral (BL, n=57) electrode placement. The correlation between the IST and clinical variables was analyzed. The estimated SI based on the patient’s age was compared with the SI determined by dose titration.
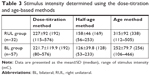
Results: Age was highly predictive of the IST for both groups (RUL, P=0.012; BL, P=0.045). Gender (P=0.006) and anticholinergic drug use (P=0.025) predicted the IST for the BL group. For the RUL group, the mean±SD (median) SI estimated using the half-age and age methods was 158±46 (169) mC and 315±92 (338) mC, respectively. The SI determined using the dose-titration method was higher compared with the half-age method and lower compared with the age method. For the RUL group, 31% of subjects using the half-age method and 22% of subjects using the age method would have received an SI within ±20% of that computed using dose titration. Additionally, 19% of subjects using the half-age method and 19% using the age method would have received unacceptably low (<50%) or high (>200%) intensities. For the BL group, 18% of subjects using the half-age method and 32% using the age method would have received an SI within ±20% of that computed using dose titration. Additionally, 39% with the half-age method and 18% with the age method would have received an unacceptably low or high SI, respectively.
Conclusion: Age strongly predicts the IST, but it does not robustly predict the SI compared with dose titration because the SI calculated using age-based methods results in an unacceptably low or high SI that is associated with a marked risk of adverse effects or inadequate response. We recommend the dose-titration method to determine the SI.
Keywords: electroconvulsive therapy, dosing, Thai patients, dose titration, age-based methods, seizure threshold, predictors
Introduction
The stimulus intensity (SI) is a critical feature of electroconvulsive therapy (ECT) because it must be substantially above the initial seizure threshold (IST) for the treatment to be effective but not so high that it unnecessarily increases the risk of cognitive side effects.1,2 Currently, the recommended SI is 50%–100% and 150%–500% above the IST for brief pulse bilateral (BL) and brief pulse right unilateral (RUL) ECT, respectively.3 The IST, which is generally defined as the minimum electrical charge needed to produce a generalized seizure lasting at least 20–25 s, exhibits marked variability (ie, 40–50-fold) between patients.1,2 Previous studies indicate that age, sex, concurrent medication, electrode placement, anesthetic agents, past ECT, and body mass index (BMI) all contribute to this variability.4–8
Two methods are typically used to calculate the SI: the dose-titration method1 and the age-based method.9–11 The dose-titration method is generally considered the “gold standard” and seeks to determine the actual IST in a single session. However, the dose-titration method typically involves nontherapeutic treatment and is associated with a risk of potential adverse effects related to restimulation.9 The age-based methods estimate the SI based on the patient’s age.3,7,12 Age (age method) or one-half of the age (half-age method) is used as a percentage of the maximum output charge to calculate the ST at the first treatment. The age-based methods, however, have the potential to cause otherwise avoidable cognitive side effects and to lengthen the duration of treatment and cumulative exposure to the risk factors.3,11,13,14
In a previous study in Thai patients, Chanpattana et al found that the ST for BL ECT determined using the dose-titration method was proportional to the patient’s age15 and lower than that calculated using either the half-age or age method.16 Additionally, the impact of ethnicity on the IST and SI remains unknown. In the current study, we compared the accuracy of the SI calculated using age-based methods with that of the dose-titration method in Thai subjects who received either RUL or BL ECT.
Materials and methods
Setting and study design
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee on Human Experimentation of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand. Ramathibodi Hospital is a 1,300-bed university hospital with a 22-bed general psychiatric unit. There are 250–300 patients admitted per year,17 and approximately 10% of these patients receive ECT.18
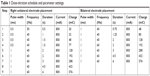
The study design is retrospective. We performed chart reviews on all patients who received inpatient ECT from January 2013 to September 2016. Patients provided verbal and written informed consent before participation. Data collected were age, gender, BMI, concurrent use of psychotropic medications, history of previous ECT, psychiatric diagnosis, electrode placement, IST, and anesthetic agents.
Electroconvulsive therapy treatment
At least one psychiatrist involved in this manuscript oversaw each patient’s ECT. All patients were assessed by psychiatry and anesthesiology before receiving ECT. Benzodiazepines were discontinued at least 15 h before treatment, which was conducted in the postanesthetic care unit. A modified technique involving a brief pulse wave generated by a Mecta Spectrum 5000Q (Mecta Corp, Portland, OR, USA) was applied typically after thiopental (1–6 mg/kg intravenously (IV)) or propofol (1–2 mg/kg IV) anesthesia and succinylcholine (0.5–1 mg/kg IV) muscle relaxant were administered. ECT was performed three times per week. The titration schedule was standardized (Table 1) but other clinical decisions were made at the physician’s discretion.
  | Table 1 Dose-titration schedule and parameter settings |
Determination of the initial seizure threshold
The IST was determined at the first ECT session using the dose-titration method as shown in Table 1, except that males started at Step 2. The method of electrode placement (BL or RUL) was determined by the symptom severity, as determined by the treating psychiatrist. The IST was defined as the dose at which there was definite evidence on the electroencephalogram of generalized seizure activity for at least 25 s. None of the patients was administered more than four stimulus doses. The subsequent SI was calculated using 6×IST for the RUL electrode placement and 1.5×IST for the BL electrode placement.
Statistical analysis
All statistical analysis was performed using SPSS 21.0 for Windows (IBM Corporation, Armonk, NY, USA). Data are presented using the mean±SD and percentage for continuous and categorical outcomes, respectively. An assessment of the data distribution was performed to determine the appropriate statistical test. Correlation between the IST and demographic data, clinical characteristics, and ECT variables was performed using Spearman’s rho because the data were not normally distributed. For the age-based IST calculation, a percentage of the maximum output charge (576 mC) determined by the patient’s age or half of their age was used. Multivariate ordinal regression was used to examine the relationship of the IST to demographic and clinical variables. P<0.05 was considered statistically significant.
Results
Demographic characteristics of the subjects
Ninety psychiatric inpatients had received ECT using the dose-titration method. Among these 90 patients, 57 patients received BL and the other 33 patients received RUL. Among the 33 patients who received RUL, one patient received ketamine as the anesthetic agent and was therefore not included in our study. Subjects’ demographic characteristics are presented in Table 2. For the RUL group, the age range was 19.5–87.7 years. For the BL group, the age range was 18.3–80.9 years.
  | Table 2 Demographic characteristics |
The initial seizure threshold and associated factors
For the RUL group, the mean±SD (median) IST was 42±21 mC (32 mC), with a range of 19–128 mC. The IST for males was 50±28 mC (48 mC) and that for females was 38±15 mC (32 mC) (Mann–Whitney U=81, z=−1.5, P=0.146). Three outliers (IST≥76) were excluded from the analysis. Age was associated with a higher IST (rs=0.465, P=0.011). For the multivariate ordinal regression analysis, only age predicted the IST (P=0.012).
For the BL group, the mean±SD (median) IST was 150±101 mC (128 mC), with a range of 32–576 mC. For males, the IST was 190±120 mC (128 mC) and for females, it was 114±62 mC (104 mC) (Mann–Whitney U=228, z=−2.9, P=0.003). For subjects who were taking concurrent anticholinergic medication, the IST was 105±72 mC (80 mC) and for subjects who were not taking concurrent anticholinergic medications, it was 162±104 mC (128 mC) (Mann–Whitney U=155.5, z=-2.3, P=0.021). The two outliers (IST>400 mC) were excluded from the analysis. Age was associated with a higher IST (rs=0.271, P=0.045), male gender was associated with a higher IST (rs=0.351, P=0.009), and taking an anticholinergic medication was associated with a lower IST (rs=-0.295, P=0.029). For other concurrent medications such as benzodiazepines, antipsychotics, antidepressants, and anticonvulsants, BMI and anesthetic agents were not associated significantly with the IST. The goodness of fit was calculated for the multivariate ordinal regression analysis (c2=318.4, df=1, P=0.531). Age (P=0.021), male gender (P=0.006), and no concurrent anticholinergic medications (P=0.025) were associated with a higher IST.
Comparison of the stimulus intensity using dose-titration and age-based methods
The SI determined using the dose-titration method and the stimulus dose used in the first treatment for both the RUL and BL groups was higher compared with that calculated using the half-age method and lower compared with that calculated using the age method (Table 3).
In the RUL group (n=32), using the half-age method, six (18.8%; Figure 1, left) subjects would have received at least the SI that was computed using the dose-titration method. However, using the age method, 26 (81.3%) subjects (Figure 1, right) would have received at least the SI that was computed using the dose-titration method. Figure 1 also reveals that ten (31.3%) subjects using the half-age method and seven (21.9%) subjects using the age method would have received a SI within ±20% of that computed using the dose-titration method. Additionally, six (18.8%) subjects using the half-age method and six (18.8%) subjects using the age method would have received a SI at least twice (200%) or less than one-half (50%) of that computed using the dose-titration method. The SI was in the range 1.5–8.6 times the subject’s IST, when determined using the half-age method and in the range 2.9–17.2 times the subject’s IST, when determined using the age method.
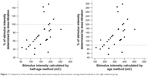  | Figure 1 Comparison of the stimulus intensity determined using the dose-titration and age-based methods in the right unilateral group. |
In summary, neither age-based method provided an accurate prediction of the SI (ie, ±20%).
For the BL group (n=57), nine (15.8%) subjects using the half-age method (Figure 2, left) and 35 (61.4%) subjects using the age method (Figure 2, right) would have received at least the SI computed using the dose-titration method. Figure 2 also shows that ten (17.5%) subjects using the half-age method and 18 (31.6%) subjects using the age method would have received an SI within ±20% of that computed using the dose-titration method. Additionally, 22 (38.6%) subjects using the half-age method and ten (17.5%) subjects using the age method would have received a SI at least twice (200%) or less than one-half (50%) of that computed using the dose-titration method. The SI was in the range 0.3–4.8 times the subject’s IST for the half-age method and in the range 0.6–9.6 times the subject’s IST for the age method.
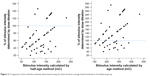  | Figure 2 Comparison of the stimulus intensity determined using the dose-titration and age-based methods in the bilateral group. |
Discussion
In our study, we found that the mean IST was 42 mC and 150 mC for the RUL and BL group, respectively. The variability in the IST was 6.7-fold for the RUL group and 18-fold for the BL group. As expected, age strongly influenced the IST for both the RUL and BL groups. Additionally, gender and concurrent anticholinergic drugs influenced the IST for the BL group. These findings are consistent with previous studies on IST variability and factors influencing the IST (such as age, sex, anticholinergic drugs).15,19,20 The SI determined using the dose-titration method was higher compared with that calculated using the half-age method and lower compared with that calculated using the age method (Table 3). The calculated SI for RUL using either the age or half-age method was in the range (±20%) of the SI obtained using the gold standard dose-titration method for only about 20%–30% of the subjects. A slightly lower percentage for both groups was markedly outside this range (ie, >200% or <50%). The overall accuracy of the two methods did not appear to be different, but it is important to note that the SI calculated using the age method is more likely to produce a therapeutic response although there is a commensurate increase in the risk of adverse effects. For the BL treatment, the age method appeared to be consistently better than the half-age method across the different indices. Fifty percent more subjects were within the range determined using the dose-titration method (32% vs 18%), and fewer than half (18% vs 39%) as many were markedly outside this range. Still fewer than half of the subjects appeared to be within the desired range using the age method.
For the RUL group, the SI may be high – up to 17.2 times higher than the subject’s IST obtained using the age method. This result was consistent with a previous study from Australia which showed that the SI determined using the age method led to an excessive SI (seven or more times higher than the IST) compared with that calculated using the dose-titration method in 30% of female subjects and 8% of male subjects who were treated with RUL ECT.12 For the BL group, the SI may be high – up to 4.8 times higher than a subject’s IST calculated using the half-age method and 9.6 times higher than a subject’s IST calculated using the age method. Although using the SI calculated by the age method would have resulted in successful stimulation on the first attempt in most patients by delivering an overestimated SI, this might cause cognitive side effects.
The study has several limitations. First, subjects included in this study were all inpatients at a university hospital in Thailand, so the results should be interpreted with caution in other settings. Second, this is a retrospective study so some information was missing. Third, there are other factors that might influence the IST, which were not identified in this clinical sample (eg, underlying neurological disease or substance use). Fourth, the IST was based on intervals, not a continuous charge. Fifth, the titration schedule differed by gender and electrode placement. Perhaps most important is that while the dose-titration method is the gold standard, we do not know if or how actual clinical outcomes would vary if the different methods were compared. Furthermore, our measures of adequacy (ie, ±20% was acceptable; >200% or <50% was highly undesirable) are somewhat arbitrary. Finally, there may also be other factors influencing the IST that should be taken into account when estimating the threshold. Thus, while we confirm the influence of age, we also confirm the influence of concurrent anticholinergic drugs, which along with BMI, concurrent psychotropic medications, and history of previous ECT may warrant further study.
Conclusion
The two age-based methods did not provide a robust substitute for the SI calculated using the dose-titration method. In particular, both methods showed equally poor results when RUL treatment was applied, and while the age-based method was superior for BL, it still appeared to expose nearly 20% of patients to unacceptably high or low charges. Thus, the dose-titration method is still recommended to determine the SI.
Acknowledgment
Special thanks to Umaporn Udomsubpayakul for statistics recommendations.
Disclosure
Pichai Ittasakul, Apichaya Likitnukul, Umporn Pitidhrammabhorn, and Punjaporn Waleeprakhon have received salary support from Mahidol University, Bangkok, Thailand. Morris B Goldman receives funding from Otsuka Pharmaceuticals. All authors declare that their funding/salary support sources (Mahidol University and Otsuka Pharmaceuticals) had no impact on the study design, data collection, analysis, and interpretation, writing the report, or the decision to submit the study for publication. The authors report no other conflicts of interest in this work.
References
Sackeim HA, Devanand DP, Prudic J. Stimulus intensity, seizure threshold, and seizure duration: impact on the efficacy and safety of electroconvulsive therapy. Psychiatr Clin North Am. 1991;14(4):803–843. | ||
Sackeim HA, Prudic J, Devanand DP, et al. Effects of stimulus intensity and electrode placement on the efficacy and cognitive effects of electroconvulsive therapy. N Engl J Med Overseas Ed. 1993;328(12):839–846. | ||
Mankad MV, Beyer JL, Weiner RD, Krystal AD. Clinical Manual of Electroconvulsive Therapy. Arlington: American Psychiatric Publishing; 2010. | ||
Chung KF, Wong SJ. Initial seizure threshold of bilateral electroconvulsive therapy in Chinese. J Ect. 2001;17(4):254–258. | ||
Petrides G, Braga RJ, Fink M, et al. Seizure threshold in a large sample: implications for stimulus dosing strategies in bilateral electroconvulsive therapy: a report from core. J Ect. 2009;25(4):232–237. | ||
van Waarde JA, Verwey B, van der Mast RC. Meta-analysis of initial seizure thresholds in electroconvulsive therapy. Eur Arch Psychiatry Clin Neurosci. 2009;259(8):467–474. | ||
Yasuda K, Kobayashi K, Yamaguchi M, et al. Seizure threshold and the half-age method in bilateral electroconvulsive therapy in Japanese patients. Psychiatry Clin Neurosci. 2015;69(1):49–54. | ||
Gálvez V, Hadzi-Pavlovic D, Smith D, Loo CK. Predictors of seizure threshold in right unilateral ultrabrief electroconvulsive therapy: role of concomitant medications and anaesthesia used. Brain Stimul. 2015;8(3):486–492. | ||
American Psychiatric Association. The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging: A Task Force Report of the American Psychiatric Association. 2nd ed. Washington, DC: American Psychiatric Publishing; 2001. | ||
Petrides G, Fink M. The “half-age” stimulation strategy for ECT dosing. Convuls Ther. 1996;12(3):138–146. | ||
Abrams R. Electroconvulsive Therapy. 4th ed. New York: Oxford University Press; 2002. | ||
Tiller JW, Ingram N. Seizure threshold determination for electroconvulsive therapy: stimulus dose titration versus age-based estimations. Aust N Z J Psychiatry. 2006;40(2):188–192. | ||
Aten JJ, Oudega M, van Exel E, Stek ML, van Waarde JA. Repeated dose titration versus age-based method in electroconvulsive therapy: a pilot study. Eur Arch Psychiatry Clin Neurosci. 2015;265(4):351–356. | ||
Bennett DM, Perrin JS, Currie J, et al. A comparison of ECT dosing methods using a clinical sample. J Affect Disord. 2012;141(2–3):222–226. | ||
Chanpattana W, Chakrabhand ML, Kitaroonchai W, Choovanichvong S, Techakasem P, Yatapootanon W. Seizure threshold in ECT: I. Initial seizure threshold. J Med Assoc Thai. 2000;83(5):529–535. | ||
Chanpattana W, Chakrabhand S, Techakasem P, Raksakietisak S. Seizure threshold in ECT: II. Dose titration vs age and half age methods. J Med Assoc Thai. 2000;83(3):278–283. | ||
Samrankitdamrong W, Ittasakul P. Prevalence of mental disorders and characteristics of psychiatric patient in inpatient unit in Ramathibodi Hospital. J Psychiatr Assoc Thailand. 2013;58(4):433–442. | ||
Pitidhrammabhorn U, Ittasakul P, Waleeprakhon P, Goldman MB. Clinical characteristics of inpatients undergoing electroconvulsive therapy (ECT) in a university hospital, Thailand. ASEAN J Psychiatry. 2016;17(2):144–150. | ||
Boylan LS, Haskett RF, Mulsant BH, et al. Determinants of seizure threshold in ECT: benzodiazepine use, anesthetic dosage, and other factors. J Ect. 2000;16(1):3–18. | ||
Coffey CE, Lucke J, Weiner RD, Krystal AD, Aque M. Seizure threshold in electroconvulsive therapy: I. Initial seizure threshold. Biol Psychiatry. 1995;37(10):713–720. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.