Back to Journals » Advances in Medical Education and Practice » Volume 13
Step-by-Step Method Combined with Simulation-Enhanced Learner Outcomes in Minimally Invasive Breast Surgery Education
Authors Wang Q, Li Z, Huang X, Fu X, Li Q, Li H
Received 21 March 2022
Accepted for publication 31 August 2022
Published 12 September 2022 Volume 2022:13 Pages 1051—1060
DOI https://doi.org/10.2147/AMEP.S367304
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Qinbo Wang,1– 3,* Zongyan Li,1,* Xiaojia Huang,1 Xiaoyan Fu,1 Qian Li,1 Haiyan Li1,3
1Department of Breast Surgery, The Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou, People’s Republic of China; 2Department of Pharmacy, The Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou, People’s Republic of China; 3Department of Graceland Medical Center, The Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Haiyan Li, Department of Breast Surgery, the Sixth Affiliated Hospital, Sun Yat-Sen University, 26# Erheng Road, Yuan Village, Tianhe District, Guangzhou, 510655, People’s Republic of China, Email [email protected]
Purpose: Traditional standardized training in ultrasound-guided minimally invasive breast surgery (UMIBS) focused on lecture-based learning (LBL) resulted in students’ insufficient analysis, limited spatial visual conversion ability, and poor practical application. This study examined the effects of the step-by-step (SBS) method combined with a simulation model in UMIBS education.
Subjects and Methods: A total of 84 residents participated in this study. The residents were divided into the SBS group (experience group, n=42) and the LBL group (control group, n=42), and the same teacher taught the two groups to ensure a comparable result. Based on the pork simulation model, two experts evaluated student performance scores, and the total time taken by each student was also counted. The participants were surveyed with 7 questions after the training, and each answer was assigned a score of 1, 2 or 3 to compare the participants’ satisfaction.
Results: The average value of the surgical skills for SBS group were significantly higher than LBS group, which was 82.8± 4.4 and 72.7± 4.0 (t=4.27, P< 0.001), the time spend of neoplasm localization by the experience group was significantly less than the control group, which was 17.9± 1.6 and 20.9± 1.2 secs, (t=1.58, P< 0.001), and there were significant differences in puncture accuracy and excision integrity between the two groups (P< 0.05). In addition, the results of the questionnaire survey showed that learning interest, surgical ability and satisfaction were better in the SBS group than in the LBS group (P< 0.05), and there were no significant differences in clinical thinking and learning pressure between the two groups.
Conclusion: The SBS teaching method may help to improve the surgical skills and learning interest, as well as reduce adverse reactions and cultivate clinical thinking of the students in UMIBS training. Future studies could consider multicenter clinical research to further confirm the practicality of this teaching method and reduce the risk of deviation.
Keywords: ultrasound, minimally invasive, step by step, lecture-based learning, simulation
Plain Language Summary
Given the strong professionalism of the technology and limited educational resources, there was decreased student operative time and limited communication between teachers and students. Current and future UMIBS training programs should combine practical skills with theoretical knowledge to promote hand-eye cooperation, spatial vision conversion ability, and a certain degree of B-scanning ability and establish the concept of three-dimensional resection. Validity and fidelity training models are essential for UMIBS skill training.
Introduction
With medical technology continuing to accumulate and advance today, ultrasound-guided minimally invasive breast surgery (UMIBS) has been widely used in the diagnosis and treatment of breast disease with the aim of reducing surgical complications and maintaining the esthetic appearance of the breast.1–3 The literature on UMIBS has mainly reported its efficacy and prognosis but has rarely reported the teaching method.4,5 The rapid development of UMIBS and the lag of the efficiency teaching mode put forward higher requirements for medical educators.
The current well-known training method for UMIBS focuses on lecture-based learning (LBL), which means that teachers lead the class but students rarely have the opportunity to practice.6,7 However, due to this lack of practice and clinical thinking during the training process, students cannot carry out clinical operations after watching the procedure,8–10 and restrictions have prompted educators to seek alternative methods to teach medical knowledge and gain procedural experience. UMIBS is a highly practical subject; in response to its practical nature, it is imperative for medical educators to employ a simulation and teaching mode to practice operational ability.11,12
In the present study, we adopted the step-by-step (SBS) method combined with a simulation model in UMIBS teaching. SBS is a method to practice surgical processes in different stages. Each step involved demonstration, deconstruction and practice, and skinned pork with mammary glands was used to simulate human breasts. SBS stage education has been applied in many medical disciplines.13,14 However, the application of SBS in UMIBS teaching has not yet been reported. Based on the simulation model, by comparison with traditional LBL, the effects of SBS and LBL teaching methods in UMIBS training were analyzed to explore the application of the step-by-step (SBS) method in UMIBS training.
Materials and Methods
Teaching Implementation
A total of 84 residents participated in UMIBS training. Participants were divided into two groups: Group A was trained with the SBS method, and Group B was trained with the LBS method. Both groups were taught by the same teacher and used the same pork simulation model to ensure the comparability of teaching effects; meanwhile, the teacher and students did not know the plan in advance. All students were told to learn the same content in advance, but the course structure was different.
Simulation Model
Skinned pork with mammary gland was used to simulate human breast tissue,15 and a 1 cm length of Chinese pickled mustard was placed in the pork where the mammary gland area was marked to simulate the breast lesion. During the assessment, learners needed to take out the pickled mustard from the pork tissue by using a puncture needle under the guidance of ultrasound, as shown in Figure 1. Through professional skills evaluation and a questionnaire survey in two groups, we compared the effects of the two methods in teaching UMIBS.
SBS Method
There were five steps in the SBS method. First, during ultrasound training, students practiced ultrasound procedures to learn the anatomical structure of the breast. Second, for the identification of neoplasms, students identified the breast masses through ultrasonic examination at the outpatient clinic and reexamined surgical traces of postoperative patients. Third, for simulation model training, students were supposed to pick up pickled mustard from the pork tissue model, scored with Visual Analog Scoring. Fourth, for operation procedure training, according to color Doppler ultrasound, mammography, CT or MR results, students were required to report the case, clarify the operation indications, and show the surgical path before the surgery, propounded prevention suggestions for possible complications and prepared surgery conversations. During the operation, students could ask questions, and the teacher explained the surgery skills and precautions. After surgery, students recorded the operation records and the teacher revised them. Fifth, during ward round tracking, students monitored postoperative recovery, analyzed the common complications, and then made a standardized postoperative rehabilitation plan, and the teacher corrected analysis deviations. The total time taken was 180 mins, and the sum of each practice step was 100 mins, as shown in Figure 2.
 |
Figure 2 Course structure of LBL group and SBS group. |
LBL Method
Study was arranged for the LBL control group in which the teacher explained the theory for 30 mins first, then demonstrated the main parts of the operation for 50 mins, and finally reserved 100 mins for the learners to practice. The time spent in each step is shown in Figure 2. Students could ask the teacher questions during the practice, and the teacher helped students solve the problems they encountered. After the course, it was arranged for two breast experts who had more than 5 years of experience to evaluate the students’ performance independently, and the two experts did not know which courses the learner had taken.
Assessment Methods
Evaluation of Localization Ability
Before resection, students were required to locate the mass accurately and searched for the maximum resection plane while measuring the size of the neoplasm to define the margin of excision. Two experts calculated the time independently to evaluate the precise localization ability in the two groups while finding the maximum section and measured the size of the tumor under ultrasound. The shorter the time needed, the better the localization ability.
Ultrasound-Guided Puncture Accuracy
During UMIBS, the puncture needle should be placed directly below the tumor to ensure accuracy. If the length of the puncture needle in the skin is equal to the length shown under ultrasound when the maximum section is exposed, then the puncture needle is parallel to the neoplasm without forming an angle. In contrast, if the length of the puncture needle in the skin is longer than the length indicated by the ultrasound, the puncture needle is not properly placed under the neoplasm. The puncture ability was counted as ultrasound display length/penetration length×100 to evaluate the puncture accuracy of the two groups. The larger the value is, the higher the puncture accuracy.
The puncture needle display length was used to compare the puncture needle penetration length ratio to evaluate the puncture needle application ability of the two groups of students before and after training. The larger the ratio is, the better the students’ ability to guide the puncture needle by B-ultrasound.
Using the needle length of the display contrast ratio of the length of the needle into the skin puncture needle to evaluate two participants before and after training application ability, the greater the ratio B ultrasound-guided needle participants’ better capacity.
Completeness of Neoplasm Excision
The surgical outcome is closely related to the completeness of neoplasm excision; it is easy to relapse if the neoplasm is not completely removed. There are no pieces of pickled mustard left if the neoplasm was resected thoroughly; conversely, there are residual pieces. Therefore, the excision integrity was counted as (1- residual mustard scale/initial mustard scale) ×100). The initial mustard scale was 5 grams.
Theoretical and Operational Assessments
The theoretical examination included knowledge of breast diseases, anatomy, complications, analysis and treatment of typical cases, essentials and postoperative treatment procedures. The operational assessment included the familiarity with the surgery, puncture application skills, resection accuracy, etc., which were based on the UMIBS procedure, proficiency and surgical results.
Questionnaire
Two groups were investigated anonymously to evaluate the training effects of the two methods. The questionnaire included interest, surgical ability, practical ability, reduction of surgical complication, clinical pressure and satisfaction.
Statistical Analysis
SPSS 22.0 software (SPSS Inc., Chicago, IL, USA) was used for data analysis. Normally distributed data are represented as the mean ± standard deviation, and the heterogeneity of the two groups was compared with a t-test. The chi-square test was used to evaluate the percentage and difference between the two groups, and the Kruskal–Wallis test was used to compare the categorical data. Values of P<0.05 were considered statistically significant.
Results
Comparison Between the Participants of the Two Groups Before Training
A total of 84 surgeons who participated in UMIBS training at the Department of Breast Surgery in the Sixth Affiliated Hospital of Sun Yat-sen University from January 1, 2021, to December 31, 2021, were enrolled. A nonrandomized controlled trial was conducted, with 42 participants allocated to Group A (35 men, 7 women) and 42 participants allocated to Group B (39 men, 3 women). The teachers in both groups were chief or deputy chief surgeons, and no students had ever performed UMIBS before. Group A was conducted with the SBS method, and Group B was conducted with LBL. Students volunteered to participate, and the mean ages of the students from Group A and Group B were 27.3±2.7 and 28.2±2.4 years respectively. There were no significant differences between the two groups in terms of age, educational background, or standardized training duration (p˃0.05; shown in Table 1).
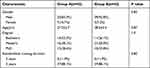 |
Table 1 Characteristics of All the Participants |
The Evaluation of Theory and Surgical Techniques Between the Two Groups
Through theoretical examination and surgical technique assessment, we objectively compared the training effects between the two groups. There were no significant differences in theoretical knowledge and surgical technique between the two groups before the training (p˃0.05), and the grades improved for both groups after the training. In particular, the grades for both theoretical knowledge and surgical technique in Group A were significantly higher than those in Group B (p<0.001; shown in Table 2, Figure 3), which means that the SBS method was more effective than the LBL method in UMIBS training.
 |
Table 2 Evaluation of Theory and Surgical Skills Before and After Training |
 |
Figure 3 Evaluation of training effects in the two groups. We compared the grades of the students in theoretical knowledge and surgical skills (100 points for each). **p<0.001, by a t-test. |
The Evaluation of Surgery Skills Between the Two Groups
To assess the training effects of the two methods, we counted the ultrasound localization time and evaluated the puncture accuracy and completeness of neoplasm excision by two experts. After the training, the real-time duration of the experience group was significantly less than that of the control group, which was 17.9±1.6 and 20.9±1.2 secs, respectively (t=1.58, p<0.001). In addition, there were significant differences between the SBS and LBL groups in terms of puncture techniques (t=4.49, p<0.001), the values were 88.9±3.2 and 81.9±4.7, respectively, and completeness of neoplasm excision (t=1.27, p<0.001), the values were 88.9±3.2 and 81.9±4.7, respectively (p<0.001; shown in Table 3). These results showed that the SBS training method was more conducive to improving localization, puncture accuracy and completeness skills for UMIBS.
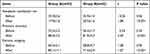 |
Table 3 Evaluation of Surgical Skills Before and After Training |
Questionnaire Results from Students
A total of 84 questionnaires were sent out and returned. The satisfaction rate in Group A was high at 78.5%, and the acting ability was 92.9% in Group A and 50% in Group B. Group A showed better feedback than Group B in learning interest, surgical operation ability, and satisfaction with the teaching mode (p<0.05, by the Kruskal–Wallis test; shown in Table 4).
 |
Table 4 Feedback on Two Teaching Methods from Students |
Discussion
According to recent literature,16,17 we are witnessing a shift in health care culture, with increased attention to patient expectations and professional liability. Along with this trend, there are rising concerns about the quality of surgical residency training in their professional lives, and surgeons must achieve new competencies, avoiding patient safety impairment. UMIBS is a highly practical technique that requires countless practice, and practice makes perfect. It is necessary to establish a simulation scenario for practice to adapt to the change from the open surgery vision field to indirect imaging under ultrasound.18 Pork has a texture similar to that of human tissue; the pork/pickle simulation training model is easy to build, and students can focus on the details of the operation when facing the simulation model by providing a psychological barrier-free platform. Compared to traditional standard training, simulation model-based learning is more practical and convenient and stimulates students’ motivation and imagination.19
The original Halstedian model of “see one, do one, teach one” is changing into modern proficiency-based training.20 In this regard, among others, webinars and online videos shared on social media portals are gaining importance, and the impact of video and multimedia sources on clinical activity and surgical training is becoming a fundamental issue, especially in the pandemic era.21 The SBS method has been applied in many disciplines and has achieved good results.22 Published literature shows that the SBS teaching method is more suitable for improving surgical ability and learning interest compared to “all in one” or “lecture-based learning” methods.23
In the present study, we divided the training plan into five steps, which focused on ultrasound training, evaluation of neoplasms, simulation training, operation, and ward rounds. After SBS method training, results were evaluated by objective indicators, such as localization time, puncture accuracy and completeness of the lesion. The surgical operation skills of Group A were significantly improved, and they obtained better scores than those of Group B. The VAS scores (mean±standard; deviation) were 82.8±4.4 better than those of Group B (72.7±4.0). The neoplasm localization ability and completeness of resection in Group A were also significantly better than those in Group B. The questionnaire survey showed that the learning interest and practical ability of Group A were significantly improved, and the satisfaction of Group A was 78.5%, which was better than that of Group B. The SBS method has effectively improved the performance of the students and stimulated their enthusiasm for learning.
Compared with the LBL method, SBS has several benefits. First, in SBS curricula, students could practice the ability of mass identification and surgical trace tracking, which not only improved the localization ability but also helped to familiarize themselves with the surgical procedure and reduce complications. Step-by-step practice can promote hand-eye cooperation, spatial vision conversion ability, and a certain degree of B-scanning ability and establish the concept of three-dimensional resection in such a specific setting, it’s the key factor to improve the student operation ability.
Second, the SBS training method was used for Group A, providing more communication opportunities between students and teachers. Teachers were required to explain the details of each step and refine each step of the teaching details.24 Which was helpful to improve the teaching quality. The teacher completed the main steps of the operation, and the students recorded the case and asked questions during the demonstration, which provided more interaction between the students and the teacher to promote the change from teacher-centered to student-oriented. Meanwhile, students could discuss with the teacher after surgery to better complete the learning goals, which increased students interest and satisfaction.
In addition, the SBS method improved students’ puncture accuracy and increased surgical operation proficiency by providing sufficient training opportunities for students. Through the postoperative ward round, students could analyze possible complications and propose solutions, and then teacher corrected analysis deviations, which enhanced students’ self-confidence in learning.
Conclusion
The SBS method in the teaching of UMIBS enhanced the students’ interest in learning and clinical thinking and improved the technique skills. In the study, the teacher’s assistant organized the distribution, collection and verification of the questionnaire before and after the lecture. The training and the observation time of training effects is relatively short, and a longer follow-up duration of assessment is needed. Another limitation is nonrandomized grouping. In the future, it is necessary to expand multicenter and randomized clinical research to further confirm the practicality and advantages of this teaching method with a further improved perspective.
Abbreviations
UMIBS, ultrasound-guided minimally invasive breast surgery; LBL, lecture-based learning; SBS, step-by-step method; Demo, demonstration; VAS, visual analog scale; CT, computed tomography; MRI, magnetic resonance imaging.
Data Sharing Statement
All data are available upon request from the corresponding author.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of the Sixth Affiliated Hospital of Sun Yat-sen University under Grant 2022ZSLYEC-264. Written consent was obtained from each of the participants.
Acknowledgments
Haiyan Li will handle correspondence, including any queries about methodology and materials. We would like to thank the colleagues of the breast surgery department for UMIBS teaching and administrative support. We would also like to thank all the residents who participated in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Guangdong Province Teaching Base Reform Project under Grant 2017JD009 and the Guangdong Province Education Department Undergraduate Teaching Reform Project under Grant 88000-18832551. Supported by National Key Clinical Discipline.
Disclosure
The authors report no conflicts of interest.
References
1. Iwuagwu OC, Calvey TA, Ilsley D, Drew PJ. Ultrasound guided minimally invasive breast surgery (UMIBS): a superior technique for gynecomastia. Ann Plast Surg. 2004;52(2):131–133. PMID: 14745260. doi:10.1097/01.sap.0000095441.40759.1f
2. Yao Y, Yang Y, Liu J, Wang Y, Zhao Y. Vacuum-assisted minimally invasive surgery-An innovative method for the operative treatment of gynecomastia. Surgery. 2019;166(5):934–939. PMID: 31248653. doi:10.1016/j.surg.2019.04.032
3. Rekman JF, Alseidi A. Training for minimally invasive cancer surgery. Surg Oncol Clin N Am. 2019;28(1):11–30. PMID: 30414676. doi:10.1016/j.soc.2018.07.007
4. Gao YH, Zhu SC, Xu Y, et al. Clinical value of ultrasound-guided minimally invasive biopsy in the diagnosis or treatment of breast nodules. Cancer Manag Res. 2020;12:13215–13222. PMID: 33380829; PMCID: PMC7767640. doi:10.2147/CMAR.S281605
5. Wang CL, Chen PY, Yang KC, Wu HC, Wang CC. Ultrasound-guided minimally invasive surgical resection of retrocalcaneal bursitis: a preliminary comparison with traditional open surgery. J Foot Ankle Surg. 2019;58(5):855–860. PMID: 31345762. doi:10.1053/j.jfas.2018.12.023
6. Yamamoto A, Obika M, Mandai Y, et al. Effects on postgraduate-year-I residents of simulation-based learning compared to traditional lecture-style education led by postgraduate-year-II residents: a pilot study. BMC Med Educ. 2019;19(1):87. PMID: 30894162; PMCID: PMC6425645. doi:10.1186/s12909-019-1509-y
7. Bleske BE, Remington TL, Wells TD, et al. A randomized crossover comparison of team-based learning and lecture format on learning outcomes. Am J Pharm Educ. 2016;80(7):120. PMID: 27756928; PMCID: PMC5066923. doi:10.5688/ajpe807120
8. Mason WT, Strike PW. See one, do one, teach one–is this still how it works? A comparison of the medical and nursing professions in the teaching of practical procedures. Med Teach. 2003;25(6):664–666. PMID: 15369918. doi:10.1080/01421590310001605705
9. Rohrich RJ. “See one, do one, teach one”: an old adage with a new twist. Plast Reconstr Surg. 2006;118(1):257–258. PMID: 16816705. doi:10.1097/01.prs.0000233177.97881.85
10. Arora S, Aggarwal R, Sirimanna P, et al. Mental practice enhances surgical technical skills: a randomized controlled study. Ann Surg. 2011;253(2):265–270. PMID: 21245669. doi:10.1097/SLA.0b013e318207a789
11. Schwartz LR, Fernandez R, Kouyoumjian SR, Jones KA, Compton S. A randomized comparison trial of case-based learning versus human patient simulation in medical student education. Acad Emerg Med. 2007;14(2):130–137. PMID: 17267529. doi:10.1197/j.aem.2006.09.052
12. Dickinson BL, Lackey W, Sheakley M, Miller L, Jevert S, Shattuck B. Involving a real patient in the design and implementation of case-based learning to engage learners. Adv Physiol Educ. 2018;42(1):118–122. PMID: 29357269. doi:10.1152/advan.00174.2017
13. Rossettini G, Rondoni A, Palese A, et al. Effective teaching of manual skills to physiotherapy students: a randomised clinical trial. Med Educ. 2017;51(8):826–838. PMID: 28699295. doi:10.1111/medu.13347
14. Palocaren J, Pillai LS, Celine TM. Medical biochemistry: is it time to change the teaching style? Natl Med J India. 2016;29(4):222–224. PMID: 28051002.
15. Gresens AA, Britt RC, Feliberti EC, Britt LD. Ultrasound-guided breast biopsy for surgical residents: evaluation of a phantom model. J Surg Educ. 2012;69(3):411–415. PMID: 22483146. doi:10.1016/j.jsurg.2011.10.015
16. Barellini L, Marcasciano M, Lo Torto F, Fausto A, Ribuffo D, Casella D. Intraoperative ultrasound and oncoplastic combined approach: an additional tool for the oncoplastic surgeon to obtain tumor-free margins in breast conservative surgery-A 2-year single-center prospective study. Clin Breast Cancer. 2020;20(3):e290–e294. PMID: 32144083. doi:10.1016/j.clbc.2019.10.004
17. Campbell EJ, Romics L. Oncological safety and cosmetic outcomes in oncoplastic breast conservation surgery, a review of the best level of evidence literature. Breast Cancer. 2017;9:521–530. PMID: 28831273; PMCID: PMC5552002. doi:10.2147/BCTT.S113742
18. Papathemelis T, Heim S, Lux MP, Erhardt I, Scharl A, Scharl S. Minimally invasive breast fibroadenoma excision using an ultrasound-guided vacuum-assisted biopsy device. Geburtshilfe Frauenheilkd. 2017;77(2):176–181. PMID: 28331240; PMCID: PMC5357216. doi:10.1055/s-0043-100387
19. Seale J, Ragbourne SC, Purkiss Bejarano N, et al. Training final year medical students in telephone communication and prioritization skills: an evaluation in the simulated environment. Med Teach. 2019;41(9):1023–1028. PMID: 31124719. doi:10.1080/0142159X.2019.1610559
20. Vozenilek J, Huff JS, Reznek M, Gordon JA. See one, do one, teach one: advanced technology in medical education. Acad Emerg Med. 2004;11(11):1149–1154. PMID: 15528578. doi:10.1197/j.aem.2004.08.003
21. Marcasciano M, Kaciulyte J, Mori FLR, et al. Breast surgeons updating on the thresholds of COVID-19 era: results of a multicenter collaborative study evaluating the role of online videos and multimedia sources on breast surgeons education and training. Eur Rev Med Pharmacol Sci. 2020;24(14):7845–7854. doi:10.26355/eurrev_202007_22289
22. Yuan JX, Yang KY, Ma J, Wang ZZ, Guo QY, Liu F. Step-by-step teaching method: improving learning outcomes of undergraduate dental students in layering techniques for direct composite resin restorations. BMC Med Educ. 2020;20(1):300. PMID: 32917189; PMCID: PMC7488449. doi:10.1186/s12909-020-02230-1
23. Liu X, Liu M, Yang Y, Fan C, Tan J. Step-by-step teaching method improves the learner achievement in dental skill training. Eur J Dent Educ. 2019;23(3):344–348. PMID: 30891903. doi:10.1111/eje.12435
24. Wei F, Sun Q, Qin Z, Zhuang H, Jiang G, Wu X. Application and practice of a step-by-step method combined with case-based learning in Chinese otoendoscopy education. BMC Med Educ. 2021;21(1):89. PMID: 33541330; PMCID: PMC7863487. doi:10.1186/s12909-021-02513-1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

