Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Statistical Joint Modeling for Predicting the Association of CD4 Measurement and Time to Death of People Living with HIV Who Enrolled in ART, Southwest Ethiopia
Authors Tiruneh F , Chewaka L , Abdissa D
Received 30 September 2020
Accepted for publication 30 December 2020
Published 22 January 2021 Volume 2021:13 Pages 73—79
DOI https://doi.org/10.2147/HIV.S283059
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Firew Tiruneh,1 Lalisa Chewaka,2 Dinaol Abdissa1,3
1Department of Midwifery, College of Health Science, Mizan Tepi University, Mizan Teferi, SNNPR, Ethiopia; 2Department of Nursing, College of Health Science, Mizan Tepi University, Mizan Teferi, SNNPR, Ethiopia; 3Department of Nutrition and Reproductive Health, School of Public Health, College of Health Science, Mizan Tepi University, Mizan Teferi, SNNPR, Ethiopia
Correspondence: Firew Tiruneh
Mizan Tepi University, PO Box 260, Mizan Teferi, Ethiopia
Tel +251-917-83-0101
Email [email protected]
Background: In much epidemiological HIV research, patients are often followed over a period of time to predict their survival on the basis of repeatedly measured CD4 status. To predict survival, statistical models of the association between mortality and longitudinal CD4 measurement have been conducted widely using time-varying Cox models. However, in the presence of repeated measure, this approach leads to biased estimates. In view of the limitation of time-varying Cox models, in the present study, we considered joint modeling to predict the association of longitudinal CD4 measurement and time to death among patients initiated on ART.
Methods: A retrospective cohort study was employed for five years from 2009 to 2014 on a randomly selected 358 samples. Data were collected from patients’ ART and pre-ART follow-up registration book, database and other clinical records. Data were analyzed using joint latent class modeling of repeated CD4 measurement and time-to-event (HIV death).
Results: We have studied a total of 358 HIV-positive patients. The median and interquartile ranges of the age of patients were 30.31 years and 13.82, respectively. Males constitute the larger proportion, 51.68%. The square root of CD4 count has declined on average over time. This has been indicated with the negative sign of the coefficient for the time effect. The deterioration of health of individuals is severe in class 1, it has been observed with a worse decline in CD4 cell counts over time in this class than other classes (β= − 0.488). Women had a larger risk rate than men (β=− 2.475, p-value=0.013). Besides, the CD4 counts measurement of patients has been revealed to decrease as age increases (β= − 0.016, p=0.008).
Conclusion: The finding indicated that the square root CD4 cell measurement dropped over time in the three classes. This clearly suggested deterioration in the health of individuals. Women were found to have a higher hazard rate than men.
Keywords: HIV, survival, joint modeling, CD4, prediction
Introduction
The impact of human immunodeficiency virus (HIV) is still a global public health challenge. At the end of 2019, there were an estimated 38 million people living with HIV (PLWHIV). Although coverage of services has been steadily increasing, 33% of PLWHIV were unable to access HIV testing, treatment and care.1 As a result of this gap in service, around 1.7 million people were newly infected and 690,000 people died from HIV-related causes in 2019. Over two thirds of all people living with HIV live in the WHO African region.2 In Ethiopia, there were 690,000 PLWHIV in 2018 with 23,000 new HIV infections and 11,000 AIDS-related deaths.3
In a number of studies, people living with HIV are often followed-up until the time-to-event of interest.4,5 In such studies, the relationship between time until event of interest and longitudinal biomarkers such as CD4 is the focus of interest. For instance, different studies have indicated that CD4 count is the most widely used biological marker for HIV progression.6,7 Many studies were conducted to assess the effect of antiretroviral therapy on the survival rate of PLWHIV.8–10
Following the start of universal test and treat protocol, less attention was given regarding the relevance of CD4 measurement. In many settings, still health-care providers uses viral load to monitor the progression of HIV disease. However, CD4 measurement is still crucial to the progression of the disease, particularly in resource constrained areas where viral load measurement is not affordable.11 In our setting, different literatures showed that patients who enrolled on ART with low CD4 measurement have a higher risk of death.12–14 In these studies, time-varying Cox model was used to examine the association between repeated CD4 measurement and mortality.
Longitudinal studies often gather repeated measurements and time-to-event data. Repeated measurements and time-to-event outcomes are traditionally analyzed, for instance, using Cox proportional hazards model. However this approach leads to biased results.15 When using standard methods for estimating treatment effect in cohort study it cannot allow us control time-varying confounders.16 A good model that takes into account the shortcomings of the Cox proportional hazards model is joint models for time-to-event data and longitudinal data.17
Joint models are preferably utilized in clinical trials for their efficient estimates of the treatment effects with reduced bias.18 Besides, joint models allow estimates with a smaller SE than the Cox proportional model.19
The two typically used joint models are the joint latent class model (JLCM) and the shared random effect model (SREM).20 It is a prevailing fact that patients may have some heterogeneity due to unobserved risk factors. In the light of addressing this issue, JLCM considers that study population have several homogeneous latent subgroups in which the study subjects share the same risk of the event and marker trajectory.21
In view of the limitation of time-varying Cox models, in the present study we used a joint latent class modeling strategy to assess the association of CD4 count on mortality among HIV infected patients using antiretroviral therapy.
Methods
Study Design and Setting
A retrospective cohort study was conducted for five years from 2009 to 2014. The study was conducted in selected ART clinics found in southwest Ethiopia. In This study southwest Ethiopia encompasses five zones; namely, Jimma, Illu Ababora, Kafa, Sheka, and Bench-Maji.
Study Participants
Source populations are all adults having a follow-up care in ART clinics in southwest Ethiopia. Study populations were 358 randomly selected who were enrolled on ART between September 2009 and August 2014. These 358 patients represent randomly selected study subjects from whom data were collected and analyzed to predict the association of repeated measurements of CD4 count and time to death using JLCM. We followed all of them until they were lost to follow-up, dead, transferred out or the study ended August 31, 2014.
Study Variables
The repeated CD4 measurement and time to death were the two outcome variables considered for this study. Time to death was measured from the time when ART was initiated to death or censored in month. We considered censored those subjects transferred to another hospital, who were lost to follow-up, or did not die at the end of the study. The CD4 count was the longitudinal outcome. It was measured per millimeter cubed of blood every six months, which was considered a biomarker for patients. We have also considered independent covariates for both survival modeling and the separate longitudinal model.
Data Collection
A standardized tool which was adapted from existing literature was used. The tool has previously been utilized. Adapted tools were translated into local languages by language experts. In the selected ART clinics routine clinical and demographic data were recorded both at base line and on each follow-up visit of the patients. Regarding CD4 count, it has been measured at baseline and then every six months unless indicated by physicians. The data collection was done through a record review method by three trained BSc clinical nurses. Relevant data were collected from patients’ pre-ART and ART follow-up logbooks, database and other clinical records. To assure quality of data extraction, a pretest was conducted on 5% of the sampled population from nonselected ART clinics ahead of data collection.
Statistical Analysis
A joint modeling of time-until-event and repeated CD4 measurement was carried out. We considered the following three steps for defining a joint model (i) a model for the time-to-event (proportional hazard model), (ii) a model for the marker trajectory (linear mixed model), and (iii) joint latent class model (linking both models using a shared latent structure).22 The proportional Weibull hazard functions were used for both models. Estimation of models’ parameters was based on maximization of the log-likelihood using the robust Marquardt algorithm.
A linear mixed model was used to model CD4 count by taking between-subject variations into consideration. In order to have an appropriate submodel we have used the square root of CD4 count and we observed covariates that significantly affect the average change in the square root of CD4 count.
Distinguishing among different profile of CD4 trajectories in the study subjects was modeled using a JLCM. Our JLCM had three elements: the longitudinal biomarker trajectories, the hazard for the time-to-event process and class membership. We supposed that each of the study subjects goes to one of the g latent classes, where g denotes number of latent classes. Study subjects with similar features and trend of CD4 count were supposed to belong to the same class. After the model fitted, each of the study subjects were assigned to the class on the basis of higher posterior probability of membership.
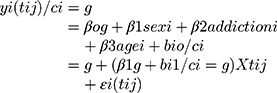
Conditionally on each latent class (g), we modeled
The CD4 trajectory of subject i by
Here, the latent class membership for each subject, i was defined using a categorical latent variable ci, which equals g if subject i belongs to latent class g (g=1 … G). We considered an unstructured variance-covariance matrix of the random effects, which are the same over latent classes.
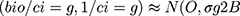
Hazard of death was modeled by:
In order to get a proper longitudinal and survival model we considered the Akaike information criteria (AKI) and the Bayesian information criteria (BIC).
Joint model estimation was done based on the Bayesian approach. Accordingly, to get an appropriate joint model the deviance information criteria (DIC) based on posterior distribution of the deviance statistics was considered.
Moreover, first we checked for the conditional independence (CI) assumption in JLCM. This essential assumption considered independence between the time-to-event and the longitudinal repeated measurements given in the latent classes. The next step was to determine the ideal number of classes that could explain the heterogeneity of the study subjects. We supposed that each study subject belongs to one of the g latent classes. We consecutively estimated the models with 1, 2 and 3 latent classes. The ideal number of classes was determined by the model with the lowest BIC.
Results
Descriptive Result
The study was conducted on 358 HIV-positive patients who met the inclusion criteria. The median and IQR for age of patients was 30.31 years and 13.82 respectively. Males constituted the larger proportion 51.68% with a median age of 36.28 years (IQR=11.27). The median for baseline CD4 cell measurement was 356 cells/mm3 (IQR=320). During the follow-up, 68 patients (18.99%) died and 97 patients (27.09%) were censored. Clinical characteristics and demographic information were included in Table 1.
 |
Table 1 Demographic and Clinical Characteristics of Study Subjects, Southwest Ethiopia |
The square root of CD4 cells count per millimeter cubed of blood which was measured nearly every six month intervals was indicated in Table 2 by the censoring and event status of the patients.
 |
Table 2 Mean and Standard Deviation of Weighted and Square Root of CD4 with Censoring Status of Patients, Southwest Ethiopia |
Joint Model Result
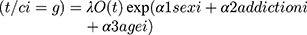
In order to determine the number of classes in JLCM, we identified three models with differing numbers of classes. Table 3 shows the comparison of BIC for JLCM.
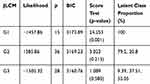 |
Table 3 Comparison of BIC of JLCMs, with a Total Number of Classes Varying from 1 to 3 |
Following the determination of the optimum number of latent classes, we estimated the full model along with the covariate variables. Table 4 presented the estimates for fitting JLCM. The square root of CD4 cell count has declined on average in all the three classes over time. This has been indicated with the negative sign of the coefficient for the time effect in The CD4 cell counts in class 1 has declined markedly over time than other classes (β= −0.488). The finding suggested that deterioration in the health of individuals in class 1 is highly pronounced. Women had a higher risk rate than men (β=−2.475, p-value=0.013). Besides, the study revealed that CD4 cell measurement of study subjects decreased as age increases (β= −0.016, p=0.008).
 |
Table 4 Estimation of JLCM for Three Class Model |
Nearly 53.05% of study subjects in class 3 had little hazard of death in time. Class 2, representing 37.56% study subjects, had a moderate risk of death while class 1, representing 9.39% of the subjects, had an intense hazard of death. Study subjects in the three classes have different profiles of CD4 measurement associated with different risks of death. We have also observed how accurately the three-class latent model allocates subjects to classes. The three-class latent model yielded very good discrimination with average maximal posterior probabilities of subjects categorized respectively, 0.84, 0.80 and 0.84 for classes 1, 2 and 3.
Discussion
In present study, we considered joint latent class modeling to estimate the survival of PLWHIV who initiated ART using CD4 cell counts and time-to-death.23 This model supposes that a latent class structure fully captures the correlation between the longitudinal marker trajectory and the risk of the event.22 As a result of its advantage in modeling the dependency between the time until event and the repeated measurement the joint latent class model was specifically well-matched for prediction studies.17,21
Our finding depicted that estimation of time to death based on longitudinal CD4 using the joint latent class model. We revealed that the risk of death hinged on longitudinal CD4 counts. The study has also indicated that the square root of CD4 cell measurement has declined on average over time in the three classes. The fact that CD4 cell counts have decreased over a period of time showed deterioration in the health of individuals. Women were found to have a higher hazard rate than men. The finding of this study is in agreement with studies that used the same analysis.24,25
The finding that indicated women had a higher rate of hazard in this study seems in contradiction with different literatures. However, our finding could be possibly justified with the prevailing socioeconomic and cultural factors. In the study area females are less economically empowered than males and their health-seeking behavior is highly affected by male involvement. In contrast home delivery and compliance to traditional treatment are unique and common to females. Although it requires substantive study, we thought that these factors can possibly justify the higher risk rate of death in females than males. Similarly, some studies in Ethiopia have shown that CD4 count is an important predictor of survival for HIV patients using traditional, standard methods.26,27
However, we found this was in disagreement with some studies from Ethiopia.28,29 The difference could be explained by the difference in statistical methods used. They have used Cox proportional hazards model to determine CD4 a predictor of survival. When using standard methods for determining predictors of survival in cohort study it cannot allow us to control time-varying confounders. Hence, this approach leads to biased results. In the current study JLCM was used; a powerful method that takes into account the limitation of the Cox proportional hazards model for longitudinal and time-to-event data.
In the present study we learnt that the three latent classes have varied profiles of CD4 measurement associated with different risks of death from low to intense. On the basis of our understanding of the finding, study subjects were classified into three classes (“high risk”, “moderate risk” and “low risk”) based on the health status of study subjects. This finding put clinicians in a position to make a better decision to help their HIV-infected patients to maximize their survival.
We have also explored the longitudinal CD4 count and the prediction of survival of HIV patients who were on ART. From the weighted square root of CD4 measurement the censored patients have an increasing mean square root of CD4 count up to 30 months and started to decrease after 30 months. For deceased patients the square root of CD4 measurements have increasing values up to 24 months and showed a decreased measurement 30 months later.
Conclusion
The finding indicated that the square root CD4 cell counts decreased on average over time in three classes. This decrement in CD4 cell counts over time revealed worsening in the health of individuals. Women were found to have a higher hazard rate than men. The CD4 counts levels of patients decreased with increasing age. Individuals were categorized with a given risk status in three classes (“high risk”, “moderate risk” and “low risk”). It is hoped that this finding helps clinicians to identify patients with risk of death and to base their action to prevent further deaths.
Ethical Approval
Ethical approval was obtained from the College of Health Science, Mizan Tepi University Ethical Review Board. A permission to collect data was obtained from the facility head. An informed written consent was obtained from each study participants to review their medical records. Confidentiality of the study subjects’ information was maintained. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgment
The authors would like to forward their heartfelt gratitude to their colleague Mrs Bethelihem Abebe for her support in each step of my review. The authors would also like to extend their sincere thanks to Dr Gizelle Arnold for her help in editing the English language.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. HIV/AIDS [Internet]. Genva; 2020. [cited September 20, 2020]. Available from https://www.who.int/health-topics/hiv-aids/#tab=tab_1.
2. World Health Organization Geneva. HIV/AIDS fact sheet [internet]. 2020 [cited September 20, 2020]. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
3. World Health Organization. HIV Country Profiles [Internet]. Geneva; 2020 [cited September 20, 2020]. Available from: https://cfs.hivci.org/country-factsheet.html.
4. Trickey A, May MT, Vehreschild JJ, et al. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV. 2017;4(8):e349–e356. doi:10.1016/S2352-3018(17)30066-8
5. Fontela C, Aguinaga A, Moreno-Iribas C, et al. Trends and causes of mortality in a population-based cohort of HIV-infected adults in Spain: comparison with the general population. Sci Rep. 2020;10(1):1–9. doi:10.1038/s41598-020-65841-0
6. May MT, Vehreschild -J-J, Trickey A, et al. Mortality according to CD4 count at start of combination antiretroviral therapy among HIV-infected Patients followed for up to 15 years after start of treatment: collaborative Cohort Study. Clin Infect Dis. 2016;62(12):1571–1577. doi:10.1093/cid/ciw183
7. Tang Z, Pan SW, Ruan Y, et al. Effects of high CD4 cell counts on death and attrition among HIV patients receiving antiretroviral treatment: an observational cohort study. Sci Rep. 2017;7(1):1–8. doi:10.1038/s41598-016-0028-x
8. Cardoso CAA, Pinto JA, Candiani TMS, de Carvalho IR, Linhares RM, Goulart EMA. The impact of highly active antiretroviral therapy on the survival of vertically HIV-infected children and adolescents in Belo Horizonte, Brazil. Mem Inst Oswaldo Cruz. 2012;107(4):532–538. doi:10.1590/S0074-02762012000400014
9. Edmonds A, Yotebieng M, Lusiama J, et al. The effect of highly active antiretroviral therapy on the survival of HIV-infected children in a resource-deprived setting: a Cohort Study. Bangsberg DR, editor. PLoS Med. 2011;8(6):e1001044. doi:10.1371/journal.pmed.1001044
10. Lv R, Li G, Wu J, Zhu Y, Qin X, Li S. Research on AIDS patients’ survival time after highly active antiretroviral therapy, treatment effect and treatment modes. Saudi Pharm J. 2016;24(3):318–321. doi:10.1016/j.jsps.2016.04.004
11. WHO. What’s new in treatment monitoring: viral load and CD4 testing [Internet]. [cited September 20, 2020]. Available from https://www.who.int/hiv/pub/arv/treatment-monitoring-info-2017/en/.
12. Kassa A, Teka A, Shewaamare A, Jerene D. Incidence of tuberculosis and early mortality in a large cohort of HIV infected patients receiving antiretroviral therapy in a tertiary hospital in Addis Ababa, Ethiopia. Trans R Soc Trop Med Hyg. 2012;106(6):363–370. doi:10.1016/j.trstmh.2012.03.002
13. Abebe N, Alemu K, Asfaw T, Abajobir AA. Survival status of HIV positive adults on antiretroviral treatment in Debre markos referral hospital, Northwest Ethiopia: retrospective cohort study. Pan Afr Med J. 2014;17:1937–8688. doi:10.11604/pamj.2014.17.88.3262
14. Jerene D, Næss A, Lindtjørn B. Antiretroviral therapy at a district hospital in Ethiopia prevents death and tuberculosis in a cohort of HIV patients. AIDS Res Ther. 2006;3(1):1–8. doi:10.1186/1742-6405-3-10
15. Asar Ö, Ritchie J, Kalra PA, Diggle PJ. Joint modelling of repeated measurement and time-to-event data: an introductory tutorial. Int J Epidemiol. 2015;44(1):334–344. doi:10.1093/ije/dyu262
16. Fewell Z, Hernán MA, Wolfe F, Tilling K, Choi H, Sterne JAC. Controlling for time-dependent confounding using marginal structural models. Stata J. 2004;4(4):402–420. doi:10.1177/1536867X0400400403
17. Ibrahim JG, Chu H, Chen LM. Basic concepts and methods for joint models of longitudinal and survival data [internet]. J Clin Oncol. 2010;28(16):2796–2801. doi:10.1200/JCO.2009.25.0654
18. Guo X, Carlin BP. Separate and joint modelling of longitudinal and event time data using standard computer packages. Am Stat. 2004;58(1):1. doi:10.1198/0003130042854
19. Chen M-H, Ibrahim JG, Sinha D. A new joint model for longitudinal and survival data with a cure fraction. J Multivar Anal. 2004;91(1):18–34. doi:10.1016/j.jmva.2004.04.005
20. Henderson R. Joint modelling of longitudinal measurements and event time data. Biostatistics. 2000;1(4):465–480. doi:10.1093/biostatistics/1.4.465
21. Lin H, McCulloch CE, Turnbull BW, Slate EH, Clark LC. A latent class mixed model for analysing biomarker trajectories with irregularly scheduled observations. Stat Med. 2000;19(10):1303–1318. doi:10.1002/(SICI)1097-0258(20000530)19:10<1303::AID-SIM424>3.0.CO;2-E
22. Liu Y, Liu L, Zhou J. Joint latent class model of survival and longitudinal data: an application to CPCRA study. Comput Stat Data Anal. 2015;91:40–50. doi:10.1016/j.csda.2015.05.007
23. Proust-Lima C, Séne M, Taylor JMG, Jacqmin-Gadda H. Joint latent class models for longitudinal and time-to-event data: a review. Stat Methods Med Res. 2014;23:74–90. doi:10.1177/0962280212445839
24. Khorashadizadeh F, Tabesh H, Parsaeian M, Esmaily H, Rahimi Foroushani A. Predicting the survival of AIDS patients using two frameworks of statistical joint modeling and comparing their predictive accuracy. Iran J Public Health. 2020;49(5):949–958.
25. Modelling progression of CD4-lymphocyte count and its relationship to survival time - PubMed [internet]. [cited September 25, 2020]. Available from: https://pubmed.ncbi.nlm.nih.gov/7786983/.
26. Biadgilign S, Reda AA, Digaffe T. Predictors of mortality among HIV infected patients taking antiretroviral treatment in Ethiopia: a retrospective cohort study. AIDS Res Ther. 2012;9(1):1–7. doi:10.1186/1742-6405-9-15
27. Ayalew MB. Mortality and Its predictors among HIV infected patients taking antiretroviral treatment in Ethiopia: a systematic review. AIDS Res Treat. 2017; 2017.
28. Alemu AW, Sebastián MS. Determinants of survival in adult HIV patients on antiretroviral therapy in Oromiyaa, Ethiopia. Glob Health Action. 2010;3(1):5398. doi:10.3402/gha.v3i0.5398
29. Tachbele E, Ameni G. Survival and predictors of mortality among human immunodeficiency virus patients on anti-retroviral treatment at Jinka Hospital, South Omo, Ethiopia: a six years retrospective cohort study. Epidemiol Health. 2016;38:e2016049. doi:10.4178/epih.e2016049
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.