Back to Journals » Cancer Management and Research » Volume 12
Splenic Diffuse Red Pulp Small B-Cell Lymphoma with Gastrointestinal Hemorrhage: A Case Report and Literature Review
Authors Xu Y, Fan X, Sun C, Yin L, Qiu T, Xia J, Zhong X, Xu L, Li D , Li Z, Zhu F , Xu K
Received 4 August 2020
Accepted for publication 15 September 2020
Published 6 October 2020 Volume 2020:12 Pages 9627—9633
DOI https://doi.org/10.2147/CMAR.S275292
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Rudolph Navari
Yanqiu Xu,1,* Xiaohui Fan,1,* Cai Sun,2 Lingling Yin,2 Tingting Qiu,2 Jieyun Xia,2 Xiaomin Zhong,3 Linyan Xu,1,4 Depeng Li,2 Zhenyu Li,1,2,4 Feng Zhu,1,2 Kailin Xu1,2,4
1Blood Disease Institute, Xuzhou Medical University, Xuzhou, Jiangsu 221002, People’s Republic of China; 2Department of Hematology, The Affiliated Hospital of Xuzhou Medical University, Xuzhou, Jiangsu 221002, People’s Republic of China; 3Department of Oncology, Affiliated Huai’an First People’s Hospital of Nanjing Medical University, Huai’an, Jiangsu Province 223300, People’s Republic of China; 4Key Laboratory of Bone Marrow Stem Cell, Xuzhou, Jiangsu Province 221002, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Feng Zhu
Department of Hematology, The Affiliated Hospital of Xuzhou Medical University, 99, West Huaihai Road, Quanshan District, Xuzhou, Jiangsu 221002, People’s Republic of China
Tel +86 516 8580 6985
Fax +86 516 8580 1527
Email [email protected]
Background: Splenic diffuse red pulp small B-cell lymphoma (SDRPSBCL) is rare and accounts for less than 1% of non-Hodgkin’s lymphoma. As the first or accompanying symptoms of SDRPSBCL, gastrointestinal hemorrhage (GIH) is rather unusual.
Patients and Methods: We reported on a patient with SDRPSBCL complicated with GIH. According to the enteroscopy, pathological sections of spleen and intestine, immunohistochemistry and other related laboratory examinations, the patient was diagnosed as SDRPSBCL (stage IVb) complicated with colon and rectal ulcers. The clinical manifestations were hematochezia, unformed stool, continuous anal pain and poor quality of life. Subsequently, the patient was treated by six cycles of CHOP (cyclophosphamide + doxorubicin + vincristine + hydroprednisone) regimens. The clinical features, diagnosis and treatment were analyzed retrospectively and the relevant literatures were reviewed.
Results: After the first course of chemotherapy, the patient did not have any more bloody stool and the stool was shaped. After six cycles of chemotherapy, the patient’s anus was no longer painful and he has been in complete remission according to the result of positron emission tomography CT.
Conclusion: Through analysis of this case, we could elucidate that after the primary disease was alleviated, the bleeding degree of digestive tract was relieved, which provided the basis for the clinical treatment of this rare disease.
Keywords: splenic diffuse red pulp small B-cell lymphoma, gastrointestinal hemorrhage, symptom, diagnosis, chemotherapy
Introduction
Splenic diffuse red pulp small B-cell lymphoma (SDRPSBCL) is a single form of B-lymphocyte diffuse involvement of the splenic red pulp1 in the classification of WHO (2016) lymphoid tumor, which is characterized by the infiltration of spleen red pulp as the main lesion.2 SDRPSBCL is less than 1% of non-Hodgkin’s lymphoma3,4 and spleen, bone marrow, peripheral blood and splenic hilar lymph nodes are usually involved.4–8 The clinical manifestations are usually splenomegaly, lymphocytosis, no hemocytopenia, anemia and rare B symptoms.9 There is still no standard treatment regimen for SDRPSBCL; splenectomy and chemotherapy are generally not necessary. Nevertheless, if patients have organs involvement or disease progression, more active treatments should be considered, including splenectomy, radiotherapy and chemotherapy.3–5,7,10,11 Rituximab or combined chemotherapy can improve clinical outcomes, but there is still lack of data on a large number of cases.11
Gastrointestinal hemorrhage (GIH) is divided into upper and lower gastrointestinal bleeding. The closer the lesion to the anus, the more common the hemorrhage will be; additionally, the closer to the upper gastrointestinal tract, the main manifestation is more common to be hemoptysis or black stool. The etiology of GIH is thought to be complex and malignant tumor is one of the causes.12 Digestive tract lymphoma may occur in the intestinal tract or other parts of the lymphoma invasion.12–15 Whereas, there are few reported cases of SDRPSBCL with digestive tract symptoms such as hemoptysis or hematochezia, the relationship between SDRPSBCL with GIH symptom and the outcomes of treatment. In this paper, a case of SDRPSBCL complicated with GIH was analyzed retrospectively and the treatment was followed up. Besides, the mechanism and the treatment scheme of bleeding symptoms were discussed, so as to provide a basis for clinical treatment.
Case Report
Patient Case
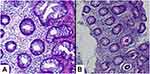
The patient was male and aged 67, who experienced repeated fever with the temperature of about 38°C, accompanied by fear of cold. The results of Doppler Ultrasound in the local county: the size of spleen was 24.2 cm x 7.6 cm. He was admitted to our department on 17 November, 2017. The main blood routine was as follows: WBC 3.2 x109/L, RBC 3.03 x1012/L, Hb 83 g/L and PLT 81 x109/L. Bone marrow morphology: proliferation was active with 55% of the granulocyte system and no metastatic cancer cells were found. The results of positron emission tomography (PET)-CT (Figure 1A) on 12 December, 2017 were that: 1. Augmentation of ascending aorta, calcification of right lobe of liver, giant spleen; 2. Thickened ileocecal intestinal wall, increased glucose metabolism with peripheral exudation and enlarged lymph node shadow. Splenectomy and right hemicolectomy were performed on 25 December 2017. Postoperative splenic pathology indicated chronic splenic congestion (Figure 2A), immunohistochemistry staining: CD20 (+), Pax-5 (+), CD3 (-), CD5 (-), CD4 (-), CD8 (-), Cyclin D1 (-), CD10 (-), Bcl-6 (-), CD25 (-), CD56 (-), CD43 (-), MPO (-), TDT (-). Right hemicolon pathology indicated lymphoproliferative lesions (Figure 2B). Immunohistochemistry of right hemicolon showed CD20 (+), PAX5 (+), CD3 (+), CD5 (+), CD30 (-), ALK (-), CD10 (-), CD43 (+), Bcl-6 (-), Bcl-2 (+), CD21 (FDC+), CD23 (-), Ki67 (+, about 80%), MUM1 (-), EMA (-), CKpan (-), CD138 (individual+), Kappa (scattered +), Lambda (scattered +), Cyclind1 (-), CD19 (+), c-Myc (+, <30%), PD-1 (-), P53 (scattered +), indicating T cells proliferated significantly in the muscular layer of intestinal wall.
In July 2018, the patient relieved the deep color bloody stool with clot followed by gradually aggravated pain symptoms (the pain score 7), he came to outpatient department of our hospital again. The previous pathological sections were sent to another hematological research institute for diagnosis. Spleen pathology was consistent with SDRPSBCL. Bone marrow immunophenotyping by flow cytometry detected abnormal cell group accounting for 1.96% of nuclear cells, which strongly expressed CD19, CD22 and CD20, expressed FMC7, Kappa, slgD, CD11c, CD103 without expressing CD5, CD10, CD23, CD200, Lambda, CD38, CD25, slgM and CD123, manifesting B-cell lymphoma had invaded bone marrow. The results of whole body Emission Computed Tomography (ECT) (Figure 1B): 1. The glycometabolism in the operation area of intestinal tract was increased slightly; 2. Local rectal wall thickening was associated with abnormal glucose metabolism. Enteroscopy: huge ulcers could be seen in the ileocecum and rectum at the 4cm of the anal entrance (Figure 3A). The intestinal pathological examination (Figure 4A) on 24 July 2018 showed acute/chronic inflammation of mucosa and proliferation of local granulation tissue in the ileocecal region and rectum.
After the diagnosis of SDRPSBCL was confirmed and excluded the contraindication of chemotherapy, the patient was treated by CHOP regimen chemotherapy [cyclophosphamide (1g D1), epirubicin (40mg D1-2), vindesine (4mg D1) and hydroprednisone (60mg D1-7)] on 15 August 2018 (for economic reason, the patient refused to use CD20 antibody). He was treated with an identical CHOP regimen for 4 cycles on 7 September, 1 October, 29 October and 21 November, 2018, respectively. After the first chemotherapy, the patient did not have any bloody stool. After the second cycle of chemotherapy, the sensation of anal pain was relieved significantly and the pain score was 4 and after the fourth course of chemotherapy, the pain score was only 2. Enteroscopy on 19 November, 2018 indicated there were ulcers in the terminal ileum, multiple ulcers and polyps of the colon (shown in Figure 3B). The pathological findings (Figure 4B) were chronic inflammation of the terminal ileal mucosa with acute/chronic inflammation of the ascending colon and the rectum.
There was no pain in the anus after the sixth cycle of chemotherapy on 30 December, 2018 (identical CHOP regimen as before). The blood routine examination was shown as follows: WBC count 8.7 x109/L, RBC 3.68 x1012/L, Hb 89 g/L and PLT 395 x109/L. Bone marrow morphology (29 December, 2018): no abnormality in each cell system and no lymphoma cells were found in bone marrow. PET-CT (Figure 1C) (29 December, 2018) demonstrated there was no increase in the glucose metabolism in the operation area. According to International Working Group consensus response evaluation criteria in lymphoma (RECIL 2017),16 the status of the patient was complete remission (CR). Because of the poor economic situation, he did not agree autologous or allogeneic hematopoietic stem cell transplantation (HSCT) after the last chemotherapy. Until recently, he is still in CR.
Discussion
As the uncommon B-cell lymphoma with a diffuse pattern of involvement of the splenic red pulp by small monomorphous B lymphocytes, SDRPSBCL has the special features of pathomorphology and immunohistochemistry. The structure of splenic red and white pulp disappears, with diffuse infiltration of lymphoid cells, medium-sized, and characteristic intrasinusoidal aggregates with occasional pseudosinuses lined by lymphoma cells having a round hyperchromatic nucleus with clumped chromatin and basophilic cytoplasm. The Immunostaining study on spleen section shows usually that CD20+, DBA44+, AnnexinA1-, CD123-, CD5-, CD43-, Cyclin D1-, CD21-, CD23-, CD10-, CD25-, CD38-, and the low proliferative index of Ki-67. For this patient in the study, there were no obvious features of lymphoma cells via pathology method without direct diagnosis as SDRRPSBCL, so combined with pathological section and bone marrow immune classification, the diagnosis of SDRRPSBCL was confirmed and the bloody stool was not ruled out because of lymphoma involving the intestinal tract. Although the results of intestinal biopsy did not support the infiltration of lymphoma cells, after six cycles of CHOP regimens, the primary disease and intestinal tract of the patient were alleviated obviously. We reviewed the relative articles and stated the hypothesis of lymphoma with GIH as follows:
- The lymphoma locates in the gastrointestinal tract. The gastrointestinal tract is the most common site for extranodal lymphomas.17 One literature18 reported the gastroscopy of the patient revealed a large malignant ulcer in the stomach; biopsy histologic examination showed the ulcer was benign. A radical gastrectomy was performed and the diagnosis was classic Hodgkin’s lymphoma. Although no lymphoma cells were detected in the intestinal ulcer of the patient in our hospital, we still suspected that the patient had splenic lymphoma infiltration in the intestinal tract; nevertheless, there might be limitations of sampling without providing direct evidence of lymphoma, thus lymphoma cells could not be found.
- Lymphoma cells invade the splenic vein, resulting in portal hypertension and eventually lead to isolated gastric varices (IGV) formation. Chen et al.19 reported a patient was admitted due to vomiting coffee-like gastric contents with tarmac stool. Gastroscopy showed gastric varices and the results of abdominal CT were as follows: spleen was enlarged and splenic vein was occluded, then the splenic biopsy was performed with the diagnosis as diffuse large B-cell lymphoma. The splenic vein occlusion disappeared after CHOP chemotherapy. After splenic vein blockage caused by lymphoma, the blood pressure was increased when passing through the short gastric vein, which resulted in the formation of IGV, rupture of the involved vein at any time and severe gastrointestinal bleeding.
Conclusion
The diagnosis of SDRPSBCL was confirmed and the clinical stage was IVb stage. After the first course of chemotherapy, the symptoms of hematochezia disappeared. After the sixth cycle of chemotherapy, anal pain disappeared. Followed up until 18 April, 2020, he is still in CR. The examinations of colonoscopy and PET-CT have been reviewed, showing the primary disease and GIH have both alleviated significantly.
Ethics Statement
Written informed consent was obtained from the patient for publication of this case and accompanied images. This research was approved by the Ethics Committee at the affiliated hospital of Xuzhou Medical University and was conducted according to the guidelines put forth in the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation of China [grant numbers 81600145, 81700199, 81800159 and 81900179], the Natural Science Foundation of Jiangsu Province [grant numbers BK20160232 and BK20180271], China Postdoctoral Science Foundation [grant number 2016M590508], the Foundation of Jiangsu Province Six Talents Peak [grant number 2015-WSW-058], the Foundation of Jiangsu Province Six-one Project [grant number LGY2018084], Jiangsu Province Postgraduate Practice Innovation Program [grant number SJCX19_0936] and the Clinical Technology Backbone Training Program of Xuzhou City [grant number 2018GG002].
Disclosure
Yanqiu Xu and Xiaohui Fan are co-first authors for this study. The authors declare no conflicts of interest in this work.
References
1. Swerdlow SH, Campo E, Harris NL, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC Press; 2008.
2. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–2390. doi:10.1182/blood-2016-01-643569
3. Gujral S, Lad P, Subramanian PG, et al. Histopathological audit of splenectomies received at a cancer hospital. Indian J Pathol Microbiol. 2011;54(3):487–496. doi:10.4103/0377-4929.85080
4. Vig T, Kodiatte TA, Manipadam MT, Aboobacker FN. A rare case of splenic diffuse red pulp small B-cell lymphoma (SDRPL): a review of the literature on primary splenic lymphoma with hairy cells. Blood Res. 2018;53(1):74–78. doi:10.5045/br.2018.53.1.74
5. Shimizu-Kohno K, Kimura Y, Kiyasu J, et al. Malignant lymphoma of the spleen in Japan: a clinicopathological analysis of 115 cases. Pathol Int. 2012;62(9):577–582. doi:10.1111/j.1440-1827.2012.02844.x
6. Cheng WY, Zhu YM, Cheng S, Chen YS, Shen Y. Development of B-cell prolymphocytic leukemia in a patient with splenic diffuse red pulp small B-cell lymphoma. Leuk Lymphoma. 2018;59:1990–1993.
7. Curiel-Olmo S, Mondéjar R, Almaraz C, et al. Splenic diffuse red pulp small B-cell lymphoma displays increased expression of cyclin D3 and recurrent CCND3 mutations. Blood. 2017;129(8):1042–1045. doi:10.1182/blood-2016-11-751024
8. Kanellis G, Mollejo M, Montes-Moreno S, et al. Splenic diffuse red pulp small B-cell lymphoma: revision of a series of cases reveals characteristic clinico-pathological features. Haematologica. 2010;95(7):1122–1129. doi:10.3324/haematol.2009.013714
9. Yamada Y, Miura M, Tagari M, et al. Splenic diffuse red pulp small B-cell lymphoma diagnosed by splenectomy initially mimicking hairy cell leukemia- Japanese variant. Rinsho Ketsueki. 2018;59:281–286.
10. Traverse-Glehen A, Baseggio L, Salles G, Coiffier B, Felman P, Berger F. Splenic diffuse red pulp small B-cell lymphoma: toward the emergence of a new lymphoma entity. Discov Med. 2012;13:253–265.
11. Traverse-Glehen A, Baseggio L, Bauchu EC, et al. Splenic red pulp lymphoma with numerous basophilic villous lymphocytes: a distinct clinicopathologic and molecular entity? Blood. 2008;111:2253–2260. doi:10.1182/blood-2007-07-098848
12. Miyake T, Iida T, Masaki Y, et al. A case of nodal malignant lymphoma presenting with arterial bleeding related to its duodenal penetration. Clin J Gastroenterol. 2018;11(3):229–234. doi:10.1007/s12328-018-0827-7
13. Zhang L, Wang H. Imaging characteristics of gastrointestinal neoplastic acute abdomen. Zhonghua Wei Chang Wai Ke Za Zhi. 2018;21:1223–1229.
14. Obleagă CV, Vere CC, Pătraşcu AM, et al. Severe upper gastrointestinal bleeding determined by a gastric lymphoma associated with Helicobacter pylori-positive atrophic gastritis. ROM J Morphol Embryol. 2017;58:611–617.
15. Ahmed R, Kumar K, Makker J, Niazi M, Balar B. Recurrent mantle cell lymphoma presenting as gastrointestinal bleeding. Case Rep Gastroenterol. 2018;12:379–384. doi:10.1159/000488193
16. Younes A, Hilden P, Coiffier B, et al. International Working Group consensus response evaluation criteria in lymphoma (RECIL 2017). Ann Oncol. 2017;28(7):1436–1447. doi:10.1093/annonc/mdx097
17. Hossain FS, Koak Y, Khan FH. Primary gastric Hodgkin’s lymphoma. World J Surg Oncol. 2007;5(1):119. doi:10.1186/1477-7819-5-119
18. Pandey M, Swain J, Iyer HM, Shukla M. Primary lymphoma of the colon: report of two cases and review of literature. World J Surg Oncol. 2019;17(1):18. doi:10.1186/s12957-018-1548-6
19. Chen BC, Wang HH, Lin YC, Shih YL, Chang WK, Hsieh TY. Isolated gastric variceal bleeding caused by splenic lymphoma-associated splenic vein occlusion. World J Gastroenterol. 2013;19(40):6939–6942. doi:10.3748/wjg.v19.i40.6939
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.