Back to Journals » International Journal of Women's Health » Volume 15
Sociodemographic Predictors of Initiating Antenatal Care Visits by Pregnant Women During First Trimester of Pregnancy: Findings from the Afghanistan Health Survey 2018
Authors Tawfiq E, Fazli MR, Wasiq AW , Stanikzai MH , Mansouri A, Saeedzai SA
Received 1 January 2023
Accepted for publication 24 March 2023
Published 1 April 2023 Volume 2023:15 Pages 475—485
DOI https://doi.org/10.2147/IJWH.S399544
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Essa Tawfiq,1 Mohammad Rafi Fazli,2 Abdul Wahed Wasiq,3 Muhammad Haroon Stanikzai,4 Amena Mansouri,5 Sayed Ataullah Saeedzai6
1Department of Epidemiology and Biostatistics, School of Population Health, the University of Auckland, Auckland, New Zealand; 2Department of Surgery, Faculty of Medicine and Health Science, the University of Auckland, Auckland, New Zealand; 3Internal Medicine Department, Faculty of Medicine, Kandahar University, Kandahar, Afghanistan; 4Public Health Department, Faculty of Medicine, Kandahar University, Kandahar, Afghanistan; 5Formerly Ghalib Teaching Hospital, Herat, Afghanistan; 6Ministry of Public Health, Kabul, Afghanistan
Correspondence: Essa Tawfiq, Building 507, Level 1, Room 1038, 28 Park Avenue, Grafton, Auckland, 1023, New Zealand, Tel +64 210661149, Email [email protected]
Purpose: Initiating antenatal care (ANC) visits by pregnant women during first trimester, known as timely initiation of ANC visits, is crucial for wellbeing of mothers and their unborn babies. We examined whether sociodemographic characteristics of pregnant women predict timely initiation of ANC visits.
Patients and Methods: Data collected for the Afghanistan Health Survey 2018 (AHS 2018) were analyzed. A binary outcome variable was created as women with ANC visits in 0– 3 months (first trimester) vs women with ANC visits in ≥ 4 months of pregnancy. A multivariable generalized linear model was employed.
Results: A total of 6862 ever-married women, aged 14– 49 years, with a history of pregnancy, including current pregnancy, were included. The prevalence of timely initiation of ANC visits was 55.8%. The likelihood (OR = odds ratio) of timely initiation of ANC visits was higher in women aged 30– 39 years [OR 1.12 (95% CI: 1.00– 1.25)], in women who could read and write [OR 1.12 (95% CI: 0.99– 1.21)], in women who used public primary care facilities [OR 1.14 (95% CI: 1.01– 1.28)], in women who received consultation on ANC from a doctor or midwife [OR 1.22 (95% CI: 0.72– 2.08), OR 1.13 (95% CI: 0.67– 1.92)] respectively, in women at fourth and highest quintiles of wealth status [OR 1.24 (95% CI: 1.04– 1.48), OR 1.14 (95% CI: 0.92– 1.40)] respectively, in women who intended to become pregnant [OR 1.56 (95% CI: 1.35– 1.81)], in women who used the internet [OR 1.53 (95% CI: 1.13– 2.06)], and in women who listened to radio [OR 1.16 (95% CI: 1.03– 1.30)]. However, the likelihood was lower in women who had given birth at least twice [OR 0.67 (95% CI: 0.50– 0.89)], and in women who lived in rural areas [OR 0.87 (95% CI: 0.75– 1.00)].
Conclusion: To promote timely initiation of ANC visits, healthcare interventions to increase availability of midwives and doctors, and improve accessibility to primary care clinics, especially in rural areas, need to be implemented.
Keywords: ANC, timely ANC, early ANC, late ANC
Introduction
Maternal mortality is unacceptably high in low- and middle-income countries (LMICs).1,2 The South Asia region alone accounts for approximately one-third of maternal mortality worldwide.3 Inadequate access of pregnant women to quality antenatal care (ANC) contributes substantially to these preventable maternal deaths.4 Pregnancy and childbirth are a period of high vulnerability for both mothers and their unborn babies.5,6 Adequate use and timely initiation of ANC visits can contribute significantly to decrease maternal and neonatal morbidity and mortality in LMICs.5,7,8
Utilization of adequate ANC services and timely initiation of ANC visits (<12 weeks of gestation) is low in Afghanistan.9–12 In Afghanistan, utilization of adequate ANC visits was reported to be 16.5%, 21.7%, and 30.5%,9–11 and timely initiation of ANC visits was revealed to be 33.1%, 48.8%, and 57%.9,11,12 WHO’s latest recommendation of a minimum of eight ANC visits signifies the key role of ANC services to reduce perinatal mortality and improve women’s health.13 Timely initiation of ANC visits and receiving the required health services and nutritional advice for pregnant women is emphasized by WHO.5 WHO emphasizes the initiation of early ANC visits as soon as conception occurs. For example, women are advised to start taking oral iron and folic acid supplements to prevent maternal anaemia, puerperal sepsis, low birth weight, and preterm birth early in pregnancy; and women are even advised to commence taking folic acid supplements before conception in order to prevent neural tube defects in babies.5
ANC is defined as the care a pregnant woman or young woman receives from a skilled healthcare professional in order to ensure the best health outcomes for the mother and her baby during pregnancy.5 ANC aims to identify risk, prevent, and manage pregnancy-related health conditions, and provide nutritional and health education to women of reproductive age. To ensure optimum care, WHO recommends that every pregnant woman should receive a minimum of eight ANC visits throughout the pregnancy, with the first visits occurring in the first trimester of pregnancy.13
Initiation of ANC attendance during the first trimester of pregnancy and optimal ANC care are crucial for the wellbeing of pregnant women and their unborn babies.14,15 Latest studies from LMICs provide evidence on the significant role of sociodemographic determinants of initiating ANC visits among pregnant women during the first trimester of pregnancy.16–33 Studies from Afghanistan reported strong associations of sociodemographic and cultural influencers with the utilization of ANC services.9–12 Two of the studies in Afghanistan examined early and late initiation of ANC visits,11,12 and both studies found that husband’s education, woman’s age, education, socioeconomic status, residential area, and family size were associated with timely (or late) initiation of ANC services by pregnant women. Husband’s occupation was strongly associated, but pregnancy intention was not associated with early initiation of ANC visits;11 however, the other study found that unplanned pregnancy and women’s lack of knowledge on timing of ANC attendance were strongly associated with late ANC initiation.12 The above studies did not examine the effects of women’s access to media, parity, women’s consultation for ANC services by type of healthcare professionals, and by type of health facilities. Considering the above gap in knowledge, in this study we examined the sociodemographic predictors of timely ANC initiation in ever-married women during their latest pregnancies.
Materials and Methods
Study Design
Data collected between March and August 2018 from 19,684 randomly selected households in the 34 provinces for the Afghanistan Health Survey 2018 (AHS 2018) were used.34 After stratifying clusters by urban and rural areas, a two-stage sampling approach was employed. At the first stage, household listing was carried out in the selected clusters, and at the second stage the list of occupied residential households was used as the sampling frame from which the required number of households were randomly selected via a systematic sampling approach within each cluster. The resulting list of selected households was used to conduct the survey. To minimize the chance of selection bias, no replacements in the selected households were allowed.
In our study, data were analyzed from ever-married women, aged 14–49 years, who gave birth in the past two years prior to the survey or those who were currently pregnant. The latest pregnancy either in the past two years or the current pregnancy was used to minimize recall bias by the respondent women who were either previously or currently pregnant. During the survey, women were interviewed by trained surveyors who used a questionnaire on seeking reproductive healthcare for women. The questionnaire on wealth status, demographic and health characteristics of the household members was used for interviewing the head of the household.
Statistical Analysis
We used data from pregnant women (currently or previously pregnant) who had at least one ANC visit during pregnancy, and their data on the outcome and explanatory variables was complete in the database. A binary outcome variable was created as women with ANC visits in 0–3 months vs women with ANC visits in ≥4 months of pregnancy. The binary outcome variable was coded as timely ANC if a woman attended one or more ANC visits in the first trimester (0–3 months) of her pregnancy and as late ANC otherwise. The explanatory variables included in the analysis were: woman’s age (14–29 years, 30–39 years, and 40–49 years), woman’s literacy (whether or not she could read and write), husband’s literacy (whether or not he could read and write), parity (the woman had not given birth [nullipara], the woman had given birth once (primipara), the woman had given birth at least twice [multipara]), type of health facility the woman attended for ANC services (private clinic, public primary care facility, public hospital), type of health worker the woman consulted with for ANC services (nurse and/or community health worker, doctor, midwife), residential area (urban vs rural), wealth status (wealth quintile from the lowest to highest), household size (2–4 people vs ≥5 people), pregnancy intention (whether or not she intended to become pregnant), access to the internet (whether or not she used the internet daily or weekly for consulting for her healthcare), access to radio (whether or not she listened to radio daily or weekly), and access to TV (whether or not she watched TV daily or weekly). For variables on access to radio, access to TV, and access to the internet, we coded those women with “less than once a week access” as part of those who did not have access to the media. The variable on wealth status was created by principal component analysis, using the household ownership of assets, household use of amenities of life, and construction material used for the household properties. We specified a generalized linear model (GLM) with binary outcome for the multivariable analysis (below):
 refers to the outcome variable for woman i (whether or not she attended ANC visits during first trimester of her pregnancy), with j category of explanatory variables. βj refers to the odds ratio (OR) of attending ANC visits during first trimester for each category of explanatory variables, except the reference category of the variable.
refers to the outcome variable for woman i (whether or not she attended ANC visits during first trimester of her pregnancy), with j category of explanatory variables. βj refers to the odds ratio (OR) of attending ANC visits during first trimester for each category of explanatory variables, except the reference category of the variable.  denotes a vector of explanatory variables, and K refers to the number of explanatory variables. β0 stands for the intercept, and
denotes a vector of explanatory variables, and K refers to the number of explanatory variables. β0 stands for the intercept, and  refers to the error term. We also fitted the above statistical model for bivariable analysis where the association between the outcome and each predictor was examined, without adjusting the model for all predictors in the study. During analysis, we added a random cluster effect in our model estimates to take the clustering effects of data at household level into account and adjusted standard errors for the ORs and 95% CI. Data were analyzed in Stata version 13.35
refers to the error term. We also fitted the above statistical model for bivariable analysis where the association between the outcome and each predictor was examined, without adjusting the model for all predictors in the study. During analysis, we added a random cluster effect in our model estimates to take the clustering effects of data at household level into account and adjusted standard errors for the ORs and 95% CI. Data were analyzed in Stata version 13.35
Results
Table 1 presents baseline characteristics of ever-married women who utilized ANC services during their latest pregnancies. The table shows that nearly two-thirds (63.1%) of women were 14–29 years old, followed by 30.2% of women aged 30–39 years, and 6.7% of women aged 40–49 years. The proportion of women and proportion of husbands who could read and write were 21.5% and 40.8%, respectively. Majority of women (83.0%) had given birth two times or more, followed by 12.9% who had given birth once, and 4.1% women who had not given birth yet. A considerable proportion of women received ANC service from private clinics (43.8%), followed by 39.3% from public primary care clinics, and 16.9% from public hospitals. Midwives provided ANC services to over two-thirds of women (66.2%), followed by doctors (32.9%), and 0.9% by nurses or community health workers (CHWs). Majority of women (74.2%) lived in rural areas, and the remaining quarter (25.8%) lived in urban areas. Women by wealth status ranged from 13.6% to 24.7%, from the lowest (poorest) to the highest quintile (richest). Majority of women (86.8%) lived in households with at least five people, and the remaining 13.2% of women lived in households with 2 to 4 people. Only 16.9% of women had intended to become pregnant for their latest pregnancies. The proportion of women with daily or weekly access to the internet, radio, and TV was 3.4%, 26.7%, and 39.1%, respectively.
 |
Table 1 Characteristics of Women Who Utilized Antenatal Care Services During Pregnancy |
Figure 1 depicts initiation of ANC visits (≥1 visits) by pregnant women during their latest pregnancies. It shows that 1 out of 2 pregnant women commenced timely ANC attendance (55.8% = 3832/6862), followed by 32.3% (2217/6832) and 11.9% (813/6832) who initiated ANC visits during second and third trimesters, respectively.
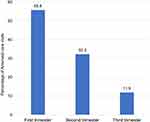 |
Figure 1 Timing of antenatal care visits by pregnant women. |
Table 2 displays odds ratios (ORs) on the likelihood of initiating timely ANC visits by the respondent women during their latest pregnancies. Results from multivariable analysis show that it was more likely [OR 1.12 (95% CI 1.00–1.25)] that women, aged 30–39 years commenced timely ANC visits compared with women aged 14–29 years. Compared with women who could not read and write, it was more likely that women who could read and write commence timely ANC visits [OR 1.12 (95% CI 0.99–1.21)]. Husband’s literacy was not associated with the initiation of timely ANC visits. Compared with pregnant women who had not given birth yet, the likelihood of initiating timely ANC visits was smaller by women who had given birth at least twice in the past [OR 0.67 (95% CI 0.50–0.89)]. Compared with women who visited private clinics for ANC services, it was more likely for women who used public primary care facilities to commence timely ANC attendance [OR 1.14 (95% CI 1.01–1.28)]. Compared with women who received consultation for ANC services by a nurse or CHW, it was more likely that women who received consultation from a doctor and from a midwife to commence timely ANC visits [OR 1.22 (95% CI 0.72–2.08, and OR 1.13: 95% CI 0.67–1.92, respectively)]. Compared with women who lived in urban areas, for women who lived in rural areas it was less likely to commence timely ANC attendance [OR (95% CI) of 0.87 (0.75–1.00)]. Compared with women at the lowest wealth status quintile, women at the second highest and highest status were more likely to commence timely ANC visits [OR (95% CI) of 1.24 (1.04–1.48), and 1.14 (0.92–1.40)], respectively. The likelihood of initiating timely ANC visits in women at the second lowest quintile as well as those at the middle quintile of wealth status were not much different from the women at the lowest quintile. Initiating timely ANC attendance was not much different for women living in households with 2–4 people vs women living in households with ≥5 people. Compared with women who did not intend to become pregnant, women who intended to become pregnant were more likely to initiate timely ANC attendance [OR (95% CI) of 1.56 (1.35–1.81)]. Access to media had positive effects on initiating timely ANC visits. Compared with women who did not use internet, for women who used internet daily or weekly it was more likely to initiate timely ANC attendance [OR (95% CI) of 1.53 (1.13–2.06)]. Likewise, for women who listened to radio daily or weekly, it was more likely to initiate timely ANC visits [OR (95% CI) of 1.16 (1.03–1.30)]. However, a slightly weaker association was found for women who watched TV daily or weekly [OR (95% CI) of 1.09 (0.97–1.23)].
 |
Table 2 Likelihood of Initiating ANC Visits by Pregnant Women in the First Trimester |
In Table 2 we also present results from bivariable analysis. We found that the likelihood of initiating timely ANC visits was significantly lower in women aged 40–49 years, as compared to women aged 14–29 years [OR (95% CI) of 0.80 (0.66–0.98)]. It was found that husband’s literacy is a strong predictor of initiating timely ANC among pregnant women [OR 1.17 (95% CI 1.06–1.29)]. A strong association between household size of ≥5 people and timely initiation of ANC was revealed [OR (95% CI) of 0.84 (0.73–0.97)]. The effect of watching TV daily or weekly was significant for the initiation of timely ANC visits [1.27 (1.15–1.40)]. Bivariable analysis, however, did not identify strong associations between timely initiation of ANC and type of health facilities.
Discussion
In this study of 6862 ever-married women, aged 14–49 years, we found that 55.8% of women commenced ANC attendance during first trimester of pregnancy. Nearly two-thirds of women were 14–29 years old, and only 4.1% had not given birth previously. Midwives and doctors provided ANC services to pregnant women. Out of 4 women, 3 of them lived in rural areas. Only 16.9% of women intended their pregnancies. Access to media was low, particularly access to the internet. The multivariable analysis showed that the likelihood of initiating timely ANC attendance was higher in women aged 30–39 years old, in women who could read and write, in women who were pregnant for the first time, in women who used public primary care facilities, in women who consulted a doctor or midwife for ANC services, in women who lived in urban areas, in women who had higher wealth status, in women who intended to become pregnant, and in women who had daily or weekly access to the media (radio and the internet). It was revealed that husband’s literacy, household size, and watching TV daily or weekly were not strong predictors of initiating timely ANC attendance by pregnant women. However, bivariable analysis found that husband’s literacy, household size, and watching TV daily or weekly were strong predictors of timely initiation of ANC visits among pregnant women. The direction of the effect size for the above three predictors of timely commencement of ANC attendance by pregnant women was not different between the results obtained from multivariable analysis and bivariable analysis. The results from bivariable analysis did not take the confounding or modifier effects of other predictors into account; however, multivariable analysis adjusted results for all predictors in the model. This may be a reason for the differences between the results from multivariable and bivariable analyses.
Previous studies from LMICs found that the prevalence of initiating timely ANC attendance by pregnant women varies substantially from country to country, and even by regions within a country. For example, in a recent multi-country analysis of Demographic and Health Surveys from sub-Saharan Africa, it was found that the percentage of pregnant women commencing timely ANC visits ranged from 14.5% in Mozambique to 68.6% in Liberia.24 Findings from several other LMICs reported that the prevalence of initiating timely ANC attendance was as low as 11% in a geographic region of Bangladesh,36 and as high as 65.7% in an urban area in Ethiopia.20 In Ethiopia, three studies from three regions of the country reported early ANC initiation of 19.5%,37 31.5%,17 and 57.8%.19 The prevalence of 55.8% found in our study supports the findings from several previous studies in LMIC settings. However, our finding of 55.8% was higher than the findings reported in two previous studies from Afghanistan,11,12 which revealed that 33.1% and 48.8% of pregnant women initiated timely ANC attendance. A reason for the difference of 22.7% (55.8% vs 33.1%) could be related to the months when data were collected for the two studies; in our study we used data collected between March and August 2018 from ever-married women who reported their use of ANC attendance in the past 2 years, including currently pregnancy women; however, in the study from Afghanistan,12 data were collected from currently pregnant women over a period of three months. This shorter time span may have contributed to a possible under-reporting of ANC attendance in their study.12 Our finding of 55.8% of timely ANC initiation is similar to the finding of 57% reported by a separate study from Afghanistan.9 Another study from Afghanistan that used data from the Afghanistan Demographic and Health Survey 2015 reported the prevalence of timely ANC initiation to be 48.8%,11 which has a difference of 7% from our finding.
Previous studies from LMICs reported significant associations between timely initiation of ANC attendance by pregnant women and women’s age,17,18,20,22–25,30–32,37 wealth status,18,24,25,31,33,37 education,18,21–25,29,31 parity,18,20,23–27,29,32 access to media,23,24,28,31,38 pregnancy intention,16,19,21,23,24,26,27,29–31,39 residential area,24,29,36 family size,17,29 and husband’s education.19,36 Except for the statistically insignificant correlation of husband’s education with pregnant women’s timely ANC attendance, our findings on the higher odds of pregnant woman’s timely ANC attendance by age, education, wealth status, parity, pregnancy intention, residential area, and access to media were fairly consistent with previous studies. A recent study, which used data from the demographic and health survey (DHS) of 36 African countries, found strong associations of sociodemographic and contextual factors with the likelihood of timely initiation of ANC visits by pregnant women.24 The authors reported that the likelihood of initiating timely ANC visits was significantly higher in women with secondary education and higher education, women aged 25–34 years, women from richest households, women perceiving distance from the health facility as not a big problem, women exposed to media, and women residing in communities with medium or higher percentage of literacy. The authors found that the likelihood of timely ANC commencement was significantly lower in women who wanted their pregnancy later, women who wanted no more pregnancies, and women living in the rural area.24 Our findings, overall, are consistent with the findings reported from the above multi-country analysis.24 Our findings are also consistent with those reported previously from Afghanistan,11,12 except for husband’s education and family size, which were not strong predictors of initiating ANC visits in the first trimester of pregnancy in our study. However, we cannot state that there is no association between timely (or late) ANC initiation and husband’s education or family size, as research from LMIC settings provides evidence that husband’s education and family size have significant influence on timely initiation of ANC attendance by pregnant women.9,12,17,19,36 In our study, the bivariable analysis, however, showed strong associations of family size, husband’s education, and exposure to TV with timely initiation of ANC visits. Likewise, the results from multivariable analysis showed higher likelihood of timely ANC initiation in women who reside in households with fewer number of people, women whose husbands were educated, and women with daily or weekly exposure to TV; however, the level of associations, shown as odds ratios, was not statistically significant.
The strengths of our study are the employment of data from a nationally representative sample, and use of data from ever-married women who reported use of ANC service over the past two years. The use of data from this national survey allows generalizability of our findings at the national level and the comparison of our findings to those studies from LMICs that employed nationally representative samples. In addition, the relatively large sample size in our study may increase the validity and statistical power of the findings. Unlike our study, several studies from LMICs used smaller sample sizes, and the samples for most of them were confined to a specific geographic location, which may limit generalizability of their findings.9,12,18,20,37–39 In our study, the data reported by ever-married women over the past two years also allowed us to capture seasonal variability in the utilization of ANC services in different regions of Afghanistan and gather data from more pregnant women. To our knowledge, timely initiation of ANC attendance by type of health workers and health facilities has not been examined previously, and our study found that it was more likely that pregnant women initiate timely ANC visits when the ANC services are provided by a midwife or doctor, or when the ANC services are offered from a public primary care clinic.
Our findings have the potential to influence healthcare policies and interventions to promote utilization of timely ANC attendance by pregnant women. The prevalence of 55.8% of pregnant women who initiated timely ANC shows that 44.2% of pregnant women commenced late ANC visits. This may inform policy makers to decide about the development and revision of health policies and interventions on the utilization and timing of ANC services. Moreover, our findings that 2 out of 3 women were under 29 years of age can be used to target younger women to educate them about the importance and timing of ANC attendance. The importance of early initiating of ANC attendance has been emphasized among young women and girls.5 Considering the crucial role of educating women on the utilization and timing of ANC services, one solution is that healthcare managers and policy makers opt to employ community-based and health facility-based health promotion interventions to increase communities’ and women’s awareness of ANC utilization and early initiation, particularly in rural areas. Another solution is to strengthen and expand education in the country, with at least primary education in rural areas, to improve women’s and children’s health in the long term. The findings on the type of healthcare professionals or health facilities may be used by healthcare managers and policy makers to prioritize and allocate resources on the deployment of health workers, and establishment and functioning of public primary care facilities, especially in rural areas. The findings on the important role of media on the utilization and timely initiation of ANC services can be used to disseminate health education messages related to ANC services targeting women and girls, husbands, and community leaders.
A limitation of our study is the use of months instead of weeks to determine the first trimester of pregnancy. This limitation may have misclassified some women either to first trimester or second trimester or vice versa. Another limitation concerns the recall bias potentially emerging from data collected from a respondent based on her past experience over a period of time.40 Because women provided the responses on the number of ANC visits from the past two years, it may be the case that the women over- or under-reported the number of ANC visits or may have misclassified the type of health worker or health facility that provided the services. Another issue with bias is the social desirability bias, which may have occurred during the interviews.41 In the case of social desirability bias, the respondent women may have over-reported the utilization or timely initiation of ANC services. A further limitation in our study is the lack of information on women’s knowledge of timing and importance of ANC visits, because previous studies have reported a strong relationship between women’s previous knowledge and awareness of ANC timing and the timely initiation of ANC attendance by pregnant women.12,19,36
Future research may investigate the relationship of associated cost of utilizing ANC services as well as the distance to public health facilities with timely initiation of ANC visits. Another area to explore may be related to the decision-making role of the husband, including husband’s occupation, and close relatives in relation to women’s timely initiation of ANC visits, as well as women’s and husbands’ knowledge of timely ANC initiation, including danger signs during pregnancy. Women’s satisfaction with quality of maternal care and its relationship with timely ANC initiation will be an interesting area to explore. Furthermore, the outcomes of late initiation of ANC visits will be an area for future research.
Conclusion
Health policy and interventions are needed to promote early initiation of ANC visits by pregnant women. Community-based and health facility-based interventions need to be implemented to promote utilization and early initiation of ANC attendance, considering our findings on the important role of media, type of health worker and health facility, residential area, and women’s age and education.
Data Sharing Statement
Data supporting the findings reported in this article can be requested from the Ministry of Public Health of Afghanistan (contact person: Dr Saeedzai [email protected]).
Ethics Approval
The study was reviewed by the Research and Ethics Committee, Faculty of Medicine, University of Kandahar, Afghanistan. The mentioned research and ethics committee approved the study and waived the ethical application because secondary data from the Afghanistan Health Survey 2018 (AHS2018) were used and analyzed in this study. For the AHS 2018, the ethics approval was obtained from the Institutional Review Board of the Ministry of Public Health of Afghanistan in 2017.
Acknowledgments
We thank the Ministry of Public Health of Afghanistan for sharing the datasets from the Afghanistan Health Survey 2018.
Author Contributions
All authors contributed to data analysis, drafting, and revising the article, and have agreed on the journal to which the article will be submitted. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN maternal mortality estimation inter-agency group. Lancet. 2016;387(10017):462–474. doi:10.1016/S0140-6736(15)00838-7
2. World Health Organization. Maternal mortality. Factsheets, 2021; 2021. Available from: https://wwwwhoint/europe/news-room/fact-sheets/item/maternal-mortality.
3. Alvi MA, Malik MZ, Iqbal S, et al. Approaches towards improving the quality of maternal and newborn health services in South Asia: challenges and opportunities for healthcare systems. Global Health. 2018;14(1):1–8. doi:10.1186/s12992-017-0319-4
4. Lawn JE, Lee AC, Kinney M, et al. Two million intrapartum-related stillbirths and neonatal deaths: where, why, and what can be done? Int J Gynaecol Obstet. 2009;107:S5–19. doi:10.1016/j.ijgo.2009.07.016
5. World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva: World Health Organization; 2016.
6. Okedo-Alex IN, Akamike IC, Ezeanosike OB, Uneke CJ. Determinants of antenatal care utilisation in sub-Saharan Africa: a systematic review. BMJ open. 2019;9(10):e031890. doi:10.1136/bmjopen-2019-031890
7. Haftu A, Hagos H, Mehari M-A, Gher B. Pregnant women adherence level to antenatal care visit and its effect on perinatal outcome among mothers in Tigray public health institutions, 2017: cohort study. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3987-0
8. Lucas AO, Stoll BJ, Bale JR Improving birth outcomes: meeting the challenge in the developing world; 2003.
9. Stanikzai MH, Wafa MH, Wasiq AW, Sayam H. Magnitude and determinants of antenatal care utilization in Kandahar city, Afghanistan. Obstet Gynecol Int. 2021;2021:1. doi:10.1155/2021/5201682
10. Azimi MW, Yamamoto E, Saw YM, et al. Factors associated with antenatal care visits in Afghanistan: secondary analysis of Afghanistan demographic and health survey 2015. Nagoya J Med Sci. 2019;81(1):121. doi:10.18999/nagjms.81.1.121
11. Alemi S, Nakamura K, Rahman M, Seino K. Male participation in antenatal care and its influence on their pregnant partners’ reproductive health care utilization: insight from the 2015 Afghanistan demographic and health survey. J Biosoc Sci. 2021;53(3):436–458. doi:10.1017/S0021932020000292
12. Samiah S, Stanikzai MH, Wasiq AW, Sayam H. Factors associated with late antenatal care initiation among pregnant women attending a comprehensive healthcare facility in Kandahar Province, Afghanistan. Indian J Public Health. 2021;65(3):298. doi:10.4103/ijph.IJPH_62_21
13. Lattof SR, Moran AC, Kidula N, et al. Implementation of the new WHO antenatal care model for a positive pregnancy experience: a monitoring framework. BMJ Glob Health. 2020;5(6):e002605. doi:10.1136/bmjgh-2020-002605
14. Nagatani S, Horiuchi S, Takahashi K, Matsuura M, Ounchit K, Yamaoka K. Risk of low birthweight associated with the timing and frequency of antenatal care visits in Lao PDR: a retrospective cohort study. BMC Pregnancy Childbirth. 2023;23(1):1–9. doi:10.1186/s12884-023-05442-7
15. Tesfay N, Hailu G, Woldeyohannes F. Effect of optimal antenatal care on maternal and perinatal health in Ethiopia. Front Pediatr. 2023;11:30. doi:10.3389/fped.2023.1120979
16. Battu GG, Kassa RT, Negeri HA, kitawu LD, Alemu KD. Late antenatal care booking and associated factors among pregnant women in Mizan-Aman town, South West Ethiopia, 2021. PLOS Global Public Health. 2023;3(1):e0000311. doi:10.1371/journal.pgph.0000311
17. Debelo BT, Danusa KT. Level of late initiation of antenatal care visit and associated factors amongst antenatal care attendant mothers in Gedo General Hospital, West Shoa Zone, Oromia Region, Ethiopia. Front Public Health. 2022;10:5. doi:10.3389/fpubh.2022.866030
18. Venyuy MA, Cumber SN, Nkfusai CN, et al. Determinants to late antenatal clinic start among pregnant women: the case of Saint Elizabeth General Hospital, Shisong, Cameroon. Pan Afr Med J. 2020;35. doi:10.11604/pamj.2020.35.112.18712
19. Tufa G, Tsegaye R, Seyoum D. Factors associated with timely antenatal care booking among pregnant women in remote area of bule hora district, southern Ethiopia. Int J Womens Health. 2020;12:657. doi:10.2147/IJWH.S255009
20. Yezengaw TY Late initiation of antenatal care and associated factors among antenatal care attendees in governmental health centers of Harar Town, Ethiopia; 2022.
21. Tadele F, Getachew N, Fentie K, Amdisa D. Late initiation of antenatal care and associated factors among pregnant women in Jimma Zone Public Hospitals, Southwest Ethiopia, 2020. BMC Health Serv Res. 2022;22(1):1–8. doi:10.1186/s12913-022-08055-6
22. Tesfu AA, Aweke AM, Gela GB, Wudineh KG, Beyene FY. Factors associated with timely initiation of antenatal care among pregnant women in Bahir Dar city, Northwest Ethiopia: cross‐sectional study. Nurs Open. 2022;9(2):1210–1217. doi:10.1002/nop2.1162
23. Shitie A, Azene ZN. Factors affecting the initiation and continuation of maternal health service utilization among women who delivered in the past one year in Enemay district, East Gojjam, Ethiopia. Arch Public Health. 2021;79(1):1–9. doi:10.1186/s13690-021-00689-y
24. Alem AZ, Yeshaw Y, Liyew AM, et al. Timely initiation of antenatal care and its associated factors among pregnant women in sub-Saharan Africa: a multicountry analysis of demographic and health surveys. PLoS One. 2022;17(1):e0262411. doi:10.1371/journal.pone.0262411
25. Appiah F. Individual and community-level factors associated with early initiation of antenatal care: multilevel modelling of 2018 Cameroon demographic and health survey. PLoS One. 2022;17(4):e0266594. doi:10.1371/journal.pone.0266594
26. Redi T, Seid O, Bazie GW, Amsalu ET, Cherie N, Yalew M. Timely initiation of antenatal care and associated factors among pregnant women attending antenatal care in Southwest Ethiopia. PLoS One. 2022;17(8):e0273152. doi:10.1371/journal.pone.0273152
27. Edessa A, Dida N, Teferi E. Early initiation of antenatal care and its associated factors among antenatal care followers at public health facilities in Ambo town administration, Central Ethiopia. J Family Med Prim Care. 2023;12(1):67–75. doi:10.4103/jfmpc.jfmpc_725_22
28. Sserwanja Q, Mutisya LM, Musaba MW. Exposure to different types of mass media and timing of antenatal care initiation: insights from the 2016 Uganda demographic and health survey. BMC Womens Health. 2022;22(1):1–8. doi:10.1186/s12905-022-01594-4
29. Ambaye E, Regasa ZW, Hailiye G. Early initiation of antenatal care and its associated factors among pregnant women attending antenatal care at public health centres in Bahir Dar Zuria zone, Northwest Ethiopia, 2021: a cross-sectional study. BMJ open. 2023;13(1):e065169. doi:10.1136/bmjopen-2022-065169
30. Girma N, Abdo M, Kalu S, et al. Late initiation of antenatal care among pregnant women in Addis Ababa city, Ethiopia: a facility based cross-sectional study. BMC Womens Health. 2023;23(1):1–8. doi:10.1186/s12905-022-02148-4
31. Adulo LA, Hassen SS. Magnitude and factors associated with late initiation of antenatal care booking on first visit among women in rural parts of Ethiopia. J Racial Ethn Health Disparities. 2022;2022:1–10.
32. Kayemba V, Kabagenyi A, Ndugga P, Wasswa R, Waiswa P. Timing and quality of antenatal care among adolescent mothers in a rural community, Uganda. Adolesc Health Med Ther. 2023;2023:45–61.
33. Dusingizimana T, Ramilan T, Weber JL, et al. Predictors for achieving adequate antenatal care visits during pregnancy: a cross-sectional study in rural Northwest Rwanda. BMC Pregnancy Childbirth. 2023;23(1):1–9. doi:10.1186/s12884-023-05384-0
34. KIT Royal Tropical Institute, National Statistics & Information Authority. Afghanistan health survey 2018; 2019. Available from: https://www.kit.nl/wp-content/uploads/2019/07/AHS-2018-report-FINAL-15-4-2019.pdf.
35. StataCorp. Stata 13 Base Reference Manual. College Station, TX: Stata Press; 2013.
36. Sarker BK, Rahman T, Rahman T, Rahman M. Factors associated with the timely initiation of antenatal care: findings from a cross-sectional study in Northern Bangladesh. BMJ open. 2021;11(12):e052886. doi:10.1136/bmjopen-2021-052886
37. Ejeta E, Dabsu R, Zewdie O, Merdassa E. Factors determining late antenatal care booking and the content of care among pregnant mother attending antenatal care services in East Wollega administrative zone, West Ethiopia. Pan Afr Med J. 2017;27(1). doi:10.11604/pamj.2017.27.184.10926
38. Geta MB, Yallew WW. Early initiation of antenatal care and factors associated with early antenatal care initiation at health facilities in southern Ethiopia. Adv Public Health. 2017;2017:1–6. doi:10.1155/2017/1624245
39. Weldearegawi GG, Teklehaimanot BF, Gebru HT, Gebrezgi ZA, Tekola KB, Baraki MF. Determinants of late antenatal care follow up among pregnant women in Easter zone Tigray, Northern Ethiopia, 2018: unmatched case–control study. BMC Res Notes. 2019;12(1):1–9. doi:10.1186/s13104-019-4789-8
40. Khare SR, Vedel I. Recall bias and reduction measures: an example in primary health care service utilization. Fam Pract. 2019;36(5):672–676. doi:10.1093/fampra/cmz042
41. Grimm P. Social desirability bias. In: Wiley International Encyclopedia of Marketing. UK: John Wiley and Sons, Ltd Chichester; 2010.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

