Back to Journals » Patient Preference and Adherence » Volume 17
Social Support, Quality of Care, and Patient Adherence to Tuberculosis Treatment in Peru: The Mediating Role of Nurse Health Education
Authors Dilas D, Flores R, Morales-García WC , Calizaya-Milla YE , Morales-García M , Sairitupa-Sanchez L, Saintila J
Received 8 October 2022
Accepted for publication 7 December 2022
Published 19 January 2023 Volume 2023:17 Pages 175—186
DOI https://doi.org/10.2147/PPA.S391930
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Delker Dilas,1 Rosarias Flores,1 Wilter C Morales-García,1,* Yaquelin E Calizaya-Milla,2 Mardel Morales-García,3 Liset Sairitupa-Sanchez,4 Jacksaint Saintila5,*
1Unit of Public Health, Postgraduate School, Peruvian Union University, Lima, Perú; 2Research Group for Nutrition and Lifestyle Research, Peruvian Union University, Lima, Perú; 3Faculty of Education, Peruvian Union University, Lima, Perú; 4School of Psychology, Peruvian Union University, Lima, Perú; 5School of Medicine, Señor de Sipán University, Chiclayo, Perú
*These authors contributed equally to this work
Correspondence: Wilter C Morales-García, Unit of Public Health, Postgraduate School, Peruvian Union University, Km 19, Carretera Central, Lima, 15033, Perú, Email [email protected] Jacksaint Saintila, School of Medicine, Señor de Sipán University, Km 5, Carretera a Pimentel, Chiclayo, 14001, Lambayeque, Perú, Email [email protected]
Background: Peru is one of the countries with the highest burden of tuberculosis (TB) and multidrug-resistant tuberculosis (MDR-TB) in the Latin American region and globally. Health education provided by nurses reinforces social support and the quality of patient care allows a greater impact on adherence to TB treatment.
Purpose: This study evaluated the mediating effect of treatment education between social support, quality of care, and treatment adherence in TB patients.
Methods: A cross-sectional study was carried out considering 162 adult TB patients from four health centers of the public sector located in the center of the city of Lima, Peru. Data were collected on variables, such as social support, quality of care, health education, and adherence to TB treatment. SmartPLS was used for data analysis.
Results: The results showed that social support and quality of care significantly influence health education. Likewise, health education mediates social support and quality of care for better adherence to treatment.
Conclusion: It is recommended that hospitals take initiatives to provide better health education on TB treatment to ensure better adherence to treatment.
Keywords: social support, quality of care, education, adherence to treatment, tuberculosis
Introduction
Tuberculosis (TB) is one of the major global public health problems. According to recent data from the World Health Organization (WHO), this disease affects 9.9 million people, including 5.5 million men, 3.3 million women, and 1.1 million children.1 It is an infectious-contagious disease caused by bacillus Mycobacterium tuberculosis that is present in all countries and age groups.1 In Latin America, the largest proportion of cases are in countries such as Brazil and Mexico, including Peru.2 In fact, Peru is among the 40 countries with the highest burden of tuberculosis and multidrug-resistant tuberculosis globally.3 Recently, an increase from 2.5% to 7.3% of MDR-TB cases has been reported in the last two decades.4
TB affects people’s physical health. In fact, TB patients suffer a number of debilitating effects that affect physical well-being and impair quality of life from a physical standpoint.5 Moreover, TB negatively affects the psychological, emotional, and social status of patients, probably because it generates hopelessness, stigma in the community, social isolation, and discrimination due to its infectious nature6 and by the beliefs and prejudices that have been nurtured over the years.7 Such unfounded perceptions become a constant challenge to what TB patients have to deal with, as they face social situations, such as loss of employment after diagnosis, financial constraints, reduced marriage prospects, and lack of social support.7,8 This further contributes to social exclusion and isolation, which, in turn, impacts adherence to treatment.9 TB patients who are not cured or do not adhere to treatment pose a serious risk not only to individuals but also to the community.10 Therefore, it is important to assess the social support and quality of care and health education provided by nursing and to identify adherence to treatment.
Social Support
Despite the condition in which TB patients find themselves, they report almost nonexistent social support from families and community members.5 Social support refers to the resources provided to an individual from institutional centers, community centers, and economic benefits;11 where they are made to believe that they are loved, cared for, esteemed, and members of a network of mutual obligations.12 Previous studies have suggested that social support promotes adherence to TB treatment and a better psychological state by changing affective states, buffering stress, increasing self-efficacy, and promoting positive behaviors.7,13,14 A study conducted in China found that social support is an effective strategy for improving treatment outcomes for TB patients.13 Furthermore, another study showed that nurses’ social support influenced nonadherence.7 However, there is evidence that social support contributes to nonadherence due to negative emotional experiences, such as feelings of guilt and competing interests between the patient and the source of support.15
Quality of Care
Quality of care is another factor associated with adherence to TB treatment. In fact, the quality of care of health professionals plays an important role not only in adherence to TB treatment but also in the control and completion of treatment.16 Improving treatment outcomes for TB patients depends on accessible and effective care that is responsive to patient needs. One study found that lack of availability of daily TB medical care in health facilities was associated with missed daily doses in patients.17 TB patients often discontinue and drop out of treatment when they do not receive adequate supervised care.17,18 Activities such as monitoring adherence to treatment, pill counting, and patient follow-up, providing accurate information could impact adherence to treatment.17
Health Education
Several studies show that treatment education facilitates adherence to TB treatment,19 this is because there is a greater understanding of the side effects and duration of treatment, and it facilitates the procedures for receiving treatment.20 Education strengthens social support and enables improved TB cure rates and improves treatment sustainability.21 Likewise, the quality of education allows to build trust between client-provider and to achieve the success of the treatment. The level of knowledge and beliefs in the treatment allow detection strategies and medical provision, this effective communication adapts to traditions and gives meaning to values, social relations guaranteeing more information, diagnosis and better adherence.22 Therefore, understanding health information allows for proper treatment follow-up.23 Health education about treatment by nurses is essential for both social support and quality of care, which in turn promotes better adherence.
Adherence to Treatment
By definition, adherence is the collaborative acceptance by the TB patient of the treatment given by the health professional.19 Patients not adherent to treatment are at risk of experiencing the increased clinical complexity characterized by resistance to tuberculostatic drugs.19 Likewise, it generates an epidemiological impact with the persistence of foci of disease transmission. Several aspects can lead to non-adherence to TB treatment, including economic factors such as poverty. In fact, people affected by TB are often those who are homeless, malnourished, or migrant.14,24 On the other hand, there are other worrying aspects related to the economic costs that the disease can generate for individuals, households, and state entities; these are closely related to the cost of the disease, which, in turn, leads to social and health consequences, such as lack of adherence and increased spread of the disease.25
Study Hypothesis
Based on the literature review and considering a transmission approach,26 it is required to establish a hypothesis where the mediating variable mediates the relationship between the dependent and independent variable (See Figure 1).
H1: Social support and quality of care positively influences health education. H2: Health education positively influences adherence to TB treatment. H3: Nurse health education mediates the relationship between social support and TB treatment adherence.
 |
Figure 1 Development framework model. |
Materials and Methods
Study Design and Participants
A cross-sectional study was carried out to evaluate patients attending four health centers located in the center of Lima, Peru. Data collection began on January 3 and ended on October 23, 2021. The survey was applied considering patients who were diagnosed with drug-sensitive tuberculosis and who have progressed to stage 2 (this stage comprises infected patients who develop the disease). On the other hand, all patients in the second stage (those exposed to contagion and infected), those with extensively drug-resistant tuberculosis (XDR TB), and MDR TB were excluded. G*Power software was used to determine the minimum sample size required. The following parameters were considered: 0.95 for the power test and 0.15 for the effect size (f2). The results indicated that the minimum sample size was 119 cases. The questionnaire was administered by the interviewer to 162 participants and was acceptable for the SmartPLS partial least squares structural equation modeling (PLS-SEM) technique.27
Ethical Approval
Before starting data collection, consent was requested and obtained from all participants. The study was approved by the Research Ethics Committee of the Universidad Peruana Unión (approval reference number: 2021-CE-FCS-UPeU-00182). In addition, all procedures contributing to the study were performed in accordance with the ethical criteria of the 1975 Declaration of Helsinki and its subsequent modifications.28
Variable Measurements
Quality of Nursing Care
6 items were used to assess patients’ perception of the nurse’s quality of care. It was based on a previous Study29 (eg, “Does the nurse greet you cordially and respectfully when you arrive at the office?” or “Does the nurse guide you in simple words about your illness?”). Responses were categorized into 3 response items from “never” to “always”.
Health Education
Also, health education provided by nurses was assessed by 5 items based on a previous study29 (eg, “Does the nurse advise you about the possible adverse effects of the treatment and how to resolve them?” or “Does the nurse advise you about the consequences, in case of abandoning the treatment?“). Each item contains 3 response options ranging from “never” to “always”.
Social Support
The measurement items for the social support variable were adopted from previous studies.30 The social support questionnaire has 14 items (eg, “someone to advise you when you have problems”) and a Likert-type scale with 5 response options from “never” to “always”.
Adherence to TB Treatment
The TB treatment adherence questionnaire has 5 items (eg, “When do you go to the health center and receive full treatment?”) with 3 response options ranging from “never” to “always”. All items of the scales were adapted for the purposes of the study.31
Statistical Analysis
Partial least squares (SmartPLS 3) were used to analyze the strength of the measurement model. The PLS allows the relationship between latent variables to be represented simultaneously and does not allow for indeterminacy of factor scores.32 Besides assuming the nonparametric assumption of predictors, PLS is a suitable tool because of its predictive power, focusing on variances and does not provide an established overall goodness-of-fit criterion.33,34 It is also reliable in small or large sample sizes, with consistent parameter estimation as the sample size increases. It can be used in a systematic two-step process to measure the model quality that evaluates the measurement model and the structural model,35 thus, convergent validity was used to validate the model by analyzing the composite reliability (CR)33 and Average Variance Extracted (AVE);32 as well as the discriminant validity with the Fornell and Larcker criterion.
For the reliability analysis by scale, Cronbach’s Alpha was used, which ranges from 0 to 1, where a rating of 0.90, 0.80, 0.70 indicate excellent, good and acceptable, respectively.33 The values obtained were: quality of care (0.799), health education (0.818), social support (0.944), and adherence to treatment (0.824). Likewise, the CR was used as a test of convergent validity and covers some deficiencies of Cronbach’s alpha.33 The results indicated adequate composite reliability: quality of care (0.846), health education (0.874), social support (0.950), the adherence to treatment (0.880). The results met the required indicators.
Convergent validity was analyzed, which consists of showing the level at which an indicator correlates positively with other indicators of the same variable. Convergent validity seeks to ensure that the items of the variables used in the study reflect the corresponding factor. Three indicators are considered to determine the convergent validity in Structural equation modeling (SEM), (1) Average Variance Extracted (AVE), (2) reliability, and (3) factor loadings.32 The AVE threshold should be greater than 0.50, indicating that the factors explain half of the variances of their respective indicators. An AVE below 0.50 indicates that the explained variance is less than the error variance.36 In this study, the AVE for all variables exceeded the threshold, ranging from 0.527 to 0.647; therefore, they were acceptable For the reliability analysis per scale, Cronbach’s Alpha was used, which ranges from 0 to 1, where a rating of 0.90, 0.80, and 0.70 indicates excellent, good, and acceptable internal consistency, respectively.33 The values of Cronbach’s Alpha for the variables quality of care, health education, social support, and adherence to treatment were 0.799, 0.818, 0.944, and 0.824, respectively. Likewise, the component reliability (CR) was used as a test of convergent validity, which covers some deficiencies of Cronbach’s alpha.33 According to the results, the CRs for quality of care, health education, social support, and treatment adherence were 0.846, 0.874, 0.95, and 0.880, respectively. The results complied with the required indicators. Regarding item loadings, values higher than 0.6 were considered as recommended by Hair et al.37
Once convergent validity was completed, discriminant validity was checked and the Fornell and Larcker criterion was used.38 Discriminant validity refers to the fact that two indicators are statistically different, it shows the level at which one variable is different from another. The correlations between variables and the square root of the AVE were analyzed, comparing the upper values of the diagonal that should be greater than those shown in the following values of the same column.39
Results
The sample was composed of 162 adult participants: mean age = 38.09, SD= 16.03), ranging from 18 to 82 years. Among them, the majority were male, representing 62.3% of the sample. The greatest proportion were single (51.9%) and 53.1% had secondary education (see Table 1).
 |
Table 1 Demographic Characteristics of Patients |
Measurement Model
Table 2 shows the loadings, reliability (Cronbach’s alpha and PR), and Average Variance Extracted (AVE) and Table 3 shows the discriminant validity (Fornell-Larcker and HTMT). Therefore, the measurement model is valid.
 |
Table 2 Measurement Model |
 |
Table 3 Discriminant Validity |
Structural Model
The model analysis evidenced that social support has a positive and significant influence on health education (β = 0.255, t = 3.075, p<0.01). Quality of care had a positive and significant influence on health education (β = 0.412, t = 2.035, p<0.05), thus these results support H1. Finally, health education had a positive and significant influence on adherence to TB treatment (β = 0.597, t = 4.673, p<0.000); similarly, H2 is not rejected. The model, in total, explains 35.6% of the variation in adherence to TB treatment. Social support and quality of TB care explain 26.3% of the variation in health education. The structural equation model is presented in Figure 2.
 |
Figure 2 Structural equation model. Abbreviations: QTC, quality of care; HE, health education; SP, social support; ATBT, adherence to tuberculosis treatment. |
Mediator Analysis
To evaluate the effect of the mediator variable, the bootstrapping procedure was used.40 Subsamples of 5000 were used to evaluate the model. For the mediation analysis, a significant relationship was considered to exist through the mediator between the independent and dependent variable. Significant indirect effect was considered for evidence of measurement (t value > 1.96, 2-tailed, p < 0.05). Therefore, the mediation effect of health education between social support and TB treatment adherence was confirmed (β = 0.152, t = 2.434, P <0.05). That is, health education influences the link between social support and treatment adherence, therefore, H3 is supported. However, the mediating effect of health education between quality of care and treatment adherence was not supported and was insignificant (β = 0.246, t = 1.576, P >0.05), so quality of care affects treatment adherence; however, its effects are insignificant (Table 4). The results of the mediation model can be seen in Figure S1.
 |
Table 4 Mediating Effect |
In addition, the coefficient of determination (R2), cross-validated redundancy (Q2), and the effect size (f 2) of the dependent variables on the independent variables were evaluated. The R2 values were 0.356 and 0.263, indicating that the independent variables explain 35.6% of the variances in adherence to TB treatment and 26.3% of the variances in health education, indicating adequate explanatory power (Table 5).
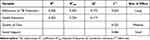 |
Table 5 Determination of Coefficient (R2), Adjusted R-Squared (R2adj), Predictive Relevance (Q2), and Effect Size (F 2) |
The Q2 was also determined by the blindfolding procedure.36 For the model to have predictive relevance according to a dependent variable, the Q2 value must be greater than 0.41 The results indicated that the Q2 values were 0.172 for adherence to tuberculosis treatment and 0.263 for health education, thus indicating the impact of the independent variables have predictive significance on the dependent variables.36 The f2 indicates the impact of the independent variables on the dependent variables. The results show that the effect of quality of care (f 2= 0.225) on health education is greater than social support (f 2= 0.086), indicating that quality of care would have a greater effect on health education (Table 5).
Discussion
This research shows the positive and significant effect of social support on health education, indicating that patients with tuberculosis have a need for health information and social support to provide motivation and supervision in treatment adherence. This result is in line with previous studies.42 In fact, patient support, community support culturally, and treatment plans to patients provide directly and positively impact patients. In addition, social support favors adherence to TB treatment, improving psychological health, decreasing stress, and increasing self-efficacy in the face of the disease.7,13,14 Improved self-efficacy in the face of TB involves patients’ belief in their own ability to succeed in managing the disease.43 On the other hand, one study found that social support is considered an effective strategy for improving treatment outcomes of TB patients.13 Also, another study conducted among patients with tuberculosis in the Philippines showed that the social support provided by nurses to patients influenced adherence to TB treatment.7 However, the lack of resources impedes the provision of support to patients, including for home treatment monitoring.44
Likewise, it was shown that the quality of nursing care significantly influences the health education provided by nurses. This finding is consistent with a previous study in which they found that improved quality of care is closely related to health education in the provision of adequate diagnosis, treatment, and outcome assessment.45 Improved quality of care provided by the nurse may allow for openness, improved communication, and patient confidence, and the patient may be more likely to listen to and apply educational information.46 In the absence of adequate quality of care, the patient may not receive health education with enthusiasm, which may influence the receipt of and adherence to treatment.47 Therefore, the interaction between the nurse and patient should be enthusiastic, motivated, and responsive to the individual and educational needs of the patient.43 This is particularly important because the health education patients receive can improve how they approach treatment goals, health care-related assignments, and challenges related to health improvement.48 In addition, it is worth mentioning that the relationship between the health professional and the patient can be a determining factor in the compliance with the treatment, therefore, it is necessary to provide better quality care characterized by adequate counseling.49
This study also showed that health education has a positive influence on adherence to tuberculosis treatment. This result is consistent with the findings of previous studies that found that increased health education such as monitoring, nurse-led educational intervention is helpful in increasing adherence to anti-TB drugs.50 Similarly, other studies have reported that health education can lead to better adherence to TB treatment;19 this may be due to the fact that it favors a better understanding of the side effects, the duration of treatment, and facilitates the procedures for receiving treatment.20 Health education strengthens social support and enables improved TB treatment rates.21 Similarly, the quality of care helps to build trust between nurses and patients and to achieve treatment success. The education that patients receive improves their level of knowledge, which allows the use of strategies for approaching and managing the disease, guaranteeing greater diagnostic information, control, and better adherence to treatment.22 Therefore, the understanding of health information allows a correct follow-up of the treatment.23 It is important to mention that increased adherence to treatment may be due to patients having a good understanding of TB prevention and treatment; therefore, health education on treatment and comprehensive patient counseling is an important step in adherence to medication and treatment of the disease.51
Likewise, health education was evaluated as a mediating variable in the relationship between social support and adherence to tuberculosis treatment. An indirect relationship was found between the variables under study. This indirect relationship is supported by previous research given that social support encourages adherence to tuberculosis treatment and that this is directed by the personal and social support of health professionals.52,53 It is worth mentioning that the success of treatment of tuberculosis depends to a large extent on the ability of patients to comply with various clinical requirements and lifestyle changes.54 In addition, lack of adherence to treatment remains a major barrier in the management of tuberculosis.54 Similarly, health education can promote successful social support, which has been consistently linked to improved health outcomes in a variety of communicable and noncommunicable diseases.55 Both health education and social support can promote better communication and care for the patient, which allows individual risk factors for noncompliance to be addressed, since patient health education and social support are the main components for adequate adherence to treatment.56
Finally, health education was evaluated as a mediating variable between quality of care and adherence to treatment. Based on the results, quality of care had no indirect relationship with adherence to treatment. Previous results indicate that quality of care is linked to treatment mediated by improved education on interventions.57 The relationship of the current study is supported by the results of this research given that to activate health education by nurses, the patient must first experience quality of care, leading to treatment adherence. This may be due to poor motivation of nurses to implement the guidelines, poor supervision, lack of clinical support, and insufficient knowledge inhibiting adherence to treatment guidelines.58
Limitations
The findings of the current study should be interpreted considering certain limitations. First, the sample was limited because data were collected from patients attending only four health centers in the metropolitan region of Lima, Peru; therefore, the results cannot be generalized. In addition, future studies should consider large hospital centers located in the three regions (coast, jungle, and highlands) of the country in order to provide evidence that can be generalized to patients in other countries. Secondly, this is a cross-sectional study, therefore, it is recommended that patient perception be assessed longitudinally to provide more information. Finally, it is unclear whether the results regarding the mediating action of health education can have the same influence in other contexts, as patient perceptions in other countries may differ.
Public Health Implications
Despite the limitations of the current study, we believe that the results may be relevant for the implementation of policies and strategies to strengthen the mediating effect of nurse health education and ensure adherence to treatment for the benefit of patients. In fact, health education coupled with real-time electronic monitoring, quality of care, and better communication between nurses and patients can promote medication adherence.47,59 In addition, these results may be useful for the activation of social support systems for the benefit of TB patients. Finally, it is important to mention that the success of these aspects (quality of care, adherence to treatment, and health education) will depend on an improvement in the quality of the work environment, regulation of working hours, avoidance of burnout, and favoring better monetary compensation, which can decrease the attrition rate of the workforce and can lead to better practice and performance in nurses.
Conclusion
The findings of the present study could contribute to the implementation of efficient measures to achieve greater adherence to treatment in TB patients. Nurses have the potential to contribute significantly to treatment success by providing better health education that improves preventive behavior, as well as increased participation and decreased prevalence of people affected by TB. The importance of this study lies in presenting the first attempts to develop and test a mediating model linking social support and quality of nursing care through health education to treatment adherence. Research shows that health education may be essential for successful adherence to TB treatment.
Data Sharing Statement
Data supporting the conclusions of this research will be made available in coordination with the corresponding authors.
Acknowledgments
We thank the Dirección Integrada de Redes de Salud Lima Centro, the patients for their valuable time, and Dr. Varisier Noel for his support.
Funding
Open access funding provided by Universidad Señor de Sipán (DIRECTORY RESOLUTION N°015-2022/ PD-USS) and Universidad Peruana Unión (Grant 041- 2022/SA).
Disclosure
The authors have declared that no competing interests exist.
References
1. World Health Organization (WHO). Tuberculosis; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis.
2. Quiroz-Ruiz HR, Sosa-Flores JL, Hernández-Palomino FN. Underreporting and exhaustiveness of tuberculosis surveillance systems in a region of Peru: a capture-recapture analysis. Cad Saude Publica. 2021;37(6). doi:10.1590/0102-311x00276020
3. Khan FMA, Kazmi Z, Hasan MM, et al. Resurgence of tuberculosis amid COVID-19 in Peru: associated risk factors and recommendations. Int J Health Plann Manage. 2021;36(6):2441–2445. doi:10.1002/hpm.3291
4. Quispe N, Asencios L, Obregon C, et al. The fourth national anti-tuberculosis drug resistance survey in Peru. Int J Tuberc Lung Dis. 2020;24(2):207–213. doi:10.5588/ijtld.19.0186
5. Roba AA, Dasa TT, Weldegebreal F, et al. Tuberculosis patients are physically challenged and socially isolated: a mixed methods case-control study of health related quality of life in Eastern Ethiopia. PLoS One. 2018;13(10):e0204697. doi:10.1371/journal.pone.0204697
6. Thomas BE, Shanmugam P, Malaisamy M, et al. Psycho-socio-economic issues challenging multidrug resistant tuberculosis patients: a systematic review. PLoS One. 2016;11(1):e0147397. doi:10.1371/journal.pone.0147397
7. Baniqued MG, Ballecer BAP, Ballesteros BDC, et al. Social support from nurses and non-adherence with directly observed therapy (DOTS) maintenance phase among patients with tuberculosis in Metro Manila, Philippines. Public Health Nurs. 2020;37(3):339–346. doi:10.1111/phn.12714
8. Fuady A, Houweling TAJ, Mansyur M, Richardus JH. Catastrophic total costs in tuberculosis-affected households and their determinants since Indonesia’s implementation of universal health coverage. Infect Dis Poverty. 2018;7(1). doi:10.1186/s40249-017-0382-3
9. Cremers AL, De Laat MM, Kapata N, Gerrets R, Klipstein-Grobusch K, Grobusch MP. Assessing the consequences of stigma for tuberculosis patients in urban Zambia. PLoS One. 2015;10(3):e0119861. doi:10.1371/journal.pone.0119861
10. Dooley KE, Lahlou O, Ghali I, et al. Risk factors for tuberculosis treatment failure, default, or relapse and outcomes of retreatment in Morocco. BMC Public Health. 2011;11(1). doi:10.1186/1471-2458-11-140
11. Estrella J. The theory of social support and its implications for the psychosocial adjustment of cancer patients. Rev Psicol Soc. 1991;6(2):257–271.
12. Cobb S. Social support as a moderator of life stress: psychosomatic medicine. Psychosom Med. 1976;38(5):300–314. doi:10.1097/00006842-197609000-00003
13. Yin J, Wang X, Zhou L, Wei X. The relationship between social support, treatment interruption and treatment outcome in patients with multidrug-resistant tuberculosis in China: a mixed-methods study. Trop Med Int Health. 2018;23(6):668–677. doi:10.1111/tmi.13066
14. Chen B, Peng Y, Zhou L, et al. Social support received by multidrug-resistant tuberculosis patients and related factors: a cross-sectional study in Zhejiang Province, People’s Republic of China. Patient Prefer Adherence. 2016;10:1063–1070. doi:10.2147/PPA.S105655
15. Palant A, Himmel W. Are there also negative effects of social support? A qualitative study of patients with inflammatory bowel disease. BMJ Open. 2019;9(1):e022642. doi:10.1136/bmjopen-2018-022642
16. Girma A, HMariam D, Deribe K. Quality of tuberculosis care in six health facilities of Afar Region, Ethiopia. Ethiop Med J. 2010;48(3):195–202.
17. Mesfin MM, Newell JN, Walley JD, et al. Quality of tuberculosis care and its association with patient adherence to treatment in eight Ethiopian districts. Health Policy Plan. 2009;24(6):457–466. doi:10.1093/heapol/czp030
18. Gebrekidan G, Tesfaye G, Hambisa MT, Deyessa N. Quality of tuberculosis care in private health facilities of Addis Ababa, Ethiopia. Tuberc Res Treat. 2014;2014:1–9.
19. Zago PTN, Maffacciolli R, Mattioni FC, Dalla-Nora CR, Rocha CMF. Nursing actions promoting adherence to tuberculosis treatment: scoping review. Rev Esc Enferm. 2021;55:1–11.
20. Widjanarko B, Gompelman M, Dijkers M, van der Werf MJ. Factors that influence treatment adherence of tuberculosis patients living in Java, Indonesia. Patient Prefer Adherence. 2009;3:231. doi:10.2147/ppa.s6020
21. Moodley N, Saimen A, Zakhura N, et al. “They are inconveniencing us” - exploring how gaps in patient education and patient centred approaches interfere with tb treatment adherence: perspectives from patients and clinicians in the free state Province, South Africa. BMC Public Health. 2020;20(1):1–10. doi:10.1186/s12889-020-08562-3
22. Tomás BA, Pell C, Cavanillas AB, Solvas JG, Pool R, Roura M. Tuberculosis in migrant populations. A systematic review of the qualitative literature. PLoS One. 2013;8(12):e82440.
23. Jové N, Masdeu E, Brugueras S, et al. Threats and interventions during the treatment of tuberculosis in an Inner-city district. Arch Bronconeumol. 2021;57(5):330–337. doi:10.1016/j.arbres.2020.05.025
24. Gao X-F, Rao Y. Quality of life of a migrant population with tuberculosis in West China. Int J Tuberc Lung Dis. 2015;19(2):223–230. doi:10.5588/ijtld.13.0866
25. Grede N, Claros JM, de Pee S, Bloem M. Is there a need to mitigate the social and financial consequences of tuberculosis at the individual and household level? AIDS Behav. 2014;18:542–553. doi:10.1007/s10461-014-0732-0
26. Rungtusanatham M, Miller JW, Boyer KK. Theorizing, testing, and concluding for mediation in SCM research: tutorial and procedural recommendations. J Oper Manag. 2014;32(3):99–113. doi:10.1016/j.jom.2014.01.002
27. Ringle CM, Wende S, Becker JM. SmartPLS 3.
28. Asocición Médica Mundial. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects– WMA – the World Medical Association; 2013. Available from: https://www.wma.net/es/policies-post/declaracion-de-helsinki-de-la-amm-principios-eticos-para-las-investigaciones-medicas-en-seres-humanos/.
29. Herrera V. Percepción del paciente con tuberculosis sobre la calidad de atención que brinda el profesional de enfermería en la estrategia sanitaria de prevención y control de tuberculosis Hospital de Barranca-2013. Universidad Nacional Mayor de San Marcos; 2013.
30. Baca DR. Confiabilidad y validez del cuestionario de apoyo social en pacientes con cáncer de Trujillo. Rev Investig en Psicol. 2016;19(1):177. doi:10.15381/rinvp.v19i1.12452
31. Oliden S, Zapata C. Adherencia al tratamiento y practicas de autocuidado de los pacientes de la estrategia sanitaria nacionla de prevención y control de tuberculosis - centro de salud en villa el salvador, 2019. Universidad Peruana Cayetano Heredia; 2019. Available from: http://repositorio.upch.edu.pe/bitstream/handle/upch/7676/Adherencia_OlidenLozano_Sally.pdf?sequence=1&isAllowed=y%0Ahttps://repositorio.upch.edu.pe/bitstream/handle/20.500.12866/7676/Adherencia_OlidenLozano_Sally.pdf?sequence=1&isAllowed=y.
32. Fornell C, Bookstein FL. Two structural equation models: LISREL and PLS applied to consumer exit-voice theory. J Mark Res. 1982;19(4):440. doi:10.1177/002224378201900406
33. Hair JF, Ringle CM, Sarstedt M. Partial least squares structural equation modeling: rigorous applications, better results and higher acceptance. Long Range Plann. 2013;46(1–2):1–12. doi:10.1016/j.lrp.2013.01.001
34. Urbach N, Ahlemann F. Structural equation modeling in information systems research using partial least squares. J Inf Technol Theor Appl. 2010;11:5–40.
35. Lewis BR, Templeton GF, Byrd TA. A methodology for construct development in MIS research. Eur J Inf Syst2017;14(4):388–400. doi:10.1057/palgrave.ejis3000552
36. Chin WW. The partial least squares approach for structural equation modeling. In: Marcoulides GA, editor. Modern Methods for Business Research. Lawrence Erlbaum Associates Publishers; 1998:295–336.
37. Hair JF, Black WC, Babin BJ, Anderson RE, Tatham RL. Análise Multivariada de Dados. Porto Alegre: Bookman Editora; 2009.
38. Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39. doi:10.1177/002224378101800104
39. Hair JF, Hult GT, Ringle C, Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM) - Joseph F. Hair, Jr., G. Tomas M. Hult, Christian Ringle, Marko Sarstedt. Sage; 2017:374.
40. Kline RB. Principles and Practice of Structural Equation Modeling. Cuarta Ed. New York, NY, US: Guilford Press; 2016.
41. Hair J, Hult G, Ringle C. A Primer on Partial Least Squares Structural Equation Modeling. Los Angeles, CA: Uniwersytet śląski, SAGE Publications; 2014.
42. Nyoman Elfiyunai N, Glorino Rumambo Pandin M, Author C. The Role of Nurses in Providing Social Support in Tuberculosis Treatment: Literature Review. Preprints; 2021.
43. Paterick TE, Patel N, Tajik AJ, Chandrasekaran K. Improving health outcomes through patient education and partnerships with patients. Bayl Univ Med Cent Proc. 2017;30(1):112–113. doi:10.1080/08998280.2017.11929552
44. Jansen-Aaldring N, van de Berg S, van den Hof S. Patient support during treatment for active tuberculosis and for latent tuberculosis infection: policies and practices in European low-incidence countries. J Adv Nurs. 2018;74(12):2755–2765. doi:10.1111/jan.13784
45. Cattamanchi A, Davis JL, Worodria W, et al. Poor performance of universal sample processing method for diagnosis of pulmonary tuberculosis by smear microscopy and culture in Uganda. J Clin Microbiol. 2008;46(10):3325–3329. doi:10.1128/JCM.01175-08
46. Gröndahl W, Muurinen H, Katajisto J, Suhonen R, Leino-Kilpi H. Perceived quality of nursing care and patient education: a cross-sectional study of hospitalised surgical patients in Finland. BMJ Open. 2019;9(4):e023108. doi:10.1136/bmjopen-2018-023108
47. Ramos-Vera C, Saintila J, Calizaya-Milla YE, Acosta Enríquez ME, Serpa Barrientos A. Relationship between satisfaction with medical care, physical health, and emotional well-being in adult men: mediating role of communication. J Prim Care Community Health. 2022;13:215013192211148. doi:10.1177/21501319221114850
48. Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff. 2001;20(6):64–78. doi:10.1377/hlthaff.20.6.64
49. Foster I, Sullivan A, Makanda G, et al. The role of counselling in tuberculosis diagnostic evaluation and contact tracing: scoping review and stakeholder consultation of knowledge and research gaps. BMC Public Health. 2022;2022(1):1–18.
50. Guix-Comellas EM, Rozas-Quesada L, Velasco-Arnaiz E, et al. Impact of nursing interventions on adherence to treatment with antituberculosis drugs in children and young people: a nonrandomized controlled trial. J Adv Nurs. 2018;74(8):1819–1830. doi:10.1111/jan.13692
51. Du L, Chen X, Zhu X, et al. Determinants of medication adherence for pulmonary tuberculosis patients during continuation phase in Dalian, Northeast China. Patient Prefer Adherence. 2020;14:1119. doi:10.2147/PPA.S243734
52. Rajan JC, Anand T, Nagaraja SB, et al. Tuberculosis treatment completion for tribal patients in Kerala: needs constant push! J Tuberc Res. 2019;7(4):185–201. doi:10.4236/jtr.2019.74018
53. Adiutama NM, Fauzi AK. Educational intervention in improving tuberculosis patient’s adherence based on the theory of planned behavior. 2nd Str Int Conf Heal. 2020;2(1):254–263.
54. Sousa H, Ribeiro O, Paúl C, et al. Social support and treatment adherence in patients with end‐stage renal disease: a systematic review. Semin Dial. 2019;32(6):562–574. doi:10.1111/sdi.12831
55. Griva K, Nandakumar M, Ng J-AH, et al. Hemodialysis self-management intervention randomized trial (HED-SMART): a practical low-intensity intervention to improve adherence and clinical markers in patients receiving hemodialysis. Am J Kidney Dis. 2018;71(3):371–381. doi:10.1053/j.ajkd.2017.09.014
56. Kielmann K, Vidal N, Riekstina V, et al. “Treatment is of primary importance, and social assistance is secondary”: a qualitative study on the organisation of tuberculosis (TB) care and patients’ experience of starting and staying on TB treatment in Riga, Latvia. PLoS One. 2018;13(10):e0203937. doi:10.1371/journal.pone.0203937
57. Subbaraman R, Nathavitharana RR, Mayer KH, et al. Constructing care cascades for active tuberculosis: a strategy for program monitoring and identifying gaps in quality of care. PLOS Med. 2019;16(2):e1002754. doi:10.1371/journal.pmed.1002754
58. Makhado L, Davhana-Maselesele M, Farley JE. Barriers to tuberculosis and human immunodeficiency virus treatment guidelines adherence among nurses initiating and managing anti-retroviral therapy in KwaZulu-Natal and North West provinces. Curationis. 2018;41(1). doi:10.4102/curationis.v41i1.1808
59. Musiimenta A, Tumuhimbise W, Atukunda EC, et al. Mobile health technologies may be acceptable tools for providing social support to tuberculosis patients in Rural Uganda: a parallel mixed-method study. Tuberc Res Treat. 2020;2020:1–8.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
