Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 14
Smoking, Hypertension, and GG Genotype of the IL-6 rs1800796 Polymorphism are Independent Risk Factors for Abdominal Aortic Aneurysm in Han Population
Received 11 July 2021
Accepted for publication 20 August 2021
Published 7 September 2021 Volume 2021:14 Pages 1115—1121
DOI https://doi.org/10.2147/PGPM.S328894
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Yuchao Zhang, Gang Xu, Ping Wang
Department of Vascular Surgery, The Affiliated Huaian No. 1 People’s Hospital of Nanjing Medical University, Huaian City, 223300, People’s Republic of China
Correspondence: Ping Wang Tel/Fax +86-0517-80872149
Email [email protected]
Background: Recent researches have investigated the link between the rs1800796 polymorphism (− 572G/C) in the interleukin-6 (IL-6) gene and the risk of abdominal aortic aneurysm (AAA). However, no Chinese studies have addressed the association between the risk of AAA and this polymorphism.
Methods: This case-control study included 153 AAA patients and 205 controls. Diabetes mellitus, hypertension, dyslipidemia, and coronary artery disease (CAD) status were collected. The AAA and control groups were 69.20 ± 7.56 and 68.50 ± 7.12 years old, respectively.
Results: The analysis revealed that the G allele and GG genotype of the IL-6 rs1800796 polymorphism were remarkedly correlated with an elevated risk of AAA. The GG genotype displayed an association with the risk of AAA after adjustment for gender, body mass index, age, drinking, and smoking. Subgroup analyses indicated that this polymorphism elevated the risk of AAA among males, individuals aged ≥ 70 years, smokers, drinkers, individuals with a body mass index (BMI) ≥ 25 kg/m2, patients without diabetes, and patients with hypertension. Univariate and multivariate analyses indicated that smoking, hypertension, and the GG genotype (rs1800796 polymorphism) were independently related with the risk of AAA.
Conclusion: The IL-6 rs1800796 polymorphism increases the risk of AAA. In addition, smoking, hypertension, and the GG genotype of the rs1800796 polymorphism are independent risk factors for AAA. Further studies of Chinese populations are needed to validate these findings.
Keywords: IL-6, abdominal aortic aneurysm, rs1800796 polymorphism, risk factors
Introduction
Abdominal aortic aneurysm (AAA) is a deadly disease associated with high morbidity and mortality in the event of aortic rupture.1 AAA is usually asymptomatic unless complications occur, and is often diagnosed via ultrasonography screening programs.2,3 Currently, the only treatment for patients with AAA is open or endovascular surgical repair, and no drug therapy is available. Studies have identified a host of risk factors for AAA, including old age, smoking, family history of AAA, male sex, presence of other cardiovascular diseases, hypertension, and dyslipidemia.4–6 Among these risk factors, smoking is the most critical. AAA has been attributed to many environmental and genetic factors.7 Genetic studies have identified many novel loci for AAA.8–11
Although the pathogenesis of AAA is unclear, accumulating evidence supports a central role for inflammation.12,13 Interleukin-6 (IL-6), a crucial proinflammatory cytokine, participates in many inflammatory responses, and in the development and complications of atherosclerotic disease.14 IL-6 has been implicated in the molecular pathway underlying vascular inflammation in AAA.15,16 An animal study showed that IL-6 was involved in the pathogenesis of AAA in mice.17 Tang et al performed a study with over 24 years of follow-up that showed that blood concentrations of IL-6 predicted the risk of AAA.18 Lindberg et al indicated that IL-6 was an inflammatory marker associated with AAA.19
The IL-6 gene, locating on chromosome 7p21, has four introns and five exons. Two recent studies addressed the potential correlation between the rs1800796 polymorphism (−572G/C) in the IL-6 gene and AAA risk.20,21 However, they yielded conflicting results. In addition, no Chinese studies have explored the link between this locus and risk of AAA. Thus, we designed this case-control study to test for a correlation between the rs1800796 polymorphism and risk of AAA in Chinese Han subjects.
Patients and Methods
Subjects
In this study, we recruited 153 patients with AAA and 205 controls from our hospital, from March 2016 to May 2020. All individuals were recruited consecutively during this period. The inclusion criterion for AAA included an abdominal aorta with a diameter of > 3 cm, as revealed by computed tomography angiography or ultrasound.5 The individuals serving as controls were recruited during the same time period from this hospital. Clinical information was collected, including age, sex, body mass index (BMI), smoking and drinking history, diabetes mellitus, hypertension disease, dyslipidemia, and coronary artery disease (CAD). All relevant information was extracted from medical records and questionnaires. Patients having hypertension should be with a diastolic blood pressure > 90 mmHg and/or systolic blood pressure > 140 mmHg. Diabetes mellitus patients were diagnosed when their fasting glucose levels were over 126 md/dl.22 The diagnosis of CAD was based on electrocardiogram, echocardiography, and coronary angiography results. Subjects with total cholesterol levels of ≥ 200 mg/dL (or exceeding 5.17 mmol/L) were defined as having dyslipidemia.23 Smokers were defined as individuals who had more than one cigarette/day on average for at least 1 year. Drinkers were defined as individuals who drank over 15 g/d of ethanol on average. The informed consent form was signed by all participating individuals. The Ethics Committee of Huaian No.1 People’s Hospital approved the protocol of this study. Then, this study was in according with the Helsinki declaration.
Genotyping
Blood samples from peripheral veins were gathered from all subjects for DNA extraction. The IL-6 rs1800796 polymorphism was genotyped using PCR-RFLP, and 10% of the samples were reanalyzed to determine if there were any potential genotyping errors; all genotyping results were consistent with previous results.
Statistical Analysis
Continuous variables (conforming to normal distribution) were mainly analyzed using Student’s t test. Categorical variables were analyzed utilizing the chi-square (χ2) test. 95% confidence intervals (CIs) and odds ratios (ORs) were determined to estimate the association between the IL-6 rs1800796 polymorphism and AAA risk with adjustment for gender, age, smoking, drinking, and BMI. The Hardy-Weinberg equilibrium (HWE) was calculated for the controls using the goodness-of-fit χ2 test. Univariate or multivariate regression analyses was used to identify relevant predictors of AAA. Cross-over analysis was utilized to estimate the correlation between genetic and environmental factors. A P-value < 0.05 indicated that it was statistically significant. Statistical analyses were calculated by use of SPSS software (ver. 21.0; SPSS Inc., Chicago, IL, USA).
Results
Demographic Data and Clinical Parameters of All Individuals
Table 1 shows the clinical characteristics and demographic information of all participants, including 153 patients with AAA and 205 control individuals. The participants in the AAA and control groups were aged 69.20 ± 7.56 and 68.50 ± 7.12 years, respectively. The age and gender were matched between the groups (P > 0.05). In addition, the rates of smoking, hypertension, dyslipidemia, and CAD in patients with AAA were remarkedly higher than in the controls (P < 0.05).
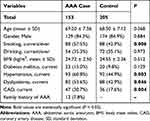 |
Table 1 Demographics and Clinical Characteristics of Study Subjects |
Association with the rs1800796 Polymorphism and AAA Risk
Table 2 shows that the genotype distribution in this study was in conformance with the HWE test in controls (PHWE = 0.767). Table 2 summarizes the allele and genotype numbers and frequencies of the investigated locus. The GG genotype of the IL-6 rs1800796 polymorphism was significantly related to an elevated risk of AAA (GG versus CC, OR, 3.06; 95% CI, 1.45–6.48; P = 0.003; GG versus CC + CG, OR, 2.99; 95% CI, 1.45–6.20; P = 0.003); and this significant association was still available after adjusting for age, gender, smoking, BMI, and drinking. In addition, the G allele showed a higher risk of AAA (G versus C, OR, 1.54; 95% CI, 1.11–2.15; P = 0.010).
 |
Table 2 Correlation Between the IL-6 rs1800796 Polymorphism and Abdominal Aortic Aneurysm Risk |
Next, we conducted subgroup analyses to address the correlation between this polymorphism and AAA for various factors, including gender, age, smoking, alcohol, BMI, diabetes mellitus, and hypertension (Table 3). We observed that the rs1800796 polymorphism correlated with an enhanced risk of AAA among males, individuals aged ≥ 70 years, smokers, drinkers, individuals with a BMI ≥ 25 kg/m2, patients without diabetes, and patients with hypertension.
 |
Table 3 Stratified Analyses Between the IL-6 rs1800796 Polymorphism and Risk of Abdominal Aortic Aneurysm |
Interactions Between Genetic Factors and Smoking/Drinking
Subgroup analyses indicated a potential association between the rs1800796 polymorphism and smoking/drinking was shown. To validate these findings, we used cross-over analysis to investigate the relationship between this polymorphism and smoking and drinking (Supplemental Table 1). Data revealed that smokers or drinkers carrying the GG genotype had an elevated risk of developing AAA (GG+ smoking vs CC+ non-smoking: OR, 4.87, 95% CI, 1.92–12.37; P < 0.001; GG+ drinking vs CC+ non-smoking: OR, 3.77, 95% CI, 1.14–12.47; P = 0.022).
Risk Factors for AAA: Results of Univariate and Multivariate Analysis
In the abovementioned analyses, we observed that genetic and environmental factors were associated with AAA development (Table 4). Univariate and multivariate analyses were performed to identify other related risk factors for AAA, including age, gender, smoking, drinking, BMI, diabetes mellitus, hypertension, dyslipidemia, CAD, and the rs1800796 polymorphism genotypes. The univariate analysis indicated that smoking, hypertension, dyslipidemia, CAD, and GG genotype correlated with the risk of AAA. The multivariate analysis suggested that smoking, hypertension and GG genotype were independent risk factors for AAA.
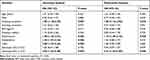 |
Table 4 Univariate and Multivariate Analysis for Related Risk Factors in Abdominal Aortic Aneurysm |
Discussion
In this study, we observed that the rs1800796 polymorphism in the IL-6 gene showed an association with an elevated risk of AAA in this Chinese Han population. Subgroup analyses confirmed association in males, individuals aged ≥ 70 years, smokers, drinkers, individuals with a BMI ≥ 25 kg/m2, patients without diabetes, and patients with hypertension. Cross-over analysis showed an interaction between the IL-6 rs1800796 polymorphism and smoking or drinking. In addition, univariate and multivariate analyses indicated that smoking, hypertension, and the GG genotype of the IL-6 rs1800796 polymorphism were independent risk factors for AAA.
Pathological changes in the aorta in cases of thoracic aortic aneurysm are related to IL-6.24 IL-6 was involved in the early inflammatory response in patients with AAA.25 IL-6 gene variants may participate in the development of AAA by regulating IL-6 levels. Two previous studies explored the potential link between AAA risk and the rs1800796 polymorphism.20,21 An Australian study by Smallwood et al uncovered that the rs1800796 polymorphism in the IL-6 gene was related to an elevated risk of AAA.21 However, they pointed out that the C allele frequency in AAA patients was low, and it may not be the major driver of AAA.21 A recent Austrian study by Jabłońska et al found that this polymorphism (rs1800796) did not associate with the risk of AAA.20 In addition to AAA, the correlation between the targeted polymorphism and intracranial aneurysm (IA) risk has also attracted the interest of researchers. In a UK study, Morgan et al were the first to find that the IL-6 rs1800796 polymorphism was a protective factor for IA.26 However, an Italian study could not verify this association in aneurysmal subarachnoid haemorrhage.27 An Indian study also observed no association between the rs1800796 polymorphism and IA risk.28 In early Chinese studies, the rs1800796 polymorphism was a risk factor for IA.29–31 However, another Chinese study indicated that this locus was not a risk factor for IA.32 Ethnic differences may not explain these inconsistencies, because the researchers also enrolled individuals from a Chinese Han population. Regional differences, differed sample sizes, and diverse risk factors may explain the discrepancies.
In this study, we explored the IL-6 rs1800796 polymorphism in AAA rather than IA. We detected that this targeted polymorphism enhanced the risk of AAA in a Chinese Han population, in line with the findings of Smallwood et al described above.21 It is of note that there was a significant difference between this study and that of Smallwood et al with respect to the genotype frequencies. To the best of our knowledge, this is the first study from China to show that the IL-6 rs1800796 polymorphism elevated the risk of AAA in a Chinese Han population.
Subgroup analysis suggested that the rs1800796 polymorphism increased the risk of AAA among males, individuals aged ≥ 70 years, smokers, drinkers, individuals with a BMI ≥ 25 kg/m2, individuals without diabetes, and patients with hypertension. Anagnostakos et al showed that smoking was a crucial risk factor for AAA.33 The prevalence and incidence rates of AAA have decreased over the last two decades, attributed partially to the decline in smoking prevalence.34 Furthermore, AAA is a multifactorial disorder, and genetic and environmental factors contribute to its development.35,36 Thus, we studied gene-environment interactions using cross-over analysis, and found an interaction between the IL-6 rs1800796 polymorphism and smoking/drinking. In addition, our multivariate analysis revealed that smoking, hypertension and the GG genotype were independent risk factors for AAA. However, Smallwood et al found that age, diastolic blood pressure, smoking, history of myocardial infarction, history of coronary artery surgery, treatment for hypertension, obesity, vigorous exercise, and the IL-6 gene genotype were also independent risk factors for AAA.21 Obviously, this study did not identify some risk factors for AAA mentioned by Smallwood et al.21 We hypothesized that several factors including sample size, clinical heterogeneity, and racial differences, may explain the discrepant findings. Further studies are needed to validate this.
Several limitations of this study should be noted. First, we did not investigate the impacts of this polymorphism on the survival of AAA. Jones et al showed that another variant in the IL-6 gene could predict the cardiovascular mortality of AAA.37 Second, the sample size was relatively small in this study. Studies with larger sample sizes are urgently needed. Third, only one polymorphism was explored in this study. Other variants in the IL-6 gene should be investigated in future studies, because a single SNP only has a limited impact on the risk of AAA. Fourth, the potential mechanisms why this polymorphism elevated the risk of AAA should be addressed by performing some cell and animal experiments. Finally, the findings cannot be generalized to other populations because only the Chinese Han population was investigated.
In summary, the IL-6 rs1800796 polymorphism increases the risk of AAA in a Chinese Han population. Stratified analysis confirms that this elevated risk in males, individuals aged ≥ 70 years old, smokers, drinkers, individuals with a BMI ≥ 25 kg/m2, patients without diabetes, and patients with hypertension. Cross-over analysis indicates an interaction of this polymorphism with smoking or drinking. In addition, smoking, hypertension, and the GG genotype are independently related to the risk of AAA. Studies of other ethnic groups should be conducted, which may verify the findings observed in this study.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Golledge J, Moxon JV, Singh TP, Bown MJ, Mani K, Wanhainen A. Lack of an effective drug therapy for abdominal aortic aneurysm. J Intern Med. 2020;288(1):6–22. doi:10.1111/joim.12958
2. Oliver-Williams C, Sweeting MJ, Turton G, et al. Lessons learned about prevalence and growth rates of abdominal aortic aneurysms from a 25-year ultrasound population screening programme. Br J Surg. 2018;105(1):68–74. doi:10.1002/bjs.10715
3. Kerut EK, To F, Summers KL, Sheahan C, Sheahan M. Statistical and machine learning methodology for abdominal aortic aneurysm prediction from ultrasound screenings. Echocardiography. 2019;36(11):1989–1996. doi:10.1111/echo.14519
4. Singh K, Bonaa KH, Jacobsen BK, Bjork L, Solberg S. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: the Tromso Study. Am J Epidemiol. 2001;154(3):236–244. doi:10.1093/aje/154.3.236
5. Golledge J. Abdominal aortic aneurysm: update on pathogenesis and medical treatments. Nat Rev Cardiol. 2019;16(4):225–242. doi:10.1038/s41569-018-0114-9
6. Golledge J, Muller J, Daugherty A, Norman P. Abdominal aortic aneurysm: pathogenesis and implications for management. Arterioscler Thromb Vasc Biol. 2006;26(12):2605–2613. doi:10.1161/01.ATV.0000245819.32762.cb
7. Mangum KD, Farber MA. Genetic and epigenetic regulation of abdominal aortic aneurysms. Clin Genet. 2020;97(6):815–826. doi:10.1111/cge.13705
8. Klarin D, Verma SS, Judy R, et al. Genetic architecture of abdominal aortic aneurysm in the million veteran program. Circulation. 2020;142(17):1633–1646. doi:10.1161/CIRCULATIONAHA.120.047544
9. Marsman J, Gimenez G, Day RC, Horsfield JA, Jones GT. A non-coding genetic variant associated with abdominal aortic aneurysm alters ERG gene regulation. Hum Mol Genet. 2020;29(4):554–565. doi:10.1093/hmg/ddz256
10. Tang W, Saratzis A, Pattee J, et al. Replication of newly identified genetic associations between abdominal aortic aneurysm and SMYD2, LINC00540, PCIF1/MMP9/ZNF335, and ERG. Eur J Vasc Endovasc Surg. 2020;59(1):92–97. doi:10.1016/j.ejvs.2019.02.017
11. Li J, Pan C, Zhang S, et al. Decoding the genomics of abdominal aortic aneurysm. Cell. 2018;174(6):1361–1372 e1310. doi:10.1016/j.cell.2018.07.021
12. Golledge AL, Walker P, Norman PE, Golledge J. A systematic review of studies examining inflammation associated cytokines in human abdominal aortic aneurysm samples. Dis Markers. 2009;26(4):181–188. doi:10.3233/DMA-2009-0629
13. Jalalzadeh H, Indrakusuma R, Planken RN, Legemate DA, Koelemay MJ, Balm R. Inflammation as a predictor of abdominal aortic aneurysm growth and rupture: a systematic review of imaging biomarkers. Eur J Vasc Endovasc Surg. 2016;52(3):333–342. doi:10.1016/j.ejvs.2016.05.002
14. Mihara M, Hashizume M, Yoshida H, Suzuki M, Shiina M. IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin Sci (Lond). 2012;122(4):143–159. doi:10.1042/CS20110340
15. Ijaz T, Tilton RG, Brasier AR. Cytokine amplification and macrophage effector functions in aortic inflammation and abdominal aortic aneurysm formation. J Thorac Dis. 2016;8(8):E746–754. doi:10.21037/jtd.2016.06.37
16. Kokje VBC, Gabel G, Koole D, et al. IL-6: a Janus-like factor in abdominal aortic aneurysm disease. Atherosclerosis. 2016;251:139–146. doi:10.1016/j.atherosclerosis.2016.06.021
17. Nishihara M, Aoki H, Ohno S, et al. The role of IL-6 in pathogenesis of abdominal aortic aneurysm in mice. PLoS One. 2017;12(10):e0185923. doi:10.1371/journal.pone.0185923
18. Tang W, Yao L, Hoogeveen RC, et al. The Association of Biomarkers of Inflammation and Extracellular Matrix Degradation With the Risk of Abdominal Aortic Aneurysm: the ARIC Study. Angiology. 2019;70(2):130–140. doi:10.1177/0003319718785278
19. Lindberg S, Zarrouk M, Holst J, Gottsater A. Inflammatory markers associated with abdominal aortic aneurysm. Eur Cytokine Netw. 2016;27(3):75–80. doi:10.1684/ecn.2016.0381
20. Jablonska A, Zagrapan B, Neumayer C, et al. Polymorphisms in the IL-6 and TNF-alpha gene are associated with an increased risk of abdominal aortic aneurysm. Int J Cardiol. 2021;329:192–197. doi:10.1016/j.ijcard.2020.12.051
21. Smallwood L, Allcock R, van Bockxmeer F, et al. Polymorphisms of the interleukin-6 gene promoter and abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2008;35(1):31–36. doi:10.1016/j.ejvs.2007.08.021
22. de Boer IH, Bangalore S, Benetos A, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(9):1273–1284. doi:10.2337/dci17-0026
23. Kopin L, Lowenstein C. Dyslipidemia. Ann Intern Med. 2017;167(11):ITC81–ITC96. doi:10.7326/AITC201712050
24. Rabajdova M, Urban P, Spakova I, et al. Detection of pathological changes in the aorta during thoracic aortic aneurysm progression on molecular level. Dis Markers. 2017;2017:9185934. doi:10.1155/2017/9185934
25. Wallinder J, Skagius E, Bergqvist D, Henriksson AE. Early inflammatory response in patients with ruptured abdominal aortic aneurysm. Vasc Endovascular Surg. 2010;44(1):32–35. doi:10.1177/1538574409339358
26. Morgan L, Cooper J, Montgomery H, Kitchen N, Humphries SE. The interleukin-6 gene −174G>C and −572G>C promoter polymorphisms are related to cerebral aneurysms. J Neurol Neurosurg Psychiatry. 2006;77(8):915–917. doi:10.1136/jnnp.2005.081976
27. Fontanella M, Rainero I, Gallone S, et al. Interleukin 6 gene polymorphisms are not associated with aneurysmal subarachnoid haemorrhage in an Italian population. J Neurol Neurosurg Psychiatry. 2008;79(4):471–473. doi:10.1136/jnnp.2007.131565
28. Sathyan S, Koshy LV, Srinivas L, et al. Pathogenesis of intracranial aneurysm is mediated by proinflammatory cytokine TNFA and IFNG and through stochastic regulation of IL10 and TGFB1 by comorbid factors. J Neuroinflammation. 2015;12:135. doi:10.1186/s12974-015-0354-0
29. Sun H, Zhang D, Zhao J. The interleukin-6 gene −572G>C promoter polymorphism is related to intracranial aneurysms in Chinese Han nationality. Neurosci Lett. 2008;440(1):1–3. doi:10.1016/j.neulet.2008.04.077
30. Zhang G, Tu Y, Feng W, Huang L, Li M, Qi S. Association of interleukin-6-572G/C gene polymorphisms in the Cantonese population with intracranial aneurysms. J Neurol Sci. 2011;306(1–2):94–97. doi:10.1016/j.jns.2011.03.036
31. Liu Y, Sun J, Wu C, Cao X, He M, You C. The interleukin-6-572G/C gene polymorphism and the risk of intracranial aneurysms in a Chinese population. Genet Test Mol Biomarkers. 2012;16(7):822–826. doi:10.1089/gtmb.2012.0004
32. Xu L, Hu L, Hu C, et al. Associations between inflammatory cytokine gene polymorphisms and susceptibilities to intracranial aneurysm in Chinese Population. Biomed Res Int. 2021;2021:8865601. doi:10.1155/2021/8865601
33. Anagnostakos J, Lal BK. Abdominal aortic aneurysms. Prog Cardiovasc Dis. 2021;65:34–43. doi:10.1016/j.pcad.2021.03.009
34. Avishay DM, Reimon JD. Abdominal Aortic Repair. Treasure Island (FL): StatPearls; 2021.
35. Kim HW, Stansfield BK. Genetic and epigenetic regulation of aortic aneurysms. Biomed Res Int. 2017;2017:7268521. doi:10.1155/2017/7268521
36. Sakalihasan N, Michel JB, Katsargyris A, et al. Abdominal aortic aneurysms. Nat Rev Dis Primers. 2018;4(1):34. doi:10.1038/s41572-018-0030-7
37. Jones KG, Brull DJ, Brown LC, et al. Interleukin-6 (IL-6) and the prognosis of abdominal aortic aneurysms. Circulation. 2001;103(18):2260–2265. doi:10.1161/01.cir.103.18.2260
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
